Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4104
Peer-review started: February 1, 2021
First decision: March 11, 2021
Revised: March 15, 2021
Accepted: April 12, 2021
Article in press: April 12, 2021
Published online: June 6, 2021
Processing time: 102 Days and 7.8 Hours
An impalement injury of the oral cavity is a common traumatic injury in children. In most cases, it is not accompanied by sequelae, but if foreign body residues are not found due to a minor injury, they may result in inflammatory responses and delayed vascular injuries in the surrounding tissues. Without early diagnosis and appropriate initial management, residual foreign bodies can cause serious complications and even mortality in some cases.
A 9-year-old boy suffered an intra-oral injury by a wooden chopstick, and the patient was discharged from the hospital after receiving conservative treatment for the injury. However, the patient was readmitted to the hospital due to intra-oral bleeding, and since neck hematoma and right internal carotid artery pseudoaneurysm formation were detected on computed tomography, emergency surgery was performed. A remnant fragment of a wooden chopstick was found during the operation, and a delayed rupture of the internal carotid artery caused by the foreign body was also found.
The failure of early detection and diagnosis of a residual foreign body may result in delayed vascular rupture.
Core Tip: Preschool children often provide inappropriate descrip
- Citation: Chung BH, Lee MR, Yang JD, Yu HC, Hong YT, Hwang HP. Delayed pseudoaneurysm formation of the carotid artery following the oral cavity injury in a child: A case report. World J Clin Cases 2021; 9(16): 4104-4109
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/4104.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.4104
An intraoral trauma and a residual foreign body from the injury may be very dangerous because they can cause life-threatening complications. Impalement injuries occurring in children are mostly caused by pencils, sticks, cylindrical toys, straws, and toothbrushes[1,2]. If the wound or the foreign body is clearly visible, treatment can be started immediately. However, preschool children often provide inaccurate descrip
The child was brought to the emergency department of our institution, presenting with the chief complaint of right neck pain and swelling, because retropharyngeal, peri-tonsillar abscess was suspected at another institution.
A 9-year-old male patient had sustained an impalement injury of the neck by a wooden chopstick when he fell riding on a scooter with a wooden chopstick in his mouth two days before hospital admission.
The patient has never had an accident on his neck before.
In his past medical history, no specific features were found except for the fact that he had received the treatment of attention deficit hyperactivity disorder for the previous six months.
A physical examination showed no symptoms of respiratory distress, and no obvious foreign body or bleeding in the oral cavity was found.
Although the hemoglobin level dropped to 7.9 g/dL, there were no significant changes in blood pressure and heart rate, and swelling around the neck did not abate.
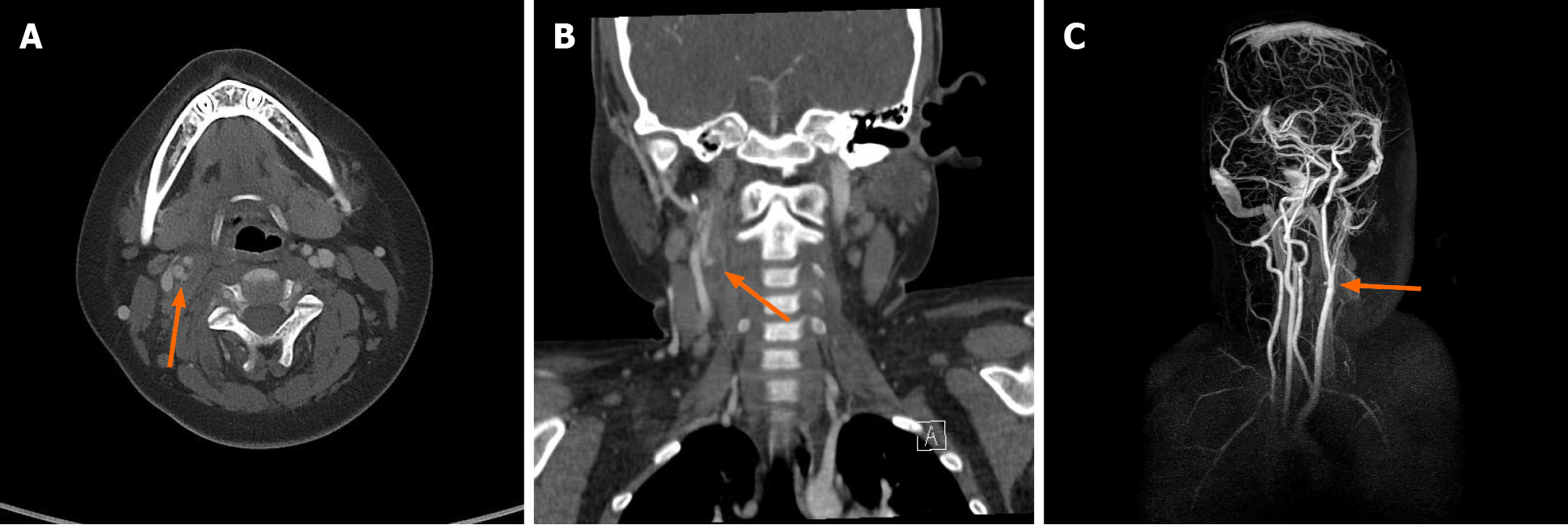
CT and MR angiography (MRA) revealed traumatic pseudoaneurysm formation accompanied by hematoma collection in the right proximal internal carotid artery about 5 mm above the right carotid bifurcation, and no active arterial extravasation was observed (Figure 1). As in the results of neck CT performed one week before, contrast-enhanced CT and MRA did not show a residual foreign body that was suspected to be a wooden chopstick fragment.
Pseudoaneurysm formation with hematoma collection in the right proximal internal carotid artery.
Emergent neck exploration.
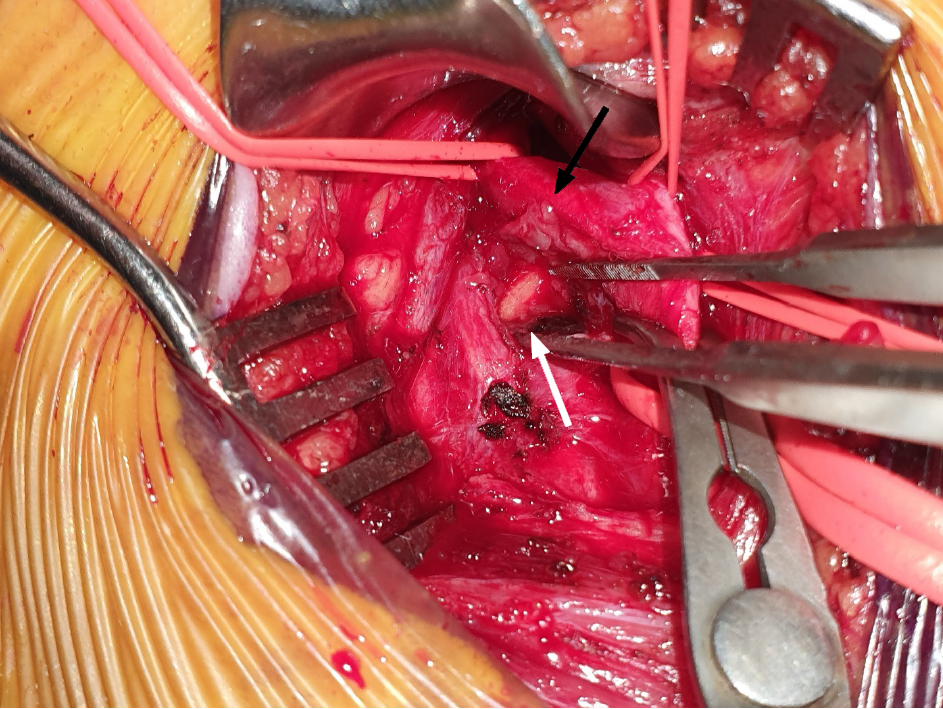
Since there were no findings indicating the presence of any intraoral wounds or bleeding, under general anesthesia with orotracheal intubation. Right neck extension was performed and exploration of the area around the right carotid artery was conducted. Inflammation and adhesion accompanied by moderate hematoma for
No neurologic defects were found after surgery, and no postoperative complications such as voice changes or respiratory failure were observed. After surgery, intravenous antibiotics were continuously administered, and gargle and ibuprofen syrup for oral hygiene were also continuously administered. The drainage tube was removed at postoperative day 4, and the follow-up neck CT at postoperative day 7 showed that the Rt. ICA injury site was intact, so the patient was discharged without any signs of complications at postoperative day 8.
A residual foreign body in the neck can cause life-threatening complications. It is not uncommon for patients to develop potentially serious sequelae after the occurrence of this type of injury. Deep neck abscess, multiple emphyema, arterial or venous thrombosis, and stroke may occur[4-7]. in this case, symptoms such as ICA pseudoaneurysm formation accompanied by intraoral bleeding and inflammatory responses in the surrounding tissues were observed about 10 d after the occurrence of the injury. A remnant foreign body can cause damage to tunica media with intact adventitia, resulting in the pseudoaneurysm formation of arteries. Reaching a definite diagnosis may be delayed during this period, and hematoma and abscess formation due to bleeding may eventually be life-threatening conditions[8].
Delayed vascular injury caused by a residual foreign body can be explained by several mechanisms. First, it may occur as a result of movements such as continuous swallowing or coughing, which can cause the broken wooden chopstick fragment to continuously cause trauma to adjacent blood vessels, damaging blood vessel walls. In addition, pseudoaneurysm may be formed due to the remnant wooden chopstick fragment, which may cause massive bleeding due to the delayed rupture of the neck vessel[9].
The broken chopstick fragment was not found until surgery was performed after the patient’s readmission to the hospital through the emergency department due to bleeding when one week elapsed after the accidental injury. One possible reason for delayed diagnosis and treatment is that detailed history taking on the accident situation regarding how the patient’s injury occurred may not have been carried out. The injury may not have been regarded as a serious one since the impalement injury of the oral cavity was accompanied only by slight bleeding, and no additional bleeding or injury to surrounding tissues and important structures were observed. In addition, although the patient received inpatient treatment for 3 d after his first visit to the emergency department, it seemed that the possibility of the presence of a residual foreign body was overlooked based only on the fact that no foreign body was found on initial CT scans without performing additional examinations of the lesion, such as ultrasound and MRA. As a result, the cause of neck trauma was not clearly elucidated, and the evaluation of remnant foreign bodies was not carried out.
It is known to be very difficult to detect or identify a wooden material penetrating an area around the neck by using plain x-ray and conventional radiogram because of the interference due to the opacity of cervical vertebra or soft tissue around the neck[10]. On the other hand, CT scan or ultrasonography is the most effective method to detect and identify the relationship of radiation-transmitting foreign bodies in soft tissue. Cross-sectional imaging by CT scan is useful for identifying the location of the foreign body and its relationship with the important structures of the neck[11]. Ultrasonography has been demonstrated to be an effective diagnostic method, and its sensitivities for 2.5 mm and 5 mm long wooden foreign bodies have been reported to be 86.7% and 93.3%, respectively[12]. In this case of impalement injury, CT scan was performed during the initial examination of the injury, but the method had limitations for making a definite diagnosis. However, the use of additional examination methods such as ultrasonography could have resulted in early diagnosis and treatment in this case.
Delayed rupture and pseudoaneurysm formation of the carotid artery in preschool children are rare, but they are potentially life-threatening diseases, and they can be caused by a residual foreign body after trauma. For child patients, from whom it is difficult to obtain a clear and accurate trauma history, a thorough physical exami
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang L S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | Lee JA, Lee HY. A case of retained wooden foreign body in orbit. Korean J Ophthalmol. 2002;16:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Shirali GN, Savant RA, Uppal PK, Bhargava KB. Toothbrush: an unusual foreign body in ENT practice. J Laryngol Otol. 1988;102:1068-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Bar T, Zagury A, Nahlieli O, London D, Yoffe B, Bibi H. Delayed signs and symptoms after oropharyngeal trauma in a child. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:15-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Moriarty KP, Harris BH, Benitez-Marchand K. Carotid artery thrombosis and stroke after blunt pharyngeal injury. J Trauma. 1997;42:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Law RC, Fouque CA, Waddell A, Cusick E. Lesson of the week. Penetrating intra-oral trauma in children. BMJ. 1997;314:50-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Rowley H, Christian J, Dennis A. Pharyngeal perforation: an easily missed finding following intra-oral injury. J Accid Emerg Med. 1995;12:145-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Borges G, Bonilha L, Santos SF, Carelli EF, Fernandes YB, Ramina R, Zanardi V, Menezes JR, Nogueira RJ. Thrombosis of the internal carotid artery secondary to soft palate injury in children and childhood. Report of two cases. Pediatr Neurosurg. 2000;32:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Thakore N, Abbas S, Vanniasingham P. Delayed rupture of common carotid artery following rugby tackle injury: a case report. World J Emerg Surg. 2008;3:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Luo Y, Yuan H, Cao ZS. Residual foreign body in the neck after trauma results in the delayed rupture of the common carotid and internal jugular vein: a case report. J Med Case Rep. 2013;7:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Kantarci M, Ogul H, Karasen RM. Detection of a giant wooden foreign body with multidetector computed tomography and multiplanar reconstruction imaging. Am J Emerg Med. 2007;25:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Mohammadi A, Ghasemi-Rad M, Khodabakhsh M. Non-opaque soft tissue foreign body: sonographic findings. BMC Med Imaging. 2011;11:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Jacobson JA, Powell A, Craig JG, Bouffard JA, van Holsbeeck MT. Wooden foreign bodies in soft tissue: detection at US. Radiology. 1998;206:45-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 130] [Article Influence: 4.8] [Reference Citation Analysis (0)] |