Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3996
Peer-review started: January 4, 2021
First decision: January 24, 2021
Revised: January 27, 2021
Accepted: February 8, 2021
Article in press: February 8, 2021
Published online: June 6, 2021
Processing time: 130 Days and 0.1 Hours
Coronary artery aneurysm combined with myocardial bridge is a very rare clinical situation. The prognosis of this clinical situation is not yet clear.
A coronary artery aneurysm and myocardial bridge in the same segment of the coronary artery were found in a 54-year-old female patient who underwent coronary angiography and intravascular ultrasound examination. Through conservative treatment, the patient was discharged from the hospital smoothly, and she was in good condition during 5 mo of follow-up.
Coronary artery aneurysm combined with myocardial bridge seems to have a good prognosis, but due to the rarity of this clinical situation, further research and follow-up are needed.
Core Tip: We found a rare condition, in which a coronary artery aneurysm and myocardial bridge co-occurred in the same segment of the coronary artery, by coronary angiography and intravascular ultrasound examination. The prognosis of this clinical situation seems to be good, but due to its rarity, further research and follow-up are needed.
- Citation: Ye Z, Dong XF, Yan YM, Luo YK. Coronary artery aneurysm combined with myocardial bridge: A case report. World J Clin Cases 2021; 9(16): 3996-4000
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3996.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3996
Coronary artery aneurysm (CAA) is defined as fractional dilation of coronary arteries. The diameter of the dilated segment is at least 1.5 times larger than that of the adjacent normal segment. When exceeding four times the diameter of the adjacent normal segment, it is called a giant coronary aneurysm. Diffuse coronary artery dilation is called coronary artery ectasia[1,2]. The normal coronary arteries and their main branches run on the surface of the heart. When some of the coronary arteries penetrate into the myocardium, they are compressed during myocardial systole. This part of the coronary arteries is called the tunnel artery, and the myocardium on its surface is called the myocardial bridge[3,4].
CAA and myocardial bridge are relatively rare diseases, and coexistence in the same segment of a coronary artery is an even rarer clinical situation. This clinical situation is rarely reported, and its prognosis is still unclear.
In May 2020, a 54-year-old woman was hospitalized with a chief complaint of exertional chest pain for more than 10 years.
Chest pain was located in the upper part of the sternum, lasted for approximately a few seconds, and could be relieved after rest. The symptoms worsened 6 mo prior, with chest pain occurring after mild activity and more frequently than before.
The patient had a history of hypertension for more than 5 years and took drugs regularly to control her blood pressure, and her blood pressure was acceptable.
The patient had no significant prior personal or family history.
The patient’s blood pressure was 159/104 mmHg on admission, and the remainder of the physical examination showed no obvious abnormalities.
The low-density lipoprotein cholesterol was 4.18 mmol/L (normal reference range: 1.10-3.50 mmol/L), cardiac biomarkers such as troponin and N-terminal pro-brain natriuretic peptide were normal, and the other blood tests were also approximately normal.
Electrocardiogram showed abnormal Q waves in leads II, III, aVF, V5-V6, and V7-V9 and slight elevation of the ST segment in leads II, III, aVF, and V1-V4. There were no remarkable findings on ultrasonic cardiogram.
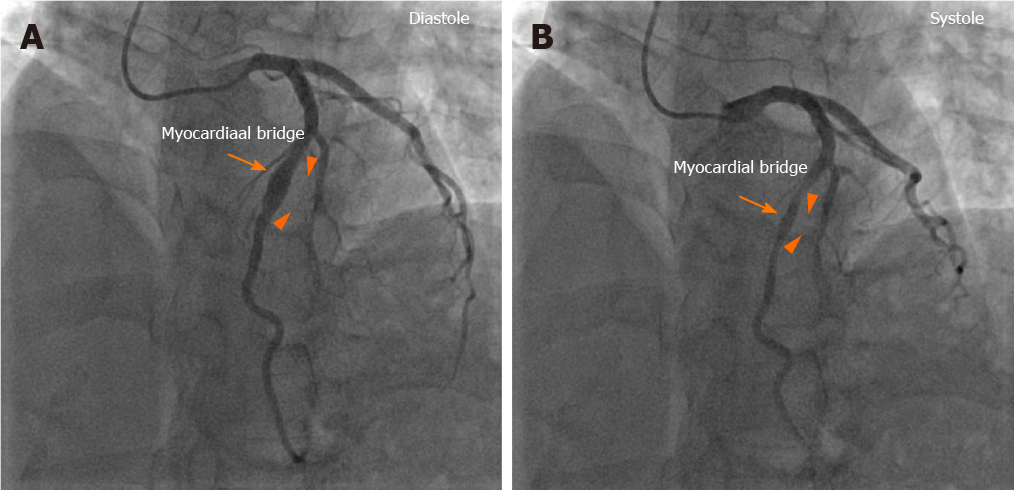
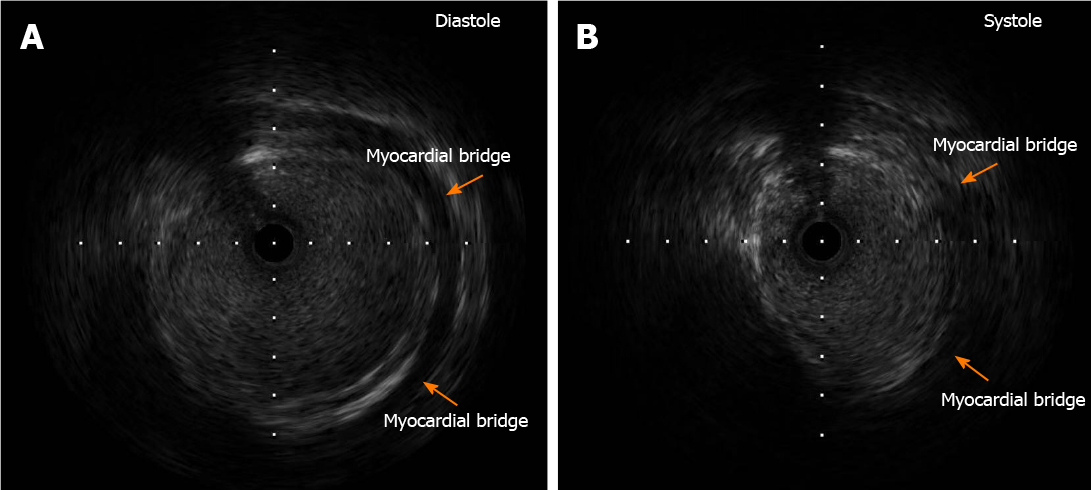
Subsequent coronary angiography (CAG) revealed a normal right coronary artery and circumflex artery without any anomalies or sign of atherosclerosis. In the proximal to middle part of the left anterior descending artery (LAD), there was a near 25 mm long tumor-like aneurysm. The diameter of this aneurysm varied with the cardiac cycle. During cardiac systole, the aneurism was compressed by approximately 70% (Figure 1A and B). There was no obvious sign of atherosclerosis within other segments of LAD. Following intravascular ultrasound (IVUS) examination showed that the maximum diameter of the CAA during systole was 7.7 mm, the minimum diameter during systole was 4.02 mm, and the muscle bridge was clearly visible above the coronary artery (Figure 2A and B).
The final diagnosis of the presented case was CAA combined with myocardial bridge.
After invasive coronary examination, the patient’s discharge medications included aspirin 100 mg/d, rosuvastatin 10 mg/d, metoprolol 47.5 mg/d, and amlodipine 5 mg/d.
The patient was then discharged because of symptom relief, and she was recently in good condition at the 5-mo follow-up by phone.
The incidence of CAA ranges from 1.2% to 4.9% and is most common in the right coronary artery, followed by the LAD branch and left circumflex branch, with the left main artery being the least affected[5]. It is currently believed that the most common cause of coronary aneurysms in adults is atherosclerosis, accounting for approximately 50%, and the most common cause in children is Kawasaki disease. Other rare causes include inflammatory diseases, connective tissue diseases, infection, congenital diseases, iatrogenic diseases, and drugs[1,6]. The detection rate of myocardial bridge in CAG ranges from 1.5% to 16%, but the detection rate in autopsy can be as high as 80%; moreover, the majority of cases of myocardial bridge occur in the LAD. Myocardial bridge is considered a congenital benign disease[3,4].
The combination of CAA and myocardial bridge at the same site of a coronary artery is relatively rare in clinical practice. Manfred Mauser and Manish Motwani have reported two such cases, but they only relied on CAG to diagnose this special coronary phenomenon[7,8]. CAG can reveal the location, size, and shape of the CAA, but the size of the CAA may be underestimated when thrombi form in the lumen of the CAA[9,10]. Therefore, we combined IVUS with CAG to conduct further examination of our patient. IVUS allows to observe whether the aneurysm has a complete three-layer vascular wall structure to distinguish between true and false aneurysms and whether there is thrombosis in the aneurysm lumen[11]. True aneurysms have intact intima, media, and adventitia, while the vascular integrity of false aneurysms is lost and they lack at least one layer of the artery wall and consist of a single or double layer that protrudes outward[12]. Myocardial bridge can manifest as a characteristic "half-moon" transparent echo area around the lumen in IVUS[13]. In this case, IVUS showed that there was no obvious plaque or thrombosis formation in the CAA segment, and the myocardial bridge was clearly shown around the CAA.
It was a pity that we missed the further functional examinations such as single photon emission tomography, scintigraphy, or nuclear magnetic resonance, so we could not exclude the presence of ischemia or microvascular disease in this case.
The prognosis of CAA may be better when it is combined with myocardial bridge. Furthermore, myocardial bridge may limit the excessive expansion of the coronary arteries, and periodic compression of the CAA by the myocardial bridge may reduce congestion in the aneurysm, which could be a risk factor for thrombosis. The outcome of such a rare combination needs further research and follow-up.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Naswhan AJ, Rostagno C S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Sheikh AS, Hailan A, Kinnaird T, Choudhury A, Smith D. Coronary Artery Aneurysm: Evaluation, Prognosis, and Proposed Treatment Strategies. Heart Views. 2019;20:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 2. | Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of Coronary Artery Aneurysms. JACC Cardiovasc Interv. 2018;11:1211-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 247] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 3. | Kalaria VG, Koradia N, Breall JA. Myocardial Bridge: a clinical review. Catheter Cardiovasc Interv. 2002;57:552-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Alegria JR, Herrmann J, Holmes DR Jr, Lerman A, Rihal CS. Myocardial bridging. Eur Heart J. 2005;26:1159-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 271] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 5. | Devabhaktuni S, Mercedes A, Diep J, Ahsan C. Coronary Artery Ectasia-A Review of Current Literature. Curr Cardiol Rev. 2016;12:318-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Morita H, Ozawa H, Yamazaki S, Yamauchi Y, Tsuji M, Katsumata T, Ishizaka N. A case of giant coronary artery aneurysm with fistulous connection to the pulmonary artery: a case report and review of the literature. Intern Med. 2012;51:1361-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Mauser M. Combination of aneurysm and myocardial bridging at the same site of a coronary artery in a patient with obstructive hypertrophic cardiomyopathy. Catheter Cardiovasc Interv. 2000;49:325-327. [PubMed] [DOI] [Full Text] |
| 8. | Motwani M, Arya S, MacDonald JE. Myocardial bridging with a coronary artery aneurysm and left ventricular stunning. Am J Med Sci. 2011;341:510-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Pahlavan PS, Niroomand F. Coronary artery aneurysm: a review. Clin Cardiol. 2006;29:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 150] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 10. | Murthy PA, Mohammed TL, Read K, Gilkeson RC, White CS. MDCT of coronary artery aneurysms. AJR Am J Roentgenol. 2005;184:S19-S20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Sanidas EA, Vavuranakis M, Papaioannou TG, Kakadiaris IA, Carlier S, Syros G, Dangas G, Stefanadis C. Study of atheromatous plaque using intravascular ultrasound. Hellenic J Cardiol. 2008;49:415-421. [PubMed] |
| 12. | Kar S, Webel RR. Diagnosis and treatment of spontaneous coronary artery pseudoaneurysm: Rare anomaly with potentially significant clinical implications. Catheter Cardiovasc Interv. 2017;90:589-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Ge J, Erbel R, Rupprecht HJ, Koch L, Kearney P, Görge G, Haude M, Meyer J. Comparison of intravascular ultrasound and angiography in the assessment of myocardial bridging. Circulation. 1994;89:1725-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 187] [Article Influence: 6.0] [Reference Citation Analysis (0)] |