Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4709
Peer-review started: January 27, 2021
First decision: February 25, 2021
Revised: March 5, 2021
Accepted: May 6, 2021
Article in press: May 6, 2021
Published online: June 26, 2021
Processing time: 135 Days and 9 Hours
Diabetes is one of the most common chronic diseases of childhood. School plays an essential role in the management of student diabetes, which reduces the risk of short- and long-term diabetes complications and ensures that students are well-positioned for optimal academic performance and growth.
The aim of this review was to systematically identify and synthesize the literature concerning theory-based diabetes care interventions in K-12 schools in the United States. It critically assessed the specific role of theories and associated essential constructs in intervention design, implementation, outcome measurement, and evaluation.
Relevant literature was identified by keyword searches of the Cochrane Library, PubMed, and Web of Science.
Four interventions met the eligibility criteria and were included in the review. Of those, two evaluated online diabetes education programs for school personnel and the other two assessed in-person interventions. Three studies adopted a one-group pre-post study design, and the remaining one adopted a one-shot case-study design. Three of the interventions adopted social cognitive theory, and the remaining one was guided by the diffusion of innovations theory. Three studies identified core constructs of a theory as predictors of behavioral change. Two used theory to select or develop intervention techniques. Two studies used theory to customize participant intervention techniques. Two studies discussed their findings in the context of theory. No study used theory to select potential intervention participants.
In conclusion, despite the value of theory in intervention design and evaluation, theory-based diabetes interventions at school remain scarce. Future research may seek ways to better integrate theory and empirical research.
Core Tip: This critical review found that theory-based diabetes care interventions in United States schools are lacking. In the rare cases where theories were applied, insufficient application and underutilization of theoretical constructs were common. Future investigations should consider applying theories in the design of intervention components and linking essential theory-relevant constructs to intervention techniques. Theory-based interventions provide opportunities to identify mediators of behavior change and effective intervention components.
- Citation: An RP, Li DY, Xiang XL. Role of theories in school-based diabetes care interventions: A critical review. World J Clin Cases 2021; 9(18): 4709-4720
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4709.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4709
Diabetes is one of the most common chronic diseases of childhood[1]. In the United States, approximately 210000 children and adolescents are living with diagnosed diabetes[2,3]. School plays an essential role in the management of student diabetes, which reduces the risk of short- and long-term diabetes complications and ensures that students are well-positioned for optimal academic performance and growth[4]. Section 504 of the Rehabilitation Act of 1973, the Americans with Disabilities Act, and the Individuals with Disabilities Education Act require schools to provide diabetes care during the school day, field trips, and all school-sponsored events so that students with diabetes may participate in school activities with little disruption[5,6]. However, the unmet needs of students with diabetes have been widely reported. Many experience discrimination at school[7,8]. They may be prohibited from consuming needed snacks in the classroom and may not receive assistance in monitoring blood glucose or administering insulin[9-11]. Some districts require students to attend a different school from their assigned one to receive diabetes care[12-14].
A number of interventions have been conducted in school settings with the aim of improving diabetes care quality through knowledge dissemination and skill training[15-17]. Some interventions were theory-based, and explicitly adopted, measured, or tested relevant theoretical constructs on intervention outcomes[18-20]. These interventions should be distinguished from “theory-inspired” interventions, in which some theoretical framework is mentioned but does not follow through in study design, measurement construction, data collection, and hypothesis testing[18,19]. Explicit use of theory in experimental design and evaluation can be valuable for several reasons. Theory-based interventions may identify key underpinning constructs that lead to changes of behavioral outcomes[18,19]. Applying theoretical constructs may facilitate the selection and refinement of intervention techniques[18]. Moreover, explicit use of theory in interventions may generate critical evidence concerning differences in effectiveness across settings and target populations, acting as a catalyst in an ascending spiral of accumulating empirical evidence and theory advancement[18,20]. To our knowledge, no review has been conducted to critically assess the application of theories to school-based diabetes care interventions.
This study systematically identified and synthesized the literature on theory-based diabetes care interventions in K-12 schools in the United States. It critically assessed the specific role of theories and constructs in intervention design, implementation, outcome measurement, and evaluation. The review findings could highlight the gaps and limitations in applying theory in diabetes care in schools and inform future investigations.
A systematic review protocol was used to identify articles that satisfied the predetermined eligibility criteria. Intervention characteristics, theories applied, the role of theory in guiding the intervention, and the main study findings were synthesized.
Studies that met all of the following criteria were included: (1) The study aim was to describe and evaluate diabetes care interventions in school settings; (2) The study design included an experiment/intervention; (3) The study participants were students with type 1 or type 2 diabetes, parents/guardians, school nurses, nonmedical school personnel involved in diabetes care, or other diabetes care stakeholders at the school; (4) The school was a public or private K-12 school in the United States; (5) The article was a peer-reviewed publication; (6) The article was published between the inception of a bibliographic database and October 10, 2020; and (7) The article was written in English. The algorithms used to search the three bibliographic databases are shown in the Supplementary Material.
Studies that met any of the following criteria were excluded: (1) The interventions were not explicitly inspired by or did not apply an existing theory; (2) It was an observational study or intervention that focused only on school-based diabetes prevention and not on diabetes care; (3) The study was conducted outside the United States; (4) The article was not written in English; and (5) Letters, editorials, reviews, or non-peer-reviewed articles were not eligible.
A keyword search was conducted in three electronic bibliographic databases, the Cochrane Library, PubMed, and Web of Science. The search algorithm included all possible combinations of two groups of keywords: (1)“school” or “schools;” and (2) “diabetes,” “diabetic,” or “diabetics.” The MeSH terms “schools” and “diabetes mellitus” were included in the PubMed search. The titles and abstracts of the articles identified by the keyword search were independently screened by two authors, and Cohen’s kappa (κ = 0.74) was used to assess inter-rater agreement. Discrepancies between the two authors were resolved through discussion. Potentially eligible articles were retrieved and full text copies were evaluated.
A “backward” reference list search and a “forward” search of the reference lists of cited articles were conducted based on the full text of articles that had been screened and met the study selection criteria. Articles identified from the backward and forward reference search were further screened and evaluated using the same study selection criteria. The reference search was repeated on all newly identified articles until no additional relevant articles were found.
A standardized data extraction form was used to collect the study characteristics, which included the authors, year of publication, study design, participant characteristics, sample size, school characteristics, intervention components, and intervention aims. We summarized the theory applied to the intervention, the specific role of theory in guiding the intervention and measurement, the operationalization and measurement of theoretical constructs, and the effectiveness of the intervention.
To assess the quality of theory application in interventions, we adapted the coding scheme described by Michie and Prestwich[18]. The scheme consisted of six true-or-false items: (1) “Theory was used to predict study participant behavior;” (2) “Theory was used to select participants for the intervention;” (3) “Theory was used to select or develop the intervention and relevant measures;” (4) “Theory was used to tailor/customize the intervention to study participants;” (5) “Theory-relevant constructs were evaluated in the study;” and (6)“Results were discussed in the context of the theory.”
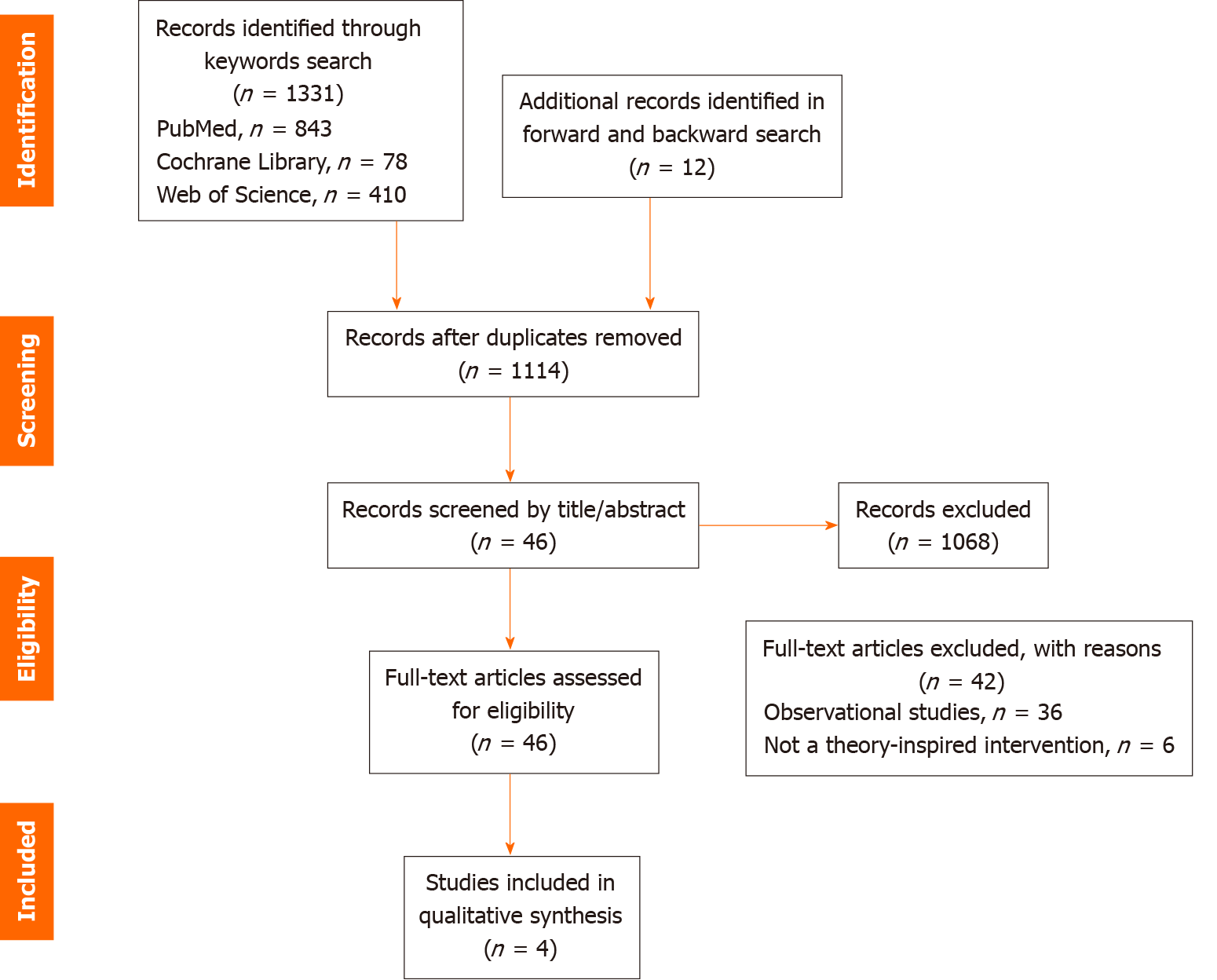
Figure 1 shows the study selection flowchart. The keyword search resulted in 1331 articles, including 843 from PubMed, 78 from the Cochrane Library, and 410 from the Web of Science. The reference list search identified an additional 12 articles. After removing duplicates, the titles and abstracts of 1114 unique articles were screened, and 46 articles were selected for full text review. Of those, 42 articles were excluded, 36 observational studies, and six that did not explicitly state the use of theory in guiding the interventions. Four interventions met the eligibility criteria and were included in this review.
Table 1 summarizes the characteristics of the four interventions. The year of publication ranged from 2005 to 2019. Three studies adopted a one-group pre-post study design and measured outcomes over time[21-23]. One adopted a one-shot case-study design and measured only post-intervention outcomes[24]. Stakeholder participation included school nurses in all the study interventions[21-24], three of which evaluated individual-level outcomes of school nurses[22-24]. One study also included health aides, and one involved nonmedical school personnel (e.g., classroom teachers, office staff, and bus drivers)[22]. Only one study assessed individual-level outcomes of students with diabetes[21].
| Study ID | Ref. | Study design | Participants: Sample size | School characteristics | Intervention aims | Intervention components |
| 1 | Faro et al[21], 2005 | Single group pre-post | Students: 27 (15 boys, 12 girls) | K-12 schools in a large urban district in New York | (1) Increase school nurse knowledge and confidence in performing diabetes care. (2) Strengthen collaboration between school health personnel and diabetes specialists. (3) Improve student self-efficacy and self-management skills | (1) Regular school visits by pediatric nurse practitioners (PNP), engaging students with diabetes, school nurses, teachers, and other school personnel. (2) Blood glucose management at home and school, diabetes knowledge and coping skills, healthy eating, carbohydrate counting, insulin dose adjustment, and hypoglycemia and hyperglycemia management |
| 2 | Bachman et al[24], 2008 | One-shot case | School nurses: 12 | Schools in Missouri | Evaluate an online continuing education program providing school nurses with updated practice principles and knowledge | Education on blood glucose management, diabetes knowledge, meal plan development, oral medications, hypoglycemia and hyperglycemia, insulin adjustment, insulin injection vs pump therapy, individual responsibilities of insulin pump management, diabetes management plan development, implementation of individual health plan, and emergency action plan, laws and regulations related to child diabetes care |
| 3 | Smith et al[23], 2012 | Single group pre-post | School nurses: 44; Health aids: 37 | Elementary, middle, and high schools, and one vocational school in New Albany-Floyd County, Indiana | Evaluate an education program for school health personnel to improve diabetes care-related knowledge and confidence | (1) The basic program was a 60-min educational session with the following components: diabetes knowledge, diabetes pathology, hypoglycemia and hyperglycemia, dietary management, exercise, blood glucose management. (2) The expanded program was a 180-min educational session that included carbohydrate counting, insulin administering, blood glucose meter, and written diabetes care plans |
| 4 | Gutierrez et al[22], 2019 | Single group pre-post | School personnel: 132 | Schools in rural districts of South Central Texas | Evaluate an online educational program for medical and nonmedical school personnel to improve diabetes-care related knowledge and confidence | Education on blood glucose monitoring, hypoglycemia and hyperglycemia, insulin and insulin regimens, insulin delivery services, dietary management, exercise management, and emergency management |
The fifth and sixth columns of Table 1 summarize intervention aims and settings (i.e. school characteristics). Regarding school characteristics, one intervention was conducted in urban school districts[21], one in rural schools[22], and the other two did not disclose urbanicity[23,24]. Regarding intervention aims, two studies described and evaluated online diabetes education programs for school personnel[22,24] and the other two assessed in-person interventions with or without practical engagement with daily diabetes care for students[21,23].
The last column of Table 1 summarizes the intervention components focused on different aspects of diabetes care at school. All four studies included diabetes pathology and basic knowledge, blood glucose monitoring and management; administering insulin, dose adjustment, transportation, and storage; and hypoglycemia and hyperglycemia management. Three studies mentioned dietary management and planning (n = 3)[21,23,24]. Two mentioned management of exercise and physical activity (n = 2)[22,23], carbohydrate counting (n = 2)[23,24], and development and implementation of individual health plan and emergency action plan (n = 2)[23,24]. Oral and over-the-counter medications[24], responsibilities of insulin pump management[24], diabetes care-related laws, regulations, and principles[24], and diabetes self-management and coping skills[22] were each mentioned in only one study.
Three studied applied the social cognitive theory (SCT). Evolved from Albert Bandura’s social learning theory in the 1960s, the SCT posits that behavior initiation and maintenance occurs in a social context with dynamic relationships between individuals and the environment[25]. The SCT consists of six essential constructs, which are reciprocal determinism, behavioral capability, observational learning, reinforcements, expectations, and self efficacy. Reciprocal determinism refers to the interactions of the individual, who possesses a set of learned experiences, along with the external social context, and an individual’s behavior in response to stimuli to achieve goals. Behavioral capability is the ability to perform a behavior based on necessary knowledge and skills. Observational learning is the ability to reproduce a behavior after observing how others do it. Reinforcement refers to the internal or external responses to individual behaviors, which influence the likelihood of maintaining or discontinuing that behavior. Primarily derived from previous experiences, expectations are the anticipated consequences of an individual’s behavior. Self-efficacy refers to the level of confidence in one’s ability to perform a behavior successfully. Self-efficacy is influenced by multiple factors including abilities and other personal characteristics and environmental level variables such as social barriers and facilitators. As a central concept of SCT, self-efficacy is one of the most widely applied constructs in health-related behavior research and interventions[26,27]. In the three interventions that applied SCT, self-efficacy guided their program development and measurement[21-23].
One study included in this review utilized the diffusion of innovations theory (DOI) described by Everett Rogers[24] to guide their evaluation on the effectiveness of an online diabetes management education program for school nurses in rural areas. DOI seeks to explain how, why, and at what rate new ideas and technologies are adopted[28]. Key elements in DOI include the innovation itself (e.g., a new idea or technology), communication channels; and time lag, as innovations are rarely adopted spontaneously; and the social system, which includes environmental factors and agents). DOI posits that innovations must be widely adopted to be self sustaining. Given an adoption rate, there exists a point at which an innovation reaches critical mass that is needed for a self-sustainable status. The process of diffusion can be complicated. Its rate and ultimate success are often highly contingent upon the type of adopters and the diffusion strategies used. There are five core determinants of innovation adoption: relative advantage, the extent to which an innovation is perceived as better than the idea or technology it replaces; compatibility, the extent to which an innovation is consistent with the experiences, values, and needs of possible adopters; complexity, the level of difficulty to understand and use the innovation; trialability, the extent to which an innovation can be experimented with before adoption; and observability, the extent to which an innovation offers tangible outcomes.
Table 2 summarizes the role of theory in each study, the operationalization and measurement for constructs, and main study findings. Table 3 concisely synthesizes the theoretical constructs and study counts. Three studies adopted SCT and its core construct, which is self-efficacy[29]. Regarding the measurement for self-efficacy, two studies adopted self-reported survey questions about the level of confidence in different aspects of school diabetes care. The questions used 7- to 9-point Likert scales that ranged from being “not at all confident” to “extremely confident” in performing a specific diabetes care task. One study measured self-efficacy using the Self Efficacy for Diabetes (SED) tool developed by Grossman et al[30]. Knowledge and experience, as a subconstruct of behavioral capability, were measured by a set of survey questions. The proportion of participants who answered those questions correctly and the mean score of knowledge tests were used to assess the intervention’s effectiveness.
| Study ID | Theories | The role of theories | Operationalization and measurement | Main findings |
| 1 | Social cognitive theory | (1) Intervention design: Improving student self-efficacy in self-diabetes management through interactive activities and model learning. (2) Effectiveness evaluation: Behavioral and perceptual measures of students’ self-efficacy and coping skills | (1) Self-efficacy was measured by the Self-Efficacy for Diabetes (SED) (Grossman et al, 1987). (2) Diabetes-related experiences with schools and parental satisfaction were measured by surveying parent perceptions. (3) Diabetes knowledge and competence in student self-management of diabetes were measured by surveying care-provider perceptions. (4) Behavioral outcomes were assessed by clinical diabetes indicators such as HbA1c level. | (1) No statistically significant differences were found between pre-and post-intervention mean scores of the SED. (2) No statistically significant differences were found between pre- and post-intervention in terms of self-care practices, parent satisfaction with school care, HbA1c, family knowledge and competence in diabetes management, and frequency of hospitalization. (3) The frequency of blood glucose monitoring at home increased. (4) The frequency of insulin administrations at school doubled. (5) Diabetes care visits in school were feasible and not disruptive to the student educational program. (6) School personnel felt less fearful about acute situations (hypoglycemia or hyperglycemia) and were more aware of students’ blood glucose trends, and were more comfortable reporting these trends to make changes in insulin dose |
| 2 | Theory of the diffusion of innovations | Evaluation of intervention effectiveness | Measurement metric included: (1) Whether school nurses found the online education program equal to or better than the education methods they currently used. (2) Whether the online education program met the needs of school nurses. (3) Whether the online education program helped school nurses learn diabetes management quickly and easily. (4) Whether the online education program was available for school nurses who were unable to attend the face-to-face workshop. (5) Whether school nurses perceived improvement in the ability to implement diabetes management for students | (1) School nurses learned more about the effects of oral-medications and over-the-counter medications on blood glucose control. (2) School nurses learned more about the process of developing a meal plan. (3) Most (91%) participants rated the online education program as useful. (4) The theory premise that innovations should be equal to or better than the current practice was inconclusive since some of the school nurses appreciated the convenience of the online program, whereas others felt it did not help them learn |
| 3 | Social cognitive theory | Evaluation of intervention effectiveness | (1) Diabetes care knowledge was measured by a set of multiple-choice survey questions such as “How many grams of carbohydrates are equal to 1 serving of carbohydrate?” (2) Self-efficacy was measured by Likert-scale questions (1 = “Strongly Disagree”; 7 = “Strongly Agree”) asking how confident the school nurses were in their abilities to perform different diabetes care tasks | (1) Correct answers to all but one knowledge-related question improved from the pre to post-test assessment. (2) School personnel who had family members with diabetes had greater pretest confidence in their understanding of diabetes (P = 0.043), the ability to measure blood glucose (P = 0.001), and knowledge of the effects of diabetes on children (P = 0.046). (3) A significant difference in overall knowledge was found between the pre- and post-test assessment (P < 0.001). Correct answers to six questions on the knowledge test showed significant improvement (P < 0.05). (4) Stuff members who had prior diabetes education had greater pretest knowledge of diabetes (P = 0.012). (5) Stuff members who had prior diabetes education were more likely to correctly answer the question about the desired range of blood glucose (P = 0.008) and the question about the effect of high blood glucose on thinking (P = 0.023). (6) Stuff members who had prior diabetes education were more likely to correctly answer the question “After treating hypoglycemia correctly, how long should you wait before re-checking the blood glucose?” on the post-test (P = 0.037). (7) All confidence items in caring for students with diabetes improved significantly between the pre- and post-test assessment (P < 0.001). (8) Confidence for all items on the pretest and post-test were significantly higher for those with prior diabetes education (P < 0.01) |
| 4 | Social cognitive theory | (1) Diabetes care knowledge was measured by 30 questions assessing different aspects of diabetes care. (2) Self-efficacy was measured by Likert scale questions (1 = “Not at all confident”; 7 = “Extremely confident”) assessing abilities to perform different diabetes care tasks | (1) There was a significant difference in the average pretest (M = 49.75, SD = 16.25) and post-test (M = 90.04, SD = 6.66) knowledge scores for nonmedical personnel [t(80) = -23.12, P = 0.000]. (2) There was a significant difference in the average pertest (M = 69.58, SD = 14.90) and post-test (M = 94.25, SD = 5.89) knowledge scores for school nurses [t(50) = -13.92, P = 0.000]. (3) There was a significant difference in the average pretest (M = 3.46, SD = 1.87) and post-test (M = 6.30, SD = 1.17) confidence scores for nonmedical personnel [t(80) = -15.45, P = 0.000]. (4) There was a significant difference in the average pretest (M = 5.80, SD = 1.34) and post-test (M = 5.80, SD = 1.34) confidence scores for school nurses [t(50) = -6.50, P = 0.000]. (5) There was a significant difference in the scores of confidence change between nonmedical personnel (M = 2.84, SD = 1.65) and school nurses [(M = 1.14, SD = 1.25), t(130) = 6.30, P = 0.000]. (6) There was no significant correlation between the participants’ rating of the usefulness of the program and the change in knowledge (r = −0.092) or confidence (r = 0.017). (7) There was a significant positive relationship between the change in knowledge scores and change in confidence scores [r = 0.442, P (one-tailed) < 0.01] |
| Theory | Main constructs | Applications to school diabetes care interventions (n = number of studies) |
| Social cognitive theory | Self-efficacy | Students’ self-efficacy in self diabetes management at school (n = 1); School nurses’ self-efficacy in diabetes management (n = 3); Nonmedical school personnel’s self-efficacy in diabetes management (n = 2) |
| Behavioral capability (knowledge and experience) | Students’ knowledge in self-diabetes management at school (n = 1); School nurses’ knowledge in diabetes management (n = 3); Nonmedical school personnel’s knowledge in diabetes management (n = 2) | |
| Observational learning | Intervention component in improving students’ self-diabetes management skills and confidence (n = 1) | |
| Reinforcements (social support) | Support for students with diabetes regarding self-diabetes management at school (n = 1) | |
| Theory of the diffusion of innovations | Relative advantage; Compatibility; Complexity; Trialability; Observability | To evaluate the successfulness of an online education program for school nurses in the rural area to improve diabetes management skills (n = 1) |
Mixed results were reported for the improvement in self efficacy and knowledge following the interventions. One intervention reported null findings of the SED scores[21], and two interventions reported statistically significant improvements in self efficacy and knowledge testing scores[22,23]. The baseline knowledge and self-efficacy levels of the study participant varied by previous diabetes education, experience in taking care of patients, and between medical and nonmedical personnel[22,23]. Also, the improvement in knowledge and self-efficacy were correlated[22]. One study found improvement in some behavioral outcomes of diabetes care (e.g., the frequency of blood glucose monitoring and hospitalization during a semester) and diabetes biomarkers (e.g., student HbA1c levels)[21], but relevant statistical testing was not reported.
Only one study used the DOI[24]. The study assessed a newly designed online program regarding the five core determinants of innovation adoption. A post-intervention survey was launched to ask school nurses whether the online program had a relative advantage over the conventional program, whether the online program met participant needs (compatibility), whether school nurses learned diabetes management information quickly and easily (complexity), whether the online program was available for school nurses (trialability), and whether the program improved school nurses’ ability to perform diabetes care (observability). The study reported that the assessment found that the online program was innovative, but relevant statistical testing was missing.
Table 4 reports findings from the assessment of the role of theory in guiding the interventions. All four studies evaluated theory-relevant constructs. Three studies identified the theoretical constructs as predictors of behavioral change. Two studies used theory to select or develop intervention techniques. Two studies used theory to customize intervention techniques. Two studies discussed their findings in the context of theory. No study used theory to select potential intervention participants.
| Criterion/study ID | 1 | 2 | 3 | 4 |
| (1) Theory was used to predict study participants’ behavior | Yes | No | Yes | Yes |
| (2) Theory was used to select participants for the intervention | No | No | No | No |
| (3) Theory was used to select or develop the intervention and relevant measures | Yes | Yes | Yes | No |
| (4) Theory was used to tailor/customize the intervention to study participants | Yes | Yes | No | No |
| (5) Theory-relevant constructs were evaluated in the study | Yes | Yes | Yes | Yes |
| (6) Results were discussed in the context of the theory | Yes | Yes | No | No |
To our knowledge, this was the first systematic review of theory-based diabetes care interventions in schools in the United States. A salient finding was the limited application of theories in the development and evaluation of school-based diabetes care interventions, as evidenced by only four studies eligible for this review. The scarcity of studies meeting our eligibility criteria was unsurprising given the lack of school-based diabetes care interventions. In a recent systematic review, Smith et al[31] found significant knowledge gaps in school-based diabetes management interventions, Pansier and Schulz[15], and Edwards et al[16] systematically reviewed school diabetes care interventions worldwide and identified only 11 and 15 unduplicated interventions, respectively. This review found ten interventions conducted in the United States, six of which did not explicitly apply a theory[32-36]. This finding suggests that the use of theories has been limited in developing and evaluating school-based diabetes care interventions. A lack of transparency in reporting may also exist.
The four theory-based interventions included in this review focused on improving diabetes-related knowledge, blood glucose management, insulin administering, and hypoglycemia and hyperglycemia management. Dietary management and carbohydrate counting, exercise management, and individual health plan and emergency plan development were only briefly considered. Less discussed aspects included over-the-counter medications, school personnel responsibilities in diabetes care, diabetes care-related laws and policies, and student self-management skills. Although the importance of collective efforts across multiple stakeholders (e.g., students with diabetes, parents, school nurses, teachers, nonmedical personnel, and community partners) was acknowledged[31], few comprehensive, science-based team interventions have been designed and implemented in school settings.
A close examination of how theories and associated constructs were used reveals application weaknesses and potential misuses. For example, self-efficacy was among the most frequently measured constructs in theory-based diabetes care interventions at school. Self-efficacy, as conceptualized by SCT, is an important determinant of health behavior. However, the studies included in this review focused on perceptions and individual beliefs and rarely examined health behavior outcomes. The theoretical link between self-efficacy and desirable behavioral outcomes, therefore, was underutilized in the intervention components. Relatedly, the relationships between outcome expectation, goal setting, and self-efficacy as delineated in SCT were not utilized. Other important SCT constructs such as mastery experience, verbal persuasion, and collective efficacy were also overlooked. In addition, other important theories related to behavioral change, for example, the transtheoretical model and the theory of planned behavior, were not utilized.
A feedback loop between theory and intervention was not observed in the studies included in the review. How well did theory predict behavior change and intervention outcomes? Which theoretical constructs were more relevant or informative to intervention designs and measurement development? What aspects of the theory were supported by or contradictory to intervention findings? Such critical assessment could be highly beneficial to future applications of theory in school-based diabetes care interventions but is currently missing.
This review has several limitations. First, only studies that explicitly described the use of theories were included. It is possible that some interventions excluded from this review were inspired by theories but did not report the details. Moreover, the article search was limited to literature published in English. Gray literature like unpublished reports and reports in languages other than English were overlooked. Additionally, study settings were limited to K-12 schools in the United States. That decision was made because school-based diabetes care practices could be highly heterogeneous across countries. The included studies differed substantially in outcome measures, which prevented us from pooling the same or similar quantitative outcome estimates together in a meta-analysis. Finally, the review was intended as a critical synthesis and appraisal of how theories were used in the development and evaluation of school-based diabetes care interventions. We did not conduct a quantitative synthesis of intervention effectiveness due to the small number of studies included.
This critical review suggests that theory-based diabetes care interventions in the United States schools are lacking. In the rare cases where theories were applied, insufficient application and underutilization of theoretical constructs were common. Future investigations should consider applying theories to design intervention components and link essential theory-relevant constructs to intervention techniques, as theory-based interventions provide better opportunities to identify mediators of behavior change and effective intervention ingredients. Another line of future research is to use theories to guide the identification of the differential impacts of interventions across population subgroups such as age group, sex, and race; context such as rural vs urban, private vs public schools), and target population including students, school nurses, and teachers. As the evidence of effectiveness for school-based diabetes care interventions strengthens, an important future direction is to apply theories to develop and evaluate implementation strategies that can facilitate the adoption and sustainment of effective interventions in schools.
Diabetes is one of the most prevalent child chronic conditions. School age children with diabetes need reliable, multifaceted diabetes care at school. School-based diabetes care interventions targeting school preparedness for diabetes care, involving multiple stakeholders, are warranted to improve school diabetes care quality. Applying theories makes the intervention effectiveness more promising. However, no studies systematically assessed how relevant theories were applied in existing interventions.
School-based diabetes care interventions benefit from applying relevant theories appropriately. The specific role of theories in existing interventions among United States K-12 schools needs to be assessed. Such studies might inform future interventions regarding applying theories in intervention design, technique selection, implementation, and evaluation and improve intervention effectiveness.
This study systematically identified and synthesized the literature concerning theory-based diabetes care interventions in K-12 schools in the United States. It critically assessed the specific role of theories and constructs in intervention design, implementation, outcome measurement, and evaluation. The review findings highlight the gaps and limitations in applying theory in diabetes care in schools and inform future investigations.
This review followed a systematic review protocol for literature search, selection, and data extraction. The application of theories in the interventions that met the selection criteria was critically discussed.
Only four studies met the criteria of theory-based intervention. Three of the studies applied social cognitive theory in the implementation and evaluation process. One study applied the diffusion of innovations theory in implementation design and evaluation. Further assessment reveals the lack of use and potential misuses of theories.
Existing theory-based diabetes care interventions in United States schools are few in number and lack the appropriate use of theories.
Future interventions would benefit from appropriately defining, operationalizing, and measuring relevant theoretical constructs, especially the use of constructs as the core modifying factors that may contribute to intervention effectiveness.
Manuscript source: Invited manuscript
Specialty type: Scientific Journal
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhou B S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Xing YX
| 1. | Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and Costs of Five Chronic Conditions in Children. J Sch Nurs. 2016;32:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 2. | Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020: Estimates of Diabetes and Its Burden in the United States. [cited 3 October 2020] Available from: https://www.cdc.gov/diabetes/data/statistics/national-diabetes-statistics. |
| 3. | Cizza G, Brown RJ, Rother KI. Rising incidence and challenges of childhood diabetes. A mini review. J Endocrinol Invest. 2012;35:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 4. | Jackson CC, Albanese-O'Neill A, Butler KL, Chiang JL, Deeb LC, Hathaway K, Kraus E, Weissberg-Benchell J, Yatvin AL, Siminerio LM. Diabetes care in the school setting: a position statement of the American Diabetes Association. Diabetes Care. 2015;38:1958-1963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 5. | Rapp Attorney JA, Quincy M, Dimmick BL, Gordon K, Jackson C. Legal Rights of Students with Diabetes Prepared By Shereen Arent Executive Vice President, Government Affairs and Advocacy American Diabetes Association 2005. [cited 3 October 2020] Available from: http://main.diabetes.org/dorg/PDFs/Advocacy/Discrimination/education-materials/Legal-rights-of-students-with-diabetes/Legal-rights-of-students-with-diabetes.pdf. |
| 6. | Wood JM. Protecting the rights of school children with diabetes. J Diabetes Sci Technol. 2013;7:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Siminerio LM, Albanese-O'Neill A, Chiang JL, Hathaway K, Jackson CC, Weissberg-Benchell J, Wright JL, Yatvin AL, Deeb LC; American Diabetes Association. Care of young children with diabetes in the child care setting: a position statement of the American Diabetes Association. Diabetes Care. 2014;37:2834-2842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 8. | Goddard CW. Children with Diabetes: Are State Statutes Needed to Protect Students’ Rights. J Law Educ. 2005;34. |
| 9. |
Lange K, Jackson C, Deeb L. Diabetes care in schools--the disturbing facts.
Pediatr Diabetes. 2009;10 Suppl |
| 10. | Nabors L, Troillett A, Nash T, Masiulis B. School nurse perceptions of barriers and supports for children with diabetes. J Sch Health. 2005;75:119-124. [PubMed] |
| 11. | Nichols PJ, Norris SL. A systematic literature review of the effectiveness of diabetes education of school personnel. Diabetes Educ. 2002;28:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Vennum MK. Students with Diabetes: Is There Legal Protection. J Law Educ. 1995;24. |
| 13. | Nabors L, Lehmkuhl H, Christos N, Andreone TL. Children with diabetes: perceptions of supports for self-management at school. J Sch Health. 2003;73:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Amillategui B, Mora E, Calle JR, Giralt P. Special needs of children with type 1 diabetes at primary school: perceptions from parents, children, and teachers. Pediatr Diabetes. 2009;10:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Pansier B, Schulz PJ. School-based diabetes interventions and their outcomes: a systematic literature review. J Public Health Res. 2015;4:467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Edwards D, Noyes J, Lowes L, Haf Spencer L, Gregory JW. An ongoing struggle: a mixed-method systematic review of interventions, barriers and facilitators to achieving optimal self-care by children and young people with type 1 diabetes in educational settings. BMC Pediatr. 2014;14:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Hynynen ST, van Stralen MM, Sniehotta FF, Araújo-Soares V, Hardeman W, Chinapaw MJ, Vasankari T, Hankonen N. A systematic review of school-based interventions targeting physical activity and sedentary behaviour among older adolescents. Int Rev Sport Exerc Psychol. 2016;9:22-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 114] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 18. | Michie S, Prestwich A. Are interventions theory-based? Health Psychol. 2010;29:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 492] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 19. | Rothman AJ. "Is there nothing more practical than a good theory? Int J Behav Nutr Phys Act. 2004;1:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 182] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 20. | Michie S, Carey RN, Johnston M, Rothman AJ, de Bruin M, Kelly MP, Connell LE. From Theory-Inspired to Theory-Based Interventions: A Protocol for Developing and Testing a Methodology for Linking Behaviour Change Techniques to Theoretical Mechanisms of Action. Ann Behav Med. 2018;52:501-512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 249] [Cited by in RCA: 235] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 21. | Faro B, Ingersoll G, Fiore H, Ippolito KS. Improving students' diabetes management through school-based diabetes care. J Pediatr Health Care. 2005;19:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Gutierrez C. Improving the care of students with diabetes in rural schools utilizing an online diabetes education program for school personnel. Rural Remote Health. 2020;20:5596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Smith CT, Chen AM, Plake KS, Nash CL. Evaluation of the impact of a diabetes education curriculum for school personnel on disease knowledge and confidence in caring for students. J Sch Health. 2012;82:449-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Bachman JA, Hsueh KH. Evaluation of online education about diabetes management in the school setting. J Sch Nurs. 2008;24:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. 1st ed. NJ: Prenctice Hall, 1985: 130-152. |
| 26. | Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1120] [Cited by in RCA: 1214] [Article Influence: 80.9] [Reference Citation Analysis (0)] |
| 27. | Fisher KL. School nurses' perceptions of self-efficacy in providing diabetes care. J Sch Nurs. 2006;22:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Rogers EM. Diffusion of Innovations: Modifications of a Model for Telecommunications. Die Diffusion von Innovationen in Der Telekommunikation. Springer Berlin Heidelberg. 25-38. [DOI] [Full Text] |
| 29. | Haider M, Kreps GL. Forty years of diffusion of innovations: utility and value in public health. J Health Commun. 2004;9 Suppl 1:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Grossman HY, Brink S, Hauser ST. Self efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care. 1987;10:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 174] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 31. | Smith LB, Terry A, Bollepalli S, Rechenberg K. School-Based Management of Pediatric Type 1 Diabetes: Recommendations, Advances, and Gaps in Knowledge. Curr Diab Rep. 2019;19:37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 32. | Bobo N, Wyckoff L, Patrick K, White C, Glass S, Carlson JP, Perreault C. A collaborative approach to diabetes management: the choice made for Colorado schools. J Sch Nurs. 2011;27:269-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Breneman CB, Heidari K, Butler S, Porter RR, Wang X. Evaluation of the Effectiveness of the H.A.N.D.S.SM Program: A School Nurse Diabetes Management Education Program. J Sch Nurs. 2015;31:402-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Berget C, Nii P, Wyckoff L, Patrick K, Brooks-Russell A, Messer LH. Equipping School Health Personnel for Diabetes Care with a Competency Framework and Pilot Education Program. J Sch Health. 2019;89:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Perfect MM, Jaramillo E. Relations between resiliency, diabetes-related quality of life, and disease markers to school-related outcomes in adolescents with diabetes. Sch Psychol Q. 2012;27:29-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Nguyen LH, Tran BX, Thi Nguyen HL, Le HT, Do HT, Kim Dang A, Nguyen CT, Latkin CA, Zhang MWB, Ho RCM. Socio-Economic Disparities in Attitude and Preference for Menu Labels among Vietnamese Restaurant Customers. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47199] [Article Influence: 2949.9] [Reference Citation Analysis (0)] |