Published online May 16, 2021. doi: 10.12998/wjcc.v9.i14.3411
Peer-review started: December 3, 2020
First decision: January 10, 2021
Revised: January 24, 2021
Accepted: March 20, 2021
Article in press: March 20, 2021
Published online: May 16, 2021
Processing time: 147 Days and 2.6 Hours
Spontaneous spinal epidural hematoma is a rare neurosurgical emergency.
A 53-year-old healthy woman suffered from complete paraplegia in both legs and loss of all sensation below the xiphoid process. She was diagnosed as acute spontaneous thoracic epidural hematoma caused by an intraspinal lymphan
This study reports a case of acute spontaneous thoracic epidural hematoma caused by an intraspinal lymphangioma with well recovery after surgical intervention.
Core Tip: This case suffered from acute spontaneous thoracic epidural hematoma caused by an intraspinal lymphangioma presenting with complete paraplegia in both legs and loss of all sensation below the xiphoid process. A posteriorly epidural space-occupying lesion at the T4-T8 level of the spinal canal was relieved via decompressive laminectomy in time and the symptoms recovered well within one month.
- Citation: Chia KJ, Lin LH, Sung MT, Su TM, Huang JF, Lee HL, Sung WW, Lee TH. Acute spontaneous thoracic epidural hematoma associated with intraspinal lymphangioma: A case report. World J Clin Cases 2021; 9(14): 3411-3417
- URL: https://www.wjgnet.com/2307-8960/full/v9/i14/3411.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i14.3411
Lymphangiomas that present as spinal soft tissue tumors in the epidural space are extremely uncommon[1-5]. However, these spontaneous spinal epidural hematomas can be a rare cause of spinal cord compression, accounting for less than 1% of spinal space-occupying lesions[6]. In this report, we present probably the first reported case of an acute spontaneous thoracic epidural hematoma caused by an intraspinal lymphangioma in a 53-year-old female patient.
A 53-year-old healthy woman was admitted to our emergency room with complete paraplegia in both legs and loss of all sensation below the xiphoid process (T5 level).
One day before admission, she had taken a walk with her husband along the dam in Kaohsiung. While walking at that time, she was only wearing a backpack and did not do any specific stretching exercises. After the walk, the patient felt a slight discomfort over her back. By noon on the next day, she complained of tightness over her bilateral chest wall, around the level of the xiphoid process. She denied straining, lifting, crying, sneezing, or coughing in the past three days. On arrival at the emergency room, 27 h after the walk, the muscle power in her lower extremities was 0/5 strength bilaterally, and she experienced no sensation below the xiphoid process. She also had difficulty in voiding her bladder. Vital signs at presentation were body temperature (BT): 36.6 ℃, respiratory rate (RR): 17/min, pulse rate (PR): 82/min and blood pressure (BP): 156/82 mmHg. A neurological examination revealed increased deep tendon reflexes over the right and left knees and ankles.
The patient was not receiving any anticoagulation therapy, and laboratory test results, including a complete blood count, chemistry panel, and coagulation profile, were all within normal limits.
The patient denied related past illness or any history of anticoagulation therapy.
The patient denied related personal and family history.
Vital signs at presentation were BT: 36.6 ℃, RR: 17/min, PR: 82/min and BP: 156/82 mmHg. A neurological examination revealed increased deep tendon reflexes over the right and left knees and ankles.
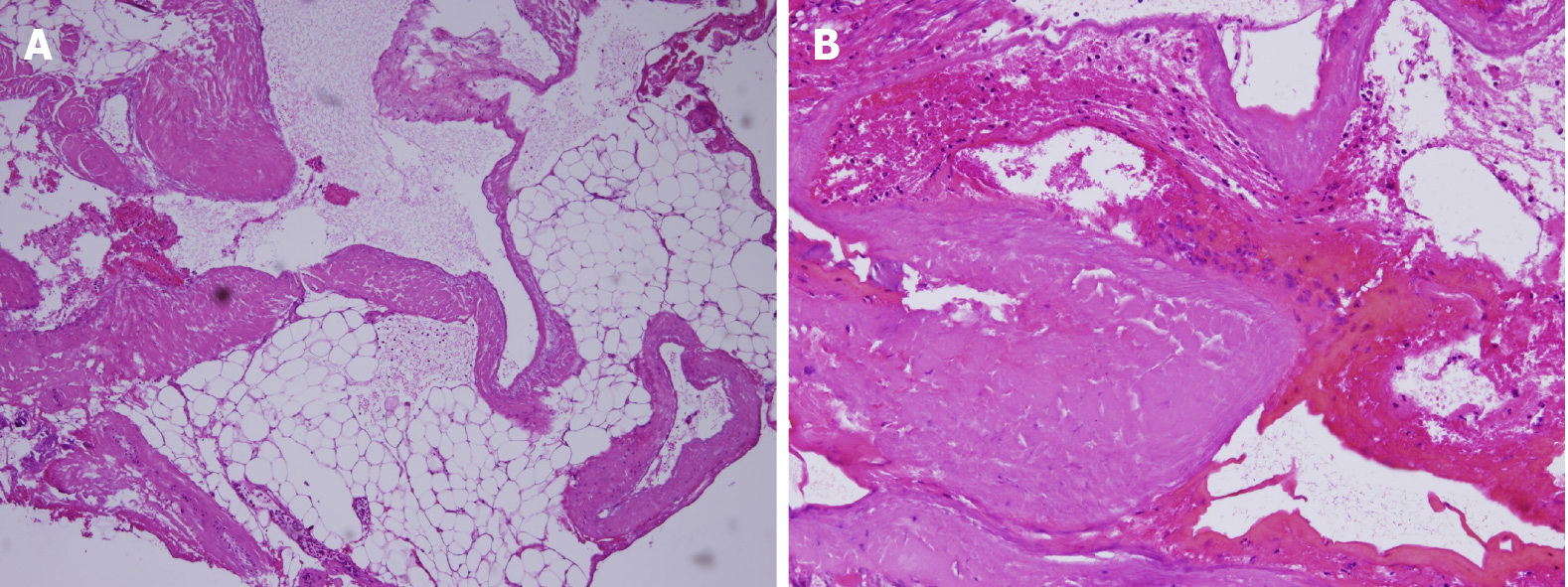
Laboratory test results, including a complete blood count, chemistry panel, and coagulation profile, were all within normal limits (platelets: 206000/μL, PT: 10.1 s, INR: 0.96, and APTT: 28.2 s). Microscopic examination of the intrathoracic abnormally dilated vascularities showed a proliferation of varying sized and focally dilated vascular channels filled with blood and lymphatic substance (Figure 1). The pathologic diagnosis was lymphangioma.
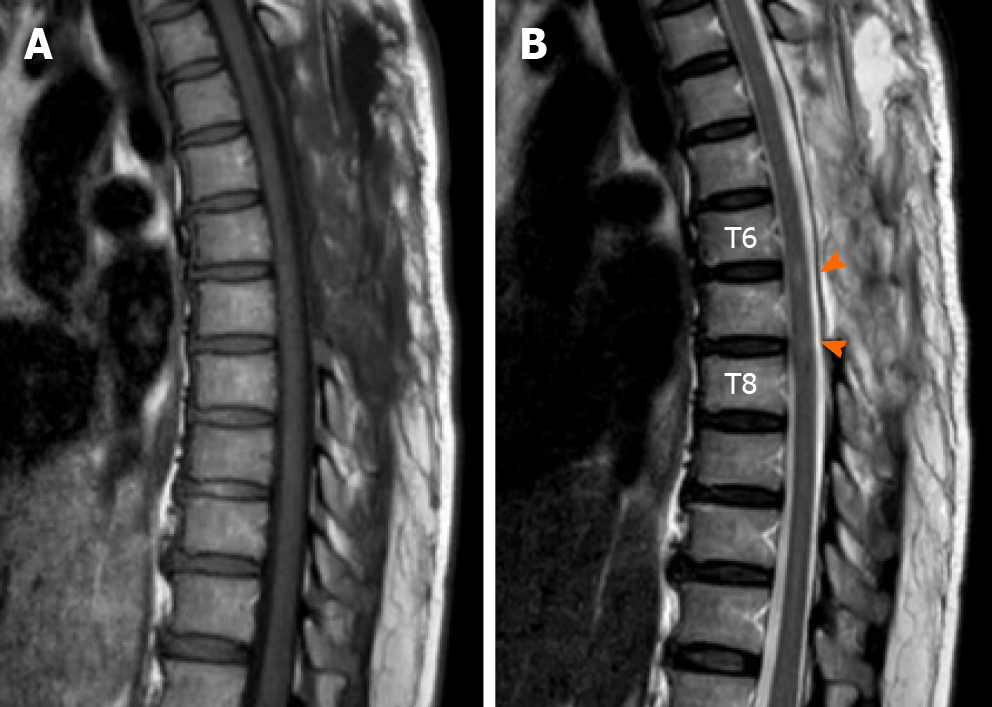
Magnetic resonance imaging (MRI) of the thoracic spine, performed one hour after abrupt onset of complete paraplegia, revealed the presence of a posteriorly epidural space-occupying lesion (7.6 mm × 18 mm × 85 mm in size) at the T4-T8 level of the spinal canal. The lesion caused obliteration of the cerebrospinal fluid (CSF) signal at the T6-T7 level thecal sac, with mildly thin peripheral enhancement (Figure 2). The scanned field showed neither a definite signal intensity changes in the spinal cord nor a significant bone marrow signal change in the vertebral body.
Based on magnetic resonance imaging, intraoperative findings, and pathological examination, acute thoracic epidural hematoma associated with intraspinal lym
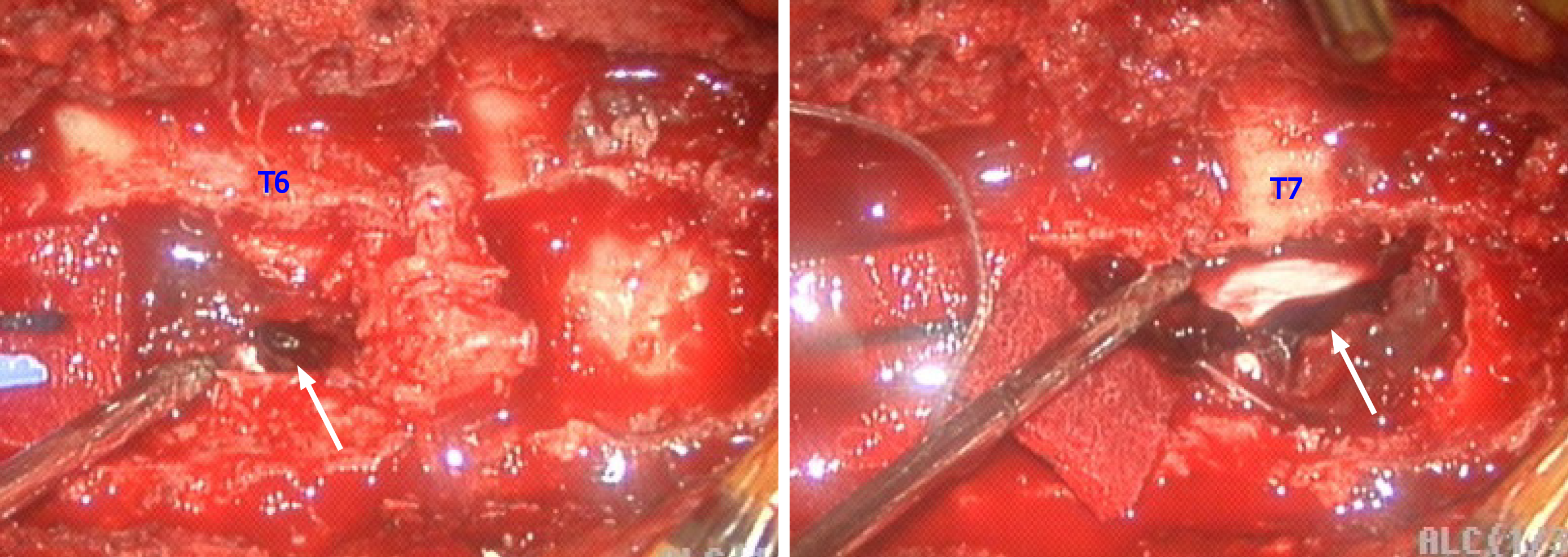
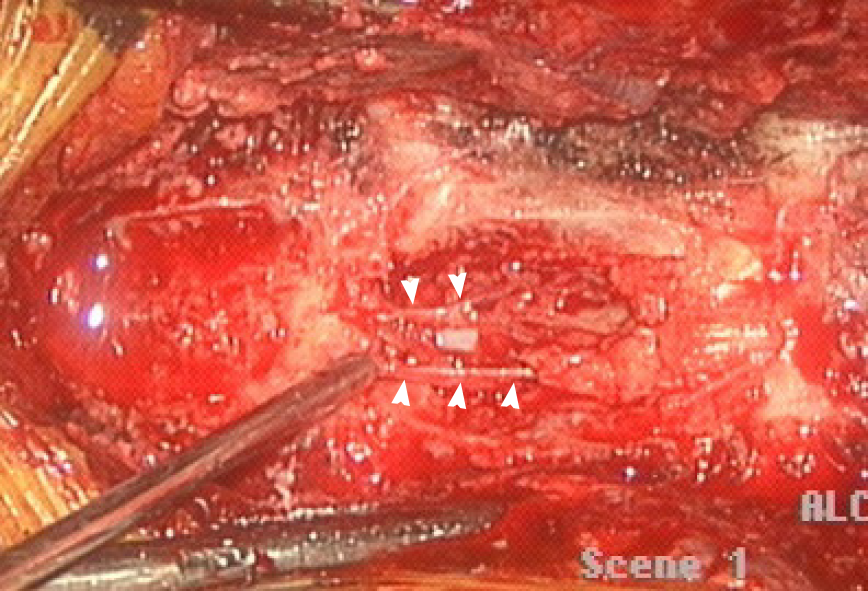
At the sixth hour following abrupt onset of complete paraplegia, a decompressive laminectomy was performed from the T4 to T7 levels. This procedure exposed an acute epidural hematoma in the T4-T7 region, predominantly at T6-T7 (Figure 3). During the surgery, numerous epidural vessels, with some abnormally dilated vascularities, were found at the T4 to upper T6 levels (Figure 4).
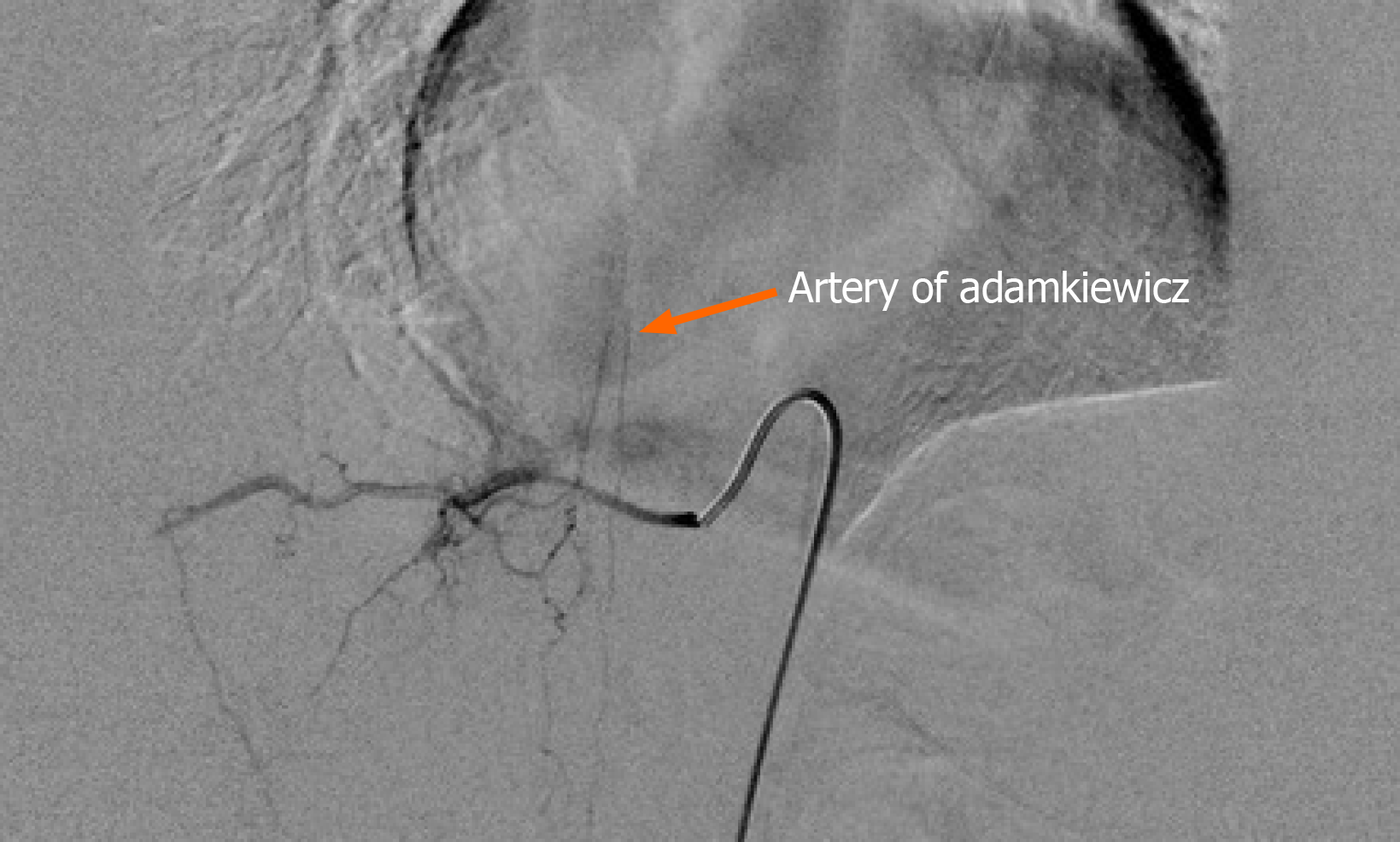
Postoperative spinal angiography performed at 3 d following the thoracic spinal surgery showed the artery of Adamkiewicz arising from the right T10 radiculo
A follow-up MRI of the thoracic spine performed 7 d postoperatively revealed no residual gross epidural hematoma and no remaining spinal cord compression except for a faint T2 hyperintense signal at the T6-T8 level spinal cord (Figure 6). On the seventh postoperative day, the patient experienced substantial recovery of the muscle power in both legs (grade 4). The sensation of proprioception, pain, pin-prick, and vibration also returned to normal. At discharge (1 mo after the operation), she regained complete sphincteric control.
Nontraumatic spinal epidural hematoma was first described by Jackson in 1869[7]. Spontaneous spinal epidural hematoma (SSEH) is a rare disease entity that is usually associated with underlying hematological disorders or other predisposing condi
Lymphangiomas are congenital lymphatic malformations that are usually discovered in early childhood. They have no racial or gender predilection[9]. In up to 10% of patients, the malformations may not be discovered until adulthood, with only a few cases appearing as late as the fifth decade of life. Frequently, a lymphangioma manifests as an asymptomatic soft or semi-firm mass. Although these lesions tend to surround and sometimes invade normal anatomic structures, they have no malignant potential[10]. However, lymphangiomas presenting as a spinal soft tissue tumor in the epidural space are extremely rare[1-5]. Surgical excision is the treatment of choice, and recurrence rates as high as 15% have been reported[11].
SSEH is a rare, but disabling or even fatal, condition. The annual incidence of SSEH has been estimated at 0.1 per 100000[12]. The male/female ratio is 1.5:1, and most cases occur between the ages of 50 and 80 years[13]. The etiology is unknown, but predis
Currently, MRI is the main investigative tool for spinal soft tissue tumors, and it allows a prompt diagnosis of a spinal epidural hematoma. On MRI, the hematoma appears as an isointense area on the spinal cord on T1-weighted images obtained within the first 24 h. After 36 h, it appears as a hyperintense or mixed signal intensity area on the spinal cord on T2-weighted images[15]. In addition to specific signal changes, contrast enhancement pattern and morphological findings on MR images can differentiate acute SSEH from spinal epidural neoplastic mass[16]. Pan et al[17] reported that, from the clinical viewpoint, most patients with spinal epidural hematomas undergo some degree of irreversible cord injury by the time the hematoma is resorbed. The prognosis of SSEH correlates with the size and level of hematoma, preoperative neurological status of the patient, and the time interval between the onset of symptoms and surgery[18,19]. Therefore, immediate surgical decompression remains the primary consideration in the management of patients with progressive neurological deficits.
Acute spontaneous spinal epidural hematoma caused by an intraspinal lymphangioma is a very rare occurrence. Neurosurgeons should consider the possibility of SSEH when their patients show neurologic symptoms related to the spinal cord or root compression. In the event of a thoracic epidural hematoma, prompt surgical inter
Manuscript source: Unsolicited manuscript
Specialty type: Clinical neurology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anghelescu A, Bains L S-Editor: Zhang H L-Editor: A P-Editor: Yuan YY
| 1. | Chu M, Li G, Wei L, Lin Y, Qi J, Wang C, Zhao S. A rare case of cavernous lymphangioma in the epidural space of the cervicothoracic spine. Spine (Phila Pa 1976). 2007;32:E48-E51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Aslan K, Bekci T, Gunbey HP, Incesu L, Turgut E. A rare cause of backache: epidural lymphangioma of the cervicothoracic spine. Spine J. 2015;15:1900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Fattahi A, Taheri M, Majdi M. Lymphangioma of the Thoracic Spine with Epidural Compression: A Case Report. Iran J Med Sci. 2019;44:172-175. [PubMed] |
| 4. | Ha BY, Park JB, Kim YM, Lyo IU. Lymphangioma in the epidural space of the thoracic spine. J Korean Neurosurg Soc. 2010;47:403-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Jiang YG, Xiang J, Zhang L. Intraspinal lymphangioma: 2 case reports and literature review. Surg Neurol. 2006;66:430-436; discussion 436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Alexiadou-Rudolf C, Ernestus RI, Nanassis K, Lanfermann H, Klug N. Acute nontraumatic spinal epidural hematomas. An important differential diagnosis in spinal emergencies. Spine (Phila Pa 1976). 1998;23:1810-1813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Jackson R. Case of spinal apoplexy. Lancet. 1869;94:5-6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 131] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003;26:1-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 474] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 9. | Ersoy AO, Oztas E, Saridogan E, Ozler S, Danisman N. An Unusual Origin of Fetal Lymphangioma Filling Right Axilla. J Clin Diagn Res. 2016;10:QD09-QD11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Zadvinskis DP, Benson MT, Kerr HH, Mancuso AA, Cacciarelli AA, Madrazo BL, Mafee MF, Dalen K. Congenital malformations of the cervicothoracic lymphatic system: embryology and pathogenesis. Radiographics. 1992;12:1175-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 116] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Glasson MJ, Taylor SF. Cervical, cervicomediastinal and intrathoracic lymphangioma. Prog Pediatr Surg. 1991;27:62-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 173] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 13. | Foo D, Rossier AB. Preoperative neurological status in predicting surgical outcome of spinal epidural hematomas. Surg Neurol. 1981;15:389-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 200] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Liao CC, Lee ST, Hsu WC, Chen LR, Lui TN, Lee SC. Experience in the surgical management of spontaneous spinal epidural hematoma. J Neurosurg. 2004;100:38-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. AJNR Am J Neuroradiol. 1999;20:1365-1372. [PubMed] |
| 16. | Chang FC, Lirng JF, Chen SS, Luo CB, Guo WY, Teng MM, Chang CY. Contrast enhancement patterns of acute spinal epidural hematomas: a report of two cases. AJNR Am J Neuroradiol. 2003;24:366-369. [PubMed] |
| 17. | Pan G, Kulkarni M, MacDougall DJ, Miner ME. Traumatic epidural hematoma of the cervical spine: diagnosis with magnetic resonance imaging. Case report. J Neurosurg. 1988;68:798-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Liu Z, Jiao Q, Xu J, Wang X, Li S, You C. Spontaneous spinal epidural hematoma: analysis of 23 cases. Surg Neurol. 2008;69:253-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Schoonjans AS, De Dooy J, Kenis S, Menovsky T, Verhulst S, Hellinckx J, Van Ingelghem I, Parizel PM, Jorens PG, Ceulemans B. Spontaneous spinal epidural hematoma in infancy: review of the literature and the "seventh" case report. Eur J Paediatr Neurol. 2013;17:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |