Published online May 16, 2021. doi: 10.12998/wjcc.v9.i14.3424
Peer-review started: December 31, 2020
First decision: January 27, 2021
Revised: February 5, 2021
Accepted: March 17, 2021
Article in press: March 17, 2021
Published online: May 16, 2021
Processing time: 118 Days and 17 Hours
Gangrenous cholecystitis is a form of acute cholecystitis which involves gangrenous alterations in the gallbladder wall and it often follows an acute and serious course. We herein report on two cases of very elderly people diagnosed early with gangrenous cholecystitis, who safely underwent laparoscopic cholecystectomy (LC) and both demonstrated a good outcome.
Case 1: An 89-year-old female. She underwent abdominal contrast-enhanced computed tomography (CECT) due to abdominal pain and diarrhea. Her gallbladder wall indicated the absence of contrast enhancement, thus leading to diagnosis of gangrenous cholecystitis and she therefore underwent LC. Although her gallbladder demonstrated diffuse necrosis and it was also partly perforated, she was able to be discharged without any serious complications. Case 2: A 91-year-old female. She made an emergency visit with a chief complaint of abdominal pain. Abdominal CECT revealed swelling of the gallbladder and an ambiguous continuity of the gallbladder wall. She was diagnosed with gan
Although a definite diagnosis of gangrenous cholecystitis is difficult to make prior to surgery, if an early diagnosis can be made and appropriate treatment can be carried out, then even very elderly individuals may be discharged without major complications.
Core Tip: Gangrenous cholecystitis is a form of acute cholecystitis which involves gangrenous alteration in the gallbladder wall and often follows acute and serious course. We report on two cases of very elderly people diagnosed with gangrenous cholecystitis, who safely underwent laparoscopic cholecystectomy and made good progress. If early diagnosis of gangrenous cholecystitis and an appropriate treatment method can be carried out, even very elderly individuals may be discharged without major complications. Our paper will be very informative and useful to the readers of World Journal of Clinical Cases in today's aging society, and will be frequently cited.
- Citation: Inoue H, Ochiai T, Kubo H, Yamamoto Y, Morimura R, Ikoma H, Otsuji E. Laparoscopic cholecystectomy for gangrenous cholecystitis in around nineties: Two case reports. World J Clin Cases 2021; 9(14): 3424-3431
- URL: https://www.wjgnet.com/2307-8960/full/v9/i14/3424.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i14.3424
Gangrenous cholecystitis is defined as cholecystitis involving necrosis and the bleeding of tissues after edematous alterations. The necrosis of tissues is said to be caused by adiemorrhysis of the arterial branches resulting from the oppression of the gallbladder wall due to an elevated biliary internal pressure. Early and appropriate treatment is desirable; however, making a preoperative diagnosis is often difficult. We herein report on two cases of very elderly people diagnosed early with gangrenous cholecystitis, who safely underwent LC and thereafter showed a good outcome.
Case 1: The subject was an 89-year-old female with a chief complaint of abdominal pain and diarrhea.
Case 2: The subject was a 91-year-old female with a chief complaint of right abdominal pain.
Case 1: While hospitalized for a left trochanteric fracture, she suddenly complained of abdominal pain and diarrhea.
Case 2: She visited a local doctor with a chief complaint of right abdominal pain. An abdominal ultrasound revealed swelling of the gallbladder at a local clinic and therefore she was referred to our hospital.
Case 1: She had a past history of Alzheimer's dementia and trochanteric fracture.
Case 2: She had a past history of hypertension, angina, and hyperlipidemia.
Their family histories have nothing notable in both Case 1 and Case 2.
Case 1: Although there were no problems with her vital signs and her abdominal region was flat and soft, she experienced localized pressure pain in her right hypochondrium. She had no obvious rebound tenderness. The Case 2 was the same as the Case 1.
Case 1: Blood biochemistry testing revealed substantial inflammation and elevated hepatic and biliary enzyme levels [C-reactive protein (CRP) 23.5 mg/dL, white blood cell (WBC) 11700/μL, neutrophils (Neut) 81.9%, alkaline phosphatase 535 IU/L].
Case 2: Blood biochemistry testing revealed substantial inflammation and elevated hepatic and biliary enzymes (CRP 15.9 mg/dL, WBC 8800/μl, Neut 87.5%, aspartate aminotransferase 117 IU/L, alanine aminotransferase 101 IU/L).
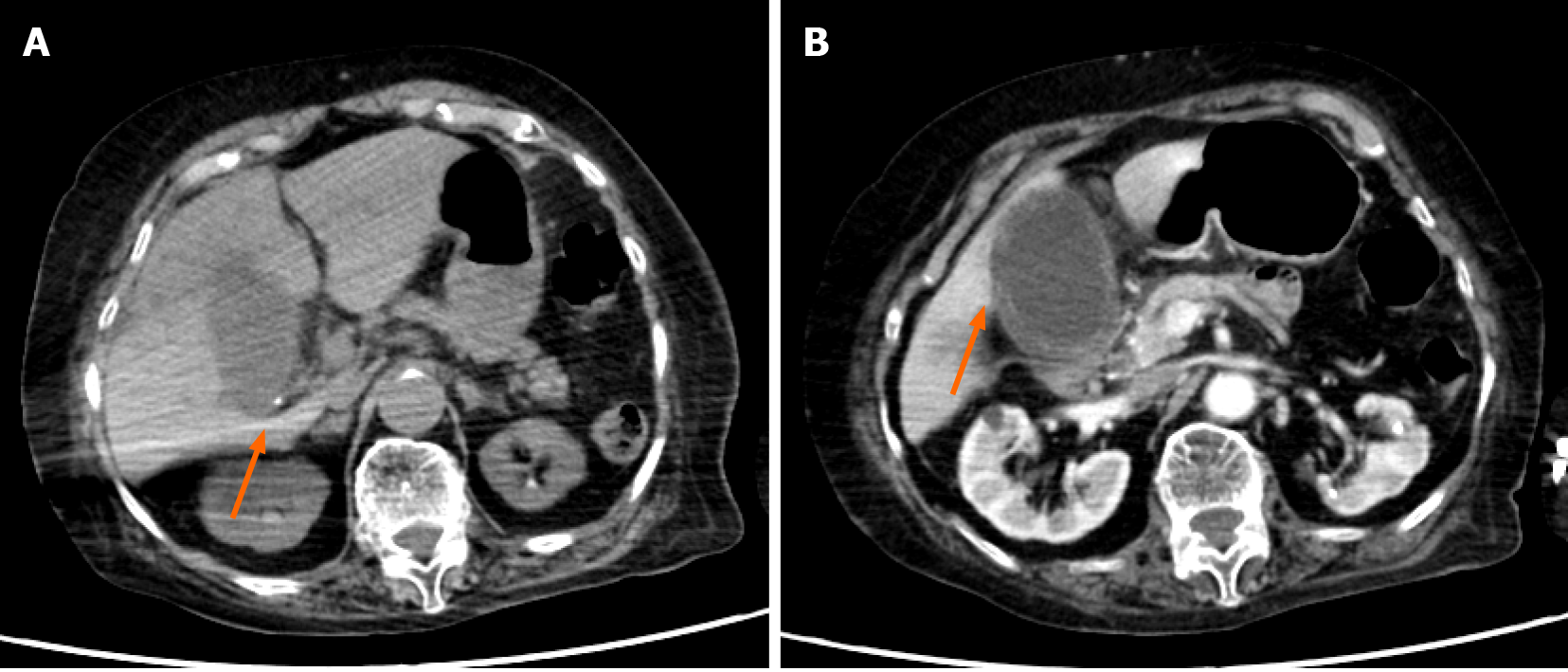
Case 1: An abdominal contrast-enhanced computed tomography (CECT) revealed significant swelling of her gallbladder and asymmetrical wall thickening (Figure 1). The gallbladder wall indicated parts with either poor or no contrast enhancement, with a partial failure of continuity of the mucosa.
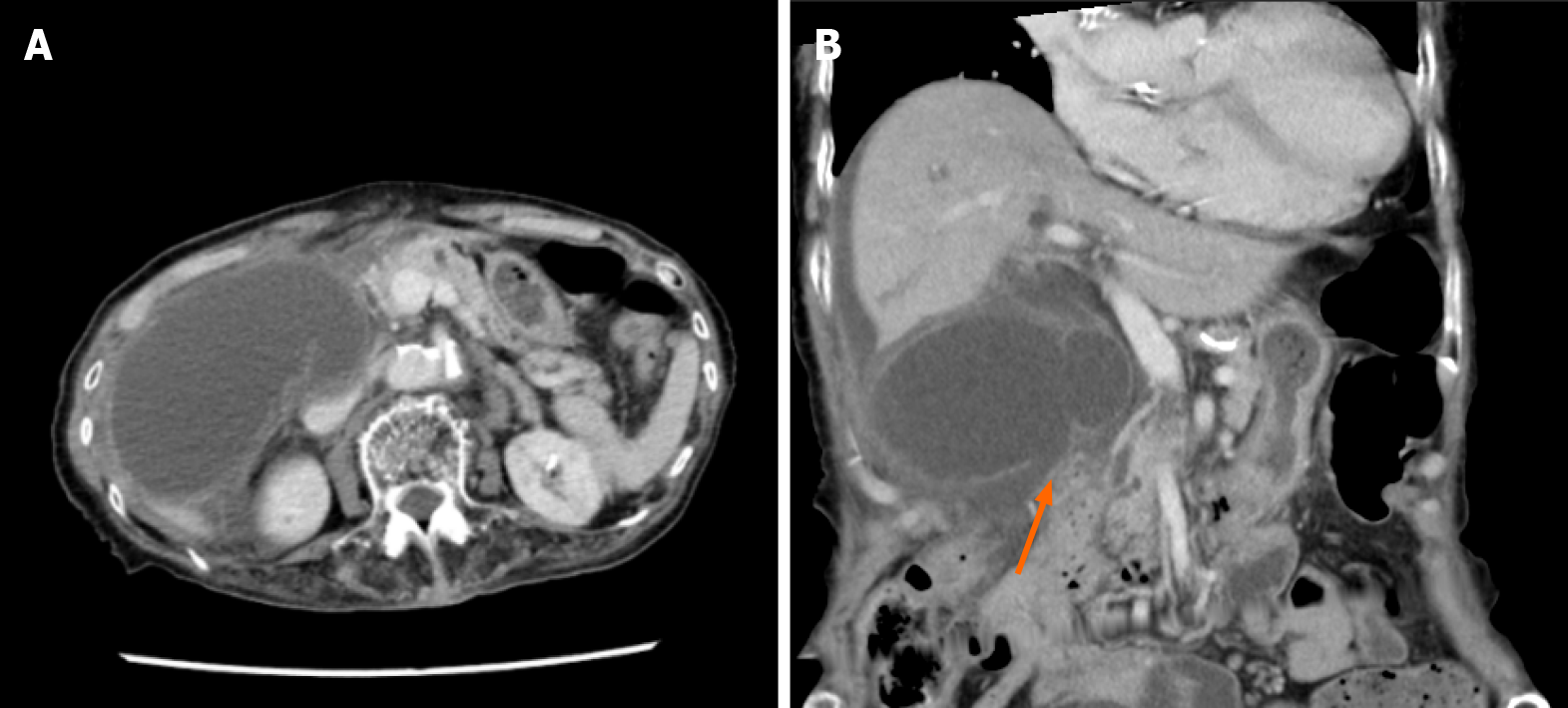
Case 2: An abdominal CECT (Figure 2) revealed significant swelling of her gallbladder and ascites around her liver. There was asymmetrical gallbladder wall thickening and the continuity of part of the wall was ambiguous.
From the above, they were diagnosed with gangrenous cholecystitis and therefore underwent emergency surgery in both Case 1 and Case 2.
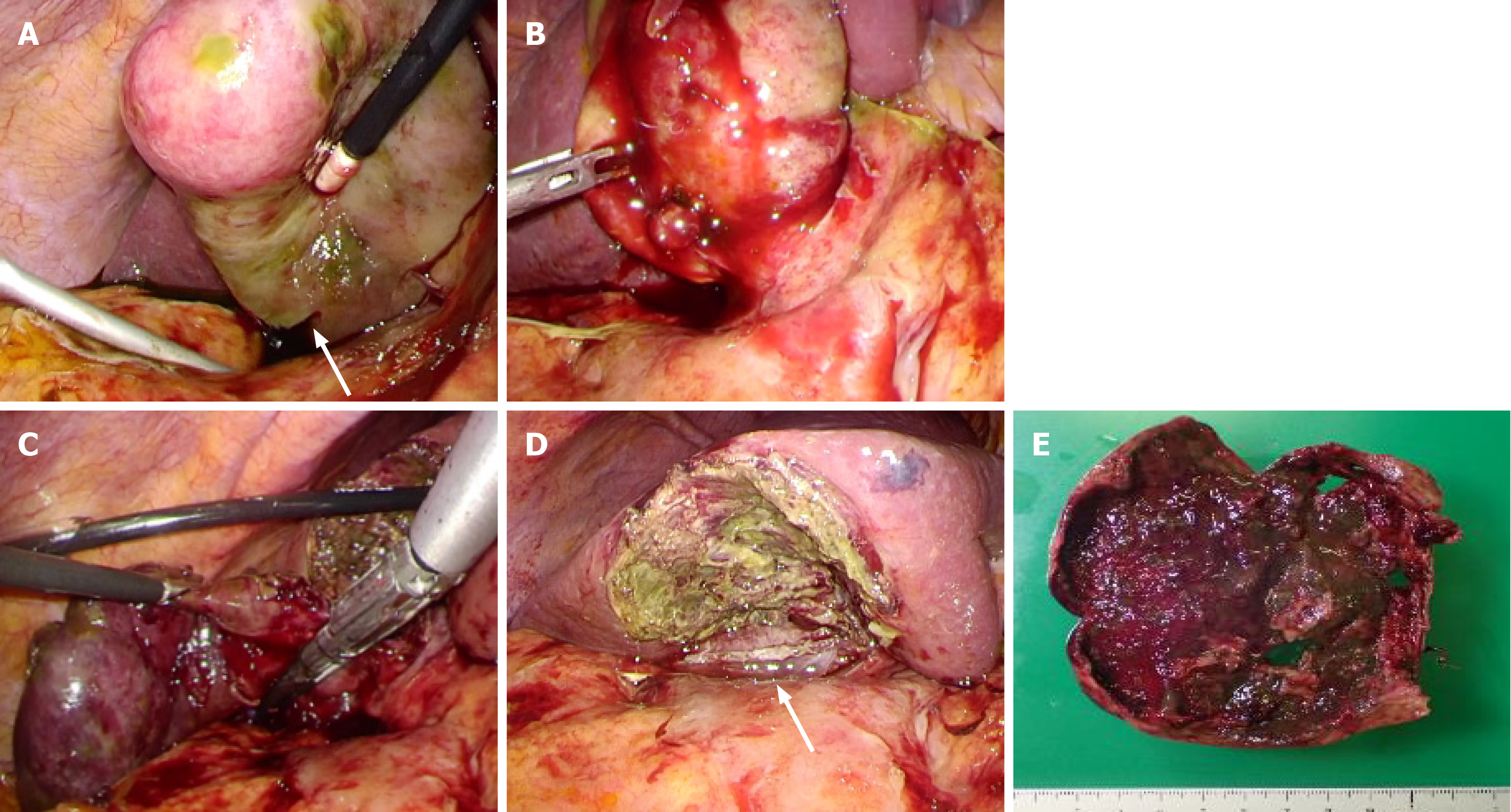
Case 1: The surgery was carried out under laparoscopy using four ports. Inside the abdominal lumen, the omentum was attached around the gallbladder and a part of gallbladder wall was found to demonstrate necrosis. Fragile parts of the gallbladder wall had partially ruptured, thus causing bile to leak (Figure 3A and B). First, we took an approach from the gallbladder neck to identify the critical view of safety (CVS). Since inflammation was substantial and the overall gallbladder was thickened with a finding of necrosis, we believed that this approach was difficult. Therefore, we switched to subtotal cholecystectomy using the fundus first technique. Upon exfoliation from the base to the neck, we cut off the parts without necrosis using an autosuture to extract the specimen (Figure 3C-E).
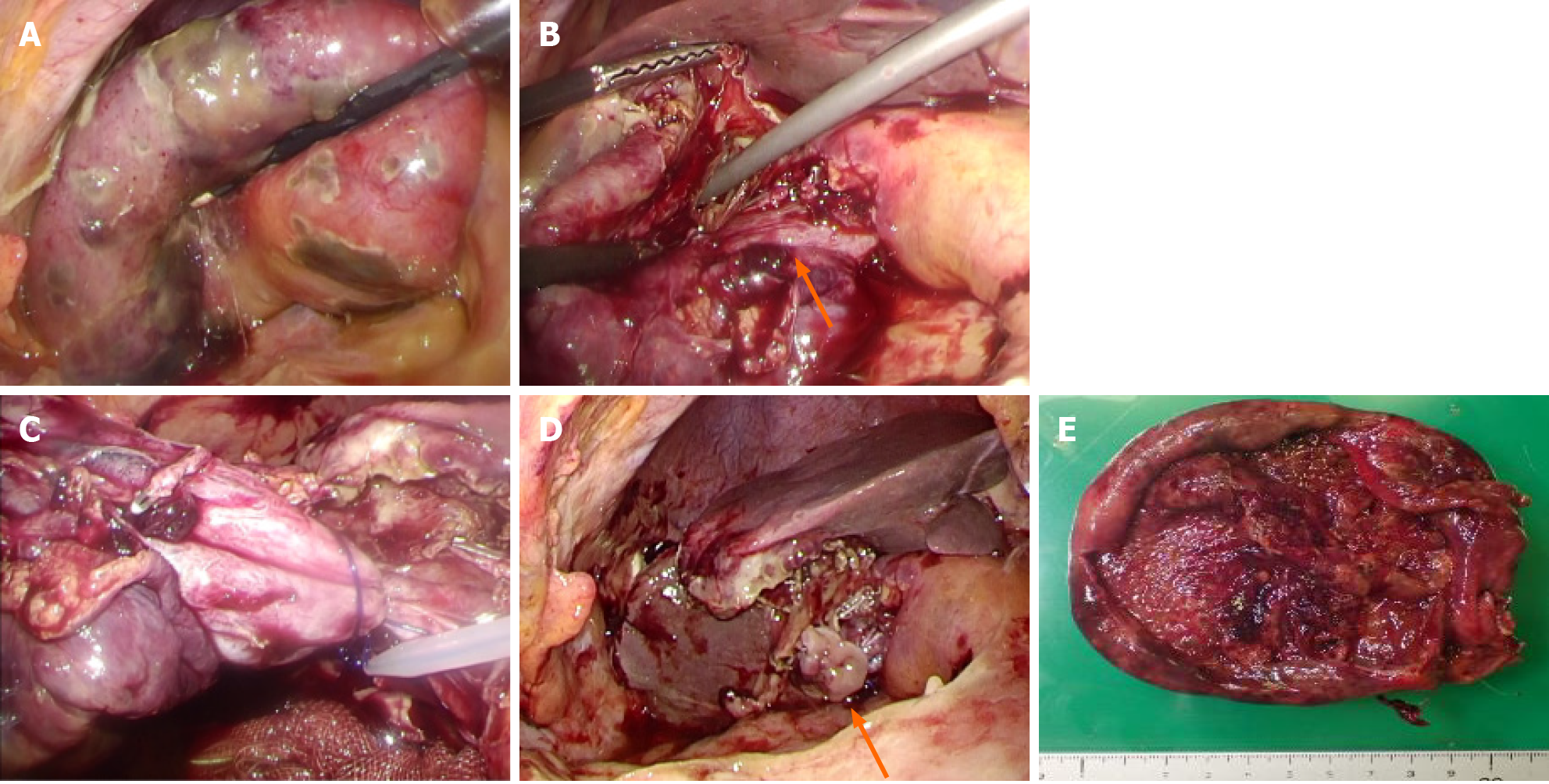
Case 2: The laparoscopic surgery was performed as in Case 1. Inside the abdominal lumen, the gallbladder was very tense with diffuse necrosis, while the gallbladder wall was maintained without leaking bile (Figure 4A). We took an approach from the gallbladder neck, identified CVS and treated the biliary artery (Figure 4B). We then attempted to treat the cystic duct. Since bleeding was substantial and it was difficult to develop the view field, and the duct had thickened substantially due to inflammation, in the end, we chose to use the fundus first technique. Upon exfoliation from the base to the neck, we identified the cystic duct again, however, we deemed that it was difficult to treat it using an autosuture due to the substantial thickness of the duct. We performed double ligature/treatment using a looped absorbable monofilament suture, carried out subtotal cholecystectomy, and extracted the specimen (Figure 4C-E).
Case 1: The patient made good progress following surgery without any major complications and she was discharged home on the 10th disease day. A histopatho
Case 2: She made good progress following surgery and was discharged home on the 10th disease day. A histopathological examination indicated necrosis of all layers with a background of edema and acute inflammatory cellular infiltration.
Ninety percent or more of acute cholecystitis cases are caused by gallstones in the gallbladder[1]. The mechanism of gallstone cholecystitis is as follows: Incarceration and occlusion of the gallstones in the cystic duct causes cholestasis in the gallbladder, leading to damage to the biliary mucosa and activation of inflammatory mediators[2]. On the other hand, cholecystitis sine concrement is caused by either: (1) Cholestasis in the gallbladder; or (2) Blood circulation disorder in the gallbladder wall due to biliary ischemia resulting from atherothrombosis and hyperlipidemia due to arterioscle
The Tokyo guidelines are thought to be useful for the diagnosis and treatment of acute cholecystitis. According to the Tokyo guidelines 2018 (TG18), abdominal ultrasonography is useful for diagnosing acute cholecystitis and defined as the first-choice imaging examination. Moreover, if a blood examination and abdominal ultrasonography cannot lead to a definite diagnosis, then abdominal CECT or abdominal MRI/MRCP is useful. On the other hand, abdominal CECT or abdominal MRI/MRCP is recommended for the diagnosis of gangrenous cholecystitis[4]. Since they have better a diagnostic capability than abdominal ultrasonography, they should be performed if gangrenous cholecystitis is suspected. Gangrenous cholecystitis is characterized by the rarefaction of the gallbladder wall, poor enhancement of the gallbladder wall, elevated concentration of adipose tissue around the gallbladder, and the existence of gas in the gallbladder and gallbladder wall. This case also recognized rarefaction of the gallbladder wall, the poor enhancement of the gallbladder wall, and an elevated concentration of adipose tissue around the gallbladder.
In TG18, the treatment strategy is determined based on the treatment flow chart according to the severity classification as well as the underlying diseases and normal condition of the patient[5]. In other words, the Charlson comorbidity index (CCI) and American Society of Anesthesiologists physical status (ASA-PS) and other predictors are taken into consideration when determining the indications for surgery. Based on these guidelines, biliary drainage may be performed other than surgery for patients with high risk from surgery. We believe the guidelines allowed us to make a more suitable determination that in actual clinical practice. Both cases in this study had Grade II cholecystitis based on the severity criteria and had CCI one point and ASA-PS two points. Therefore, we chose surgery.
The first choice of surgery for acute cholecystitis is LC except if cancer is suspected[6]. It has been reported in randomized controlled trial and meta-analysis that LC has an equivalent treatment outcome with open cholecystectomy along with a "shorter postoperative admission duration,” "lower incidence of complications," and "superiority in mortality and mobidity"[7-12]. On the other hand, it is said to cause more biliary tract damage due to anatomical misidentification compared to laparotomy, which is a problem associated with its introduction[13]. It is said to be essential to identify CVS to avoid biliary tract damage and safely conduct laparoscopic surgery[3,14]. Moreover, it is believed to be important to operate at the anterior Rouvier groove because the right hepatic artery and bile duct right branch are at the posterior Rouvier groove, to perform exfoliation and vessel treatment as close to the gallbladder as possible, and to perform exfoliation while being aware of the subserosa-inner layer, which is said to cause bleeding and damage less frequently[15]. However, for cholecystitis with severe local inflammation such as gangrenous cholecystitis, it is often difficult to perform LC perfectly according to the above procedure. In the above case, it is recommended to consider using laparosonic coagulating shears, adding ports, the fundus first technique[16], subtotal cholecystectomy[17] and open conver
Recently, there has been an increasing number of cases of very elderly people who require surgery as in our cases. It has been reported that because very elderly people sometimes have a chief complaint which is difficult to understand or different from ordinary complaints, consultation or examination tend to be late and the diseases tend to become severe[18]. Since it is difficult to find out the past history and physical findings, blood examinations and imaging examinations are therefore recommended. In our cases, we were able to avoid vital complications by early examinations, a timely diagnosis, and treatment after identifying the symptoms. For surgery involving very elderly people, we believe appropriate and early diagnosis and treatment are necessary to avoid procedural accidents during surgery and postoperative compli
We experienced two cases of very elderly people with gangrenous cholecystitis. Although a definite diagnosis of gangrenous cholecystitis is difficult to make prior to surgery, if an early diagnosis can be made and appropriate treatment methods can be carried out, then even very elderly people may be discharged without any major complications.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bao Y S-Editor: Liu M L-Editor: A P-Editor: Yuan YY
| 1. | Strasberg SM. Clinical practice. Acute calculous cholecystitis. N Engl J Med. 2008;358:2804-2811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 232] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 2. | Akriviadis EA, Hatzigavriel M, Kapnias D, Kirimlidis J, Markantas A, Garyfallos A. Treatment of biliary colic with diclofenac: a randomized, double-blind, placebo-controlled study. Gastroenterology. 1997;113:225-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Barie PS, Eachempati SR. Acute acalculous cholecystitis. Gastroenterol Clin North Am. 2010;39:343-357, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 4. | Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Giménez ME, de Santibañes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:41-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 679] [Article Influence: 97.0] [Reference Citation Analysis (0)] |
| 5. | Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, Iwashita Y, Hibi T, Pitt HA, Umezawa A, Asai K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WS, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, Nakamura M, Horiguchi A, Wakabayashi G, Cherqui D, de Santibañes E, Shikata S, Noguchi Y, Ukai T, Higuchi R, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Shibao K, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25:55-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 490] [Article Influence: 70.0] [Reference Citation Analysis (0)] |
| 6. | Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, Endo I, Umezawa A, Asai K, Suzuki K, Mori Y, Okamoto K, Pitt HA, Han HS, Hwang TL, Yoon YS, Yoon DS, Choi IS, Huang WS, Giménez ME, Garden OJ, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan ACW, Lau WY, Liu KH, Su CH, Misawa T, Nakamura M, Horiguchi A, Tagaya N, Fujioka S, Higuchi R, Shikata S, Noguchi Y, Ukai T, Yokoe M, Cherqui D, Honda G, Sugioka A, de Santibañes E, Supe AN, Tokumura H, Kimura T, Yoshida M, Mayumi T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:73-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 287] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 7. | Kiviluoto T, Sirén J, Luukkonen P, Kivilaakso E. Randomised trial of laparoscopic vs open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 254] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic vs open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 181] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Zacks SL, Sandler RS, Rutledge R, Brown RS Jr. A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97:334-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Flowers JL, Bailey RW, Scovill WA, Zucker KA. The Baltimore experience with laparoscopic management of acute cholecystitis. Am J Surg. 1991;161:388-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 94] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L. Randomized clinical trial of open vs laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg. 2005;92:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 143] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 12. | Purkayastha S, Tilney HS, Georgiou P, Athanasiou T, Tekkis PP, Darzi AW. Laparoscopic cholecystectomy vs mini-laparotomy cholecystectomy: a meta-analysis of randomised control trials. Surg Endosc. 2007;21:1294-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Zha Y, Chen XR, Luo D, Jin Y. The prevention of major bile duct injures in laparoscopic cholecystectomy: the experience with 13,000 patients in a single center. Surg Laparosc Endosc Percutan Tech. 2010;20:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010;211:132-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 332] [Article Influence: 22.1] [Reference Citation Analysis (1)] |
| 15. | Honda G, Hasegawa H, Umezawa A. Universal safe procedure of laparoscopic cholecystectomy standardized by exposing the inner layer of the subserosal layer (with video). J Hepatobiliary Pancreat Sci. 2016;23:E14-E19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Tartaglia N, Cianci P, Di Lascia A, Fersini A, Ambrosi A, Neri V. Laparoscopic antegrade cholecystectomy: a standard procedure? Open Med (Wars). 2016;11:429-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. Subtotal Cholecystectomy-"Fenestrating" vs "Reconstituting" Subtypes and the Prevention of Bile Duct Injury: Definition of the Optimal Procedure in Difficult Operative Conditions. J Am Coll Surg. 2016;222:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 200] [Article Influence: 20.0] [Reference Citation Analysis (1)] |
| 18. | Launay-Savary MV, Rainfray M, Dubuisson V. Emergency gastrointestinal surgery in the elderly. J Visc Surg. 2015;152:S73-S79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |