Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3936
Peer-review started: November 16, 2020
First decision: December 13, 2020
Revised: December 26, 2020
Accepted: March 18, 2021
Article in press: March 18, 2021
Published online: June 6, 2021
Processing time: 178 Days and 19.4 Hours
Appendiceal mucocele is a rare disease that causes obstructive dilatation of the appendix due to the intraluminal accumulation of mucin. We report a case of endoscopic diagnosis and treatment of an appendiceal mucocele.
A 47-year-old man presented with a protrusion around the orifice of the appendix discovered by colonoscopy incidentally. He was admitted to our hospital for a routine checkup without any symptoms. Abdominal computed tomography showed a cystic mass approximately 3 cm in diameter with fat stranding. The preoperative diagnosis was non-neoplastic appendiceal mucocele, and endoscopic treatment was performed. The endoscopic findings and pathological results supported our preoperative diagnosis. The endoscopic treatment of appendiceal mucocele was feasible and effective, which was confirmed by repeated endoscopy and post-operative computed tomography after 7 mo.
Endoscopic therapy provides a new method for the treatment of appendiceal mucocele.
Core Tip: Appendiceal mucocele is rare and was formerly treated by surgical resection. However, iatrogenic rupture of the mucocele may lead to peritoneal dissemination in malignant cases. Colonoscopy is not only significant for diagnosis but also helps treat appendiceal mucocele. Here, we report a case of appendiceal mucocele that was successfully diagnosed and treated by endoscopy.
- Citation: Wang TT, He JJ, Zhou PH, Chen WW, Chen CW, Liu J. Endoscopic diagnosis and treatment of an appendiceal mucocele: A case report. World J Clin Cases 2021; 9(16): 3936-3942
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3936.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3936
Appendiceal mucocele is a rare disease that causes obstructive dilatation of the appendix due to the intraluminal accumulation of mucin. The incidence of this condition is 0.2%-0.3% of all appendectomy specimens and 8%-10% of all appendiceal tumors[1]. Appendiceal mucocele is more common in females aged 50-60 years old[2]. Mucoceles may mostly result from luminal obstruction of the appendix root and mucus retention secreted by the distal appendiceal mucosa, causing the appendix to gradually expand into a cystic structure[3]. The preoperative diagnosis of appendiceal mucocele is very difficult. Up to 50% of cases are asymptomatic and discovered incidentally during radiology, endoscopy, or surgery[4]. The most frequent symptom is nonspecific abdominal pain, usually accompanied by a palpable mass in the right iliac fossa, nausea, vomiting, and weight loss[5]. Surgical resection is the traditionally recommended management strategy for appendiceal mucocele. We report a case of endoscopic diagnosis and treatment of an appendiceal mucocele.
A 47-year-old man presented with a protrusion around the orifice of the appendix discovered by colonoscopy incidentally.
The patient denied the presence of abdominal pain, abdominal distention, nausea, or vomiting without weight loss.
No significant past medical history was recorded, such as smoking or drinking.
The patient had no previous or family history of similar illnesses.
The vital signs and physical examination showed no pathological changes.
All the laboratory test results were within the reference ranges.
Abdominal computed tomography (CT) revealed a cystic mass approximately 3 cm in diameter with fat stranding (Figure 1).
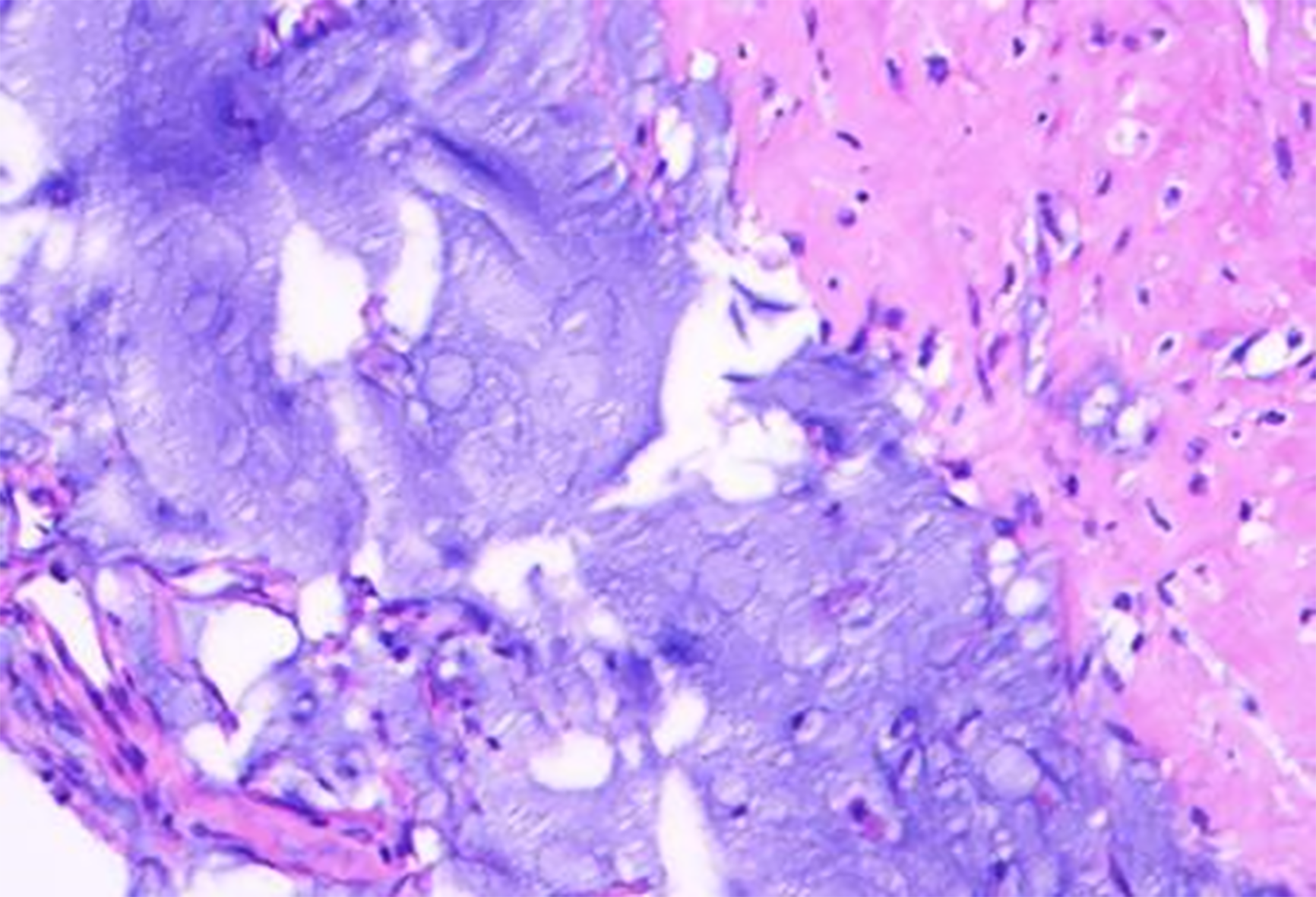
The preoperative diagnosis was non-neoplastic appendiceal mucocele. Biopsy of the protrusion revealed inflammatory changes in the cecal mucosa and a small amount of myxoid tissue in the focal zone (Figure 2). The intraoperative findings and histopa
The patient underwent endoscopic treatment under intravenous anesthesia. The procedure was performed using a single-channel endoscope (CV-290, Olympus) and a high-frequency electric cutting device (VIO 300D, ERBE). The unit was set for Endocut-Q, effect 3, cutting width 2, and time interval 4.
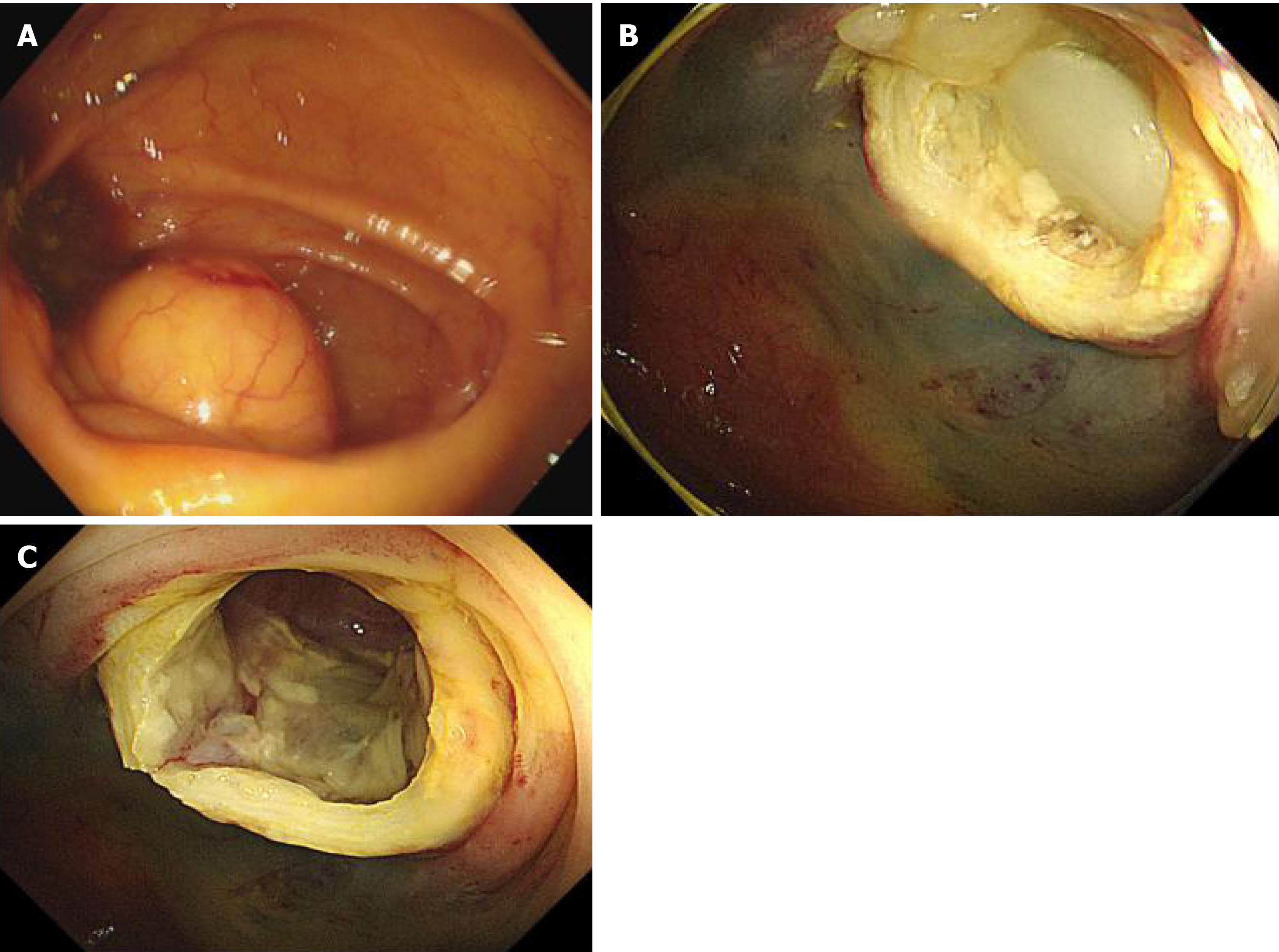
The detailed operation steps in our case were as follows: Endoscopy revealed a smooth-surfaced submucosal mass of the cecum, in which the appendiceal orifice was located in the center (Figure 3A). We injected the mixed solution of saline, indigo carmine, and epinephrine into the submucosa to elevate the lesion. Then, a snare was placed at the base of the lesion, and the submucosal mass was removed after tightening the snare. After resection of the submucosal mass, a large amount of clear yellowish mucus flowed through the appendiceal orifice into the cecum (Figure 3B). The endoscope was advanced into the appendiceal cavity after flushing the mucus completely. After clearing the mucus, the smooth inner wall of the appendix was exposed, and no nodules were visualized (Figure 3C).
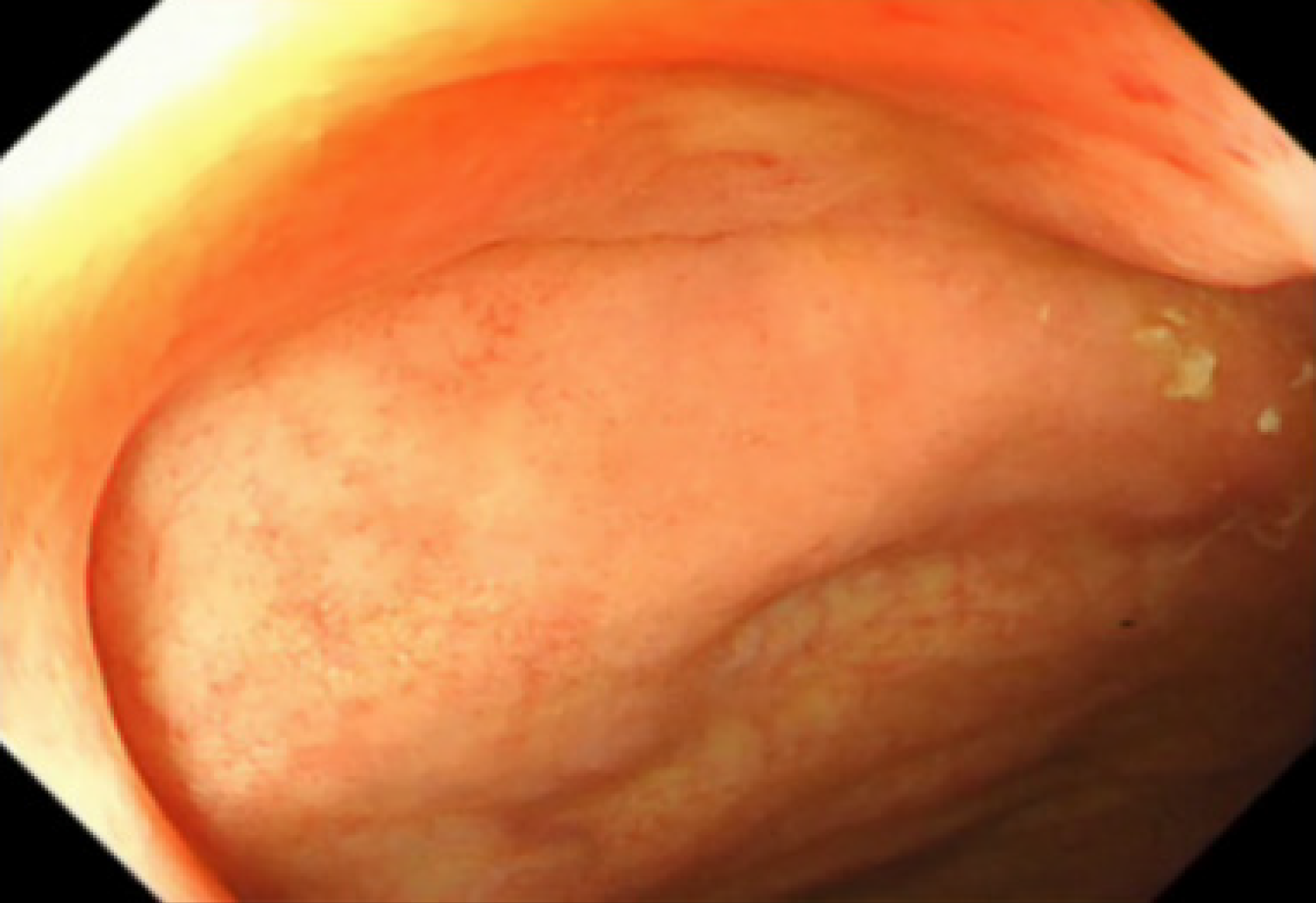
The patient was asymptomatic during follow-up. Repeat endoscopy performed approximately 7 mo later revealed no submucosal mound in the normal appendiceal orifice (Figure 4). Postoperative CT showed no abnormalities in the appendix (Figure 5).
In this study, we report a case of appendiceal mucocele that was asymptomatic and discovered incidentally during colonoscopy. It was successfully diagnosed and treated by endoscopy. And there was no recurrence at the 7-mo follow-up.
Appendiceal mucoceles have been classified into four pathologic entities[6]: (1) Simple/retention mucocele; (2) Hyperplastic mucocele (5%-25%); (3) Mucinous cystadenoma (63%-84%); and (4) Mucinous cystadenocarcinoma (11%-20%). Luminal dilatation of a simple mucocele and hyperplastic mucocele is generally mild, and their short-axis diameter rarely exceeds 2 cm. However, mucoceles greater than 6 cm in size may be associated with cystadenoma or cystadenocarcinoma and have a higher perforation rate, which may lead to the development of pseudomyxoma peritonei (PMP)[7].
It is difficult to make an appropriate preoperative diagnosis because of the nonspecific clinical presentation of appendiceal mucocele. In recent years, with the improvement of diagnostic techniques and accumulation of clinical experience, the preoperative diagnosis rate has been improved. CT is the most commonly used preoperative diagnosis method. The typical feature of a mucocele is a well-encap
Surgical resection is the only recommended treatment for appendiceal mucocele. Carcinomas represent 11%-20% of all cases and the surgical treatment plan should be carefully made on the basis of pathology. Cubro et al[6] reported a case of appendiceal mucocele that was discovered accidentally by surgical procedure. And there was no recurrence at the 6-mo follow-up after a simple appendectomy. Motsumi et al[4] presented a case of giant appendiceal mucocele that was treated by a right hemicolectomy, and the patient recovered uneventfully. Simple appendectomy is the optimal treatment for patients with a histological diagnosis of benign mucocele. If the histological diagnosis is cystadenocarcinoma, appendectomy combined with right colectomy should be performed[13]. However, the disadvantages of surgical procedures include a high degree of trauma, high cost, and possible serious complications caused by mucocele rupture. For non-neoplastic appendiceal mucocele, colonoscopy could replace traditional surgery to achieve good therapeutic effects by fully flushing the mucus. For neoplastic appendiceal mucocele, surgical resection increases the risk of implantation metastasis caused by mucocele rupture if the intraluminal pressure of the appendix is high. However, colonoscopy can relieve the pressure on the appendicular lumen by flushing the mucus, thus reducing the risk of rupture caused by subsequent surgery. Due to the disadvantages of surgical procedures that have been described above and the patients’ preference for endoscopic minimally invasive treatment, we decided to try to achieve a satisfactory therapeutic effect by endoscopic treatment.
Appendectomy for simple mucocele, hyperplastic mucocele, and mucinous cystadenoma has a 90%-100% 5-year survival rate. The outcome of cystadenocarcinoma without the base of the appendix or peritoneal or adjacent organ involvement after surgical resection is also excellent[14]. However, PMP often recurs after treatment and the 10-year survival rate falls to 63% for PMP after surgery[15]. Our patient in this case had no evidence of recurrence over 7 mo of follow-up after endoscopic treatment. Therefore, we did not recommend further surgical resection for this patient.
In conclusion, we report a case of appendiceal mucocele that was successfully diagnosed and treated by endoscopy. For non-neoplastic appendiceal mucocele, the colonoscopy procedure can not only help obtain a diagnosis but also help achieve a satisfactory therapeutic effect by fully flushing the mucus. Moreover, for neoplastic appendiceal mucocele, colonoscopy might relieve the pressure on the appendicular lumen by flushing the mucus and reduce the risk of rupture.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bustamante-Balen M S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Abuoğlu H, Yıldız MK, Kaya B, Odabaşı M. Clinicopathological analysis of patients operated for appendiceal mucocele. Ulus Travma Acil Cerrahi Derg. 2017;23:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Van Hooser A, Williams TR, Myers DT. Mucinous appendiceal neoplasms: pathologic classification, clinical implications, imaging spectrum and mimics. Abdom Radiol (NY). 2018;43:2913-2922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | Athanassiou E, Spyridakis M, Karasavvidou F, Vamvakopoulou D, Karaiskou E, Vamvakopoulos N, Theodosiou P, Hatzitheofilou C. Low-Grade Appendiceal Mucinous Neoplasm Presenting as a Surgical Emergency: A Case Report. Case Rep Oncol. 2009;2:7-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Motsumi MJ, Motlaleselelo P, Ayane G, Sesay SO, Valdes JR. A case report of a giant appendiceal mucocele and literature review. Pan Afr Med J. 2017;28:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Rymer B, Forsythe RO, Husada G. Mucocoele and mucinous tumours of the appendix: A review of the literature. Int J Surg. 2015;18:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Cubro H, Cengic V, Burina N, Kravic Z, Beciragic E, Vranic S. Mucocele of the appendix presenting as an exacerbated chronic tubo-ovarian abscess: A case report and comprehensive review of the literature. Medicine (Baltimore). 2019;98:e17149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Pickhardt PJ, Levy AD, Rohrmann CA Jr, Kende AI. Primary neoplasms of the appendix: radiologic spectrum of disease with pathologic correlation. Radiographics. 2003;23:645-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 202] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | Dixit A, Robertson JH, Mudan SS, Akle C. Appendiceal mucocoeles and pseudomyxoma peritonei. World J Gastroenterol. 2007;13:2381-2384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Sharma P, Soin P, Chugh M, Goyal P. Dilated Appendix: Is There More to It? J Clin Imaging Sci. 2019;9:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Sharma P, Hegde R, Kulkarni A, Soin P, Kochar P, Rotem E. Imaging right lower quadrant pain: Not always appendicitis. Clin Imaging. 2020;63:65-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Leshchinskiy S, Ali N, Akselrod D. The onion skin sign of appendiceal mucocele. Abdom Radiol (NY). 2018;43:2527-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Zanati SA, Martin JA, Baker JP, Streutker CJ, Marcon NE. Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc. 2005;62:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Nagata H, Kondo Y, Kawai K, Ishihara S, Kazama S, Nirei T, Soma D, Yamada J, Sunami E, Kitayama J, Kubota Y, Watanabe T. A giant mucinous cystadenocarcinoma of the appendix: a case report and review of the literature. World J Surg Oncol. 2016;14:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | McFarlane ME, Plummer JM, Bonadie K. Mucinous cystadenoma of the appendix presenting with an elevated carcinoembryonic antigen (CEA): Report of two cases and review of the literature. Int J Surg Case Rep. 2013;4:886-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Glasgow SC, Gaertner W, Stewart D, Davids J, Alavi K, Paquette IM, Steele SR, Feingold DL. The American Society of Colon and Rectal Surgeons, Clinical Practice Guidelines for the Management of Appendiceal Neoplasms. Dis Colon Rectum. 2019;62:1425-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |