Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3796
Peer-review started: January 23, 2021
First decision: February 8, 2021
Revised: February 10, 2021
Accepted: March 24, 2021
Article in press: March 24, 2021
Published online: June 6, 2021
Processing time: 110 Days and 18.3 Hours
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is spreading at an alarming rate, and it has created an unprecedented health emergency threatening tens of millions of people worldwide. Previous studies have indicated that SARS-CoV-2 ribonucleic acid could be detected in the feces of patients even after smear-negative respiratory samples. However, demonstration of confirmed fecal-oral transmission has been difficult. Clinical studies have shown an incidence rate of gastrointestinal (GI) symptoms ranging from 2% to 79.1% in patients with COVID-19. They may precede or accompany respiratory symptoms. The most common GI symptoms included nausea, diarrhea, and abdominal pain. In addition, some patients also had liver injury, pancreatic damage, and even acute mesenteric ischemia/thrombosis. Although the incidence rates reported in different centers were quite different, the digestive system was the clinical component of the COVID-19 section. Studies have shown that angiotensin-converting enzyme 2, the receptor of SARS-CoV-2, was not only expressed in the lungs, but also in the upper esophagus, small intestine, liver, and colon. The possible mechanism of GI symptoms in COVID-19 patients may include direct viral invasion into target cells, dysregulation of angiotensin-converting enzyme 2, immune-mediated tissue injury, and gut dysbiosis caused by microbiota. Additionally, numerous experiences, guidelines, recommendations, and position statements were published or released by different organizations and societies worldwide to optimize the management practice of outpatients, inpatients, and endoscopy in the era of COVID-19. In this review, based on our previous work and relevant literature, we mainly discuss potential fecal-oral transmission, GI manifestations, abdominal imaging findings, relevant pathophysiological mechanisms, and infection control and prevention measures in the time of COVID-19.
Core Tip: Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 has led to an unprecedented global public health crisis. Based on our previous work and the relevant literature, the aim of this review is to discuss mainly the current status and progress, the problems that have been resolved and those that remain to be resolved, and the future research directions in the field of COVID-19 and the digestive system, with special focus on potential fecal-oral transmission, gastrointestinal manifestations, abdominal imaging, pathophysiological mechanisms, and infection control and prevention measures in outpatient visits, inpatient ward, and endoscopy centers in the time of COVID-19.
- Citation: Wang MK, Yue HY, Cai J, Zhai YJ, Peng JH, Hui JF, Hou DY, Li WP, Yang JS. COVID-19 and the digestive system: A comprehensive review. World J Clin Cases 2021; 9(16): 3796-3813
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3796.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3796
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has led to an unprecedented global public health crisis since December 2019[1]. As of March 16, 2021, 119218587 confirmed cases of COVID-19 patients have been reported with 2642673 deaths in 212 countries globally[2]. Although respiratory symptoms, such as cough and dyspnea, are the most prominent clinical presentations in COVID-19 patients; extra-pulmonary manifestations, including gastrointestinal (GI) problems, such as nausea, diarrhea, and vomiting, are now being increasingly reported, occasionally even as the initial symptom[3-5]. A previous study has shown that the clinical investigation of disease onset has been underestimated, especially in terms of GI symptoms, and COVID-19 patients presenting with GI symptoms as initial symptoms need a longer duration of viral shedding and hospitalization than patients presenting with pulmonary symptoms[6]. Additionally, SARS-CoV-2 enters the host cells via the interaction of the viral spike (S) protein with the human angiotensin-converting enzyme 2 (ACE2) receptor, and ACE2 is abundantly expressed in the small intestine and lung epithelium, indicating routes of efficient coronavirus infection through the airway and GI tract in humans[3,7,8]. In this review, we mainly discuss potential fecal-oral transmission, GI manifestations, pathophysiological mechanisms, and infection control and prevention measures.
SARS-CoV-2 RNA was first detected in a stool specimen from the first reported COVID-19 patient in the United States[9]. Later, numerous studies found that fecal samples of hospitalized patients were positive for SARS-CoV-2, including those with or without GI symptoms[10,11]. Based on the current research, SARS-CoV-2 RNA has been detected in 29%-55% of stool samples from COVID-19 patients[12,13]. More importantly, Xiao et al[14] isolated infectious SARS-CoV-2 from stool samples, confirming the release of the infectious virus into the GI tract, and showed that the ACE2 protein was abundantly expressed in the glandular cells of gastric, duodenal, and rectal epithelia, supporting the entry of SARS-CoV-2 into the host GI tract cells. Cheung et al[11] found that GI symptoms were present in 17.6% of COVID-19 patients, and viral shedding in stool was detected in 48.1% of patients and could persist for up to 33 d from the illness onset even after negative viral RNA in respiratory specimens. van Doorn et al[15] also found that detection of the infectious virus in stool samples or anal swabs can persist long after negative respiratory testing and drew a conclusion that stool sample or anal swab testing should be considered while isolating or discharging a patient. Our published data[16] showed that anal swab positives but throat swab negatives were observed in two of the seven turn-positive patients, indicating that fecal-oral transmission and environmental contamination should not be ignored in patients with SARS-CoV-2. Xie et al[17] compared the positive proportion of SARS-CoV-2 nucleic acid amplification test results from different samples, including oropharyngeal swab, blood, urine, and stool, and found that the positive proportion was about 40% using stool samples or oropharyngeal swab samples. Zhang et al[18] found that 35.7% of the confirmed patients had a positive stool sample for SARS-CoV-2 nucleic acid, and nucleic acid detection of COVID-19 in fecal specimens was as accurate as that in pharyngeal swab specimens. To avoid missed diagnosis in positive patients, diagnostic tests with higher specificity and sensitivity are urgently needed, and combination of computed tomography scans and nucleic acid detection may also be a choice[17]. Additionally, the demonstration of confirmed fecal-oral transmission is difficult, as researchers need to control for respiratory droplet exposure, which may be difficult in a clinical setting. However, more studies are needed to understand the potential role of fecal-oral transmission in the current pandemic, as it may affect the isolation recommendations and prevention and control measures[19].
The main manifestations of COVID-19 patients were fever and/or respiratory symptoms, but studies also showed that about 2%-79.1% of patients had GI symptoms[10,20-23]. These symptoms can appear at the beginning of the disease, even before the onset of fever and respiratory tract symptoms. The most common GI symptoms include decreased appetite, nausea and vomiting, diarrhea, and abdominal pain. Severe patients may have GI bleeding. Based on existing literature and reports, GI manifestations of SARS-CoV-2 are still emerging and variant, and there are no specific symptoms and signs in COVID-19 patients. In addition to the above GI symptoms, some patients also had liver injury, pancreatic damage, and even acute mesenteric ischemia/thrombosis. Although the incidence rates reported in different centers were quite different, the digestive system was the clinical component of the COVID-19 section.
A series of studies have consistently reported GI symptoms among COVID-19 patients. In the cohort of 140 COVID-19 patients in Wuhan, GI symptoms included nausea in 24 (17.3%), vomiting in seven (5.0%), and diarrhea in 18 (12.9%) patients; however, abdominal pain or discomfort was only reported in 2.2%-5.8% of patients[24]. A large study in China that collected data of 1099 patients from 552 hospitals reported nausea or vomiting in 55 (5.0%) and diarrhea in 42 (3.8%) patients[20]. Several other cohorts reported frequencies of diarrhea ranging from 2.0%-10.1% and nausea and/or vomiting ranging from 1.0%-10.1%[10,20-24]. Tian et al[25] analyzed the available studies (from the end of December 2019 to the end of February 2020) and found a variable incidence: Vomiting (3.6%-66.7%), nausea (1%-29.4%), anorexia (39%-50.2%), diarrhea (2%-49.5%), GI bleeding (4%-13.7%), and abdominal pain (2.2%-6.0%). However, in a recent review, 26 studies were included to analyze the prevalence of GI symptoms, and it was found that the prevalence of nausea and vomiting, diarrhea, abdominal pain, and anorexia was 7%, 8%, 3%, and 17%, respectively[26]. In addition, belching and constipation were also reported in COVID-19 patients[27,28].
Nausea had an acute onset, and it was an early warning of a problem in the upper digestive tract and a component of the body’s epithelial defenses, which indicated nausea may be the first indication of GI infection by SARS-CoV-2. This may be a serious omission as nausea and vomiting can be the presenting symptoms, as exemplified by the first cases of COVID-19 in the United States and China[9,23]. Andrews et al[29] analyzed 41 studies including more than 2000 COVID-19 patients and showed that the median incidence of nausea was 10.5% and that of diarrhea was 11%. These findings supported the view that nausea and diarrhea should be given equal importance as symptoms of SARS-CoV-2 infection. To date, there are scarce data on the temporal pattern of nausea and vomiting during the course of the disease[30,31]. Most published studies have only reported the presence or absence of nausea and vomiting while not taking their severity into consideration. More attention should be paid to recognizing nausea as a potential early symptom of COVID-19, as revealed by the epidemiological data.
Diarrhea was another common GI symptom of COVID-19 patients. Diarrhea mostly occurred within 1-8 d after onset, with a median of 3.3 d; the duration was 1-14 d, with an average of 4.1 ± 2.5 d in COVID-19 patients. The frequency of diarrhea was 3.3 times, and occasionally it even reached nine times a day. Watery stool accounted for 34.3%[32]. Jin et al[23] showed that the incidence of critical cases in patients with digestive system symptoms was significantly higher than that in patients without digestive system symptoms (22.97% vs 8.14%, P < 0.001), and 8.6% of patients had diarrhea on admission. Median duration of diarrhea was 4 d, and most of the patients had self-limiting symptoms. Stool cultures were negative in all patients, and there were no fecal leukocytes. Recently, an analysis of 43 studies including 10676 COVID-19 patients summarized that the pooled prevalence of diarrhea symptoms was 7.7%; and the pooled prevalence of diarrhea in studies from other countries was much higher at 18.3% in comparison to that in the study from China, where the prevalence was 5.8%. Meanwhile, the pooled prevalence in hospitalized patients was slightly higher at 10.4% compared with that in outpatients at 4.0%, and the pooled prevalence of diarrhea, as one of the initial symptoms in hospitalized COVID-19 patients from 33 studies, was 9.3%[33]. Another study in 175 hospitalized patients reported that 19.4% of patients had diarrhea, with symptom duration ranging from 1-4 d, with an average of six times per day[34]. Wang et al[22] reported that 14 of 138 hospitalized patients presented with diarrhea and nausea 1-2 d before the development of fever and dyspnea. Luo et al[35] found that 183 of 1141 (16%) patients presented with GI symptoms in the absence of respiratory symptoms (sometimes diarrhea as the only presenting symptom), while the majority of patients (96%) had lung infiltrates on chest computed tomography. Fang et al[32] showed that the incidence of new diarrhea (excluding diarrhea caused by adverse drug reactions) was 22.2%, while that after antiviral drugs was about 55.2%. Lin et al[10] found that 24% of patients had diarrhea, while only 5.2% of patients had diarrhea on admission. Most of the patients developed diarrhea during hospitalization, owing to medications or other treatments. For instance, antibiotics can cause intestinal microecological imbalance and lead to antibiotic-associated diarrhea[10].
Abdominal pain was another common GI symptom, and it was variably described as stomach ache, epigastric pain, and abdominal discomfort, without any further details regarding the quality or nature of pain[10,23,25,26,30,31]. The pooled prevalence of abdominal pain was 3.6% in an analysis of 15 studies including 4031 COVID-19 patients[33]. A subgroup analysis demonstrated a slightly higher pooled prevalence of 5.3% in patients from regions besides China compared with 2.7% of patients from China[33].
In brief, to understand more accurately the true prevalence of digestive symptoms in COVID-19 patients, it is critical to systematically collect the following information: Onset of nausea and vomiting, diarrhea, abdominal pain; duration of symptoms; and documentation of whether and how long GI symptoms precede the upper respiratory infection symptoms.
Except for GI symptoms, such as diarrhea, nausea, and vomiting, liver injury was observed in a substantial proportion of COVID-19 patients and it was worthy of our attention[36]. Most of the cases reported had mildly elevated levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and lactate dehydro
Several studies have reported about the association between the presence of abnormal liver function and severity of disease or outcomes, and they have declared that liver injury was associated with high risk of admission as well as higher risk of intensive care unit admission and/or death[10,43-45]. As liver biochemical indicators are closely related to the severity and prognosis of COVID-19 patients, measurement of these liver biochemical parameters might assist clinicians to evaluate the prognosis of COVID-19[46,47]. We also suggest checking the baseline liver function markers in all patients on admission and monitoring throughout hospitalization, particularly in patients undergoing drug therapy for COVID-19 associated with potential hepato
The etiology of liver injury may include viral immunologic injury, drug-induced liver injury, the systemic inflammatory response, hypoxic hepatitis, and the exacerbation of preexisting liver disease[50]. For instance, electron microscopic analyses of liver samples from two deceased COVID-19 patients with liver dysfunction demonstrated the presence of viral particles in the cytoplasm of hepatocytes[51]. Moreover, SARS-CoV-2 virions in vessel lumens and endothelial cells of portal veins in COVID-19 liver specimens were found using in situ hybridization[52]. The mechanism of liver injury may be complicated, including direct cytotoxicity from active viral replication of SARS-CoV-2 in the immune-mediated liver damage due to a severe inflammatory response, vascular changes due to coagulopathy, endotheliitis from right heart failure, hypoxic changes induced by respiratory failure, drug-induced liver injury, and exacerbation of underlying liver disease[40]. More detailed and crucial questions, such as which molecular processes are dysregulated by the infection and what is the real factor of direct cytopathic effects, hypoxia, or cytokine storm in hepatic dysfunction, need to be answered by performing further research.
Studies have demonstrated that ACE2, the receptor of SARS-CoV-2, was expressed in the pancreas[53-56]. Despite this, little attention has been paid to the extent and details of pancreatic injury caused by COVID-19[53]. Fortunately, so far, an increasing number of studies have reported pancreatic injury in patients with COVID-19 infection, which received the attention of clinicians and researchers[57-62]. Combined with clinical data, Liu et al[53] showed that 1%-2% of non-severe and 17% of severe patients with COVID-19 had pancreatic injury. Some critically ill patients already had developed pancreatic injury before admission. The possibility of drug-induced pancreatitis, the consequences of pancreatic injury such as aggravating systemic inflammation, accelerating the occurrence of acute respiratory distress syndrome, and even developing into chronic pancreatitis, which may have a serious impact on the health and quality of life of patients, should be considered. Akarsu et al[63] reported that the presence of pancreatic damage triggered by SARS-CoV-2 could deteriorate the clinical condition of patients, and the mortality rate may increase in these patients. Wang et al[64] also reported that the incidence of pancreatic injury was 17% in patients with COVID-19 pneumonia. Using several methodologies, Fignani et al[56] showed that ACE2 was highly expressed in pericytes in the pancreatic microvasculature and insulin producing beta-cells. Pancreatic injuries or even acute pancreatitis may develop during SARS-CoV-2 infection, especially in those with pre-existing diabetes mellitus. Monitoring of pancreatic enzymes was suggested in COVID-19 patients, especially in those with pre-existing diabetes mellitus[65]. Simou et al[58] also reported a patient diagnosed with acute pancreatitis associated with SARS-CoV-2, and they suggested that serum levels of amylase and lipase enzymes should be tested in all patients with COVID-19, even in asymptomatic subjects. Nevertheless, Bansal et al[66] found that serum amylase or lipase did not correlate with the severity of COVID-19 or its mortality; and the prevalence of hyperamylasemia in patients with COVID-19 was 33%, while that of elevated lipase was 24.1%. Additionally, Suchman et al[60] showed that pancreatitis may occur in pediatric patients with COVID-19. Based on the above-mentioned studies, more research may be needed to investigate whether more elevated amylase and lipase levels are associated with a more severe course of this specific virosis.
Cheung et al[67] described the first presumptive case of COVID-19-associated acute superior mesenteric artery thrombosis and acute intestinal ischemia. Macrovascular arterial/venous thrombosis was reported in almost half of COVID-19 patients with bowel ischemia. Overall mortality in COVID-19 patients with GI ischemia and radiologically evident mesenteric thrombotic occlusion was 38.7% and 40%, retrospectively[68]. Thromboembolic complications of COVID-19 should not be ignored, as coagulation dysfunction was one of the major causes of death in patients with severe COVID-19 infection. Clinicians managing patients with suspected or confirmed SARS-CoV-2 infection should monitor their potential late complications, as delayed diagnosis can lead to increased morbidity and mortality[67]. Norsa et al[69] also suggested that a high level of suspicion for intestinal ischemia should be maintained in COVID-19 patients presenting with GI symptoms or with arising abdominal pain because this complication could account for an increase mortality risk. Paul et al[70] discussed a case of severe COVID-19 pneumonia, developing ischemic colitis, for several reasons, including hypercoagulable state, coagulopathy leading to thromboembolic complications, and use of vasopressors in severely ill patients with hemodynamic compromise. Singh et al[71] conducted a rapid review of the current scientific literature available in PubMed to identify cases of acute mesenteric ischemia (AMI) in COVID-19 patients, and they summarized the clinical characteristics of COVID-19 patients with AMI. A total of 13 cases were found. Of these, six patients had pre-existing comorbidities, while seven patients had no comorbidities. Abdominal pain, nausea, and vomiting were the main common symptoms of these patients. The diagnosis of AMI was made by contrast-enhanced computed tomography. Ten patients underwent surgery, and three patients received conservative management. Out of these 13 patients, four patients died. The pathological mechanism may include the following: Direct invasion of the bowel tissue by the virus resulting in expression of ACE2 on enterocytes; viral infection of the endothelial cells leading to diffuse endothelial inflammation or increased procoagulant factors, like factor VIII, von Willebrand factor, and fibrinogen; virus-induced cytokine storm leading to coagu
Abdominal venous thrombosis, such as the superior mesenteric vein (SMV) thrombosis, was also reported. Recently, a 29-year-old male construction worker from India was reported to present with left-sided colicky abdominal pain without any acute respiratory symptoms[76]. A retrospective cross-sectional study revealed bowel-wall abnormalities, such as bowel wall thickening and pneumatosis, in 31% of the CT scans, and signs of late ischemia in 20% of CT scans of intensive care unit (ICU) patients (2.7% of ICU patients), for which the established etiology was small-vessel arterial thrombosis[77]. Hence, early evaluation of abdominal vessels in COVID-19 patients who present with any abdominal symptoms should be considered, especially in those who have an elevated D-dimer level. Early treatment of thrombosis with low-molecular-weight heparin can have a significant impact on the therapeutic outcome. In addition to anticoagulants, other therapies, such as anticomplement and interleukin (IL)-1 receptor antagonists, need to be explored, and other new agents should be discovered as they emerge from our better understanding of the pathogenetic mechanisms[75].
A systematic review identified 36 primary studies addressing the GI symptoms and radiologic manifestations of SARS-CoV-2 infection and showed that typical GI findings included non-specific small and large bowel wall thickening and liquid stool throughout the bowel and other more rare presentations included pneumatosis intestinalis, pneumoperitoneum, and large volume ascites. Identifying these features on abdominal imaging also highlight the need to consider and evaluate for other manifestations of COVID-19 such as lung parenchymal findings[78]. In a recent retrospective cross-sectional study, 34% of inpatients had GI symptoms at admission, CT was most commonly performed for abdominal pain or sepsis, and ultrasound was most frequently performed for elevated liver enzyme levels. Bowel wall abnormalities were shown on 31% of the CT scans, such as bowel wall thickening and pneumatosis. Ultrasound examinations were mostly performed because of liver laboratory findings (87%, 32 of 37), and 54% (20 of 37) revealed a dilated sludge-filled gallbladder, suggestive of bile stasis[77]. Bowel abnormalities and gallbladder bile stasis were common findings on abdominal images of COVID-19 patients. Patients who underwent laparotomy often had ischemia, possibly due to small-vessel thrombosis[77]. Another retrospective study included 81 COVID-19 patients with abdominal CT, and 45 (55%) had positive abdominopelvic findings. The most common abdominal imaging features were intestinal imaging findings (24%), including colorectal (5%) and small bowel thickening (12%), intestinal distension (18%), pneumatosis (1%), and intestinal perforation (1%)[79]. Morparia et al[80] reported abdominal imaging findings in critically ill children admitted with multisystem inflammatory syndrome associated with COVID-19. Hepatomegaly, nephromegaly, gallbladder wall edema, ascites, intestinal inflammation, and mesenteric lymphade
Due to the risk of direct exposure, non-essential endoscopic procedures should be cancelled, and only emergency endoscopies were permitted[83]. Xiao et al[14] showed that no abnormalities were observed in the stomach, duodenum, colon, and rectum, with the exception of mucosa damage in the esophagus at endoscopy. Histology showed numerous infiltrating plasma cells and lymphocytes as well as interstitial edema in the laminapropria of the stomach, duodenum, and rectum. However, a recent cohort of 95 COVID-19 patients reported an additional six cases who underwent endoscopy examination, revealing esophageal bleeding with erosions and ulcers in one severe patient. SARS-CoV-2 RNA was detected in esophagus, stomach, duodenum, and rectum specimens for two severe patients. In contrast, only duodenum was positive in one of the four non-severe patients[10]. Endoscopic diagnosis and treatment has been served as an indispensable part in the management of severe COVID-19 cases, as placing jejunal nutrition tubes in these patients to improve their overall nutritional status and performing emergency bedside endos
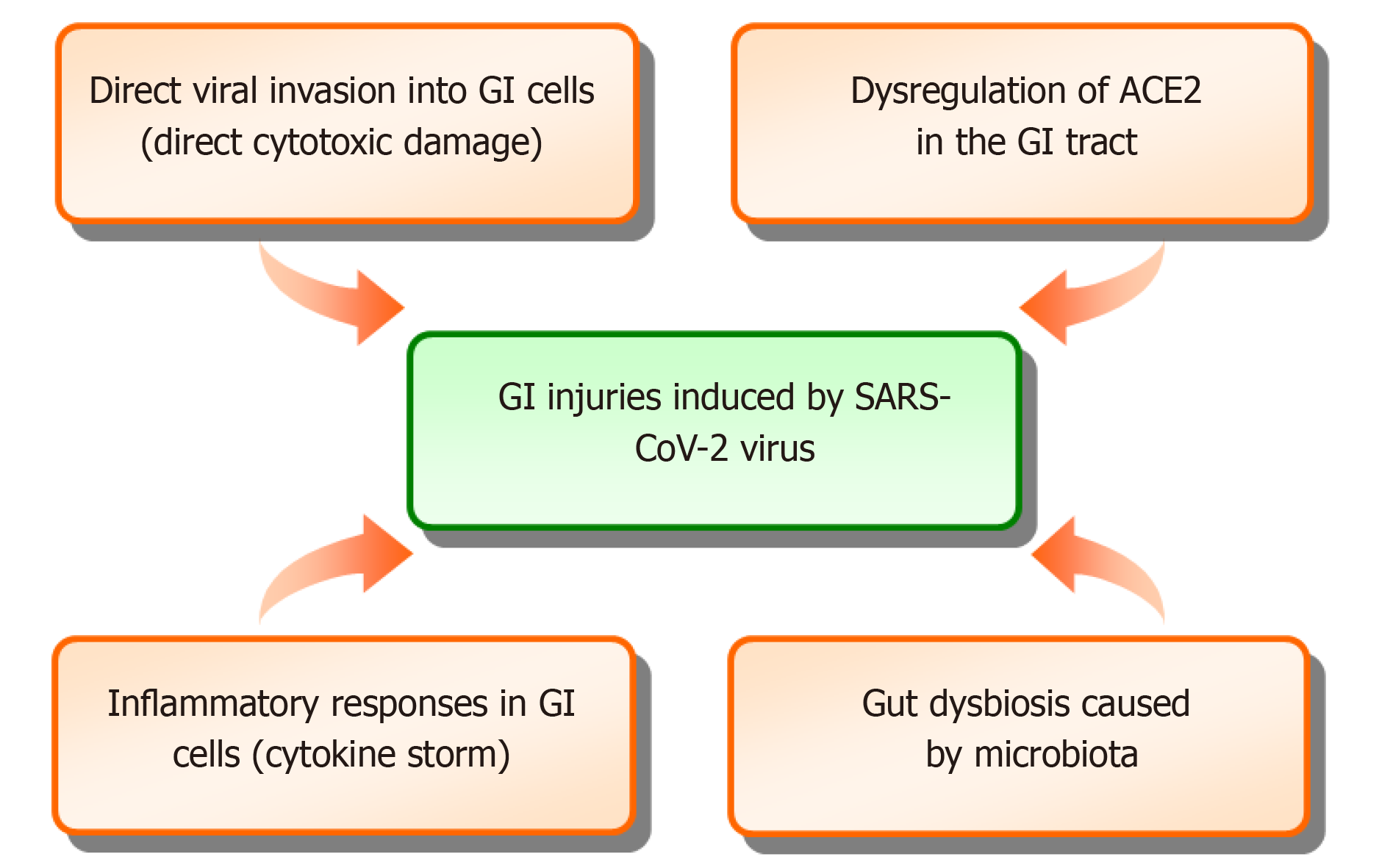
Studies have demonstrated that SARS-CoV-2 enters into host cells by binding to the ACE2 receptor more tightly than SARS, resulting in COVID-19[85,86]. The ACE2 receptor is highly expressed in type 2 alveolar cells, causing pulmonary infection. However, abundant expressions of ACE2 have been found in epithelial cells throughout the GI tract, such as stomach, duodenum, ileum, and colon[14,87]. Recent studies have shown that the detailed mechanisms of digestive tract infection are referred to as direct viral invasion into target cells, dysregulation of ACE2, immune-mediated tissue injury, and gut dysbiosis caused by microbiota[14,25,87,88] (Figure 1).
It has been found that positive staining of ACE2 is rarely present in the esophageal epithelium, but ACE2 is abundantly expressed in the cilia of glandular epithelia, which is mainly distributed in the cytoplasm of the digestive epithelial cells[14]. Consistent with the findings of ACE2 staining, in COVID-19 patients, the presence of viral nucleocapsid protein has been observed in the cytoplasm of gastric, duodenal, and rectal glandular epithelial cells, apart from the esophagus[14]. Pathological examination demonstrates the presence of SARS-CoV-2 in the epithelial cells of the GI tract, leading to the detection of the viral nucleic acid in fecal samples. In addition, the proteases, including transmembrane serine protease 2, cleaves the spike protein of SARS-CoV-2 binding to ACE2, essential for virus entry into the recipient cell[8,89,90]. SARS-CoV-2 RNA is then released into the cytoplasm, and viral replication is initiated. Notably, Basigin/CD147, another host receptor of SARS-CoV-2, is present on human oocytes, blastocysts, and ocular surface[89,91], but its expression in digestive cells is not clear. However, ACE2 is generally recognized as the primary receptor of SARS-CoV-2, triggering the virus entry into the host cell.
Attachment of the virus to ACE2 leads to the downregulation of ACE2, which mediates the involved signal pathways to regulate the intestinal functions[92]. ACE2 mediated dysregulation of sodium-dependent glucose transporter (SGLT) in the intestinal epithelium may be associated with the mortality of COVID-19 patients with diabetes[90]. Moreover, ACE2 regulating the renin-angiotensin-aldosterone system may be important in the pathogenesis of chronic liver disease, but direct cytotoxic damage caused by SARS-CoV-2 in the liver is still questionable[93,94]. ACE2 also exhibits a renin-angiotensin-aldosterone system-independent effect as a regulator of amino acid transport, particularly tryptophan, to regulate amino acid homeostasis in the intestine[93,94]. Thus, SARS-CoV-2 directly invades into the digestive system via binding to ACE2 or CD147 and then replicates in the recipient cells and regulates the involved signaling pathways, resulting in GI dysfunction.
Previous studies have suggested that excessive host immune responses play an important role in the pathogenesis of COVID-19[14,88], similar to SARS[95] and influenza infections[96]. In early studies, higher levels of proinflammatory cytokines and chemokines in plasma are found in patients with COVID-19, resulting in a probable “cytokine storm”[97-99]. Compared with the non-ICU patients, the ICU patients have higher concentrations of proinflammatory mediators, such as IL-2, IL-7, IL-10, and tumor necrosis factor α, in plasma[97]. Another recent study has shown abnormally increased CRP and IL-6 in both COVID-19 and other pneumonia patients, but there was no difference between the two groups[98]. Moreover, from a patholo
Both direct cytotoxic damage and dysregulation of ACE2 influence the intestinal epithelium function. However, recent studies have revealed that SARS-CoV-2 infection can alter the intestinal microbiota in COVID-19 patients, characterized by the enrichment of pathogenic microbes and opportunistic pathogens, resulting in gut dysbiosis[100-105]. As described previously, the absorption of tryptophan is associated with neurological abnormities, as it is the precursor for the synthesis of 5-hydroxytryptophan in the brain[103]. It also regulates the levels of antimicrobial peptides that affect the composition of the gut microbiota, leading to increased sensitivity to intestinal inflammation and epithelial dysfunction[106]. Thus, this viral infection might affect the homeostasis of the gut-brain axis through the intestinal microbiota[103,107]. However, further investigations are needed to clarify whether the dysbiosis is specific to SARS-CoV-2 infection or a consequence of critical illness.
Currently, there is no specific treatment for COVID-19, and scarce literature is available on the treatment of GI symptoms. No evidence is available on the efficacy of antidiarrheal drugs, but adequate rehydration and electrolyte monitoring may be performed in all patients with diarrhea. COVID-19 patients with diarrhea can be mostly treated with montmorillonite powder or probiotics[108]. Berberine and some other TCM have been suggested in China for the treatment of general COVID-19, but they might need further clinical trials[109]. Antibiotics and antivirals were often used for COVID-19 treatment, which could cause diarrhea and likely alteration of the gut microbiota[110,111]. However, a rapid improvement in diarrhea was also found after using antiviral therapy[4]. Intestinal microbiota played an important role in maintaining the balance of the GI microecological environment. China’s National Health Commission recommended that patients with diarrhea and severe COVID-19 could be treated by probiotics to preserve the intestinal balance and prevent secondary bacterial infections[108]. Therefore, probiotics are recommended to maintain the intestinal microecological balance; however, further evidence is needed. To date, there is scarce literature on the treatment of liver injury. Zhang et al[39] suggested that liver damage in mild cases of COVID-19 was often transient and can return to the normal level without any special treatment, and liver protective drugs were usually given when severe liver damage occurred. Unfortunately, specific medications for liver protection were not described in that study.
Outpatient visits and inpatient ward
Nosocomial transmission of SARS-CoV-2 has been reported during the early stage of the COVID-19 outbreak[22]. To reduce patient aggregation and avoid cross-infection, it has been suggested to use the appointment system, time-divided diagnosis, and time-divided treatment[112]. The outpatient visits could be booked through a telephone triage[113]. Reception of inpatients could be conditional based on a negative swab for COVID-19 obtained with a drive-in procedure. Healthcare professionals and administrative staff should take suitable precautions to protect themselves, including wearing proper personal protective equipment (PPE) and should be restricted and monitored with the use of periodic swabs[113]. Significant environmental contamination by patients with SARS-CoV-2 through respiratory droplets and fecal shedding suggested that the environment was a potential medium of transmission, and environmental and hand hygiene was important[114]. The ward should strengthen ventilation and disinfect the surfaces frequently contacted by patients every day[112]. Placing patients in accommodation isolated from those without infection, hand hygiene, wearing of appropriate PPE, and thorough environmental cleaning and disinfection were demonstrated to be effective interventions in preventing the spread of SARS-CoV-2 in the hospital[115]. These measures implemented may not be universally applicable in every hospital. Nonetheless, these infection control methods were practically executed and could be referenced or modified to fit each hospital's unique condition[116,117].
Due to the main routes of droplet and contact transmission, SARS-CoV-2 has been found in the GI secretions and asymptomatic carrier transmission, and endoscopy centers were considered to be high-risk areas for exposure to COVID-19[118,119]. All endoscopies should be considered as aerosol-generating procedures, and they can lead to subsequent airborne transmission. It was recommended to cancel non-essential endoscopic procedures, and only emergency endoscopies were permitted[83]. However, postponement of elective endoscopy conditionally in inflammatory bowel disease patients may harbor potential risks, such as increasing the risk of high-grade dysplasia and colorectal cancer diagnosis[120]. Thorough screening of incoming patients, separation of diagnostic and treatment areas, regional management, hierarchical protection, disinfection protocols, and other measures were enforced to prevent virus transmission during endoscopic treatments[121]. Hamid et al[122] suggested that fecal testing for SARS-CoV-2 should be performed in patients undergoing elective lower GI endoscopy. Pre-endoscopy COVID-19 testing has now become the norm; however, pre-procedural universal testing has some advantages and disadvantages[123].
Numerous guidelines, recommendations, or position statements were released by different organizations and societies worldwide, such as Asian Pacific Society for Digestive Endoscopy[124], Japan Gastroenterological Endoscopy Society[125], and Canadian Association of Gastroenterology for Endoscopy Facilities[126], to optimize the practice of endoscopy in the era of COVID-19. Teng et al[119] compared these practices regarding endoscopy during COVID-19 between different countries and shared their experiences regarding endoscopy in COVID-19. Additionally, Ang et al[127] provided guidance for the safe conduct of GI endoscopy procedures during the COVID-19 pandemic in Singapore. In order to help better the medical staff and patients while performing endoscopy during the COVID-19 pandemic, the Chinese Society of Digestive Endoscopy (CSDE) has also launched “CSDE guideline for endoscopy works during COVID- 19”[128]. Taken together, these guidelines and recommendations or experiences on endoscopy during COVID-19 can be classified into measures before, during, and after endoscopy that must be considered for both non-infected and infected patients, or prehospital management, intrahospital management, and posthospital management[118,119,127]. These management strategies in the digestive endoscopy center during the COVID-19 pandemic could be summarized into the following five aspects: Human, instruments, materials, methods, and environment[129]. As the pandemic develops in individual countries and these measures might not necessarily reflect the current state of practice, improvement in quality and safety of endoscopy continually and further protection of patients and medical staff are required in the era of COVID-19.
Nausea, diarrhea, and abdominal pain are the common GI symptoms, although the reported incidence varies widely among the patients suffering from COVID-19. GI symptoms may appear with or without respiratory symptoms. Patients with GI symptoms tend to have a longer and more severe disease and continue to shed SARS-CoV-2 virus in the stool although the virus has been cleared from the respiratory system[130]. Clinicians should avoid overlooking or underestimating GI symptoms in COVID-19 patients. The primary aim is to manage nausea, diarrhea, and abdominal pain via symptomatic treatment options along with the use of probiotics to control the occurrence of intestinal dysbiosis[131]. There are no specific symptoms and signs in COVID-19 patients. Radiologic manifestations of SARS-CoV-2 infection in the GI tract included non-specific small and large bowel wall thickening and liquid stool throughout the bowel[78]. Although it was recommended to cancel non-essential endoscopic procedures and only emergency endoscopies were permitted, endoscopic diagnosis and treatment has been served as an indispensable part in the management of severe COVID-19 cases[83,84]. In-depth exploration of the relationship between COVID-19 and the digestive system is urgently needed. The ACE2 receptor is thought to be the potential entry point in the GI tract[132]. Studies have shown that the possible mechanisms of digestive tract infection may include direct viral invasion into target cells, dysregulation of ACE2, immune-mediated tissue injury, and gut dysbiosis caused by microbiota[14,25,87,88]. The pathogenesis of digestive tract involvement is complex and needs further study.
At present, the main transmission routes of COVID-19 are respiratory droplets and close contact. Aerosol transmission can be caused by exposure to virus-contaminated objects and environments under certain conditions. Fecal-oral transmission might be possible, while tear (conjunctival) and mother-to-fetus transmission are yet to be confirmed, providing a reference basis for COVID-19 prevention and public protection[133-135]. Since GI symptoms alone are quite rare in COVID-19 patients, a routine SARS-CoV-2 stool test is not indicated, and it should be performed only in patients with negative nasopharyngeal swabs in the presence of clear imaging features indicative of interstitial pneumonia[131]. However, there is no definite suggestion on whether a routine SARS-CoV-2 stool test is needed in COVID-19 patients who were cured and had negative nasopharyngeal swabs. During the pandemic, appointment system, drive-in procedure, proper wearing of PPE, strengthening ventilation and disinfection, only emergency endoscopies, and various prevention measures (including human, instruments, materials, methods, and environment) should be enforced in the outpatient visits, inpatient ward, and endoscopy centers. Meanwhile, in the era of COVID-19, these prevention strategies should be improved continually to fit their own unique condition, including released guidelines, recommendations, position statements, or published practical experiences by different organizations and societies worldwide. Increasing evidence suggests that fecal-oral transmission and environmental contamination by COVID-19 patients should not be ignored
We thank all colleagues, the reviewers, and the editors for improving our paper.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Manenti A, Shoenfeld Y S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Xing YX
| 1. | Abdulrab S, Al-Maweri S, Halboub E. Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm. Med Hypotheses. 2020;143:109897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | WHO. Weekly epidemiological update on COVID-19 –16 March 2021. [cited 10 December 2020].Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update---16-march-2021. |
| 3. | Nie K, Yang YY, Deng MZ, Wang XY. Gastrointestinal insights during the COVID-19 epidemic. World J Clin Cases. 2020;8:3934-3941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (2)] |
| 4. | Song Y, Liu P, Shi XL, Chu YL, Zhang J, Xia J, Gao XZ, Qu T, Wang MY. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut. 2020;69:1143-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 221] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 5. | Yang X, Zhao J, Yan Q, Zhang S, Wang Y, Li Y. A case of COVID-19 patient with the diarrhea as initial symptom and literature review. Clin Res Hepatol Gastroenterol. 2020;44:e109-e112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Yang TY, Li YC, Wang SC, Dai QQ, Jiang XS, Zuo S, Jia L, Zheng JB, Wang HL. Clinical characteristics of patients with COVID-19 presenting with gastrointestinal symptoms as initial symptoms: Retrospective case series. World J Clin Cases. 2020;8:2950-2958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3643] [Cited by in RCA: 4143] [Article Influence: 197.3] [Reference Citation Analysis (0)] |
| 8. | Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020; 181: 271-280. e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11946] [Cited by in RCA: 14213] [Article Influence: 2842.6] [Reference Citation Analysis (0)] |
| 9. | Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4155] [Cited by in RCA: 3819] [Article Influence: 763.8] [Reference Citation Analysis (1)] |
| 10. | Lin L, Jiang X, Zhang Z, Huang S, Fang Z, Gu Z, Gao L, Shi H, Mai L, Liu Y, Lin X, Lai R, Yan Z, Li X, Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997-1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 630] [Cited by in RCA: 655] [Article Influence: 131.0] [Reference Citation Analysis (0)] |
| 11. | Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan KH, Yuen KY, Leung WK. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis. Gastroenterology. 2020;159:81-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1113] [Cited by in RCA: 1126] [Article Influence: 225.2] [Reference Citation Analysis (1)] |
| 12. | Wang MW, Zhou MY, Ji GH, Ye L, Cheng YR, Feng ZH, Chen J. Mask crisis during the COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:3397-3399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 13. | Deidda S, Tora L, Firinu D, Del Giacco S, Campagna M, Meloni F, Orrù G, Chessa L, Carta MG, Melis A, Spolverato G, Littera R, Perra A, Onali S, Zorcolo L, Restivo A. Gastrointestinal coronavirus disease 2019: epidemiology, clinical features, pathogenesis, prevention, and management. Expert Rev Gastroenterol Hepatol. 2021;15:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-1833. e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1985] [Cited by in RCA: 1992] [Article Influence: 398.4] [Reference Citation Analysis (1)] |
| 15. | van Doorn AS, Meijer B, Frampton CMA, Barclay ML, de Boer NKH. Systematic review with meta-analysis: SARS-CoV-2 stool testing and the potential for faecal-oral transmission. Aliment Pharmacol Ther. 2020;52:1276-1288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 83] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 16. | Peng J, Wang M, Zhang G, Lu E. Seven discharged patients turning positive again for SARS-CoV-2 on quantitative RT-PCR. Am J Infect Control. 2020;48:725-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Xie C, Jiang L, Huang G, Pu H, Gong B, Lin H, Ma S, Chen X, Long B, Si G, Yu H, Yang X, Shi Y, Yang Z. Comparison of different samples for 2019 novel coronavirus detection by nucleic acid amplification tests. Int J Infect Dis. 2020;93:264-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 18. | Zhang J, Wang S, Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol. 2020;92:680-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 278] [Cited by in RCA: 301] [Article Influence: 60.2] [Reference Citation Analysis (0)] |
| 19. | Cha MH, Regueiro M, Sandhu DS. Gastrointestinal and hepatic manifestations of COVID-19: A comprehensive review. World J Gastroenterol. 2020;26:2323-2332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 124] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (2)] |
| 20. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18839] [Article Influence: 3767.8] [Reference Citation Analysis (7)] |
| 21. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12958] [Article Influence: 2591.6] [Reference Citation Analysis (1)] |
| 22. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14749] [Article Influence: 2949.8] [Reference Citation Analysis (0)] |
| 23. | Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, Hao SR, Jia HY, Cai H, Zhang XL, Yu GD, Xu KJ, Wang XY, Gu JQ, Zhang SY, Ye CY, Jin CL, Lu YF, Yu X, Yu XP, Huang JR, Xu KL, Ni Q, Yu CB, Zhu B, Li YT, Liu J, Zhao H, Zhang X, Yu L, Guo YZ, Su JW, Tao JJ, Lang GJ, Wu XX, Wu WR, Qv TT, Xiang DR, Yi P, Shi D, Chen Y, Ren Y, Qiu YQ, Li LJ, Sheng J, Yang Y. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 944] [Cited by in RCA: 868] [Article Influence: 173.6] [Reference Citation Analysis (0)] |
| 24. | Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2139] [Cited by in RCA: 2339] [Article Influence: 467.8] [Reference Citation Analysis (0)] |
| 25. | Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 594] [Cited by in RCA: 582] [Article Influence: 116.4] [Reference Citation Analysis (0)] |
| 26. | Dong ZY, Xiang BJ, Jiang M, Sun MJ, Dai C. The Prevalence of Gastrointestinal Symptoms, Abnormal Liver Function, Digestive System Disease and Liver Disease in COVID-19 Infection: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2021;55:67-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 27. | Zhang MQ, Wang XH, Chen YL, Zhao KL, Cai YQ, An CL, Lin MG, Mu XD. [Clinical features of 2019 novel coronavirus pneumonia in the early stage from a fever clinic in Beijing]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 28. | Wang Z, Chen X, Lu Y, Chen F, Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends. 2020;14:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 336] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 29. | Andrews PLR, Cai W, Rudd JA, Sanger GJ. COVID-19, nausea, and vomiting. J Gastroenterol Hepatol. 2021;36:646-656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 30. | Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, Li P, Hu B, Wang J, Hu C, Jin Y, Niu X, Ping R, Du Y, Li T, Xu G, Hu Q, Tu L. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am J Gastroenterol. 2020;115:766-773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1160] [Cited by in RCA: 1203] [Article Influence: 240.6] [Reference Citation Analysis (0)] |
| 31. | Elmunzer BJ, Spitzer RL, Foster LD, Merchant AA, Howard EF, Patel VA, West MK, Qayed E, Nustas R, Zakaria A, Piper MS, Taylor JR, Jaza L, Forbes N, Chau M, Lara LF, Papachristou GI, Volk ML, Hilson LG, Zhou S, Kushnir VM, Lenyo AM, McLeod CG, Amin S, Kuftinec GN, Yadav D, Fox C, Kolb JM, Pawa S, Pawa R, Canakis A, Huang C, Jamil LH, Aneese AM, Glamour BK, Smith ZL, Hanley KA, Wood J, Patel HK, Shah JN, Agarunov E, Sethi A, Fogel EL, McNulty G, Haseeb A, Trieu JA, Dixon RE, Yang JY, Mendelsohn RB, Calo D, Aroniadis OC, LaComb JF, Scheiman JM, Sauer BG, Dang DT, Piraka CR, Shah ED, Pohl H, Tierney WM, Mitchell S, Condon A, Lenhart A, Dua KS, Kanagala VS, Kamal A, Singh VK, Pinto-Sanchez MI, Hutchinson JM, Kwon RS, Korsnes SJ, Singh H, Solati Z, Willingham FF, Yachimski PS, Conwell DL, Mosier E, Azab M, Patel A, Buxbaum J, Wani S, Chak A, Hosmer AE, Keswani RN, DiMaio CJ, Bronze MS, Muthusamy R, Canto MI, Gjeorgjievski VM, Imam Z, Odish F, Edhi AI, Orosey M, Tiwari A, Patwardhan S, Brown NG, Patel AA, Ordiah CO, Sloan IP, Cruz L, Koza CL, Okafor U, Hollander T, Furey N, Reykhart O, Zbib NH, Damianos JA, Esteban J, Hajidiacos N, Saul M, Mays M, Anderson G, Wood K, Mathews L, Diakova G, Caisse M, Wakefield L, Nitchie H, Waljee AK, Tang W, Zhang Y, Zhu J, Deshpande AR, Rockey DC, Alford TB, Durkalski V; North American Alliance for the Study of Digestive Manifestations of COVID-19. Digestive Manifestations in Patients Hospitalized With Coronavirus Disease 2019. Clin Gastroenterol Hepatol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 32. | Fang D, Ma JD, Guan JL, Wang MR, Song Y, Tian DA, Li PY. Manifestations of digestive system of hospitalized patients with coronavirus disease 2019 in Wuhan, China: a single-center descriptive study. Zhonghua Xiaohua Zazhi. 2020;40:151-156. [DOI] [Full Text] |
| 33. | Sultan S, Altayar O, Siddique SM, Davitkov P, Feuerstein JD, Lim JK, Falck-Ytter Y, El-Serag HB; AGA Institute. Electronic address: ewilson@gastro.org. AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19. Gastroenterology 2020; 159: 320-334. e27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 309] [Cited by in RCA: 292] [Article Influence: 58.4] [Reference Citation Analysis (1)] |
| 34. | Chen D, Li X, Song Q, Hu C, Su F, Dai J, Ye Y, Huang J, Zhang X. Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China. JAMA Netw Open. 2020;3:e2011122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 159] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 35. | Luo S, Zhang X, Xu H. Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19). Clin Gastroenterol Hepatol. 2020;18:1636-1637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 234] [Cited by in RCA: 233] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 36. | Wang M, Yan W, Qi W, Wu D, Zhu L, Li W, Wang X, Ma K, Ni M, Xu D, Wang H, Chen G, Yu H, Ding H, Xing M, Han M, Luo X, Chen T, Guo W, Xi D, Ning Q. Clinical characteristics and risk factors of liver injury in COVID-19: a retrospective cohort study from Wuhan, China. Hepatol Int. 2020;14:723-732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 37. | Li J, Fan JG. Characteristics and Mechanism of Liver Injury in 2019 Coronavirus Disease. J Clin Transl Hepatol. 2020;8:13-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 205] [Article Influence: 41.0] [Reference Citation Analysis (2)] |
| 38. | Liu C, Jiang ZC, Shao CX, Zhang HG, Yue HM, Chen ZH, Ma BY, Liu WY, Huang HH, Yang J, Wang Y, Liu HY, Xu D, Wang JT, Yang JY, Pan HQ, Zou SQ, Li FJ, Lei JQ, Li X, He Q, Gu Y, Qi XL. [Preliminary study of the relationship between novel coronavirus pneumonia and liver function damage: a multicenter study]. Zhonghua Gan Zang Bing Za Zhi. 2020;28:107-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 54] [Reference Citation Analysis (0)] |
| 39. | Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1348] [Cited by in RCA: 1293] [Article Influence: 258.6] [Reference Citation Analysis (4)] |
| 40. | Wan J, Wang X, Su S, Zhang Y, Jin Y, Shi Y, Wu K, Liang J. Digestive symptoms and liver injury in patients with coronavirus disease 2019 (COVID-19): A systematic review with meta-analysis. JGH Open. 2020;4:1047-1058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Nardo AD, Schneeweiss-Gleixner M, Bakail M, Dixon ED, Lax SF, Trauner M. Pathophysiological mechanisms of liver injury in COVID-19. Liver Int. 2021;41:20-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 281] [Cited by in RCA: 271] [Article Influence: 67.8] [Reference Citation Analysis (2)] |
| 42. | Liu R, Zhao L, Cheng X, Han H, Li C, Li D, Liu A, Gao G, Zhou F, Liu F, Jiang Y, Zhu C, Xia Y. Clinical characteristics of COVID-19 patients with hepatitis B virus infection - a retrospective study. Liver Int. 2021;41:720-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 43. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18175] [Article Influence: 3635.0] [Reference Citation Analysis (0)] |
| 44. | Hajifathalian K, Krisko T, Mehta A, Kumar S, Schwartz R, Fortune B, Sharaiha RZ; WCM-GI research group*. Gastrointestinal and Hepatic Manifestations of 2019 Novel Coronavirus Disease in a Large Cohort of Infected Patients From New York: Clinical Implications. Gastroenterology 2020; 159: 1137-1140. e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 45. | Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2289] [Cited by in RCA: 2546] [Article Influence: 509.2] [Reference Citation Analysis (2)] |
| 46. | Wu Y, Li H, Guo X, Yoshida EM, Mendez-Sanchez N, Levi Sandri GB, Teschke R, Romeiro FG, Shukla A, Qi X. Incidence, risk factors, and prognosis of abnormal liver biochemical tests in COVID-19 patients: a systematic review and meta-analysis. Hepatol Int. 2020;14:621-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 47. | Ye L, Chen B, Wang Y, Yang Y, Zeng J, Deng G, Deng Y, Zeng F. Prognostic value of liver biochemical parameters for COVID-19 mortality. Ann Hepatol. 2021;21:100279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 48. | An YW, Song S, Li WX, Chen YX, Hu XP, Zhao J, Li ZW, Jiang GY, Wang C, Wang JC, Yuan B, Liu HQ. Liver function recovery of COVID-19 patients after discharge, a follow-up study. Int J Med Sci. 2021;18:176-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 49. | An YW, Yuan B, Wang JC, Wang C, Liu TT, Song S, Liu HQ. Clinical characteristics and impacts of traditional Chinese medicine treatment on the convalescents of COVID-19. Int J Med Sci. 2021;18:646-651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 50. | Yang RX, Zheng RD, Fan JG. Etiology and management of liver injury in patients with COVID-19. World J Gastroenterol. 2020;26:4753-4762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (2)] |
| 51. | Wang Y, Liu S, Liu H, Li W, Lin F, Jiang L, Li X, Xu P, Zhang L, Zhao L, Cao Y, Kang J, Yang J, Li L, Liu X, Li Y, Nie R, Mu J, Lu F, Zhao S, Lu J, Zhao J. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020;73:807-816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 353] [Cited by in RCA: 457] [Article Influence: 91.4] [Reference Citation Analysis (0)] |
| 52. | Sonzogni A, Previtali G, Seghezzi M, Grazia Alessio M, Gianatti A, Licini L, Morotti D, Zerbi P, Carsana L, Rossi R, Lauri E, Pellegrinelli A, Nebuloni M. Liver histopathology in severe COVID 19 respiratory failure is suggestive of vascular alterations. Liver Int. 2020;40:2110-2116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 218] [Article Influence: 43.6] [Reference Citation Analysis (0)] |
| 53. | Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 Expression in Pancreas May Cause Pancreatic Damage After SARS-CoV-2 Infection. Clin Gastroenterol Hepatol 2020; 18: 2128-2130. e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 343] [Cited by in RCA: 472] [Article Influence: 94.4] [Reference Citation Analysis (0)] |
| 54. | Taneera J, El-Huneidi W, Hamad M, Mohammed AK, Elaraby E, Hachim MY. Expression Profile of SARS-CoV-2 Host Receptors in Human Pancreatic Islets Revealed Upregulation of ACE2 in Diabetic Donors. Biology (Basel). 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 55. | Mukherjee R, Smith A, Sutton R. Covid-19-related pancreatic injury. Br J Surg. 2020;107:e190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 56. | Fignani D, Licata G, Brusco N, Nigi L, Grieco GE, Marselli L, Overbergh L, Gysemans C, Colli ML, Marchetti P, Mathieu C, Eizirik DL, Sebastiani G, Dotta F. SARS-CoV-2 Receptor Angiotensin I-Converting Enzyme Type 2 (ACE2) Is Expressed in Human Pancreatic β-Cells and in the Human Pancreas Microvasculature. Front Endocrinol (Lausanne). 2020;11:596898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 140] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 57. | Kumaran NK, Karmakar BK, Taylor OM. Coronavirus disease-19 (COVID-19) associated with acute necrotising pancreatitis (ANP). BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 58. | Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;20:1026-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 141] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 59. | Juhász MF, Ocskay K, Kiss S, Hegyi P, Párniczky A. Insufficient etiological workup of COVID-19-associated acute pancreatitis: A systematic review. World J Gastroenterol. 2020;26:6270-6278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 60. | Suchman K, Raphael KL, Liu Y, Wee D, Trindade AJ; Northwell COVID-19 Research Consortium. Acute pancreatitis in children hospitalized with COVID-19. Pancreatology. 2021;21:31-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 61. | Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members. Pancreatology. 2020;20:665-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 169] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 62. | Patnaik RNK, Gogia A, Kakar A. Acute pancreatic injury induced by COVID-19. IDCases. 2020;22:e00959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 63. | Akarsu C, Karabulut M, Aydin H, Sahbaz NA, Dural AC, Yegul D, Peker KD, Ferahman S, Bulut S, Dönmez T, Asar S, Yasar KK, Adas GT. Association between Acute Pancreatitis and COVID-19: Could Pancreatitis Be the Missing Piece of the Puzzle about Increased Mortality Rates? J Invest Surg. 2020;1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 64. | Wang F, Wang H, Fan J, Zhang Y, Zhao Q. Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia. Gastroenterology. 2020;159:367-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 276] [Cited by in RCA: 325] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 65. | Akkus C, Yilmaz H, Mizrak S, Adibelli Z, Akdas O, Duran C. Development of pancreatic injuries in the course of COVID-19. Acta Gastroenterol Belg. 2020;83:585-592. [PubMed] |
| 66. | Bansal P, Margekar SL, Suman V, Sud R, Meena S, Sharma AK, Islam SY, Gurtoo A, Agrawal A, Pangtey GS, Prakash A. Pancreatic Injury in COVID-19 Patients. J Assoc Physicians India. 2020;68:58-60. [PubMed] |
| 67. | Cheung S, Quiwa JC, Pillai A, Onwu C, Tharayil ZJ, Gupta R. Superior Mesenteric Artery Thrombosis and Acute Intestinal Ischemia as a Consequence of COVID-19 Infection. Am J Case Rep. 2020;21:e925753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 68. | Keshavarz P, Rafiee F, Kavandi H, Goudarzi S, Heidari F, Gholamrezanezhad A. Ischemic gastrointestinal complications of COVID-19: a systematic review on imaging presentation. Clin Imaging. 2020;73:86-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 69. | Norsa L, Bonaffini PA, Indriolo A, Valle C, Sonzogni A, Sironi S. Poor Outcome of Intestinal Ischemic Manifestations of COVID-19. Gastroenterology 2020; 159: 1595-1597. e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 70. | Paul T, Joy AR, Alsoub HARS, Parambil JV. Case Report: Ischemic Colitis in Severe COVID-19 Pneumonia: An Unforeseen Gastrointestinal Complication. Am J Trop Med Hyg. 2021;104:63-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 71. | Singh B, Kaur P. COVID-19 and acute mesenteric ischemia: A review of literature. Hematol Transfus Cell Ther. 2021;43:112-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 72. | Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417-1418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4227] [Cited by in RCA: 4561] [Article Influence: 912.2] [Reference Citation Analysis (0)] |
| 73. | Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, Pesenti A, Peyvandi F, Tripodi A. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738-1742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 926] [Cited by in RCA: 952] [Article Influence: 190.4] [Reference Citation Analysis (0)] |
| 74. | Parry AH, Wani AH, Yaseen M. Acute Mesenteric Ischemia in Severe Coronavirus-19 (COVID-19): Possible Mechanisms and Diagnostic Pathway. Acad Radiol. 2020;27:1190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 75. | Manolis AS, Manolis TA, Manolis AA, Papatheou D, Melita H. COVID-19 Infection: Viral Macro- and Micro-Vascular Coagulopathy and Thromboembolism/Prophylactic and Therapeutic Management. J Cardiovasc Pharmacol Ther. 2021;26:12-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 76. | Thuluva SK, Zhu H, Tan MML, Gupta S, Yeong KY, Cheong Wah ST, Lin L, Yap ES. A 29-Year-Old Male Construction Worker from India Who Presented with Left- Sided Abdominal Pain Due to Isolated Superior Mesenteric Vein Thrombosis Associated with SARS-CoV-2 Infection. Am J Case Rep. 2020;21:e926785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 77. | Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Catalano O, Gee MS, Hahn PF, Harisinghani M, Kilcoyne A, Lee SI, Mojtahed A, Pandharipande PV, Pierce TT, Rosman DA, Saini S, Samir AE, Simeone JF, Gervais DA, Velmahos G, Misdraji J, Kambadakone A. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology. 2020;297:E207-E215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 181] [Cited by in RCA: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 78. | Lui K, Wilson MP, Low G. Abdominal imaging findings in patients with SARS-CoV-2 infection: a scoping review. Abdom Radiol (NY). 2021;46:1249-1255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 79. | Horvat N, Pinto PVA, Araujo-Filho JAB, Santos JMMM, Dias AB, Miranda JA, de Oliveira CV, Barbosa CS, Morais TC, N Assuncao-Jr A, Nomura CH, Viana PCC. Abdominal gastrointestinal imaging findings on computed tomography in patients with COVID-19 and correlation with clinical outcomes. Eur J Radiol Open. 2021;8:100326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 80. | Morparia K, Park MJ, Kalyanaraman M, McQueen D, Bergel M, Phatak T. Abdominal Imaging Findings in Critically Ill Children With Multisystem Inflammatory Syndrome Associated With COVID-19. Pediatr Infect Dis J. 2021;40:e82-e83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 81. | Shiralkar K, Chinapuvvula N, Ocazionez D. Cross-Sectional Abdominal Imaging Findings in Patients With COVID-19. Cureus. 2020;12:e9538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Wilson MP, Katlariwala P, Low G. Potential implications of novel coronavirus disease (COVID-19) related gastrointestinal symptoms for abdominal imaging. Radiography (Lond). 2020;26:274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 83. | Mao R, Liang J, Wu KC, Chen MH. Responding to COVID-19: Perspectives From the Chinese Society of Gastroenterology. Gastroenterology. 2020;158:2024-2027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 84. | Gu Q, Wang HF, Fang Y, Lu Y, Shen Z, Wang Y, Wu X, Cen L, Chen YS. Analysis of an improved workflow of endoscope reprocessing for bedside endoscopic diagnosis and treatment on COVID-19 patients. J Zhejiang Univ Sci B. 2020;21:416-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 85. | Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020; 181: 281-292. e6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4743] [Cited by in RCA: 6133] [Article Influence: 1226.6] [Reference Citation Analysis (0)] |
| 86. | Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260-1263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5792] [Cited by in RCA: 6459] [Article Influence: 1291.8] [Reference Citation Analysis (0)] |
| 87. | Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Cui X, Xiao J, Zhan J, Meng T, Zhou W, Liu J, Xu H. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69:1010-1018. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 314] [Cited by in RCA: 379] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 88. | Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, Tsoukalas N, Viazis N, Liatsos C, Mantzaris GJ. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. 2020;26:4579-4588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 98] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (5)] |
| 89. | Leonardi A, Rosani U, Brun P. Ocular Surface Expression of SARS-CoV-2 Receptors. Ocul Immunol Inflamm. 2020;28:735-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 90. | Kumar A, Faiq MA, Pareek V, Raza K, Narayan RK, Prasoon P, Kumar P, Kulandhasamy M, Kumari C, Kant K, Singh HN, Qadri R, Pandey SN, Kumar S. Relevance of SARS-CoV-2 related factors ACE2 and TMPRSS2 expressions in gastrointestinal tissue with pathogenesis of digestive symptoms, diabetes-associated mortality, and disease recurrence in COVID-19 patients. Med Hypotheses. 2020;144:110271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 91. | Essahib W, Verheyen G, Tournaye H, Van de Velde H. SARS-CoV-2 host receptors ACE2 and CD147 (BSG) are present on human oocytes and blastocysts. J Assist Reprod Genet. 2020;37:2657-2660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 92. | Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N Engl J Med. 2020;382:1653-1659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1484] [Cited by in RCA: 1561] [Article Influence: 312.2] [Reference Citation Analysis (0)] |
| 93. | Galanopoulos M, Doukatas A, Gazouli M. Origin and genomic characteristics of SARS-CoV-2 and its interaction with angiotensin converting enzyme type 2 receptors, focusing on the gastrointestinal tract. World J Gastroenterol. 2020;26:6335-6345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (2)] |
| 94. | Zhong P, Xu J, Yang D, Shen Y, Wang L, Feng Y, Du C, Song Y, Wu C, Hu X, Sun Y. COVID-19-associated gastrointestinal and liver injury: clinical features and potential mechanisms. Signal Transduct Target Ther. 2020;5:256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 141] [Article Influence: 28.2] [Reference Citation Analysis (1)] |
| 95. | van den Brand JM, Haagmans BL, van Riel D, Osterhaus AD, Kuiken T. The pathology and pathogenesis of experimental severe acute respiratory syndrome and influenza in animal models. J Comp Pathol. 2014;151:83-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 122] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 96. | Gao R, Bhatnagar J, Blau DM, Greer P, Rollin DC, Denison AM, Deleon-Carnes M, Shieh WJ, Sambhara S, Tumpey TM, Patel M, Liu L, Paddock C, Drew C, Shu Y, Katz JM, Zaki SR. Cytokine and chemokine profiles in lung tissues from fatal cases of 2009 pandemic influenza A (H1N1): role of the host immune response in pathogenesis. Am J Pathol. 2013;183:1258-1268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 97. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30049] [Article Influence: 6009.8] [Reference Citation Analysis (3)] |
| 98. | Zhao D, Yao F, Wang L, Zheng L, Gao Y, Ye J, Guo F, Zhao H, Gao R. A Comparative Study on the Clinical Features of Coronavirus 2019 (COVID-19) Pneumonia With Other Pneumonias. Clin Infect Dis. 2020;71:756-761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 239] [Cited by in RCA: 294] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 99. | Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020;383:2255-2273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1324] [Cited by in RCA: 2070] [Article Influence: 414.0] [Reference Citation Analysis (0)] |
| 100. | Kaźmierczak-Siedlecka K, Vitale E, Makarewicz W. COVID-19 - gastrointestinal and gut microbiota-related aspects. Eur Rev Med Pharmacol Sci. 2020;24:10853-10859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 101. | Donati Zeppa S, Agostini D, Piccoli G, Stocchi V, Sestili P. Gut Microbiota Status in COVID-19: An Unrecognized Player? Front Cell Infect Microbiol. 2020;10:576551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 102. | Penninger JM, Grant MB, Sung JJY. The Role of Angiotensin Converting Enzyme 2 in Modulating Gut Microbiota, Intestinal Inflammation, and Coronavirus Infection. Gastroenterology. 2021;160:39-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 103. | Shinu P, Morsy MA, Deb PK, Nair AB, Goyal M, Shah J, Kotta S. SARS CoV-2 Organotropism Associated Pathogenic Relationship of Gut-Brain Axis and Illness. Front Mol Biosci. 2020;7:606779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 104. | Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, Wan Y, Chung ACK, Cheung CP, Chen N, Lai CKC, Chen Z, Tso EYK, Fung KSC, Chan V, Ling L, Joynt G, Hui DSC, Chan FKL, Chan PKS, Ng SC. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology 2020; 159: 944-955. e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 739] [Cited by in RCA: 1056] [Article Influence: 211.2] [Reference Citation Analysis (0)] |
| 105. | Segal JP, Mak JWY, Mullish BH, Alexander JL, Ng SC, Marchesi JR. The gut microbiome: an under-recognised contributor to the COVID-19 pandemic? Therap Adv Gastroenterol. 2020;13:1756284820974914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 106. | Mitsuyama K, Tsuruta K, Takedatsu H, Yoshioka S, Morita M, Niwa M, Matsumoto S. Clinical Features and Pathogenic Mechanisms of Gastrointestinal Injury in COVID-19. J Clin Med. 2020;9:3630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 107. | Chaves Andrade M, Souza de Faria R, Avelino Mota Nobre S. COVID-19: Can the symptomatic SARS-CoV-2 infection affect the homeostasis of the gut-brain-microbiota axis? Med Hypotheses. 2020;144:110206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 108. | Gao QY, Chen YX, Fang JY. 2019 Novel coronavirus infection and gastrointestinal tract. J Dig Dis. 2020;21:125-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 246] [Cited by in RCA: 278] [Article Influence: 55.6] [Reference Citation Analysis (0)] |
| 109. | Luo H, Tang QL, Shang YX, Liang SB, Yang M, Robinson N, Liu JP. Can Chinese Medicine Be Used for Prevention of Corona Virus Disease 2019 (COVID-19)? Chin J Integr Med. 2020;26:243-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 316] [Cited by in RCA: 331] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 110. | Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002;346:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 863] [Cited by in RCA: 762] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 111. | Logan C, Beadsworth MB, Beeching NJ. HIV and diarrhoea: what is new? Curr Opin Infect Dis. 2016;29:486-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 112. | Liu TT, Shen XZ. Suggestions on the prevention and control of novel coronavirus infection in digestive departments. Shanghai Yixue. 2020;43:181-183. [DOI] [Full Text] |
| 113. | Leonardi R, Bellinzoni P, Broglia L, Colombo R, De Marchi D, Falcone L, Giusti G, Grasso V, Mantica G, Passaretti G, Proietti S, Russo A, Saitta G, Smelzo S, Suardi N, Gaboardi F. Hospital care in Departments defined as COVID-free: A proposal for a safe hospitalization protecting healthcare professionals and patients not affected by COVID-19. Arch Ital Urol Androl. 2020;92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 114. | Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. 2020;323:1610-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1461] [Cited by in RCA: 1390] [Article Influence: 278.0] [Reference Citation Analysis (0)] |
| 115. | Jerry J, O'Regan E, O'Sullivan L, Lynch M, Brady D. Do established infection prevention and control measures prevent spread of SARS-CoV-2 to the hospital environment beyond the patient room? J Hosp Infect. 2020;105:589-592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 116. | Chen HC, Chang K, Chen SC. Infection control strategies of medical institutions in response to COVID-19. Kaohsiung J Med Sci. 2020;36:565-567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 117. | Chang YT, Lin CY, Tsai MJ, Hung CT, Hsu CW, Lu PL, Hou MF. Infection control measures of a Taiwanese hospital to confront the COVID-19 pandemic. Kaohsiung J Med Sci. 2020;36:296-304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 118. | Gao Y, Ye LS, Du J, Zhang QY, Hu B. Management of an endoscopy center during the outbreak of COVID-19: Experience from West China Hospital. World J Gastroenterol. 2020;26:5749-5758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 119. | Teng M, Tang SY, Koh CJ. Endoscopy during COVID-19 pandemic: An overview of infection control measures and practical application. World J Gastrointest Endosc. 2020;12:256-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 120. | Su S, Shen J, Zhu L, Qiu Y, He JS, Tan JY, Iacucci M, Ng SC, Ghosh S, Mao R, Liang J. Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges. Therap Adv Gastroenterol. 2020;13:1756284820934626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 121. | Yu Q, Xu P, Gan H, Jia Y, Xiao D, Liao W, Pi G, Yu W. Comprehensive gastroenterology endoscopy unit workflow and infection prevention during the COVID-19 Pandemic: Experience with 159 cases in Wuhan, China. Dig Endosc. 2021;33:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 122. | Hamid HKS. Fecal testing for SARS-CoV-2 in patients undergoing elective lower gastrointestinal endoscopy is advised. J Gastroenterol Hepatol. 2020;35:1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 123. | Perisetti A, Goyal H, Sharma N. Gastrointestinal Endoscopy in the Era of COVID-19. Front Med (Lausanne). 2020;7:587602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 124. | Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling Hu E, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020;69:991-996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 249] [Article Influence: 49.8] [Reference Citation Analysis (0)] |
| 125. | Irisawa A, Furuta T, Matsumoto T, Kawai T, Inaba T, Kanno A, Katanuma A, Kawahara Y, Matsuda K, Mizukami K, Otsuka T, Yasuda I, Tanaka S, Fujimoto K, Fukuda S, Iishi H, Igarashi Y, Inui K, Ueki T, Ogata H, Kato M, Shiotani A, Higuchi K, Fujita N, Murakami K, Yamamoto H, Ito T, Okazaki K, Kitagawa Y, Mine T, Tajiri H, Inoue H. Gastrointestinal endoscopy in the era of the acute pandemic of coronavirus disease 2019: Recommendations by Japan Gastroenterological Endoscopy Society (Issued on April 9th, 2020). Dig Endosc. 2020;32:648-650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 126. | Tse F, Borgaonkar M, Leontiadis GI. COVID-19: Advice from the Canadian Association of Gastroenterology for Endoscopy Facilities, as of March 16, 2020. J Can Assoc Gastroenterol. 2020;3:147-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 127. | Ang TL, Li JW, Vu CKF, Ho GH, Chang JPE, Chong CH, Chua TS, Ong DEH, Yip BCH, Gwee KA. Chapter of Gastroenterologists professional guidance on risk mitigation for gastrointestinal endoscopy during COVID-19 pandemic in Singapore. Singapore Med J. 2020;61:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 128. | Chinese Society of Digestive Endoscopy (CSDE). CSDE guideline for endoscopy works during COVID- 19. Zhonghua Weichang Neijing Dianzi Zazhi. 2020;7:11-14. [DOI] [Full Text] |
| 129. | Wei J, Zhang ST. Management of the digestive endoscopy center under the outbreak of COVID-19. Linchuang He Shiyan Yixue Zazhi. 2020;19:687-690. [DOI] [Full Text] |
| 130. | Qureshi H. The digestive system and the COVID-19. J Pak Med Assoc. 2020;70(Suppl 3):S98-S100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 131. | Caio G, Lungaro L, Cultrera R, De Giorgio R, Volta U. Coronaviruses and gastrointestinal symptoms: an old liaison for the new SARS-CoV-2. Gastroenterol Hepatol Bed Bench. 2020;13:341-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 132. | Ye Q, Wang B, Zhang T, Xu J, Shang S. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. Am J Physiol Gastrointest Liver Physiol. 2020;319:G245-G252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (2)] |
| 133. | Yang C, Ma QY, Zheng YH, Yang YX. [Transmission routes of 2019-novel coronavirus (2019-nCoV)]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54:374-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 134. | Han Q, Lin Q, Ni Z, You L. Uncertainties about the transmission routes of 2019 novel coronavirus. Influenza Other Respir Viruses. 2020;14:470-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 135. | Li H, Wang Y, Ji M, Pei F, Zhao Q, Zhou Y, Hong Y, Han S, Wang J, Wang Q, Li Q. Transmission Routes Analysis of SARS-CoV-2: A Systematic Review and Case Report. Front Cell Dev Biol. 2020;8:618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 136. | He Y, Wang Z, Li F, Shi Y. Public health might be endangered by possible prolonged discharge of SARS-CoV-2 in stool. J Infect. 2020;80:e18-e19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 137. | Bonato G, Dioscoridi L, Mutignani M. Fecal-Oral Transmission of SARS-COV-2: Practical Implications. Gastroenterology. 2020;159:1621-1622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |