Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3869
Peer-review started: December 28, 2020
First decision: January 17, 2021
Revised: January 30, 2021
Accepted: March 10, 2021
Article in press: March 10, 2021
Published online: June 6, 2021
Processing time: 136 Days and 17.8 Hours
Dynamic cervical implant (DCI) stabilization has been reported to have satisfactory clinical and radiological results with short- and mid-term follow-up in the treatment of cervical degenerative disc disease. However, few reports about the clinical and radiological outcome with more than 5-year follow-up exist.
To investigate the long-term clinical and radiological results of DCI arthroplasty.
A total of 40 patients who received DCI arthroplasty were consecutively reviewed from May 2010 to August 2015. Visual analogue scale (VAS), neck disability index (NDI) score, Japanese Orthopaedic Association (JOA) score, and SF-36 items were used to assess neural function rehabilitation. Static and dynamic radiographs and 3-dimentional computed tomography were used to evaluate the radiological outcomes.
The scores of neck/arm VAS, NDI, JOA, and 8-dimensions of SF-36 were significantly improved at the 1-mo follow-up (P < 0.05) and maintained until the last follow-up (P < 0.05). The range of motion (ROM) of C2-C7, functional spinal unit (FSU), upper/lower adjacent level, C2-C7 lateral bending, and FSU lateral bending decreased at the 1-mo follow-up (P < 0.05), whereas they increased to the preoperative level at the later follow-up intervals (P > 0.05), except the ROM of FSU lateral bending (P < 0.05). The C2-C7 alignment and FSU angle kept more lordotic at the last follow-up (P < 0.05). The intervertebral height increased significantly at the 1-mo follow-up (P < 0.05) and decreased at later follow-ups (P > 0.05). At the last follow-up, 12 (26.1%) segments developed heterotopic ossification.
DCI arthroplasty is a safe and effective non-fusion technique to treat cervical degenerative disc disease in long-term follow-up.
Core Tip: Dynamic cervical implant (DCI) stabilization has been reported to have satisfactory clinical and radiological results with short- and mid-term follow-up in the treatment of cervical degenerative disc disease. This is a 5-year follow-up study to investigate long-term results of DCI arthroplasty. The results showed the patients’ clinical results were significantly improved at the last follow-up. The functional spinal unit lateral bending was limited, the segmental flexion-extension range of motion could be partially preserved, and the range of motion at adjacent level could be maintained after DCI arthroplasty. We believe that DCI arthroplasty is a safe and effective non-fusion technique to treat cervical degenerative disc disease.
- Citation: Zou L, Rong X, Liu XJ, Liu H. Clinical and radiological outcomes of dynamic cervical implant arthroplasty: A 5-year follow-up. World J Clin Cases 2021; 9(16): 3869-3879
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3869.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3869
Anterior cervical discectomy and fusion (ACDF) was first reported by Cloward[1] in the late 1950s. It is a safe and effective treatment for symptomatic cervical spondylosis[2,3]. However, this technique yields a loss of mobility at the surgically treated segment and increased stress on adjacent segments, which contribute to the adjacent segment disease (ASD)[4-6]. In the past two decades, cervical artificial disc replacement (C-ADR) offered several theoretical advantages over ACDF. C-ADR could preserve the segmental range of motion (ROM) at the treated level and minimize abnormal kinematics and stress at the adjacent level, which in theory could avoid the acceleration of the degeneration at the adjacent level. Although C-ADR was reported to be successful in treating the cervical degenerative disc disease (DDD), several complications, such as heterotopic ossification, delayed spontaneous fusion, and hypermobility of prosthesis, were observed by some authors[7,8].
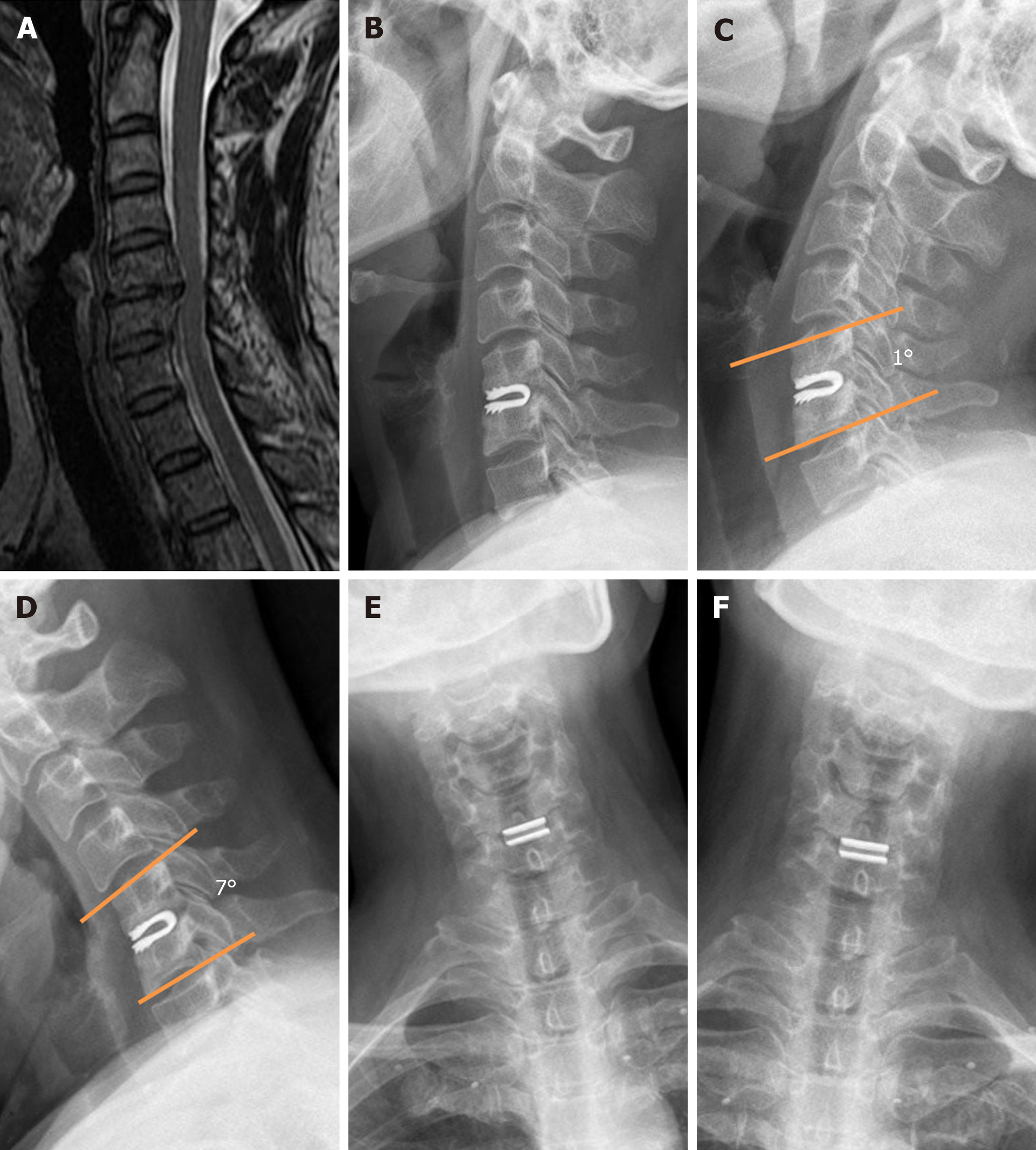
Recently, a novel anterior cervical implant design, the dynamic cervical implant (DCI, Paradigm Spine, New York, NY, United States), which is designed to function between ACDF and arthroplasty, has been introduced. Unlike the artificial cervical disc and plate-cage system, this “U”-shaped titanium implant is designed to have the characteristics of immediate stability, semi-constrained flexion-extension motion, and shock absorption. To our knowledge, previous studies mainly focused on short or mid-term follow-up[9-12]. This study was designed as a 5-year follow-up to investigate the long-term clinical and radiological results of DCI arthroplasty.
The patients who received DCI implantation were consecutively collected at our institution from May 2010 to August 2015 retrospectively. This study was approved by the biomedical ethics committee of West China Hospital. The inclusion criteria were age from 18 to 70 years, radiculopathy or myelopathy due to cervical DDD from C3 to C7 level refractory to non-operative therapy for more than 3 mo, and follow-up for more than 5 years. The exclusion criteria included active infection, metabolic or systemic disease, pregnancy, rheumatoid arthritis, bony cervical canal stenosis, severe osteoporosis, tumor, cervical spondylolisthesis, being hyper-reactive to metal and functional spinal unit (FSU), and ROM < 6°. Facet disease was not an absolute contraindication for DCI.
After anesthesia, the patient was placed supine with the arms at the sides and shoulders taped to keep the cervical alignment in a neutral position. A 5 to 6 cm transverse incision was made on the right side of the neck. The standard Smith-Robinson approach was adopted to expose the index level with the assistance of Caspar Cervical Retractor System (CCRS, Aesculap, Burlingame, CA, United States). Discectomy was performed with the posterior longitudinal ligament and extruded disc removed subsequently. The osteophytes at the posterior rim of the vertebra were excised, whereas the osteophytes at the anterior rim were seldom dealt with. The cartilaginous endplates were completely scraped, with the bony endplates kept intact. Then, the appropriate size of the prosthesis was determined on the intra-operative C-arm images. Keel cuts were made using the trail as a guide and keel cutting chisel. After the DCI prosthesis was inserted, the intra-operative C-arm images were taken to confirm the appropriateness of the size and placement of the implant. The superior and inferior surface of the implant should cover the endplate as large as possible. The prosthesis should be placed in the middle of the intervertebral space with the anterior and posterior borders more than 3 mm from the vertebral body rims.
Comprehensive neurological examinations were performed on all patients preoperatively and at the 1-, 6-, 12-, 24-, and 60-mo follow-ups. Visual analogue scale (VAS), neck disability index (NDI), and Japanese Orthopaedic Association (JOA) score were used to evaluate the pain, disability, and quality of life, respectively. The 8-dimension SF-36 score (physical function, mental health, bodily pain, vitality, role-physical, role-emotional, society function, and general health) was adopted to evaluate the quality of life. Odom et al[13]’s criteria were used to evaluate the patients’ satisfaction.
Radiographic examinations were performed preoperatively and at the 1-, 6-, 12-, 24-, and 60- mo follow-ups. The intervertebral disc space height of operated segment was measured on the lateral radiographs, and the C2-C7 alignment and FSU angle were determined using Harrison et al[14]’s method. Both the flexion-extension and lateral bending ROMs of C2-C7, FSU, and adjacent levels were determined on dynamic radiographs, using the Cobb method with Canvas 11(ACD Systems, Seattle, WA, United States) software. Computed tomography (CT) examination was introduced to assess the heterotopic ossification (HO) formation at the 1-, 12-, and 60-mo follow-ups postoperatively. All the measurements were performed by Zou L and Liu XJ independently, blindly to the clinics and the operation.
Continuous data are presented as the mean ± SD, and categorical data are presented as numbers and percentages. Differences between two groups were assessed by the independent sample t test or the Mann-Whitney test for continuous variables, and by chi-square or Fisher’s exact test for categorical variables. Intraclass correlation coefficient (ICC) was calculated to measure the inter-observer agreement of radiographic analysis by Cohen’s k statistic[15]. Kappa values greater than 0.75 were taken to represent excellent agreement, values between 0.4-0.75 represented good agreement, and values below 0.4 poor agreement. All statistical analyses were performed using SPSS software (Version 19, Chicago, IL, United States). The statistical significance levels were all two-sided; the statistical significance was set at P < 0.05.
A total of 48 patients accepted DCI arthroplasty at our institution from May 2010 to August 2015. Among them, 40 patients who completed 60-mo follow-up were enrolled. All operations were conducted by Liu H using the same surgical protocol. Patient data were collected retrospectively with a minimum follow-up of 60 mo (mean, 70.8 mo; range, 60-92 mo). The demographic data are presented in Table 1.
| Demographic | |
| Gender (male:female) | 22:18 |
| Age (years) | 45.6 (26-66) |
| Symptoms | |
| Radiculopathy | 18 |
| Myelopathy | 12 |
| Both | 10 |
| Implanted level | |
| C3/4 | 4 |
| C4/5 | 9 |
| C5/6 | 23 |
| C6/7 | 10 |
| Blood loss (mL) | |
| Single-level | 97 ± 18 |
| Double-level | 120 ± 26 |
| Operation time (min) | |
| Single-level | 93 ± 15 |
| Double-level | 131 ± 27 |
| Hospital day (d) | 10 |
| Ambulation after operation | 2th day |
| Alcohol (%) | 15 (37.5) |
| Smoking (%) | 10 (25) |
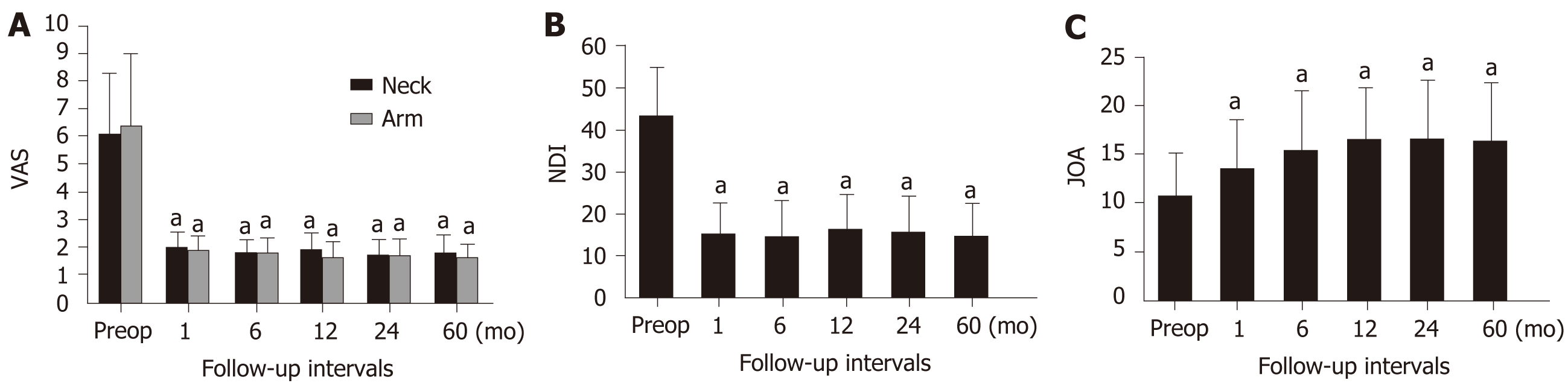
The clinical outcomes were evaluated with several questionnaires and scales. The neck and arm VAS scores were 6.1 ± 2.2 and 6.4 ± 2.6 preoperatively, which dropped at 1 mo postoperatively to 2.0 ± 0.6 and 1.9 ± 0.8 (P < 0.05), respectively. The scores dropped further at the 60-mo follow-up (1.8 ± 0.7 and 1.6 ± 0.5, respectively) (P < 0.05) (Figure 1A). The NDI score was 43.4 ± 11.3 preoperatively, and improved greatly to 14.8 ± 7.7 at the 60-mo follow-up (P < 0.05) (Figure 1B). The NDI success or ≥ 15-point improvement in NDI at 60 mo postoperatively was 92.5%. JOA score was used to assess the restoration of cervical myelopathy. It was 10.8 ± 4.3 preoperatively, and slightly improved at 1 mo postoperatively (13.6 ± 4.9, P < 0.05), which continued to improve at the 12-mo follow-up (16.5 ± 5.2, P < 0.05) and maintained at the final follow-up (16.4 ± 5.8, P < 0.05) (Figure 1C).
Eight subscores of SF-36 were analyzed. All the subscores had an improvement at each follow-up interval compared to preoperation (P < 0.05) (Table 2). Based on Odom et al[13]’s criteria, 24 (60%) patients had excellent outcomes, 13 (32.5%) had good outcomes, and 3 (7.5 %) had fair outcomes. No one complained symptoms and signs unchanged or worsen.
| Preop | 1-mo | 6-mo | 12-mo | 24-mo | 60-mo | |
| Physical function | 54.1 ± 22.0 | 74.3 ± 21.2a | 77.5 ± 18.4a | 85.0 ± 24.2a | 84.4 ± 20.1a | 83.3 ± 22.1a |
| Role-physical | 47.5 ± 18.2 | 60.5 ± 20.3a | 66.3 ± 19.9a | 64.1 ± 21.0a | 64.8 ± 17.4a | 65.2 ± 18.4a |
| Bodily pain | 38.5 ± 12.6 | 70.0 ± 19.8a | 72.5 ± 21.3a | 67.5 ± 18.2a | 68.3 ± 16.4a | 67.3 ± 19.7a |
| General health | 41.1 ± 14.2 | 66.6 ± 18.4a | 72.5 ± 21.4a | 70.8 ± 15.1a | 69.3 ± 22.5a | 68.3 ± 23.4a |
| Vitality | 48.1 ± 19.3 | 68.6 ± 22.9a | 80.0 ± 16.3a | 67.5 ± 23.6a | 72.4 ± 21.4a | 70.4 ± 22.5a |
| Social function | 58.4 ± 21.0 | 77.1 ± 26.7a | 75.2 ± 19.8a | 81.3 ± 24.3a | 80.2 ± 20.7a | 81.2 ± 23.7a |
| Role-emotional | 37.2 ± 12.9 | 71.4 ± 14.3a | 73.5 ± 24.6a | 83.3 ± 23.1a | 79.3 ± 18.7a | 78.3 ± 15.7a |
| Mental health | 61.8 ± 18.6 | 75.1 ± 22.3a | 78.0 ± 19.4a | 82.2 ± 23.6a | 83.5 ± 19.2a | 84.5 ± 20.1a |
We analyzed radiographs of the 40 patients preoperatively and at 1-, 6-, 12-, 24-, and 60-mo postoperatively. The height of operated intervertebral space was 4.2 ± 1.2 mm preoperatively, and it restored to 6.0 ± 1.3 mm at 1 mo postoperatively (P < 0.05); at the final follow-up, it sustained at 5.2 ± 1.1 mm (P < 0.05). The average ROM of C2-C7 was 50.2° ± 14.6° preoperatively, which decreased to 44.8° ± 12.6° at the 1-mo follow-up (P < 0.05), then recovered to 48.2° ± 13.6° at the 6-mo follow-up (P > 0.05), and maintained at 49.2° ± 13.7° at the 60-mo follow-up (P > 0.05). The ROM of FSU was 8.7° ± 3.1° preoperatively, which decreased to 6.2° ± 2.8° at the 1-mo follow-up (P < 0.05), but recovered to 8.0° ± 2.5° at the final follow-up (P > 0.05) (Figure 2). For the upper and lower adjacent levels, the average ROM was 9.3° ± 4.0° and 8.5° ± 3.2° preoperatively, which decreased to 7.4° ± 3.8° and 7.1° ± 2.5° at the 3-mo follow-up (P < 0.05) and restored to 9.0° ± 3.1° and 8.8° ± 2.7° at the final follow-up (P > 0.05), respectively. There was no increase of upper and lower adjacent level ROM at each follow-up interval compared with those preoperatively (P > 0.05). The average ROM of C2-C7 left and right lateral bending was 27.9° ± 9.6° and 30.3° ± 10.2° preoperatively, decreased to 21.4° ± 5.9° and 22.6° ± 6.5° at the 1-mo follow-up (P < 0.05), and maintained at 26.3° ± 8.1°and 26.8° ± 7.7° at the 60-mo follow-up (P > 0.05). Correspondingly, the average ROM of FSU left and right lateral bending was 3.5° ± 1.6° and 3.4° ± 1.6° preoperatively, decreased to 1.5° ± 0.4° and 1.6° ± 0.5° at the 1-mo follow-up (P < 0.05), and decreased further (1.1° ± 0.3° and 1.0° ± 0.2°) (P < 0.05) at the final follow-up (Figure 2). At the final follow-up, cervical lordosis of C2-C7 alignment and FSU angle were improved to 16.5° ± 7.9° and 5.5° ± 1.5° from 10.3° ± 9.0° and 2.2° ± 1.6° preoperatively, respectively (P < 0.05; Table 3). The kappa values between Zou L and Liu XJ for radiology analyses were 0.937, which indicated excellent agreement.
| Preop | 1-mo | 6-mo | 12-mo | 24-mo | 60-mo | |
| C2-C7 ROM | 50.2 ± 14.6 | 44.8 ± 12.6a | 48.2 ± 13.6 | 48.9 ± 13.8 | 49.4 ± 14.4 | 49.2 ± 13.7 |
| FSU ROM | 8.7 ± 3.1 | 6.2 ± 2.8a | 8.0 ± 2.6 | 8.5 ± 2.7 | 8.3 ± 2.5 | 8.0 ± 2.5 |
| Upper adjacent level ROM | 9.3 ± 4.0 | 7.4 ± 3.8a | 9.5 ± 3.4 | 9.4 ± 3.2 | 9.1 ± 3.0 | 9.0 ± 3.1 |
| Lower adjacent level ROM | 8.5 ± 3.2 | 7.1 ± 2.5a | 7.9 ± 2.6 | 8.1 ± 2.7 | 8.4 ± 2.9 | 8.8 ± 2.7 |
| C2-C7 left lateral bending | 27.9 ± 9.6 | 21.4 ± 5.9a | 27.3 ± 7.8 | 25.6 ± 8.1 | 26.7 ± 7.8 | 26.3 ± 8.1 |
| C2-C7 right lateral bending | 30.3 ± 10.2 | 22.6 ± 6.5a | 28.8 ± 7.6 | 27.3 ± 8.5 | 27.5 ± 7.9 | 26.8 ± 7.7 |
| FSU left lateral bending | 3.5 ± 1.6 | 1.5 ± 0.4a | 1.4 ± 0.4a | 1.2 ± 0.3a | 1.2 ± 0.5a | 1.1 ± 0.3a |
| FSU right lateral bending | 3.4 ± 1.6 | 1.6 ± 0.5a | 1.6 ± 0.6a | 1.3 ± 0.4a | 1.2 ± 0.3a | 1.0 ± 0.2a |
| C2-C7 alignment | 10.3 ± 9.0 | 13.5 ± 7.6a | 14.5 ± 8.9a | 16.3 ± 9.4a | 15.9 ± 7.8a | 16.5 ± 7.9a |
| FSU angle | 2.2 ± 1.6 | 3.4 ± 1.2a | 4.5 ± 1.9a | 5.4 ± 1.7a | 5.3 ± 1.6a | 5.5 ± 1.5a |
| Intervertebral height | 4.2 ± 1.2 | 6.0 ± 1.3a | 5.8 ± 1.6a | 5.7 ± 1.4a | 5.5 ± 1.3a | 5.2 ± 1.1a |
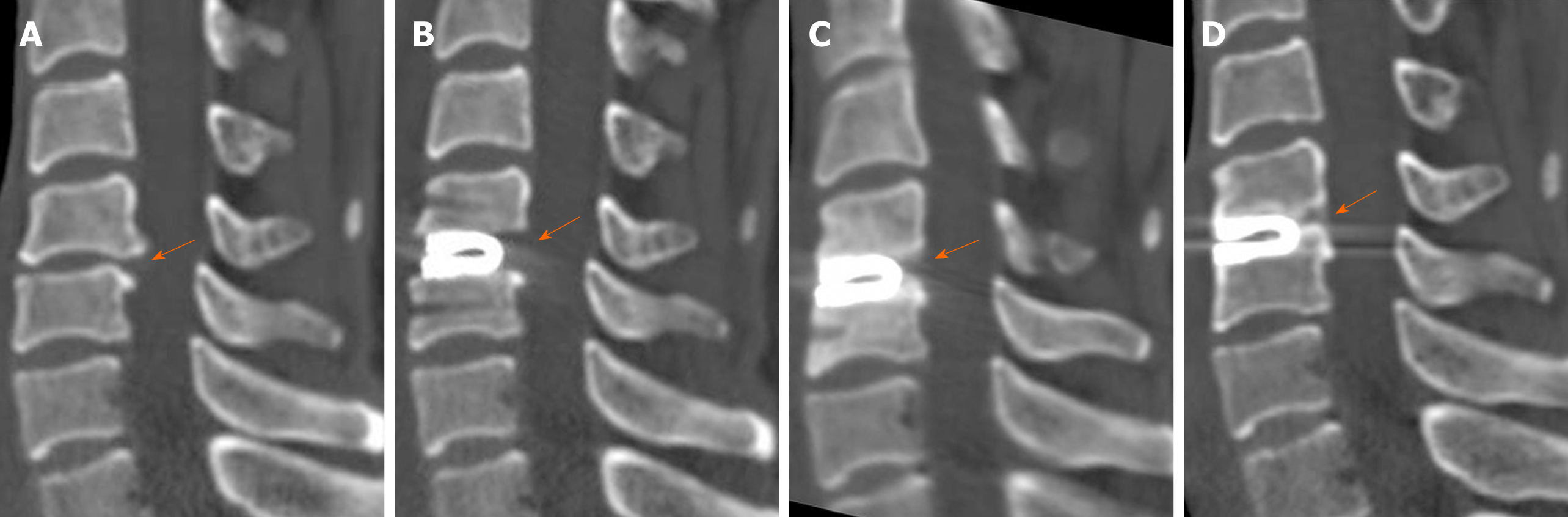
At the final follow-up, 12 (26.1%) implanted segments developed HO (Figure 3). According to Mehren et al[16]’s grading system, of the 46 implanted segments, grade I HO occurred in 5 (10.9%), grade II in 3 (6.5%), grade III in 3 (6.5%), and grade IV in 1 (2.2%). No postoperative neural deficit was observed. A total of four patients complained of dysphagia, which disappeared in two cases in 3 d, 1 case in 1 wk, and 1 case in 3 wk spontaneously. Eleven patients suffered mild to moderate neck and back pain, which relieved soon after taking nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxant drugs. Only one patient was found with 2 mm anterior migration of the prosthesis, with no symptoms at the 3-mo follow-up. No further migration was noted at the later follow-ups. No subsidence or device failure was observed. No patients received a secondary operation at the implanted segments or adjacent segments.
ACDF has been the gold standard treatment for patients experiencing cervical radiculopathy and/or myelopathy refractory to non-operative treatments. The safety and effectiveness of this procedure have been established and demonstrated in the previous literature. However, ACDF is associated with several peri- and post-operative complications, such as decreased ROM and adjacent segment dege
Unlike the plate-cage system of ACDF, the “U” shaped titanium DCI allows for flexion-extension mobility due to its unique architecture, thus it may not increase the ROM of adjacent segments to compensate for the ROM of global cervical spine. The DCI demonstrated favorable kinematics over ACDF at the adjacent levels. Matgé et al[11] conducted a prospective evaluation of 53 patients who underwent DCI stabilization. After 24-mo follow up, the mean ROM at upper and lower adjacent levels decreased by -1.7% and -4.1%. The biomechanical studies also indicated that the motion preservation of index-level of DCI produces a physiological distribution of ROM and strains at operative and adjacent levels, thus reducing the risk for developing ASD[12,19]. Our study gained similar results compared with the previous studies. The flexion-extension ROM of the operated level was maintained along the 5-year follow-up (8.0° ± 2.5° at the final follow-up vs 8.7° ± 3.1° before the surgery) except the 1-mo visit, which might be contributed to the neck pain and a strong protective mentation against normal neck motion at the early stage of operation for Chinese. As the ROM of the operated level was preserved, the segmental ROM of the upper and lower adjacent levels did not increase significantly at the last follow-up or any other follow-up intervals compared to that before surgery. At the last follow-up, we had not found any patient developing ASD. This result could be interpreted by the protection function of the motion preservation to the adjacent segment. As an alternative approach for treating cervical DDD to ACDF, DCI had the superiority of maintaining the kinematics of adjacent levels, thus preventing adjacent segment from accelerated degeneration.
C-ADR was popularized by neurosurgeons due to its segmental motion preservation meanwhile preventing adjacent segment degeneration from fusion[20]. C-ADR mimics the physiological motion of normal cervical disc to a great extent. However, some limitations such as hypermobility and increased loading of the index level were documented by some authors. Park et al[21] conducted a retrospective study to investigate the kinematics of four kinds of cervical disc prostheses. The ROM of the operated level in patients who received Mobi-C and Bryan prostheses increased at the last follow-up compared with preoperative values. DCI was designed to provide controlled extension and flexion, which is the primary motion mode in the subaxial cervical spine, and to limit the lateral bending and rotation. Thus, it put lesser strains at the index levels[12,19]. A finite element study conducted by Mo et al[19] compared the intact cervical configuration with single level DCI arthroplasty, C-ADR (Prodisc-C) and ACDF. The authors concluded that the DCI model produced a small increase of 7% ROM in flexion-extension, while there were 30% and 20% decreases in axial rotation and lateral bending. In C-ADR model, the ROM of flexion-extension increased by 108%, while 74% and 73% increases were observed during axial rotation and lateral bending. At the adjacent levels, up to 34% decrease occurred in C-ADR model and 17% decrease in DCI model. The capsular ligament strain of index level increased by 147% in Prodisc-C and by 13% in the DCI model. The radiological findings of our study were partially consistent with Mo et al[19]’s finite element investigation. The flexion-extension ROM of the operated level was decreased slightly but not significant at the last follow-up compared with that of preoperation, while Mo et al[19] found an increase by 7%. The left and right lateral bending of the operated level in our study decreased significantly (over 50%) at any follow-up intervals compared with that of preoperation, while Mo et al[19]’s finding demonstrated a 20% decrease. There must be a difference between finite element and in vivo study, but both of the findings indicated the controlled motion preservation in flexion-extension and limited lateral bending for DCI. The controlled or semi-constrained motion might not impose excessive strains on the facet joints of the operated level from over-motion of the disc prosthesis. Therefore, it acts as a protector for the facet joints especially for those with facet joint disease.
The scores of VAS, NDI, JOA, and the 8-dimensional SF-36 improved significantly at all follow-up intervals from pre-operation. And the rate of excellent to good results was 90.9%. The fairly good clinical results were attributed to the excellent neurological decompression and motion stability, which were comparable to C-ADR and ACDF[10,11]. There were four patients who suffered mild dysphagia after operation, which relieved spontaneously in several days to a few weeks. Dysphagia was a common complication for anterior cervical surgeries, often caused by using the hook retractor, intubation, and improper prosthesis implantation. There was no patient who received a second operation at the index or the adjacent levels. At the final follow-up, we observed no subsidence or failure of DCI.
Recently, concerns had arisen regarding the HO after cervical total disc replacement. HO had an adverse effect on the ROM of the operated level, which goes against the primary function of the motion preservation of the artificial disc replacement. According to the previous literature, the rate of HO occurrence varied from 17.8% to 69.6%. Although the reason is still unclear, several risk factors for HO formation were suggested, including blood and bone dust, carpentry, muscle trauma, number of operation level, and postoperative ROM at the operated level[22,23]. Kim and Heo[23] conducted a 5-year study of 23 patients who received single-level arthroplasty with Prodisc-C. Radiography and CT revealed that 16 (69.6%) patients developed HO at the operated segment. Hypermobility of the FSU and over-correction of the height of the operated segment may increase the formation of HO after C-ADR. Several studies reported the incidence of HO after DCI stabilization to be 22.3% to 35%, which seemed to be in a lower range than that in C-ADR popula
DCI implantation has more extensive indications than conventional cervical total disc prosthesis. First, DCI is a nonfusion prosthesis allowing controlled motion in flexion/extension while nearly blocking rotation and lateral bending. This spares the facet joint overload that has been observed with unconstrained C-cervical disc replacement (CDR). Thus, the patients with facet joints disease or degeneration are indicated for DCI but contraindicated for C-CDR. Second, the “U” shaped design of DCI had an anterior mouth higher than the posterior part and when implanted in the intervertebral space, it can restore the alignment of surgical segment from kyphosis to lordosis, which is contraindicated for C-CDR.
Our study has some limitations. First, this is a retrospective study without control group. However, the operations of the included patients were all conducted by Professor Liu H, which limited operation bias. Second, the sample size of this study is limited. Our study aimed to conduct a 5-year follow-up to investigate the long-term clinical and radiological results of DCI arthroplasty. Hence, some patients lost to follow-up were excluded.
DCI is a safe and effective non-fusion technique to treat cervical DDD. After DCI arthroplasty, the FSU lateral bending was limited, the segmental flexion-extension ROM could be partially preserved, and the ROM at adjacent level could be maintained. A longer prospective randomized controlled study is necessary to investigate the advantages and disadvantages of DCI over ACDF and C-ADR.
Dynamic cervical implant (DCI) stabilization has been reported to have satisfactory clinical and radiological results with short- and mid-term follow-up in the treatment of cervical degenerative disc disease.
Few reports about the clinical and radiological outcome with more than 5-year follow-up exist.
This is a 5-year follow-up study to investigate the long-term clinical and radiological results of DCI arthroplasty.
A total of 40 patients who received DCI arthroplasty were consecutively reviewed from May 2010 to August 2015. The clinical results and radiological outcomes were retrospectively analyzed.
The patients’ clinical results were significantly improved at the last follow-up. The functional spinal unit lateral bending was limited, the segmental flexion-extension range of motion could be partially preserved, and the range of motion at adjacent level could be maintained after DCI arthroplasty. At the last follow-up, 12 (26.1%) segments developed heterotopic ossification.
DCI arthroplasty is a safe and effective non-fusion technique to treat cervical degenerative disc disease in long-term follow-up.
In the future, we hope to conduct multicenter randomized controlled trials to compare the DCI implantation and cervical disc replacement with regard to clinical and radiological results.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mehren C S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1248] [Cited by in RCA: 1108] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 2. | Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976). 2005;30:2138-2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 267] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 3. | Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 730] [Cited by in RCA: 683] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 4. | Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 324] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 5. | Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1256] [Cited by in RCA: 1187] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 6. | Wang XF, Meng Y, Liu H, Hong Y, Wang BY. Surgical strategy used in multilevel cervical disc replacement and cervical hybrid surgery: Four case reports. World J Clin Cases. 2020;8:3890-3902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R, Pointillart V. Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine (Phila Pa 1976). 2003;28:2673-2678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 247] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 8. | Parkinson JF, Sekhon LH. Cervical arthroplasty complicated by delayed spontaneous fusion. Case report. J Neurosurg Spine. 2005;2:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Wang L, Song YM, Liu LM, Liu H, Li T. Clinical and radiographic outcomes of dynamic cervical implant replacement for treatment of single-level degenerative cervical disc disease: a 24-month follow-up. Eur Spine J. 2014;23:1680-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Liu S, Song Y, Liu L, Wang L, Zhou Z, Zhou C, Yang X. Clinical and radiologic comparison of dynamic cervical implant arthroplasty and cervical total disc replacement for single-level cervical degenerative disc disease. J Clin Neurosci. 2016;27:102-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Matgé G, Berthold C, Gunness VR, Hana A, Hertel F. Stabilization with the Dynamic Cervical Implant: a novel treatment approach following cervical discectomy and decompression. J Neurosurg Spine. 2015;22:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Welke B, Schwarze M, Hurschler C, Book T, Magdu S, Daentzer D. In vitro investigation of a new dynamic cervical implant: comparison to spinal fusion and total disc replacement. Eur Spine J. 2016;25:2247-2254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 361] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976). 2000;25:2072-2078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 336] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 15. | Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] |
| 16. | Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976). 2006;31:2802-2806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 185] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 17. | Zhang HX, Shao YD, Chen Y, Hou Y, Cheng L, Si M, Nie L. A prospective, randomised, controlled multicentre study comparing cervical disc replacement with anterior cervical decompression and fusion. Int Orthop. 2014;38:2533-2541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Sasso RC, Best NM. Cervical kinematics after fusion and bryan disc arthroplasty. J Spinal Disord Tech. 2008;21:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Mo ZJ, Zhao YB, Wang LZ, Sun Y, Zhang M, Fan YB. Biomechanical effects of cervical arthroplasty with U-shaped disc implant on segmental range of motion and loading of surrounding soft tissue. Eur Spine J. 2014;23:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Quan GM, Vital JM, Hansen S, Pointillart V. Eight-year clinical and radiological follow-up of the Bryan cervical disc arthroplasty. Spine (Phila Pa 1976). 2011;36:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Park SB, Kim KJ, Jin YJ, Kim HJ, Jahng TA, Chung CK. X-Ray-based Kinematic Analysis of Cervical Spine According to Prosthesis Designs: Analysis of the Mobi C, Bryan, PCM, and Prestige LP. J Spinal Disord Tech. 2015;28:E291-E297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Lei T, Liu Y, Wang H, Xu J, Ma Q, Wang L, Shen Y. Clinical and radiological analysis of Bryan cervical disc arthroplasty: eight-year follow-up results compared with anterior cervical discectomy and fusion. Int Orthop. 2016;40:1197-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Kim KS, Heo DH. Do Postoperative Biomechanical Changes Induce Heterotopic Ossification After Cervical Arthroplasty? Clin Spine Surg. 2016;29:E309-E313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Dostal M, Kaech DL. Radiologic and Clinical Evaluation 12 Months after Anterior Cervical Diskectomy and Dynamic Stabilization of the Segment with Dynamic Cervical Implant. J Neurol Surg A Cent Eur Neurosurg. 2016;77:474-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |