Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4607
Peer-review started: January 19, 2021
First decision: March 25, 2021
Revised: April 5, 2021
Accepted: April 20, 2021
Article in press: April 20, 2021
Published online: June 26, 2021
Processing time: 143 Days and 1.9 Hours
Thoracic intervertebral foramen puncture is the key step for interventional therapy on the thoracic nerve roots or dorsal root ganglia. The anatomical features of the thoracic spine are complex, and puncture injury to the pleura, blood vessels, spinal cord, and other tissues may cause serious complications. The spatial anatomical characteristics and related parameters for thoracic intervertebral foramen puncture remain poorly understood.
To observe and summarize the spatially applied anatomical characteristics for intervertebral foramen puncture on different vertebral segments.
A total of 88 patients (41 males and 47 females) who underwent thoracic minimally invasive interventional treatment at Nanjing Drum Tower Hospital from January 2019 to June 2020 were included. Computed tomography images of 167 thoracic vertebral segments scanned in the prone position were collected. The width of the intertransverse space (DP), the height of the rib neck/head above the lower transverse process (DR), the width of the lateral border of the articular process/lamina (WP), and the width of the posterior border of the vertebral body (WV) were measured. At the upper 1/3 of the intervertebral foramina, the horizontal inclination angle (α) from the lateral border of the articular process/lamina to the posterolateral border of the vertebral body was measured. The ratios DR/DP and WP/WV were calculated. The intervertebral foramen parameters were compared between segments.
No rib head/neck occlusion (DR/DP > 0) was found in the intertransverse spaces of T1-2 and T12-L1. The incidence of occlusion for the upper thoracic segments (T1-5, n = 138), middle thoracic segments (T5-9, n = 116), and lower thoracic segments (T9-L1, n = 80) were 76.81%, 100%, and 82.50%, respectively. The incidence of occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments (P < 0.05). The incidence of > 1/2 occlusion (DR/DP > 1/2) for the upper, middle, and lower thoracic segments was 7.97%, 74.14%, and 32.50%, respectively. The incidence of > 1/2 occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments (P < 0.05). WP was longer than WV on T1-2 to T9-10 and shorter than WV on T10-11 to T12-L1. The horizontal puncture angle (α) into the external opening of the intervertebral foramina was positively correlated with the segments of the thoracic vertebrae from the cephalic to caudal portion (left: r = 0.772, P < 0.01; right: r = 0.771, P < 0.01), and the horizontal inclination angle for T11-12 and T12-L1 was 90°.
It is necessary to identify the spatial impact of the rib head/neck on the puncture path of the intervertebral foramina and design appropriate puncture angles for different segments.
Core Tip: We measured and summarized the features of applied anatomy for thoracic intervertebral foramina cannulation. Based on our results, we found that the rib head/neck in the middle thoracic segments greatly influences the puncture path for the intervertebral foramen. It is necessary to identify the space between the transverse process and rib head/neck for puncture. The inclination angle for puncture varies in different segments. The closer the segment is to the lower thoracic vertebrae, the larger the horizontal inclination angle of puncture is. This study also provides an anatomic reference for performing clinical intervertebral foramen puncture with ultrasound guidance.
- Citation: Wang R, Sun WW, Han Y, Fan XX, Pan XQ, Wang SC, Lu LJ. Observation and measurement of applied anatomical features for thoracic intervertebral foramen puncture on computed tomography images. World J Clin Cases 2021; 9(18): 4607-4616
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4607.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4607
Interventional therapy on the thoracic nerve roots or dorsal root ganglia (DRGs) is an important means to relieve chronic pain of the chest and abdomen, such as postherpetic neuralgia, incision pain, or other thoracic nerve pain[1-3]. The thoracic intervertebral foramina (TIVFs) are the most direct and frequently used channels for reaching the DRGs with interventional tools[4,5]. Therefore, accurate TIVF puncture is the key step for interventional treatment, which can determine the success or failure of total therapy. The anatomical features of the thoracic spine are complex. The presence of the transverse processes, ribs, and pleural and lung tissue increases the difficulty and risk of TIVF puncture[6,7]. Interventional procedures involving passage through the TIVFs have been performed for many years, and X-ray, computed tomography (CT), and ultrasound imaging have been used as common guidance solutions[5,7,8]. However, few studies on the anatomy of the TIVFs have been reported, and even fewer literature reviews on the applied anatomy for TIVF cannulation have been published.
The thoracic spine is located between the cervical and lumbar vertebrae and includes the skeletal features of these vertebrae. However, the spatial relationship of the thoracic spine and the surrounding tissue is more complex than that of the cervical and lumbar segments. The anterior, superior, and inferior boundaries of the TIVFs consist of the corresponding vertebrae and their intervertebral discs, the inferior part of the pedicle, and the superior part of the pedicle. The posterior boundaries of the TIVFs consist of the articular processes of the zygapophyseal joint. Outside of the TIVFs are the thoracic paravertebral spaces and pleura on the lateral sides and the transverse processes on the superior lateral and inferior lateral sides. Inside of the TIVFs is the spinal cord[6]. The puncture trajectory usually passes from lateral to medial along the outer edge of the articular process. Therefore, the accessible space for TIVF cannulation is restricted to the intertransverse process space (ITPS). Additionally, the spinal nerves regularly exit the intervertebral foramina from the upper part, increasing the precision requirement of target positioning[4,9,10]. The available space for puncture adjustment is further restricted due to the presence of lung tissue and ribs, which is another difference from the anatomy of the cervical and lumbar spines. Although the spatial features of the TIVFs and surrounding structures are important for cannulation, the corresponding applied anatomy has not been sufficiently summarized. The difference in features between the upper, middle, and lower thoracic segments has also been vaguely described.
In TIVF puncture, the rib head and rib neck are the leading obstructions to achieving the desired trajectory. In this article, we summarize and report on the spatial relationship between the ribs and intertransverse spaces as well as the puncture characteristics for TIVF cannulation. This study may provide an important reference for image-guided TIVF puncture, especially using ultrasound imaging.
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital Clinical College of Xuzhou Medical University (Ethical Number: 2020-347-01). A total of 88 patients who underwent thoracic minimally invasive treatment at Nanjing Drum Tower Hospital from January 2019 to June 2020 were admitted, including 41 males and 47 females, with an average age of 58.46 ± 10.12 years (range, 42-91 years). CT images of 167 segments of the thoracic intervertebral foramina were scanned and collected with the patients in the prone position during their operations. The inclusion criteria were as follows: (1) Minimally invasive surgery of the thoracic spinal nerve under CT guidance; (2) scanning of the TIVFs with slice thickness < 2 mm; and (3) scans obtained with patients in the prone position, cushioned with a pillow below the chest. Patients with the following criteria were excluded: (1) Spinal deformities, spinal bone lesions, or other diseases that affect normal thoracic anatomy; (2) a history of spinal surgery; (3) body mass index > 35 kg/m2; (4) severe skew in the scanning posture; and (5) severe osteoporosis. For the T1-2 to the T12-L1 TIVF segments, images were obtained from 6, 17, 23, 23, 14, 16, 12, 16, 16, 16, 10, 8, and 6 patients, respectively.
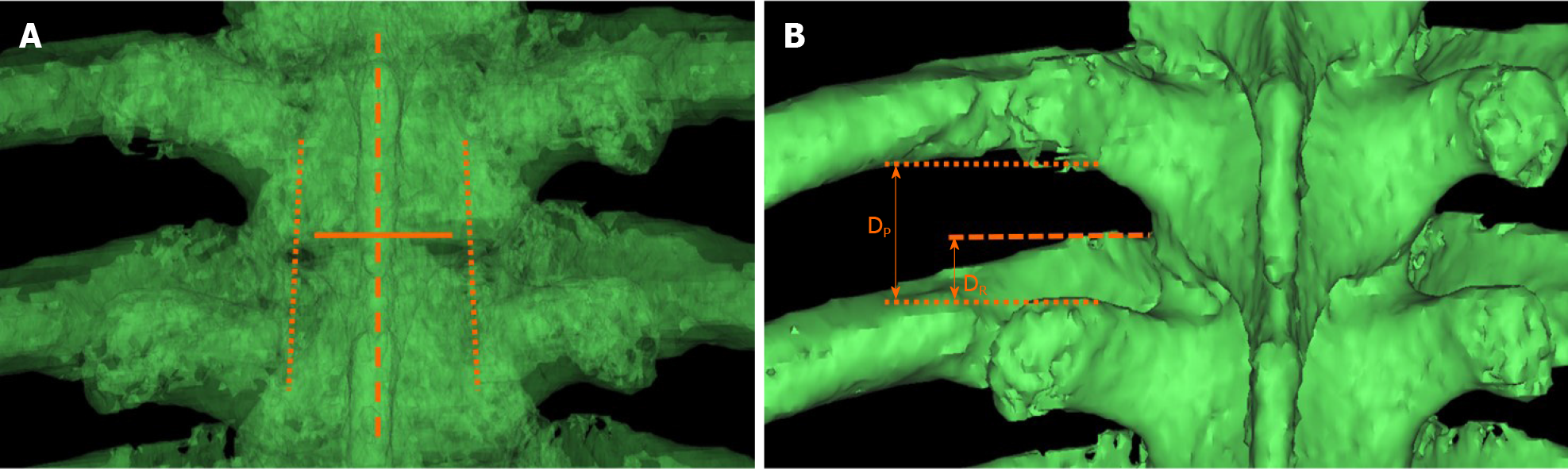
CT data of the thoracic vertebrae in DICOM format were imported into Mimics software (materialize 17.0, Belgium), and three-dimensional skeletal structure models of the thoracic vertebrae were reconstructed. To improve the consistency of the characteristic measurements for different TIVF segments, the viewing angle was adjusted to the anteroposterior position. That is, when observed with the software in fluoroscopy mode, the spinous process line coincides with the middle line of the bilateral pedicle, and the anterior edge of the inferior border of the superior thoracic vertebra coincides with the posterior edge. Before measurement of each TIVF, the observation angle of the measured segment image was readjusted again. Then, the spatial position parameters of the rib head/neck and the transverse process space on both sides were measured (Figure 1).
Under this observation angle, the following parameters were measured: (1) The width of the intertransverse process space (DP), that is, the vertical distance from the horizontal line of the inferior margin of the superior transverse process to the horizontal line of the superior margin of the inferior transverse process; and (2) the height of the rib neck/head protrusion (DR), that is, the vertical distance from the horizontal line of the highest point of the rib neck/head to the horizontal line of the superior margin of the inferior transverse process. The ratio DR/DP was used to assess the occlusion of the thoracic transverse process space by the rib head/neck. The value of DR/DP for each intervertebral foramen was calculated and trichotomized as DR/DP = 0, 0 < DR/DP ≤ 1/2, or DR/DP > 1/2. Then, the DR/DP values of the upper (T1-5), middle (T5-9), and lower (T9-L1) segments were compared.
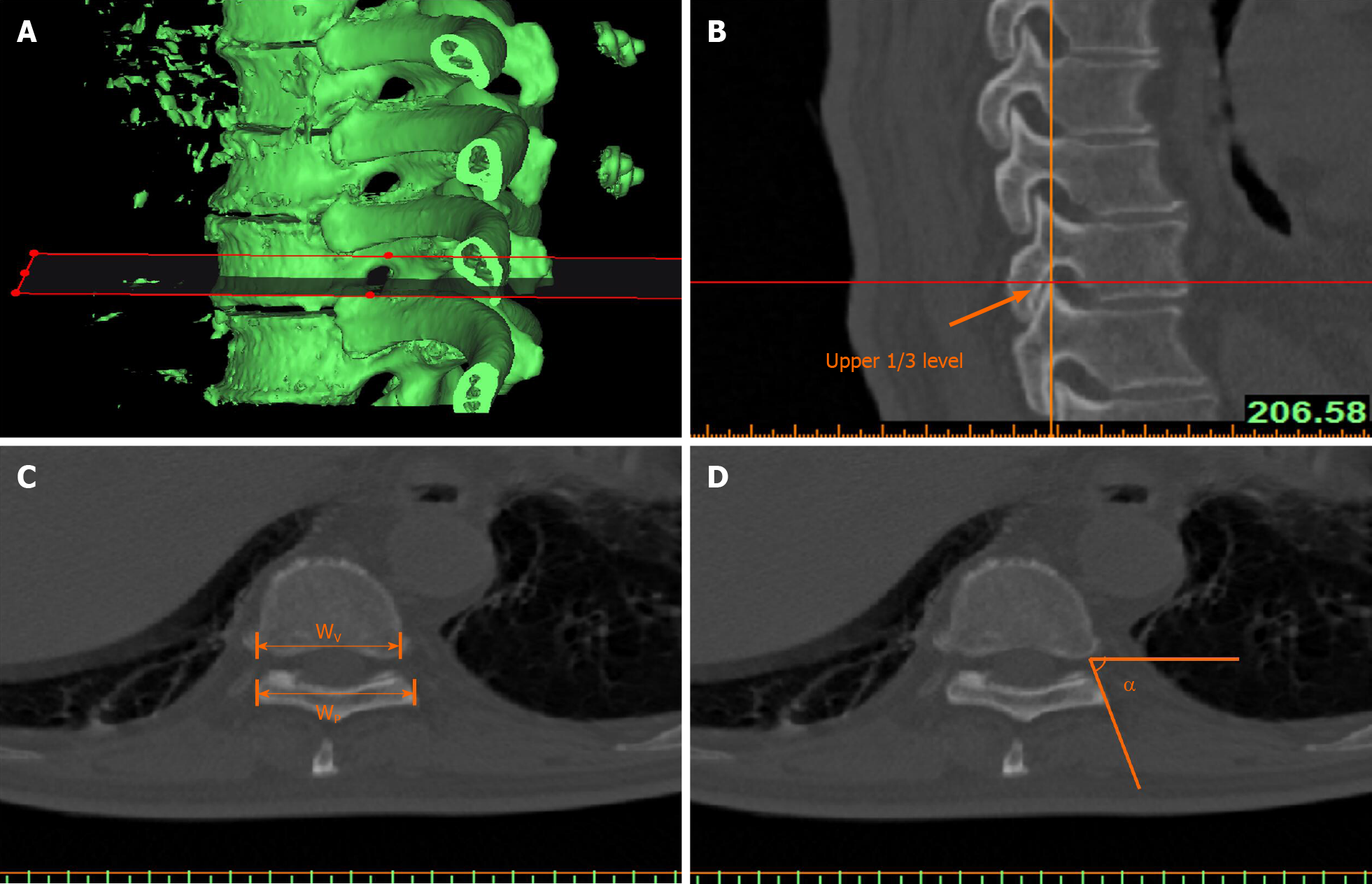
The three-dimensional model of the thoracic vertebrae was sectioned with the reslice function of the software. The tomographic plane was placed parallel to the inferior border of the superior vertebral body, and the parameters were measured on the newly obtained tomographic plane. After positioning the tomographic image at the upper 1/3 level of the intervertebral foramen, the following parameters were measured: (1) The width of the lateral border of the articular process/lamina (WP); (2) The width of the posterior border of the vertebral body (WV); and (3) The horizontal inclination angle (α) from the lateral border of the articular process/lamina to the posterolateral border of the vertebral body (Figure 2). The ratio Wp/Wv was calculated to evaluate the changes in the vertebral body parameters of different segments. The inclination angles were compared between two sides. The correlation between inclination angle and segment location was also counted.
Statistical analyses were carried out using SPSS Version 22.0 (IBM Corporation, Armonk, NY, United States). The Shapiro-Wilk test was used to assess the normality of the distribution of the quantitative parameters. Quantitative data conforming to a normal distribution are described as the mean ± SD, and comparisons were made by t-tests. Qualitative parameters are expressed as counts and percentages and were compared by the chi-square test. Pearson linear correlation analysis was used to describe the direction and degree of linear correlation between two quantitative variables. P < 0.05 was considered statistically significant.
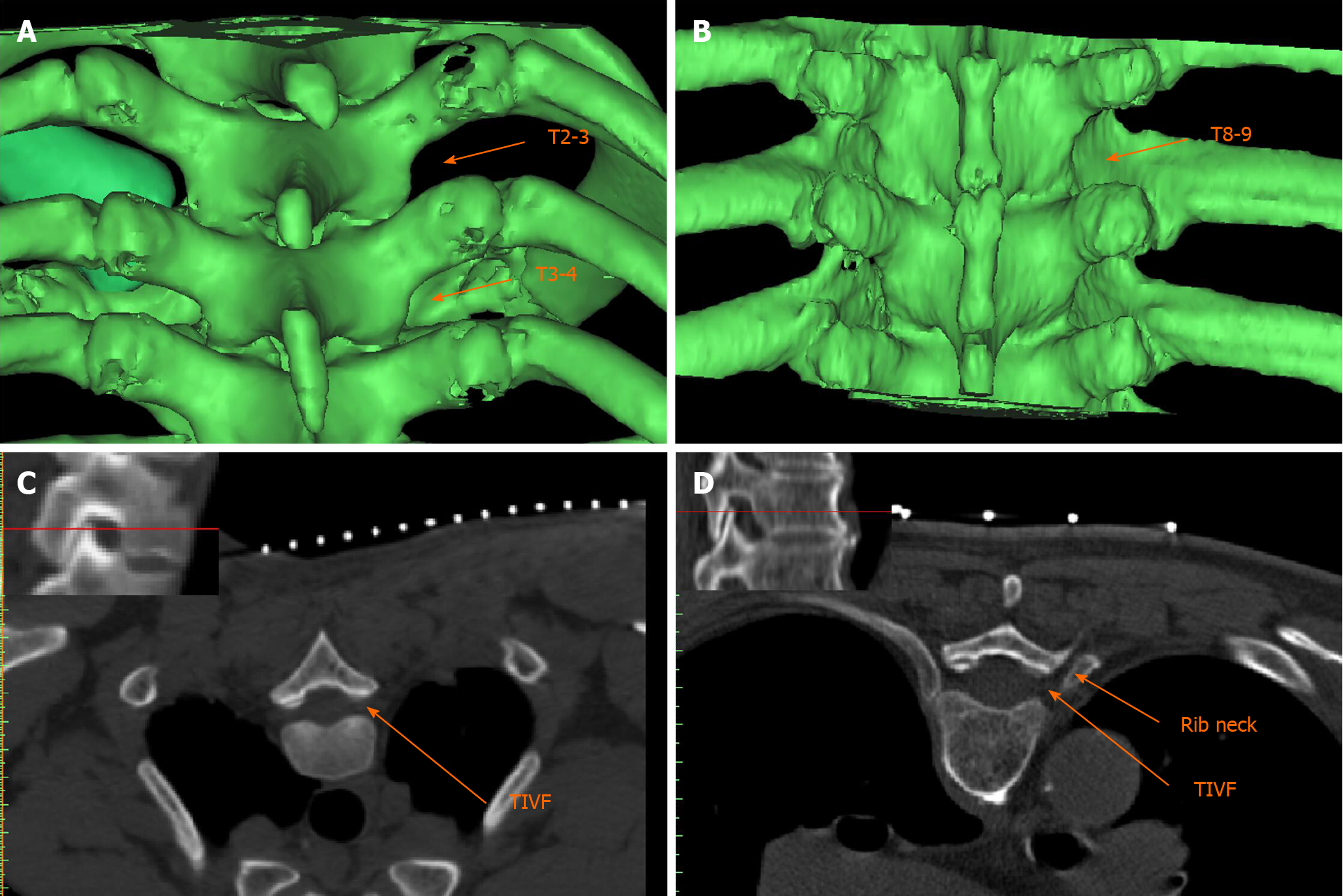
The height of the rib neck/head protruding into the ITPS differed in different thoracic vertebral segments, resulting in different degrees of occlusion (Figure 3). No rib head/neck occlusion (DR/DP > 0) onto the ITPS was found on segments T1-2 and T12-L1, and the remaining thoracic segments were all occluded by the rib. The details of ITPS obstruction by the rib head/neck from T1-2 to T12-L1 are shown in Table 1. The incidence of occlusion for the upper thoracic segments (T1-5, n = 138), middle thoracic segments (T5-9, n = 116), and lower thoracic segments (T9-L1, n = 80) was 76.81%, 100%, and 82.50%, respectively. The incidence of occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments (P < 0.05). The incidence of > 1/2 occlusion (DR/DP > 1/2) of the ITPS for the upper, middle, and lower thoracic segments was 7.97%, 74.14% and 32.50%, respectively. The incidence of > 1/2 ITPS occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments (P < 0.05) (Table 2).
| Segment | No occlusion | 0 < Occlusion ≤ 1/2 | Occlusion > 1/2 |
| T1-2 (n = 12) | 12 (100%) | 0 | 0 |
| T2-3 (n = 34) | 15 (44.12%) | 19 (55.88%) | 0 |
| T3-4 (n = 46) | 5 (10.87%) | 39 (84.78%) | 2 (4.35%) |
| T4-5 (n = 46) | 0 | 37 (80.43%) | 9 (19.57%) |
| T5-6 (n = 28) | 0 | 15 (53.57%) | 13 (46.43%) |
| T6-7 (n = 32) | 0 | 4 (12.50%) | 28 (87.50%) |
| T7-8 (n = 24) | 0 | 5 (20.83%) | 19 (79.17%) |
| T8-9 (n = 32) | 0 | 6 (18.75%) | 26 (81.25%) |
| T9-10 (n = 32) | 0 | 10 (31.25%) | 22 (68.75%) |
| T10-11 (n = 20) | 0 | 16 (80.00%) | 4 (20.00%) |
| T11-12 (n = 16) | 2 (12.50%) | 14 (87.50%) | 0 |
| T12-L1 (n = 12) | 12 (100%) | 0 | 0 |
At the upper 1/3 level of the intervertebral foramina, the width of the lateral border of the articular process/lamina (Wp) was longer than the width of the posterior border of the vertebral body (Wv) for segments T1-2 to T9-10. WP started to be shorter than WV from segment T10-11 to segment T12-L1 (Table 3). No significant difference in the horizontal puncture angle (α) was found between the left and right sides. The horizontal puncture angle (α) into the external opening of the intervertebral foramina was positively correlated with the thoracic vertebral segments from the cephalic to caudal portion (left: r = 0.772, P < 0.01; right: r = 0.771, P < 0.01). On the T11-12 and T12-L1 segments, the horizontal inclination angle was 90°, and a perpendicular puncture close to the lateral border of the lamina/articular process entered the external opening of the intervertebral foramina.
| Segment | Wp/Wv > 1 | Wp/Wv ≤ 1 | Puncture angle (left) | Puncture angle (right) | P value |
| T1-2 (n = 6) | 6 (100%) | 0 | 42.73 ± 2.73 | 48.95 ± 2.20 | 0.151 |
| T2-3 (n = 17) | 17 (100%) | 0 | 62.55 ± 8.51 | 61.76 ± 6.71 | 0.484 |
| T3-4 (n = 23) | 23 (100%) | 0 | 69.02 ± 5.76 | 69.68 ± 6.09 | 0.705 |
| T4-5 (n = 23) | 23 (100%) | 0 | 71.76 ± 4.89 | 71.93 ± 6.67 | 0.925 |
| T5-6 (n = 14) | 14 (100%) | 0 | 71.10 ± 6.13 | 70.88 ± 7.00 | 0.709 |
| T6-7 (n = 16) | 16 (100%) | 0 | 73.78 ± 3.39 | 73.68 ± 4.53 | 0.944 |
| T7-8 (n = 12) | 12 (100%) | 0 | 76.96 ± 4.96 | 75.91 ± 4.22 | 0.581 |
| T8-9 (n = 16) | 16 (100%) | 0 | 79.26 ± 5.25 | 79.74 ± 5.65 | 0.805 |
| T9-10 (n = 16) | 16 (100%) | 0 | 76.65 ± 4.98 | 77.12 ± 5.72 | 0.808 |
| T10-11 (n = 10) | 7 (70%) | 3 (30%) | 83.29 ± 6.92 | 82.98 ± 6.53 | 0.918 |
| T11-12 (n = 8) | 0 | 8 (100%) | 90 ± 0 | 90 ± 0 | - |
| T12-L1 (n = 6) | 0 | 6 (100%) | 90 ± 0 | 90 ± 0 | - |
Accurate TIVF puncture can reduce operation risks and complications of interventional treatment[11]. By measuring the relevant parameters of thoracic intervertebral foramen puncture on three-dimensional reconstructed CT images, the purpose of this study was to observe the spatial, applied anatomical characteristics of different thoracic intervertebral foramen segments. We also sought to provide an anatomical basis for clinical puncture operations, especially in the application of ultrasound-guided thoracic intervertebral foramen puncture.
The thoracic intervertebral foramina are important channels for the minimally invasive interventional treatment on the thoracic nerve roots and dorsal root ganglia in the field of pain management[4]. Accurate localization and puncture of the TIVFs are the basis for successful treatment[11]. Currently, thoracic intervertebral foramen puncture is usually performed under the guidance of C-arm or CT. X-rays can show the relationship between bony structures and the puncture needle. Three-dimensional reconstructed CT images can not only show the 3D spatial relationship between the structures adjacent to the TIVF but also provide a reference for operation planning and puncture path optimization[4,12,13]. However, C-arm and CT guidance also have some disadvantages, such as radiation exposure to the operators and patients, poor portability, and inability to guide in real time.
The thoracic intervertebral foramina are the bony channels where the thoracic nerve roots leave the spinal cord. The structure of the thoracic intervertebral foramina is significantly different from that of the cervical and lumbar segments, which is mainly manifested by rib head/neck occlusion. Our results showed that only the T1-2 and T12-L1 segments lacked rib occlusion in the ITPS. The ITPSs of the other segments were all occluded by the rib head/neck. The middle thoracic segments had the highest incidence of occlusion, and their incidence of > 1/2 occlusion was significantly higher than that of the upper thoracic and lower thoracic segments.
At the upper 1/3 level of the intervertebral foramina, the width of the lateral border of the articular process/lamina of the T1-10 segments was longer than the width of the posterior border of the vertebral body, which indicates that the puncture needle needs to pass through the lateral margin of the lamina at a certain angle to enter the intervertebral foramen. From the cephalic to caudal portion, the horizontal inclination angle required to enter the external opening of the intervertebral foramen gradually increases. Therefore, on the upper thoracic segments, especially the T1-2 segment, sufficient lateral distance is required to enter the intervertebral foramen. On the middle thoracic segments, the lateral distance is smaller than that on the upper thoracic segments. However, because the rib head/neck occupies the ITPS, it is necessary to design the trajectory along the tangent line of the rib head/neck and lamina so that the needle can smoothly pass through the gap and enter the intervertebral foramen. On the lower thoracic segments, the width of the lateral border of the lamina/facet joint becomes increasingly shorter than that of the posterior border of the vertebral body. Therefore, excessive lateral distance should be avoided due to the risk of puncture into the spinal canal, which can lead to spinal cord injury and other serious complications.
In recent years, ultrasound has been increasingly used in minimally invasive interventional treatment of the spine[14,15]. However, because ultrasound cannot penetrate bone, the location of spinal targets often relies on the surface anatomical characteristics of bony structures[6,16]. The 12 segments of the thoracic vertebrae are located between the cervical and lumbar vertebral segments. The upper and lower thoracic spines possess characteristics of the cervical and lumbar spines, respectively. However, the paravertebral structure of the thoracic vertebrae is more complex, and the application of ultrasound-guided TIVF puncture is highly risky[11]. This study summarized the spatial features of the skeletal structure and provides a reference for ultrasonic TIVF puncture.
In the process of ultrasound-guided TIVF puncture, the short axis section of the transverse process should be assessed first. Then, the probe should be moved to the caudal side until the transverse process disappears, where the ITPS section can be obtained. Generally, the main structure of the ITPS section includes the lamina/articular process, paravertebral space, and pleura[17,18]. In this section, the intervertebral foramen is the space formed by the superficial lamina/facet joint and the posterior margin of the deep vertebral body. Adopting the in-plane technique, the TIVF can be entered along the lateral border of the lamina/articular process. However, based on the results of this study, we found that not only the pleura is found outside the TIVF in the ITPS section but also a hyperechoic rib head/neck may occupy the external area of the TIVF and occlude the puncture path (Figure 3C and D), especially in the middle thoracic segments. After moving the probe caudally until the transverse process echo disappears, combined ultrasonic images of the vertebral plate/articular process, rib head/neck, and pleura appear. Since the space between the rib head/neck and lamina/articular process is not a joint structure, we propose that this gap should be a feasible puncture path into the intervertebral foramen in this plane.
In summary, the anatomical structure of the thoracic intervertebral foramen is unique. The rib head/neck in the middle thoracic segments greatly influences the puncture path for the intervertebral foramen; therefore, it is necessary to identify the space between the transverse process and rib head/neck for puncture. The inclination angle for puncture differs in different segments. The closer the segment is to the lower thoracic vertebrae, the larger the horizontal inclination angle of puncture is. This study also provides an anatomic reference for performing clinical intervertebral foramen puncture with ultrasound guidance.
When conducting interventional therapy on the thoracic nerve roots or dorsal root ganglia for treatment of chronic pain, thoracic intervertebral foramen (TIVF) is the most frequently used channel and TIVF puncture is the key step for the therapy. The anatomical features of the structure around TIVF are complex. Despite the assistance of many imaging guidance, clinical application of TIVF cannulation is still challenging. Improper operation may injure the pleura, blood vessels, spinal cord, and other tissues, causing serious complications.
The intertransverse process space (ITPS) for TIVF cannulation is severely restricted by the lung and ribs, but the spatial anatomical characteristics and related parameters for TIVF puncture remain poorly understood. The difference in features between the upper, middle, and lower thoracic segments has also been vaguely described.
To observe and summarize the spatially applied anatomical characteristics for TIVF puncture on different vertebral segments.
A total of 88 patients who underwent thoracic minimally invasive interventional treatment were included. Computed tomography images of 167 thoracic vertebral segments scanned in the prone position were collected. We measured the width of the ITPS (DP), the height of the rib neck/head above the lower transverse process (DR), the width of the lateral border of the articular process/lamina (WP), and the width of the posterior border of the vertebral body (WV). The horizontal inclination angle (α) for TIVF puncture at the upper 1/3 level of the intervertebral foramina was measured. The above measured parameters and calculated ratios (DR/DP and WP/WV) were compared between segments.
No rib head/neck occlusion (DR/DP > 0) was found in the ITPS of T1-2 and T12-L1. The incidence of occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments. The incidence of > 1/2 occlusion for the middle thoracic segments was significantly higher than that for the upper and lower thoracic segments. WP was longer than WV on T1-2 to T9-10 and shorter than WV on T10-11 to T12-L1. The horizontal puncture angle (α) into the external opening of the TIVF was positively correlated with the segments of the thoracic vertebrae from the cephalic to caudal portion.
The impact of the rib head/neck on the puncture path of the TIVF varies on different segments. It is necessary to identify spatial structure and design appropriate puncture angles for different segments.
In this article, we summarize and report on the spatial relationship between the ribs and ITPS as well as the puncture characteristics for thoracic intervertebral foramina cannulation. This study also provides an anatomic reference for performing clinical intervertebral foramen puncture, especially with ultrasound guidance.
Manuscript source: Unsolicited manuscript
Specialty type: Anatomy and morphology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Watanabe K S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Han Z, Hong T, Ding Y, Wang S, Yao P. CT-Guided Pulsed Radiofrequency at Different Voltages in the Treatment of Postherpetic Neuralgia. Front Neurosci. 2020;14:579486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Makharita MY, Amr YM. Effect of Repeated Paravertebral Injections with Local Anesthetics and Steroids on Prevention of Post-herpetic Neuralgia. Pain Physician. 2020;23:565-572. [PubMed] |
| 3. | Cohen SP, Sireci A, Wu CL, Larkin TM, Williams KA, Hurley RW. Pulsed radiofrequency of the dorsal root ganglia is superior to pharmacotherapy or pulsed radiofrequency of the intercostal nerves in the treatment of chronic postsurgical thoracic pain. Pain Physician. 2006;9:227-235. [PubMed] |
| 4. | Zhu J, Fei Y, Deng J, Huang B, Yao M. Application and Therapeutic Effect of Puncturing of the Costal Transverse Process for Pulsed Radiofrequency Treated T1-T3 Herpes Zoster Neuralgia. J Pain Res. 2020;13:2519-2527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Lee HJ, Park HS, Moon HI, Yoon SY. Effect of Ultrasound-Guided Intercostal Nerve Block Versus Fluoroscopy-Guided Epidural Nerve Block in Patients With Thoracic Herpes Zoster: A Comparative Study. J Ultrasound Med. 2019;38:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, Groen GJ. Different Approaches to Ultrasound-guided Thoracic Paravertebral Block: An Illustrated Review. Anesthesiology. 2015;123:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 7. | Ding Y, Li H, Hong T, Zhao R, Yao P, Zhao G. Efficacy and Safety of Computed Tomography-Guided Pulsed Radiofrequency Modulation of Thoracic Dorsal Root Ganglion on Herpes Zoster Neuralgia. Neuromodulation. 2019;22:108-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Zhao P, Mei L, Wang W. Clinical Study of Ultrasound-Guided Methylene Blue Thoracic Paravertebral Nerve Block for the Treatment of Postherpetic Neuralgia. Turk Neurosurg. 2019;29:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Hetta DF, Mohamed SAB, Mohamed KH, Mahmoud TAE, Eltyb HA. Pulsed Radiofrequency on Thoracic Dorsal Root Ganglion Versus Thoracic Paravertebral Nerve for Chronic Postmastectomy Pain, A Randomized Trial: 6-Month Results. Pain Physician. 2020;23:23-35. [PubMed] |
| 10. | Kim WJ, Park HS, Park MK. The effect of needle tip position on the analgesic efficacy of pulsed radiofrequency treatment in patients with chronic lumbar radicular pain: a retrospective observational study. Korean J Pain. 2019;32:280-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Taketa Y, Fujitani T. Approach affects injectate spread in ultrasound-guided thoracic paravertebral block: a cadaveric trial. Br J Anaesth. 2017;119:339-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W. Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J Neurosurg Spine. 2011;14:532-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Luo C, Yang B, Yang LQ, Wu BS, Wang XP, He LL, Zhao R, Ni JX, Tang YZ. Computed Tomography-Guided Percutaneous Coblation of the Thoracic Nerve Root for Treatment of Postherpetic Neuralgia. Pain Physician. 2020;23:E487-E496. [PubMed] |
| 14. | Patel A, Kumar V, Garg R, Bhatnagar S, Mishra S, Gupta N, Bharti SJ, Kumar S. Comparison of analgesic efficacy of ultrasound-guided thoracic paravertebral block versus surgeon-guided serratus anterior plane block for acute postoperative pain in patients undergoing thoracotomy for lung surgery-A prospective randomized study. Saudi J Anaesth. 2020;14:423-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Ji K, Wang Z, Zheng X, Wei H, Shi Y, Qian P. Application of ultrasound-guided paravertebral nerve block in preemptive analgesia of thoracic surgery. Panminerva Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Chang KV, Wu WT, Özçakar L. Ultrasound-Guided Interventions of the Cervical Spine and Nerves. Phys Med Rehabil Clin N Am. 2018;29:93-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Luyet C, Eichenberger U, Greif R, Vogt A, Szücs Farkas Z, Moriggl B. Ultrasound-guided paravertebral puncture and placement of catheters in human cadavers: an imaging study. Br J Anaesth. 2009;102:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 18. | Luyet C, Siegenthaler A, Szucs-Farkas Z, Hummel G, Eichenberger U, Vogt A. The location of paravertebral catheters placed using the landmark technique. Anaesthesia. 2012;67:1321-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |