Published online May 16, 2021. doi: 10.12998/wjcc.v9.i14.3379
Peer-review started: November 9, 2020
First decision: February 12, 2021
Revised: February 22, 2021
Accepted: March 12, 2021
Article in press: March 12, 2021
Published online: May 16, 2021
Processing time: 167 Days and 20.8 Hours
The ampulla of Vater is an opening at the confluence of the common bile duct and pancreatic duct. It is located in the second portion of the duodenum. An ectopic papilla of Vater is an anomalous termination. Few cases have been reported. We report the rare case of a man with an ectopic ampulla of Vater in the pylorus.
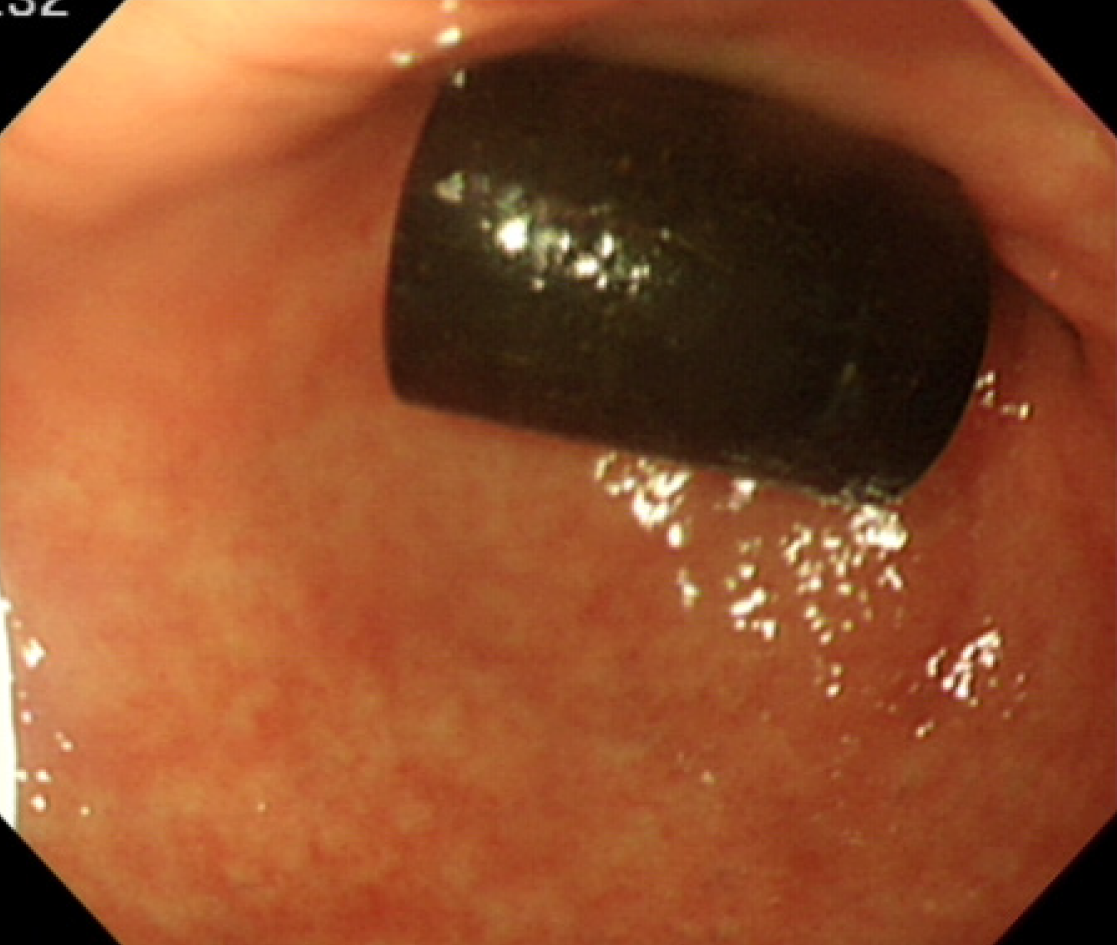
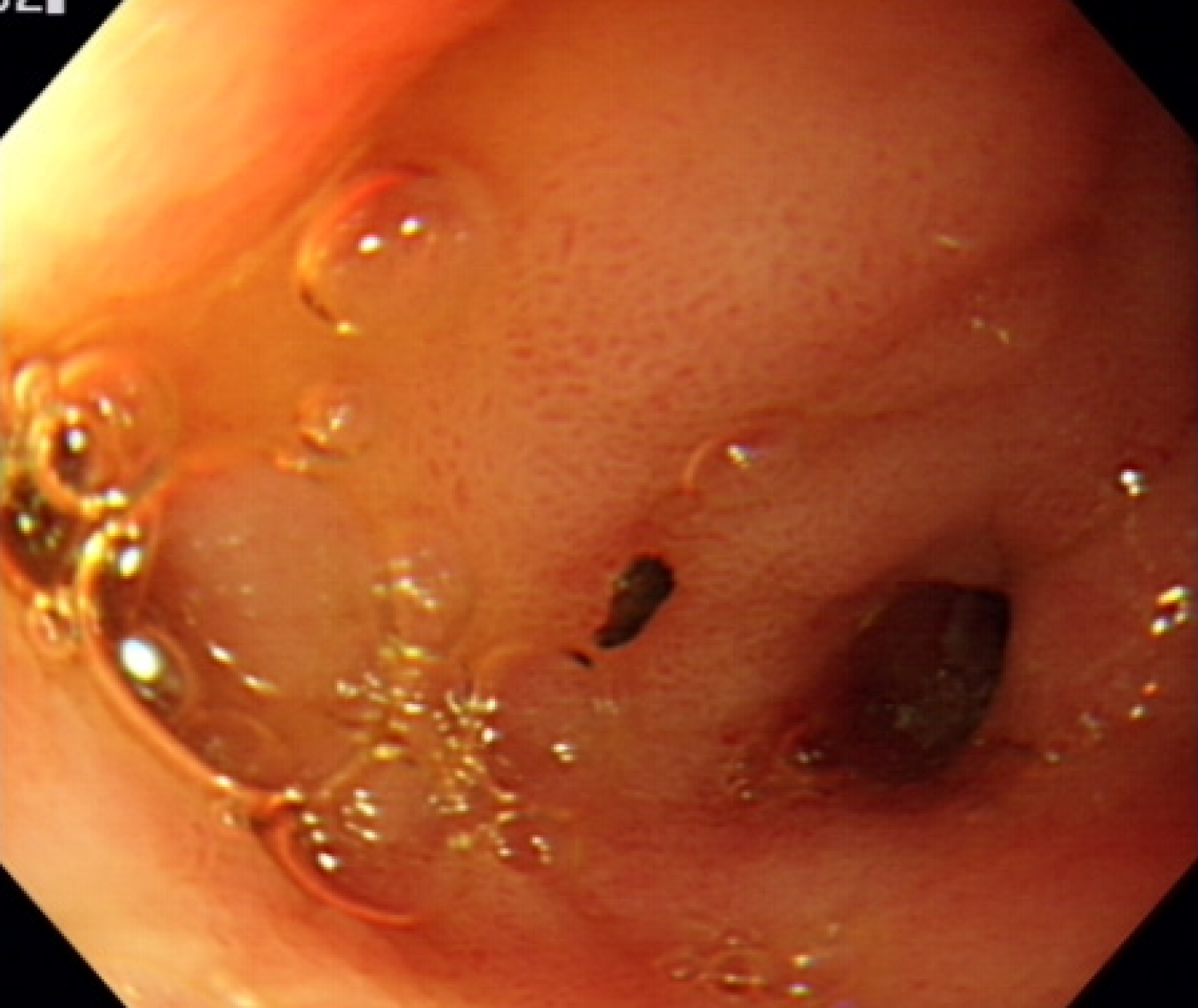
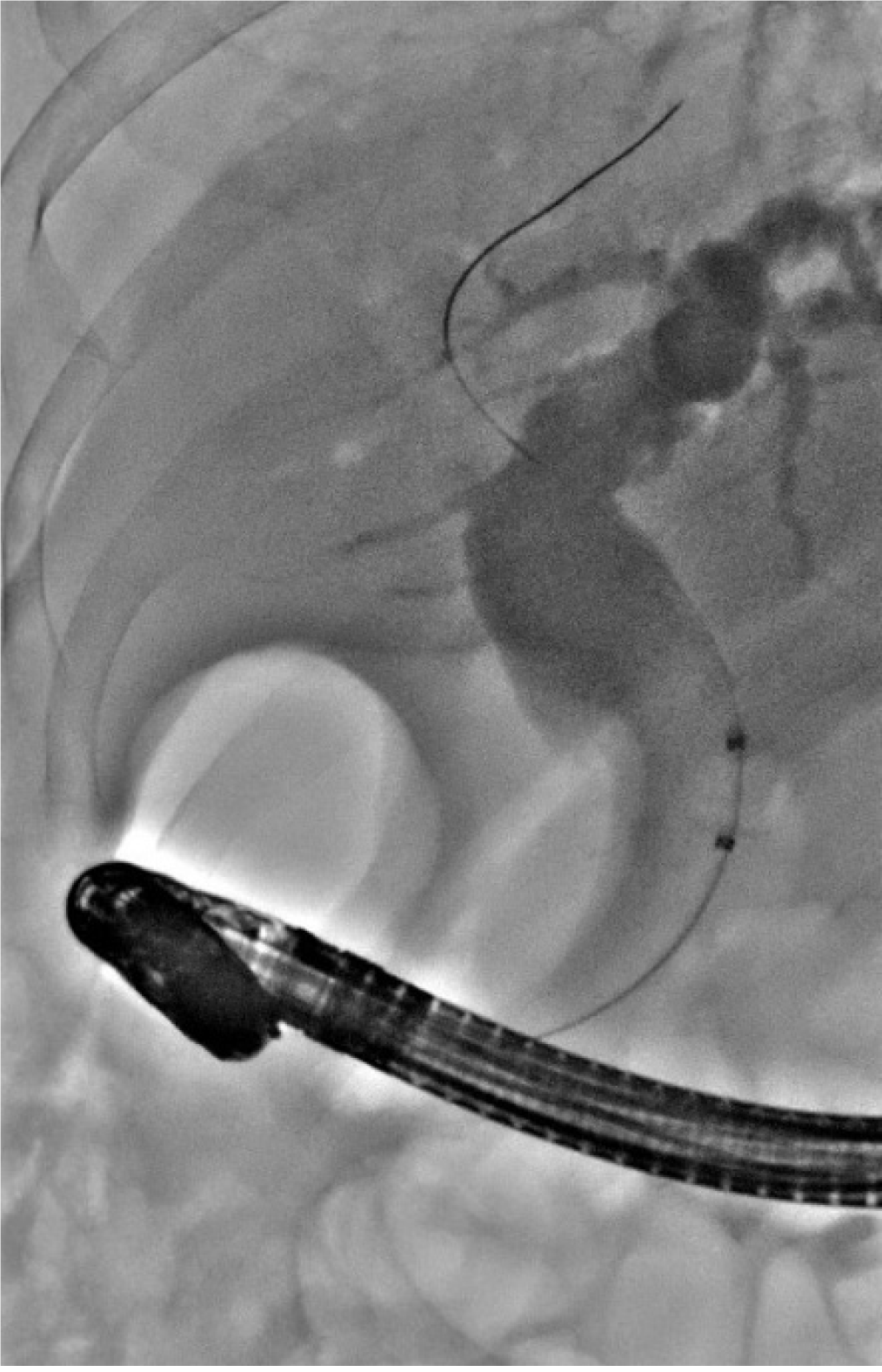
An 82-year-old man had experienced abdominal pain and fever with chills 1 d before his presentation. A computed tomography scan of the abdomen demonstrated dilatation of the common bile duct approximately 2.2 cm in width. Gas retention was found in his intrahepatic ducts. Acute cholangitis with pneumobilia was identified, and he was hospitalized. Esophagogastroduo-denoscopy and endoscopic retrograde cholangiopancreatography disclosed no ampulla of Vater in the second portion of the duodenum. Moreover, a capsule-like foreign body (pharmaceutical desiccant) approximately 1 cm × 2 cm in size was found at the gastric antrum and peri-pyloric region. After the foreign body was removed, one orifice presented over the pyloric ring in the stomach, a suspected ectopic ampulla of Vater. Subsequently, sludge in the common bile duct was cleaned, and balloon dilatation was performed. The general condition improved daily. The patient was discharged in a stable condition and followed in our outpatient department.
This case involved an ampulla of Vater in an unusual location. Endoscopic retrograde cholangiopancreatography with balloon dilatation is the main treatment recommended and performed.
Core Tip: Ectopic papilla of Vater is scarcely reported. Potential locations of ectopic papilla are the stomach, pyloric canal, duodenal bulb, or third or fourth portion of the duodenum. Anomalous termination in the stomach is rare. Although this anatomy may mislead endoscopic retrograde cholangiopancreatography operators, this nonetheless constitutes a safe and common therapeutic procedure. When no ampulla of Vater is detected in the second portion of the duodenum, ectopic papilla of Vater should be considered.
- Citation: Lee HL, Fu CK. Acute cholangitis detected ectopic ampulla of Vater in the antrum incidentally: A case report. World J Clin Cases 2021; 9(14): 3379-3384
- URL: https://www.wjgnet.com/2307-8960/full/v9/i14/3379.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i14.3379
The ampulla of Vater is an opening at the confluence of the common bile duct and pancreatic duct. It is located in the second portion of the duodenum and is surrounded by the sphincter of Oddi. Anomalous termination of the common bile duct, known as ectopic papilla of Vater, is predominant in men, though uncommon and potentially related to abnormal embryogenetic formation. The reported incidence of anomalous termination of bile duct termination is approximately 5.6% to 23.0%[1]. The incidence can be underestimated because of the limited number of cases, and the condition remains undetected until symptoms present. Increases in incidence and in prevalence may be due to the increasingly common use of endoscopic retrograde cholangiopan-creatography (ERCP). Potential locations for ectopic papilla are the stomach, pyloric canal, duodenal bulb, and the third or fourth portion of the duodenum[2]. In most cases, it remains undetected until symptoms present. Complications such as pancreatitis, biliary tract infection, and hyperamylasemia are mild and may be alleviated by conventional therapies[3]. Thus, we report the case of a man with an ectopic ampulla of Vater in the pylorus.
An 82-year-old man experienced abdominal pain and fever with chills 1 d before his presentation.
The severity of these symptoms increased gradually. Nausea and vomiting were also subsequently noted.
The patient had a history of hypertension. The patient underwent surgical repair due to bowel perforation and laparoscopic cholecystectomy due to cholecystitis.
There was no significant personal or family history.
The patient’s temperature was 38.6 °C, his heart rate was 101 bpm, his respiratory rate was 22 breaths per minute, and his blood pressure was 112/84 mmHg. Yellow skin discoloration and tenderness over the upper abdominal region were noted.
The patient’s leukocyte count was 14300/μL with 85.9% neutrophils, 7.4% lymphocytes, and 6.2% monocytes. Other blood tests revealed impaired liver function, reporting aspartate aminotransferase: 181 U/L, alanine aminotransferase: 131 U/L, total bilirubin: 2.3 mg/dL, and C-reactive protein: 12.48 mg/dL. The bile culture yielded Enterococcus faecium, Escherichia coli, Klebsiella pneumoniae, and Bacteroides fragilis.
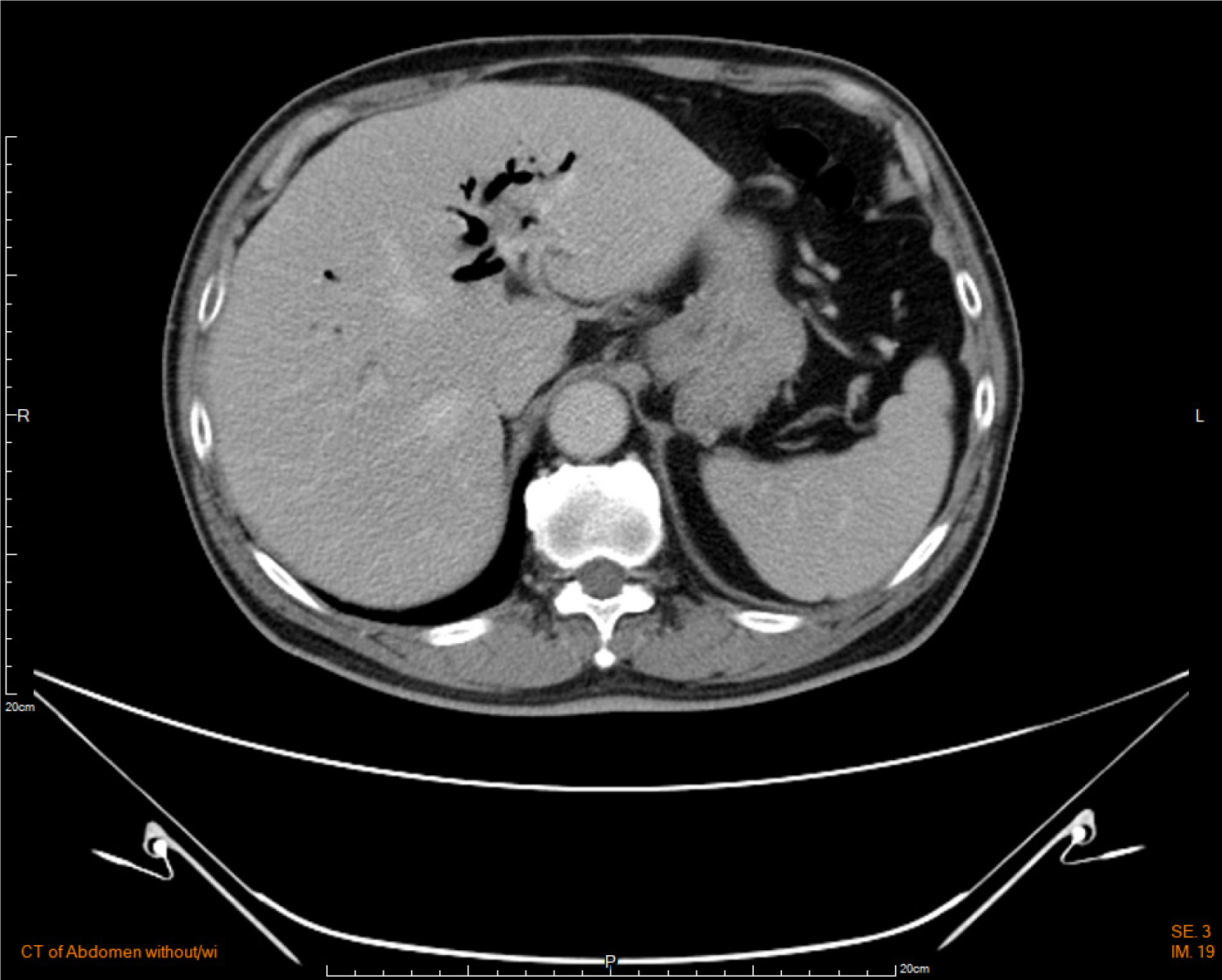
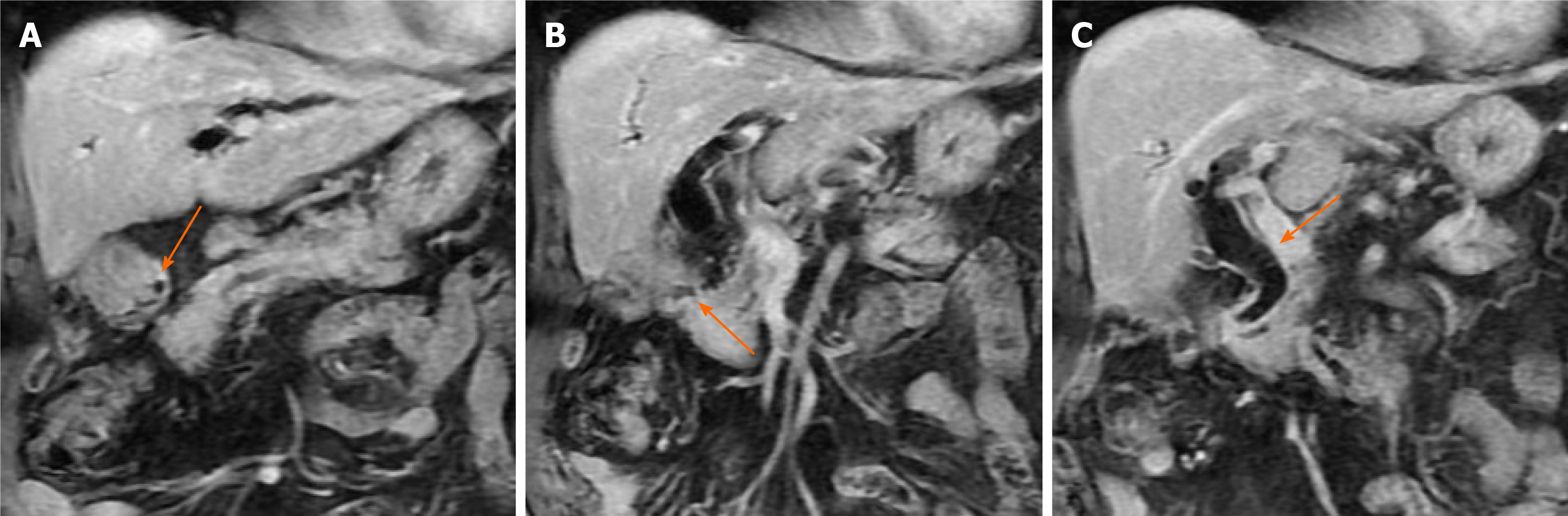
Computed tomography of the abdomen demonstrated dilatation of the common bile duct measuring approximately 2.2 cm. Gas retention was present in the intrahepatic ducts (Figure 1). Cholangitis with pneumobilia was suggested.
The patient underwent percutaneous transhepatic cholangiography and drainage and collection of bile for culture. We also performed esophagogastroduodenoscopy and ERCP, which disclosed a gastric ulcer over the antrum and pylorus stenosis with partial gastric outlet obstruction. However, the ampulla of Vater was not located in the second portion of the duodenum. Moreover, a capsule-like foreign body (pharmaceu
The final diagnosis of the presented case was acute cholangitis with an ectopic ampulla of Vater.
Initially, we prescribed ceftriaxone (2 g IV QD) as an empirical antibiotic. After percutaneous transhepatic cholangiography and drainage, epigastric pain improved. Nevertheless, high fever was persistent, and we therefore consulted an infectologist and shifted the antibiotic treatment to Doripenam (250 mg IV Q8H) and vancomycin (1 g IV Q12H). These antibiotics were effective for all bile cultures. Because obstruction of the common bile duct was resolved and antibiotics were effective according to bile culture results, the patient’s fever gradually subsided, and sepsis was brought under control.
The patient’s general condition improved daily. He was discharged in a stable condition and follow-ups continued in our outpatient department. We also educated the patient about lifestyle modification and avoidance of the supine position immediately after meals or eating before sleep. After doing so, there was no recurrent cholangitis.
Ectopic papilla of Vater is an underdiagnosed disease, and anomalous termination in the stomach is rare[2,4]. A retrospective study with 6133 enrollees who had received ERCP in Taiwan between 1988 and 2010 reported an incidence of approximately 0.13%, corresponding to the prevalence rate of Taiwan’s general population[2].
The hepatic diverticulum is usually divided into the hepatic pars and cystic pars during embryogenesis. The hepatic pars develops into both the liver and hepatic ducts, whereas the cystic pars develops into the gallbladder and cystic duct. The common bile duct originates in the hepatic antrum, which is the common area of the hepatic diverticulum[4]. Anomalies in biliary tree drainage can cause early subdivision and disruption of the hepatic diverticulum, which later develops into a duct emptying into the stomach[5]. However, the anomalous embryogenetic formation process remains unclear and is not fully understood.
The presenting clinical symptoms include epigastric abdominal pain, dyspepsia, nausea, vomiting, fever, and jaundice. These may be associated with the absence of a sphincter, which allows the passage of gastroduodenal contents into the main bile duct, potentially causing biliary obstruction and even cholangitis[4]. In our case, reducing gastric contents or volume decreased the possibility for debris refluxing into the common bile duct. In addition, prokinetic drugs could be helpful by increasing the motility of the stomach and accelerating gastric emptying. Those might be beneficial to prevent recurrent cholangitis[6].
The pathogenesis of ectopic papilla associated malignancy is unclear. Only one case report is available of periampullary carcinoma with an ectopic ending of the ampulla of Vater in the fourth part of the duodenum[7].
Diagnosis is dependent on the observation of the orifice location and duct through radiographic visualization with contrast medium[2,8]. Recognizing an ectopic papilla of Vater and ruling out fistulas, which may be secondary to ulcer diseases or choledocho-lithiasis, spontaneous or iatrogenic surgical fistulas, or surgical choledochoenteric diversions are also crucial[9].
Currently, an ectopic papilla of Vater can be detected through various methods, such as percutaneous transhepatic cholangiography, upper gastrointestinal endoscopy, ERCP, magnetic resonance cholangiopancreatography, and barium meals[10]. In particular, ERCP is a putatively effective procedure with efficacy and safety, although anatomical alteration increases the difficulty of intervention and the risk of complications; that is, ERCP operators may be unable to establish the location of the ectopic orifice of papilla. Infrequent complications related to ERCP include pancreatitis, bleeding, perforation, biliary tract infection, and hyperamylasemia. A hook-shaped configuration may sometimes be visible with cholaniography, but this cannot be considered a reliable criterion. The reason for this is that the configuration may dynamically alter according to a patient’s position[2]. Balloon dilatation is the main treatment recommended and performed. Surgery is the last resort in cases when endoscopic treatment is ineffective.
We presented a rare case of an ectopic ampulla of Vater in the pylorus. When the ampulla of Vater is not visible in the second portion of the duodenum, ectopic papilla of Vater should be considered as a diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gao DJ, Moon SH S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Saritas U, Senol A, Ustundag Y. The clinical presentations of ectopic biliary drainage into duodenal bulbus and stomach with a thorough review of the current literature. BMC Gastroenterol. 2010;10:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Peng YC, Chow WK. Ectopic papilla of Vater in duodenum bulb: A hospital-based study. Medicine (Baltimore). 2019;98:e14642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Hong J, Pan W, Zuo W, Wang A, Zhu L, Zhou X, Li G, Liu Z, Liu P, Zhen H, Zhu Y, Ma J, Yuan J, Shu X, Lu N, Chen Y. Efficacy and safety of therapeutic ERCP in patients with ectopic papilla of Vater. Medicine (Baltimore). 2020;99:e18536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Guerra I, Rábago LR, Bermejo F, Quintanilla E, García-Garzón S. Ectopic papilla of Vater in the pylorus. World J Gastroenterol. 2009;15:5221-5223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Bernard P, Le Borgne J, Dupas B, Kohnen-Shari N, Raoult S, Hamel A. Double common bile duct with ectopic drainage into the stomach. Case report and review of the literature. Surg Radiol Anat. 2001;23:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Koek GH, Vos R, Sifrim D, Cuomo R, Janssens J, Tack J. Mechanisms underlying duodeno-gastric reflux in man. Neurogastroenterol Motil. 2005;17:191-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Jin SG, Chen ZY, Yan LN, Zeng Y, Huang W, Xu N. A rare case of periampullary carcinoma with ectopic ending of Vater's ampulla. World J Gastroenterol. 2009;15:4729-4731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Lee SS, Kim MH, Lee SK, Kim KP, Kim HJ, Bae JS, Seo DW, Ha HK, Kim JS, Kim CD, Chung JP, Min YI. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc. 2003;57:679-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Pereira-Lima J, Pereira-Lima LM, Nestrowski M, Cuervo C. Anomalaous location of the papilla of vater. Am J Surg. 1974;128:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Nasseri-Moghaddam S, Nokhbeh-Zaeem H, Soroush Z, Bani-Solaiman Sheybani S, Mazloum M. Ectopic location of the ampulla of vater within the pyloric channel. Middle East J Dig Dis. 2011;3:56-58. [PubMed] |