Published online May 16, 2021. doi: 10.12998/wjcc.v9.i14.3432
Peer-review started: December 4, 2020
First decision: December 21, 2020
Revised: January 5, 2021
Accepted: February 22, 2021
Article in press: February 22, 2021
Published online: May 16, 2021
Processing time: 145 Days and 11.5 Hours
Ectopic thyroid is defined as a rare developmental anomaly where thyroid tissues are atypically found in locations other than its normal anatomical position: Anterolateral to the second, third, and fourth tracheal cartilages. An intemperate descent or a migration failure of the thyroid anlage results in sub-diaphragmatic thyroid ectopia, a sparse clinical entity.
This case portrays a 63-year-old female patient presenting with chronic abdominal discomfort at a local hospital whereby a computed tomography (CT) scan revealed a well-defined mass in the hepatic entrance. For further examination, the patient underwent a CT scan with contrast, magnetic resonance imaging (MRI), and CT-angiography (CTA) at our department. The CT scan showed a well-defined and high attenuated mass measuring 43 mm × 38 mm in the hepatic entrance with calcification. The CTA revealed an additional finding: Blood supply to the mass from the right hepatic artery. MRI of the upper abdomen demonstr
This case delivers a rare insight of pre-operative radiological imaging of an ectopic thyroid located in the liver. These findings can aid in narrowing down potential differential diagnosis when managing a patient with those subsequent findings.
Core Tip: Thyroid ectopia specifically at the porta hepatis level is quite a rare clinical entity without any conclusive protocol for radiological diagnosis. This paper reviews the limited corresponding literature as well as the presentation of a clinical case in order to help physicians alongside radiologists to minimize misinterpretations and misdiagnosis of ectopic thyroid. This paper will hopefully contribute to the spectrum of information by portraying computed tomography, magnetic resonance imaging, computed tomography angiography, and histopathology amongst a plethora of other data that will contribute in the optimization of the prevalence in conjunction with the management of thyroid ectopia.
- Citation: Chooah O, Ding J, Fei JL, Xu FY, Yue T, Pu CL, Hu HJ. Radiological insights of ectopic thyroid in the porta hepatis: A case report and review of the literature. World J Clin Cases 2021; 9(14): 3432-3441
- URL: https://www.wjgnet.com/2307-8960/full/v9/i14/3432.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i14.3432
Ectopic thyroid is a rare developmental anomaly defined as the atypical presence of thyroid tissues in locations other than its normal anatomical position of being anterolateral to the second, third, and fourth tracheal cartilages[1]. Statistically, it is prevalent in 1 per 100000-300000 persons and it has been reported that 1 in 4000-8000 patients suffering from thyroid disease have this condition[2].
The thyroid gland is embryonically the premier endocrine gland that develops on the 24th day of gestation[3]. It is made up of two distinct types of cells, namely, thyroid follicular cells, responsible for the production of thyroid hormones, and parafollicular or C cells that produce calcitonin[4]. According to several reports, a consensual hypothesis for the formation of sub-diaphragmatic thyroid ectopia is the failure of migration or the intemperate descent of the thyroid anlage[3,5,6]. Other studies have shown that abdominal ectopic thyroid may also be due to the common embryologic origin from the foregut endoderm shared by the thyroid as well as the gastro-intestinal tract, the pancreas, and the liver[7,8]. Clinical literature pertaining to abdominal thyroid ectopia is limited, which can be explained by the fact that the majority of patients with this condition are mostly asymptomatic and may present as an incidental finding or as an emergency. Clinicians may also misdiagnose an ectopic thyroid as a neoplasm of adjacent tissues or lipoma or cyst[9]. This case highlights the imaging features of ectopic thyroid in the liver by presenting the subsequent imaging observations made in computed tomography (CT), magnetic resonance imaging (MRI), and CT-angiography (CTA). This report is aimed to optimize the clinician’s as well as the radiologist’s diagnostic prospect when encountering thyroid ectopia.
A 63-year-old Chinese woman presented to our department after the discovery of a mass in the hepatic portal entrance on a CT scan at a local hospital.
The patient initially visited the local hospital with complaints of chronic intermittent abdominal discomfort. A CT scan of the gallbladder, liver, pancreas, and spleen was consequently performed. A mass in the hepatic portal entrance was noted and the case was referred to our hospital for further investigation. Physical examination was unremarkable, preliminary blood tests and tumor markers were within normal limits. The patient had no known liver diseases. For additional work-up, the patient underwent CT with contrast, MRI, and CTA at our department.
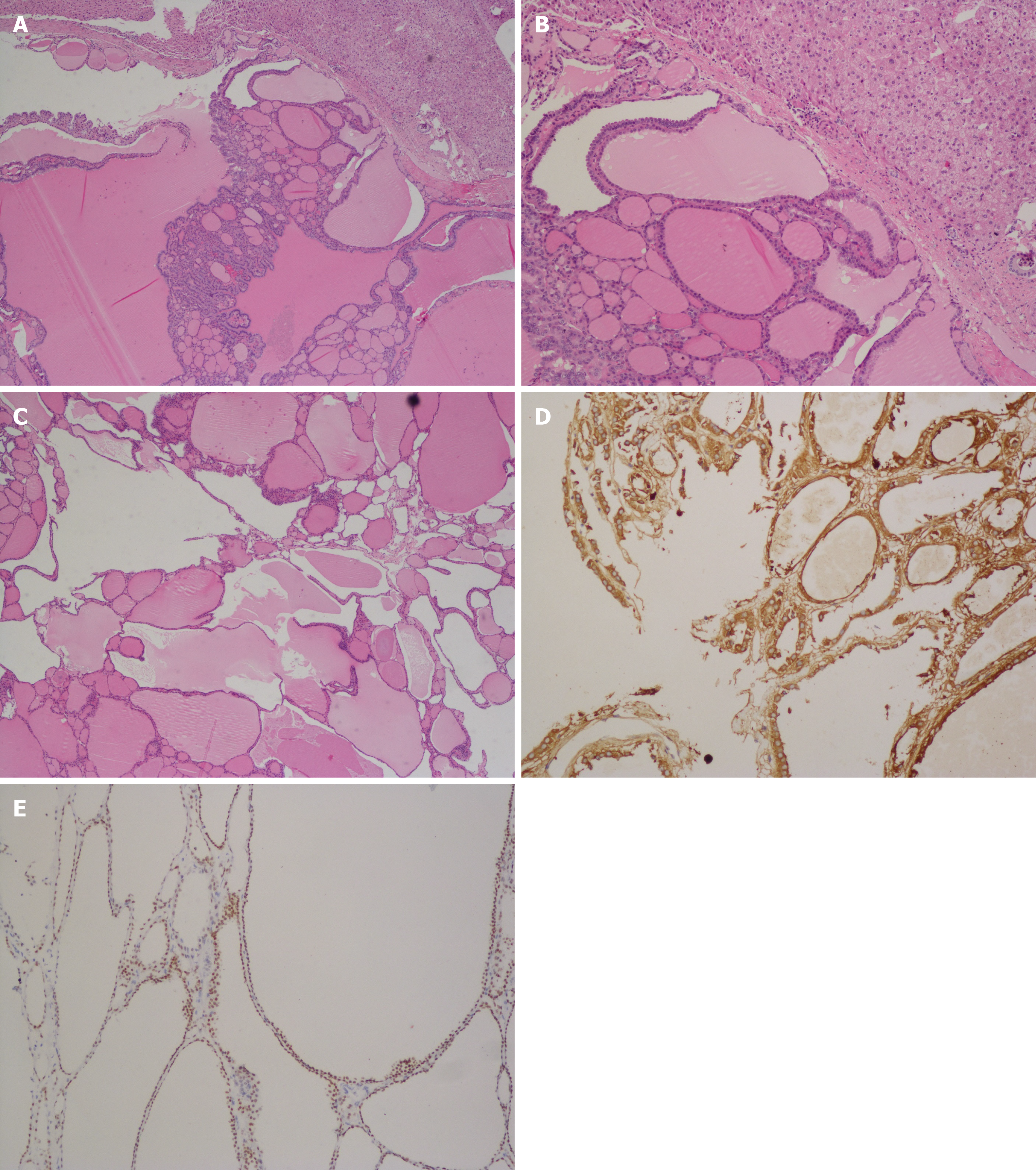
Histopathological report concluded that the mass resected from the liver lobe consisted of thyroid and liver tissue as portrayed in Figure 1A-C. Immunohisto
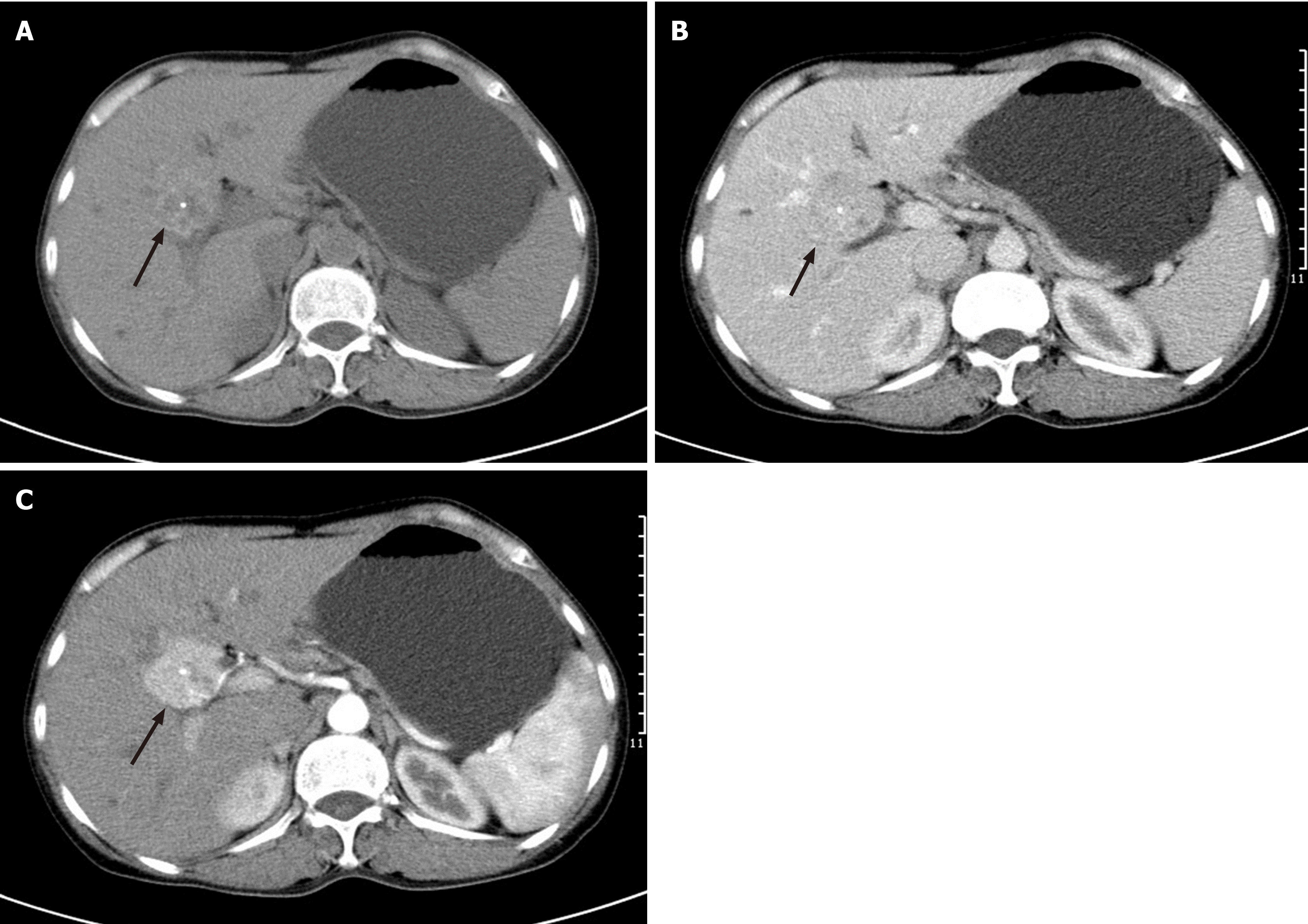
A non-enhanced CT scan revealed a well-circumscribed, heterogeneous and high attenuation mass in comparison to the liver parenchyma with calcification. A contrast- enhanced CT scan of the abdomen and pelvic area revealed a group of high density (compared to the surrounding liver parenchyma) nodules with exhibition of well-defined borders in the hepatic entrance with calcification and an expansive size of 43 mm × 38 mm. The lesion was greatly enhanced in the arterial phase and there was prolonged enhancement in the venous phase with decreasing attenuation, as shown in Figure 2.
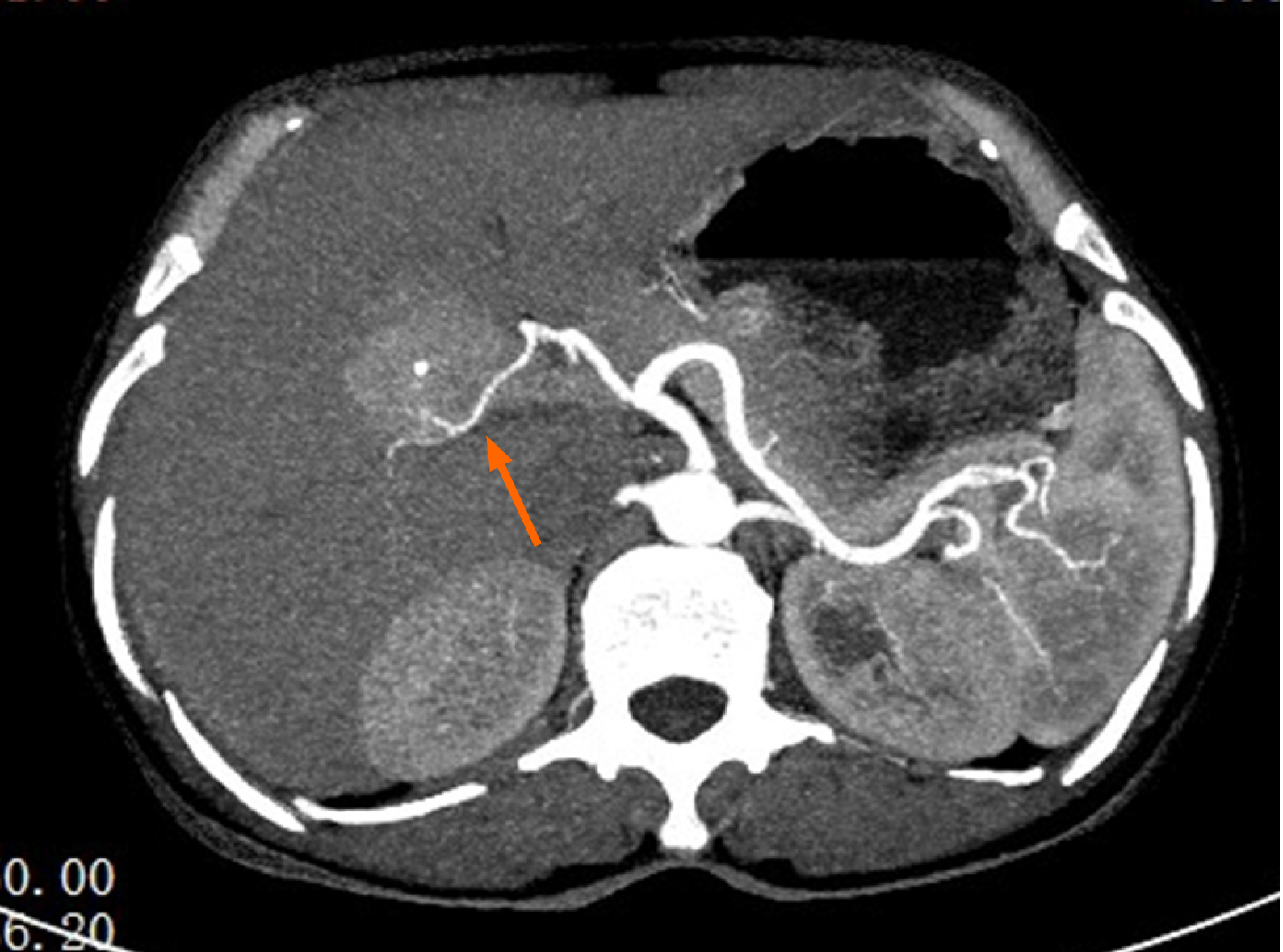
On CTA, in the hepatic entrance, a mass with low attenuation alongside calcification in the middle was observed. In the arterial phase, the mass was supplied by a blood vessel branching from the right hepatic artery as shown in Figure 3.
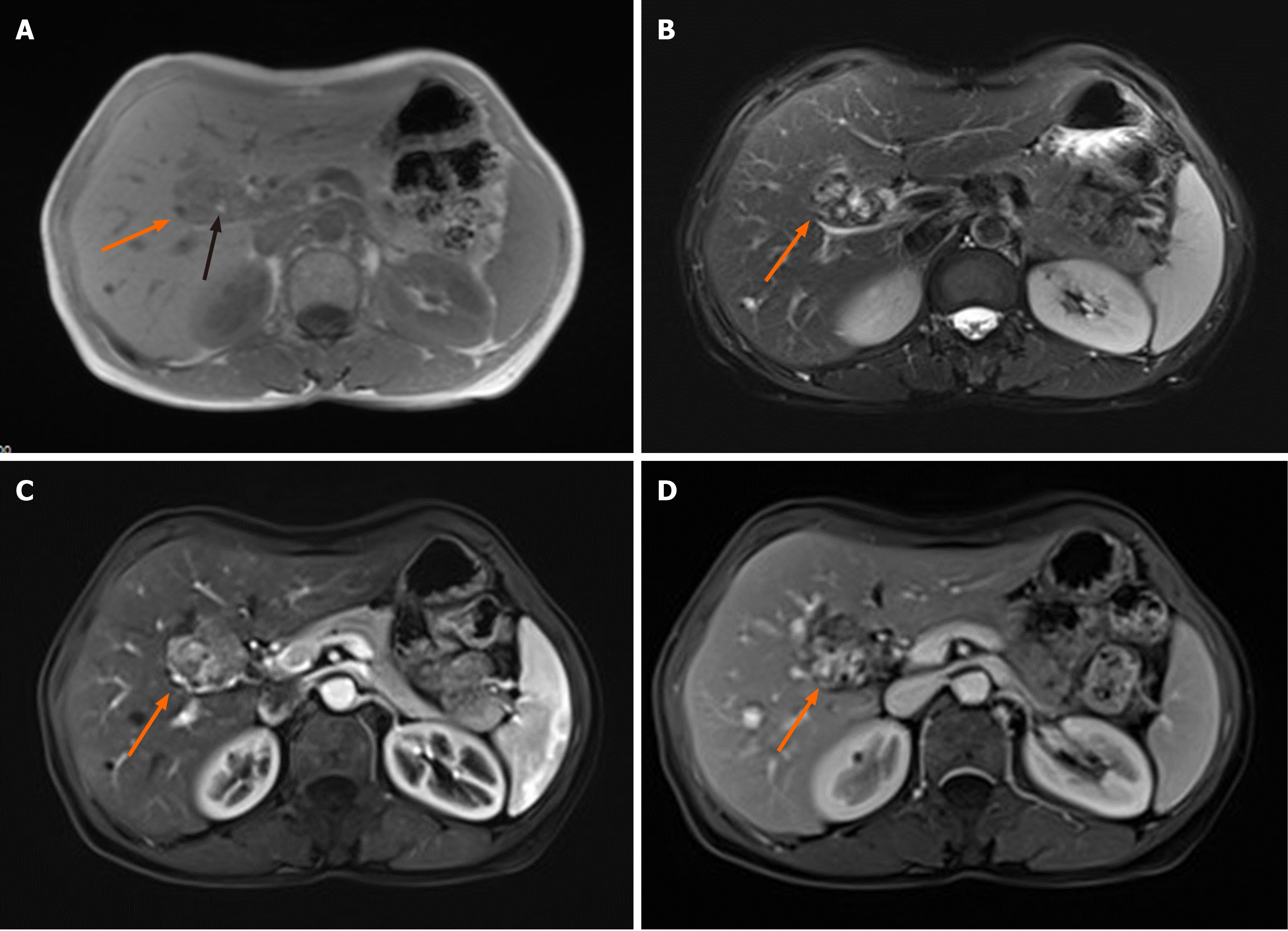
MRI of the upper abdomen demonstrated subsequent enhancement in the hepatic entrance with mixed signal intensity in the observed mass on both T1 and T2 weighted images. The mass was demarcated from the surface of the liver and there was diminished signal intensity in the arterial phase and in the venous phase, as shown in Figure 4.
On the basis of the above findings, a definitive diagnosis of ectopic thyroid in the porta hepatis with nodules was established.
The patient underwent surgery with resection of multiple nodules in the hepatic entrance. The surgical intervention revealed a single mass with a clear surface membrane measuring 30 mm in the hepatic entrance. The mass was interlinked with the right hepatic artery, the right branch of hepatic portal vein, and the common hepatic duct. Blood supply was observed from the right hepatic artery. The resected mass was sent for a histopathological study bearing the results mentioned above.
Postoperatively, the patient had an uneventful recovery. A one-year follow-up showed that the patient’s thyroid function was within normal limits.
Lingual thyroid is the most common type of ectopic thyroid, accounting for almost 90% of reported cases[6]. While reviewing the English literature available when this paper was being written, occurrences of ectopic thyroid in other distant locations (though very rare in incidence) were documented, which consist of the following sites: The mediastinum[10], heart[11], ascending aorta[12], thymus[13], esophagus[14], duode
The prevalence of ectopic thyroid is approximately 1 per 100000-300000 persons[24]. Ma et al[17] reported a predominance of the clinical entity in women as early as the 30th week of gestation to 76 years of age. The first case of ectopic thyroid was reported in 1869 by Hickman[25] and up to present, only 700 cases approximately have been documented worldwide, which makes this pathologic developmental condition a rarity. The occurrence of thyroid tissue in the liver has been explained as an arrest of migration[6] of the thyroid from the common embryologic origin: The foregut endoderm[9]. Additionally, excessive descent of the thyroglossal duct remnants has also been suggested for the aberrant development of ectopic thyroid in distant locations[26] such as the gallbladder[5], stomach bed[16], porta hepatis[1], and adrenal gland[19].
From a genetic perspective, mutations in regulatory genes also play a vital role during thyroid embryonic development[4,27]. A mutation in transcription factors such as FOXE1, PAX8, NKX2-1, and TITF-1 may be involved in thyroid dysgenesis[2,28].
At present, true prevalence of ectopic thyroid cannot be evaluated due to the fact that most patients are asymptomatic and the majority of cases are incidental findings. For symptomatic patients, clinical management usually depends on the age of the patient, thyroid function tests (TFT), severity of the symptoms, histopathological examinations, size of the mass, and complications of the ectopic mass (ulceration, bleeding, cystic degeneration, or malignancy)[10,29-32]. For intra-abdominal thyroid, the symptoms may vary from abdominal pain to diarrhea, and generalized weakness due to a porta hepatis mass[33]. This case report contributes to this statement by presenting a patient with an initial chief complaint of chronic abdominal discomfort, which is a non-specific symptom. However, the assortment of tests and procedures identified the cause to be secondary to a mass within the liver consistent with thyroid ectopia in the porta hepatis. Detection for thyroid ectopia in formerly asymptomatic patients is mostly possible when demands for thyroid hormones increase, e.g., during pregnancy/puberty (physiologic conditions) and trauma/infections (pathologic conditions)[3]. Hence, individuals having ectopic thyroid often suffer from hypothy
Malignant transformation is relatively sparse (< 1%) and appears with distinct histotypes: Mixed follicular and papillary, follicular, papillary, medullary, and Hurthle cell[29].
When a differential diagnosis of thyroid ectopia is considered in a patient, it is important to perform a TFT to assess the serum levels of T3, T4, TSH, and thyroglo
Ultrasound is the first imaging modality favored in the initial assessment of a case suspected to be an ectopic thyroid[17]. It is non-invasive, available in many health institutions, cost-effective, and quick and does not expose the patient to ionizing radiation, hence accessible to a wide array of patients[3]. The sensitivity is further improved by the incorporation of color Doppler that aids in showing hypervascularity through peripheral or internal color flow signals[35]. From literature study, a hyperechoic mass[17] or heterogeneous mass[8,29] is usually observed. B-flow imaging (BFI) is an innovative ultrasound modality that offers direct visualization of blood reflectors compared to Doppler technology and is adequate in the analysis of complex hemodynamics. BFI technique is beneficial to identify twinkling sign patterns for the analysis of thyroid nodules[36-38].
CT is the second mode of imaging for diagnostic workup as it delineates the mass from other anatomic locations, which is helpful in a pre-surgical evaluation[10,31,35]. Contrast CT usually shows an intensely enhancing mass as compared to non-enhanced CT that basically demonstrates high attenuation (due to the intrinsic iodine content) in relation to surrounding tissues[3,6,17]. The masses in the porta hepatis portray solid or semi-solid masses with cystic lesions[1,5,39] with a well circumscribed border and calcifications[1].
CTA provides valuable input in determining vascularization patterns and can also be used for pre-operative embolization in order to minimize risk of hemorrhage during a surgical procedure[40].
Notably, MRI is another radiological approach that helps in localizing ectopic tissue and provides a detailed picture of the mass in contrast to the tissues surrounding it. Presentations of thyroid ectopia on MRI are, however, not uniform[1,5,41] as they depend on the gelatinous material[42].
According to a plethora of literature, it has been shown that radionuclide imaging is also a useful diagnostic tool when ectopy is considered as a differential diagno
Additionally, fine needle aspiration cytology is a valuable diagnostic tool for differentiation between a malignant and benign lesion prior to surgery[6]. Last but not least, immunohistochemistry showing positive staining for TTF-1 and TGB is important for diagnosis of thyroid ectopia.
The most appropriate management of this entity has not yet been established; however, a mass in the porta hepatis may also be suggestive of fibroma, lymphoma, lipoma, hemangioma, dermoid cyst, lymphangioma, squamous cell carcinoma, and a variety of complications such as bleeding, cystic degeneration, or malignancy. Hence, surgical excision is recommended[9,17].
We searched the PubMed database for articles published up to the year 2018 (when the patient was first admitted). The search had the following keywords: “Ectopic thyroid” and “porta hepatis”, altogether. There were a total of 11 retrieved articles, out of which only 5 had proper radiological imaging description of cases in the porta hepatis. These findings have been tabulated (Table 1) for a better comparison. The present case has the same findings as most cases except for that reported by Strohschneider et al[39]. However, presentations on MRI were not mentioned as it was either not widespread during the 1990s or mostly because presentations on MRI are not uniform, showing low to high signal intensity on either T1 or T2 weighted imaging depending on the gelatinous material content, hence making it the least used imaging modality in thyroid ectopia. Apart from CT images that have been rightfully displayed in ectopic thyroid papers, the authors advocate a novel imaging modality for thyroid ectopia: CTA. We believe that CTA will play its part in narrowing down the differential diagnosis amongst a plethora of other hepatic clinical abnormalities based on abnormal hepatic arterial circulation (as shown in Figure 3). Hence, CTA can preferentially be advised as a radiological work-up as compared to MRI and will consequently reduce time consumption, human resources in a clinical setting, and most importantly, the financial burden on a patient. This report is the only one that has altogether documented the CT, CTA, and MRI findings of thyroid ectopia. The authors believe that it will help in lessening the differential diagnosis whereby conditions such as fibroma, lymphoma, lipoma, hemangioma, dermoid cyst, lymphangioma, and squamous cell carcinoma are considered. This will lead to a better representation of incidence of ectopic thyroid cases in the liver as well as minimize misdiagnosis and hopefully facilitate the selection process for patients who have to undergo scintigraphy and eventually surgical resection.
| Ref. | Radiological imaging findings |
| Strohschneider et al[39] | Unenhanced CT: Hyperdense, well-defined mass in comparison to the normal parenchyma |
| Jamshidi et al[33] | Contrast-enhanced CT: Hyperdense appearance compared to normal liver parenchyma |
| Ghanem et al[1] | Unenhanced CT: Inhomogeneous, slightly attenuated, lobulated, well-circumscribed, isodense and hypodense mass compared to the liver tissue with some calcifications. Contrast-enhanced CT: Inhomogeneous contrast enhancement |
| Salam et al[8] | Contrast-enhanced CT: Mass adjacent to the portal vein enhanced in the arterial phase and washed out in the portal phase |
| Fernandez et al[9] | Contrast-enhanced CT: Heterogeneously enhancing mass |
| Present case | Non-enhanced CT: Heterogenous, well-circumscribed, high density mass compared to liver parenchyma with calcification. Contrast-enhanced CT: Well-circumscribed, intensely enhancing mass in the arterial phase with decreasing intensity in the venous phase alongside calcification |
| CT Angiography (widened image thickness construct): Right hepatic artery supplying the lesion shown clearly in arterial phase | |
| MRI: Well-demarcated mass with enhancement on T1 and T2 weighted imaging with mixed signal intensity. Diminished signal intensity in both arterial and venous phases |
The objective of this case report with literature review is to help clinicians with a preliminary identification and diagnosis as well as a consideration for a differential diagnosis of ectopic thyroid in a patient presenting with a mass in the porta hepatis. The rarity of this case in clinical set-ups and academic literature has led to many misinterpretations of thyroid ectopia. The authors believe that this paper will hopefully provide them with the necessary spectrum of information, more specifically radiological insights, of this pathology in order to send for the proper laboratory work-up and to use the appropriate imaging modalities so as to optimize treatment and management of ectopic thyroid in the porta hepatis in symptomatic as well as asymptomatic patients.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Do SI, Torres US S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Ghanem N, Bley T, Altehoefer C, Högerle S, Langer M. Ectopic thyroid gland in the porta hepatis and lingua. Thyroid. 2003;13:503-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Yoon JS, Won KC, Cho IH, Lee JT, Lee HW. Clinical characteristics of ectopic thyroid in Korea. Thyroid. 2007;17:1117-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Ibrahim NA, Fadeyibi IO. Ectopic thyroid: etiology, pathology and management. Hormones (Athens). 2011;10:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | De Felice M, Di Lauro R. Thyroid development and its disorders: genetics and molecular mechanisms. Endocr Rev. 2004;25:722-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 389] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 5. | Liang K, Liu JF, Wang YH, Tang GC, Teng LH, Li F. Ectopic thyroid presenting as a gallbladder mass. Ann R Coll Surg Engl. 2010;92:W4-W6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165:375-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 224] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 7. | Cassol CA, Noria D, Asa SL. Ectopic thyroid tissue within the gall bladder: case report and brief review of the literature. Endocr Pathol. 2010;21:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Salam M, Mohideen A, Stravitz RT. Ectopic thyroid presenting as a liver mass. Clin Gastroenterol Hepatol. 2012;10:xxx. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Fernandez HT, Kim PTW, Cimo M, Goldstein RM. A mass in the porta hepatis: A rare presentation of ectopic thyroid. Int J Hepatobil Pancreat Dis. 2016;6:14-17. |
| 10. | Carannante F, Frasca L, Depalma M, Longo F, Crucitti P. Ectopic thoracic thyroid removed by uniportal VATS approach. A case report. Int J Surg Case Rep. 2019;61:111-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Comajuan SM, Ayerbe JL, Ferrer BR, Quer C, Camazón NV, Sistach EF, Capllonch FG, Baliarda XR, Tudela VV. An intracardiac ectopic thyroid mass. Eur J Echocardiogr. 2009;10:704-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Ozpolat B, Dogan OV, Gökaslan G, Erekul S, Yücel E. Ectopic thyroid gland on the ascending aorta with a partial pericardial defect: report of a case. Surg Today. 2007;37:486-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Spinner RJ, Moore KL, Gottfried MR, Lowe JE, Sabiston DC Jr. Thoracic intrathymic thyroid. Ann Surg. 1994;220:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Salam MA. Ectopic thyroid mass adherent to the oesophagus. J Laryngol Otol. 1992;106:746-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Takahashi T, Ishikura H, Kato H, Tanabe T, Yoshiki T. Ectopic thyroid follicles in the submucosa of the duodenum. Virchows Arch A Pathol Anat Histopathol. 1991;418:547-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Ciçek Y, Taşçi H, Gökdoğan C, Oneş S, Göksel S. Intra-abdominal ectopic thyroid. Br J Surg. 1993;80:316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Ma A, Liu H. Ectopic thyroid of the pancreas: A case report and literature review. Medicine (Baltimore). 2017;96:e8707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Güngör B, Kebat T, Ozaslan C, Akilli S. Intra-abdominal ectopic thyroid presenting with hyperthyroidism: report of a case. Surg Today. 2002;32:148-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Hagiuda J, Kuroda I, Tsukamoto T, Ueno M, Yokota C, Hirose T, Deguchi N. Ectopic thyroid in an adrenal mass: a case report. BMC Urol. 2006;6:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Roth LM, Miller AW 3rd, Talerman A. Typical thyroid-type carcinoma arising in struma ovarii: a report of 4 cases and review of the literature. Int J Gynecol Pathol. 2008;27:496-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Hoda SA, Huvos AG. Struma salpingis associated with struma ovarii. Am J Surg Pathol. 1993;17:1187-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Yilmaz F, Uzunlar AK, Sögütçü N. Ectopic thyroid tissue in the uterus. Acta Obstet Gynecol Scand. 2005;84:201-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Kurman RJ, Prabha AC. Thyroid and parathyroid glands in the vaginal wall: report of a case. Am J Clin Pathol. 1973;59:503-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Santangelo G, Pellino G, De Falco N, Colella G, D'Amato S, Maglione MG, De Luca R, Canonico S, De Falco M. Prevalence, diagnosis and management of ectopic thyroid glands. Int J Surg. 2016;28 Suppl 1:S1-S6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 25. | Hickman W. Congenital tumor of the base of the tongue, pressing down the epiglottis on the larynx and causing death by suffocation sixteen hours after birth. Trans Pathol Soc Lond. 1869;20:160-161. |
| 26. | Harach HR. Ectopic thyroid tissue adjacent to the gallbladder. Histopathology. 1998;32:90-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Gillam MP, Kopp P. Genetic regulation of thyroid development. Curr Opin Pediatr. 2001;13:358-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Batsakis JG, El-Naggar AK, Luna MA. Thyroid gland ectopias. Ann Otol Rhinol Laryngol. 1996;105:996-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 85] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Guerra G, Cinelli M, Mesolella M, Tafuri D, Rocca A, Amato B, Rengo S, Testa D. Morphological, diagnostic and surgical features of ectopic thyroid gland: a review of literature. Int J Surg. 2014;12 Suppl 1:S3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 30. | Talwar N, Mohan S, Ravi B, Andley M, Kumar A. Lithium-induced enlargement of a lingual thyroid. Singapore Med J. 2008;49:254-255. [PubMed] |
| 31. | Chawla M, Kumar R, Malhotra A. Dual ectopic thyroid: case series and review of the literature. Clin Nucl Med. 2007;32:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Douglas PS, Baker AW. Lingual thyroid. Br J Oral Maxillofac Surg. 1994;32:123-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Jamshidi M, Kasirye O, Smith DJ. Ectopic thyroid nodular goiter presenting as a porta hepatis mass. Am Surg. 1998;64:305-306. [PubMed] |
| 34. | Adelchi C, Mara P, Melissa L, De Stefano A, Cesare M. Ectopic thyroid tissue in the head and neck: a case series. BMC Res Notes. 2014;7:790. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Ohnishi H, Sato H, Noda H, Inomata H, Sasaki N. Color Doppler ultrasonography: diagnosis of ectopic thyroid gland in patients with congenital hypothyroidism caused by thyroid dysgenesis. J Clin Endocrinol Metab. 2003;88:5145-5149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Napolitano G, Romeo A, Bianco A, Gasperi M, Zeppa P, Brunese L. B-flow twinkling sign in preoperative evaluation of cervical lymph nodes in patients with papillary thyroid carcinoma. Int J Endocrinol. 2013;2013:203610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Brunese L, Romeo A, Iorio S, Napolitano G, Fucili S, Biondi B, Vallone G, Sodano A. A new marker for diagnosis of thyroid papillary cancer: B-flow twinkling sign. J Ultrasound Med. 2008;27:1187-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Brunese L, Romeo A, Iorio S, Napolitano G, Fucili S, Zeppa P, Vallone G, Lombardi G, Bellastella A, Biondi B, Sodano A. Thyroid B-flow twinkling sign: a new feature of papillary cancer. Eur J Endocrinol. 2008;159:447-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Strohschneider T, Timm D, Worbes C. [Ectopic thyroid gland tissue in the liver]. Chirurg. 1993;64:751-753. [PubMed] |
| 40. | Wong RJ, Cunningham MJ, Curtin HD. Cervical ectopic thyroid. Am J Otolaryngol. 1998;19:397-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Sekine S, Nagata M, Hamada H, Watanabe T. Heterotopic thyroid tissue at the porta hepatis in a fetus with trisomy 18. Virchows Arch. 2000;436:498-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Tada A, Tanaka T, Takamoto A, Yanai H, Sato S, Kanazawa S. Ectopic thyroid tissue in the adrenal gland: CT and MRI findings. Diagn Interv Imaging. 2016;97:373-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Lim-Dunham JE, Feinstein KA, Yousefzadeh DK, Ben-Ami T. Sonographic demonstration of a normal thyroid gland excludes ectopic thyroid in patients with thyroglossal duct cyst. AJR Am J Roentgenol. 1995;164:1489-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |