Published online Apr 26, 2021. doi: 10.12998/wjcc.v9.i12.2874
Peer-review started: December 1, 2020
First decision: January 17, 2021
Revised: January 26, 2021
Accepted: February 22, 2021
Article in press: February 22, 2021
Published online: April 26, 2021
Processing time: 134 Days and 14.8 Hours
Pulmonary alveolar proteinosis (PAP) is a pulmonary syndrome wherein large volumes of phospholipid and protein-rich surfactants accumulate within the alveoli. PAP forms include primary (auto-immune PAP), secondary, and congenital. Nocardiosis is a form of suppurative disease induced upon infection with bacteria of the Nocardia genus. Clinically, cases of PAP complicated with Nocardia infections are rare, regardless of form. Unfortunately, as such, they are easily overlooked or misdiagnosed. We describe, here, the case of a patient suffering from simultaneous primary PAP and nocardiosis.
A 45-year-old Chinese man, without history of relevant disease, was admitted to our hospital on August 8, 2018 to address complaints of activity-related respiratory exertion and cough lasting over 6 mo. Lung computed tomography (CT) revealed diffuse bilateral lung infiltration with local consolidation in the middle right lung lobe. Subsequent transbronchial lung biopsy and CT-guided lung biopsy led to a diagnosis of primary PAP (granulocyte-macrophage colony-stimulating factor antibody-positive) complicated with nocardiosis (periodic acid-Schiff-positive). After a 6 mo course of anti-infective treatment (sul-famethoxazole), the lesion was completely absorbed, such that only fibrous foci remained, and the patient exhibited significant symptom improvement. Follow-up also showed improvement in pulmonary function and the CT imaging findings of PAP. No whole-lung lavage has been conducted to date. This case highlights that active anti-nocardia treatment may effectively improve the symptoms and alleviate PAP in patients with PAP and nocardia, possibly reducing the need for whole-lung lavage.
When evaluating patients presenting with PAP and pulmonary infections, the potential for nocardiosis should be considered.
Core Tip: We present the case of a patient suffering from simultaneous primary pulmonary alveolar proteinosis (PAP) and nocardiosis. This case highlights the importance of considering the potential for nocardiosis when evaluating patients presenting with PAP and pulmonary infections. The successful management of our case also shows that active anti-nocardia treatment may effectively alleviate the concomitant PAP and may also reduce the need for whole-lung lavage.
- Citation: Wu XK, Lin Q. Pulmonary alveolar proteinosis complicated with nocardiosis: A case report and review of the literature. World J Clin Cases 2021; 9(12): 2874-2883
- URL: https://www.wjgnet.com/2307-8960/full/v9/i12/2874.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i12.2874
Pulmonary alveolar proteinosis (PAP) is a rare diffuse pulmonary syndrome of unknown etiology characterized by the accumulation of large volumes of phospholipid and protein-rich substances within the alveoli[1-3]. PAP is believed to develop as a consequence of abnormal alveolar surfactant metabolism and clearance, resulting in surfactant-derived substance deposition in the alveolar cavity[4-7]. Its forms include primary PAP, secondary PAP, and congenital PAP (surfactant dysfunction syndrome). The primary form is characterized by the presence of antibodies to granulocyte-macrophage colony-stimulating factor (GM-CSF). As such, the gold-standard for primary PAP diagnosis is enzyme-linked immunosorbent assay detection of the anti-GM-CSF antibodies (> 19 mg/mL provides specific diagnosis, and < 10 mg/mL has good negative predictive value)[8]. In general, however, the diagnosis of PAP begins with a computed tomography (CT) scan, which is followed by confirmatory staining of bronchoalveolar lavage fluid (BALF) or biopsied lung tissue. PAP patients typically present with symptoms such as cough, dyspnea, and chest tightness, and exhibit the CT imaging findings of "pavement stone" and "gravel-road-like" patterns[9,10]. Meanwhile, the BALF from these patients shows milky white coloration and both the BALF and lung biopsy tissue show positivity to periodic acid-Schiff (PAS) staining[11,12]. Finally, pulmonary function testing can demonstrate restrictive ventilation dysfunction and diffusion dysfunction. The standard of care for symptomatic PAP patients is whole-lung lavage[13-15].
Nocardia is a genus of filamentous, Gram-positive, acid fast weak-positive, aerobic bacteria found in soils worldwide[16,17]. It is responsible for acute or chronic infections, primarily occurring in immunocompromised hosts and particularly those with impaired cell-mediated immunity related to autoimmune deficiency syndrome and transplant. The Nocardia asteroides complex accounts for approximately 85% of all nocardial infections and most pulmonary infections[17-19]. The sulfonamide anti-infectives (e.g., sulfamethoxazole) serve as both the first-line treatment for Nocardia infection and the first choice for empirical treatment. For people with normal immune function, the treatment is generally administered in a 3-6 mo course; while, for people with immune deficiency, the duration is at least 1 year[20].
Herein, we report the case of a patient diagnosed with PAP with nocardiosis. Through this report, we hope to alert clinical care providers to the possibility of PAP complicated with rare infections, such as Nocardia infection. For such patients, early diagnosis and active anti-infective therapy are necessary, and may reduce the need for whole-lung lavage treatment.
A 45-year-old Chinese man was admitted to our hospital in August 2018 after presenting with complaints of persistent and ongoing activity-related respiratory exertion and cough.
The patient reported that his symptoms had begun 6 mo prior.
The patient’s medical history was unremarkable.
Physical examination detected diminished breath sound in both lungs. No other positive sign was observed, including fever, chest pain, sputum production, hemoptysis, or other discomfort.
Routine blood work-up revealed elevated leukocyte count (10.60 × 109/L; reference range: 3.5-9.5 × 109/L), platelet count (355 × 109/L; reference range: 125-350 × 109/L), and CD8+ T cell percentage (39.9%; reference range: 15.8%-37.5%). All other blood parameters were within normal range, including CD4+ T cell percentage (32.0%), absolute value of neutrophils (6.08 × 109/L), neutrophil percentage (0.574%), red blood cell count (5.43 × 1012/L), hemoglobin concentration (165 g/L), and blood gas pH (7.421).
Other abnormal findings were elevated keratin 21-1 level (10.7 ng/mL; reference range: 0-3.3 ng/mL) and neurogene-specific enolase level (19.5 ng/mL; reference range: 0-15 ng/mL). Normal levels of squamous cell carcinoma antigen (0.50 mg/L) and gastrin-releasing peptide precursor (44 ng/L) were found.
Tests of pulmonary gas pressures and respiratory physiology showed decreased oxygen partial pressure (50.7 mmHg; reference range: 80-100 mmHg), carbon dioxide partial pressure (32.3 mmHg; reference range: 35-45 mmHg), and oxygen saturation (86.1%; reference range: 91%-99%). Pulmonary function tests revealed mild restrictive ventilation dysfunction with moderately decreased dispersion (Table 1).
| August 2018 | April 2019 | December 2019 | |
| FEV1 in L | 3.12 | 3.18 | 3.43 |
| FVC in L | 3.2 | 3.3 | 3.8 |
| FEV1/FVC, % | 97.5 | 96.4 | 90.3 |
| FEV1/pred, % | 90.6 | 92.4 | 95.3 |
| FVC/pred, % | 77.0 | 79.3 | 91.3 |
| DLCO SB in mmol/min/kPa | 4.50 | 4.74 | 7.62 |
| DLCO SB/pred, % | 46.4 | 48.9 | 78.6 |
No abnormalities were detected in tests of renal and hepatic functions, D-dimer, erythrocyte sedimentation rate, C-reactive protein, pro-calcitonin, coagulation function, sputum smears, thyroid function, immunoglobulin levels, auto-antibody levels, antineutrophil cytoplasmic antibodies-related antibody levels, (1,3)-D glucan test, galactomannan, and Cryptococcus capsular antigen.
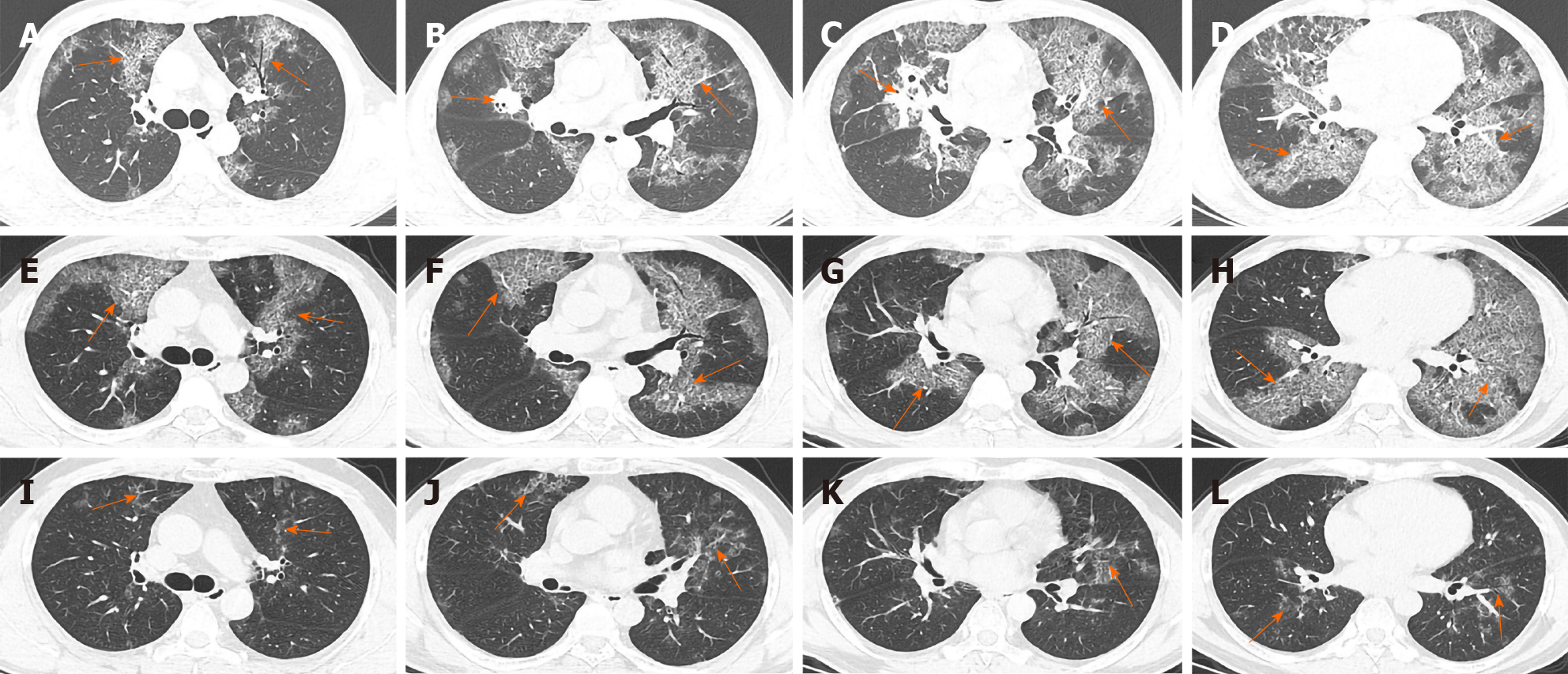
Thin-slice lung CT revealed the presence of diffuse bilateral pulmonary interstitial changes as well as the presence of local consolidation within the middle lobe of the right lung (Figure 1A-D).
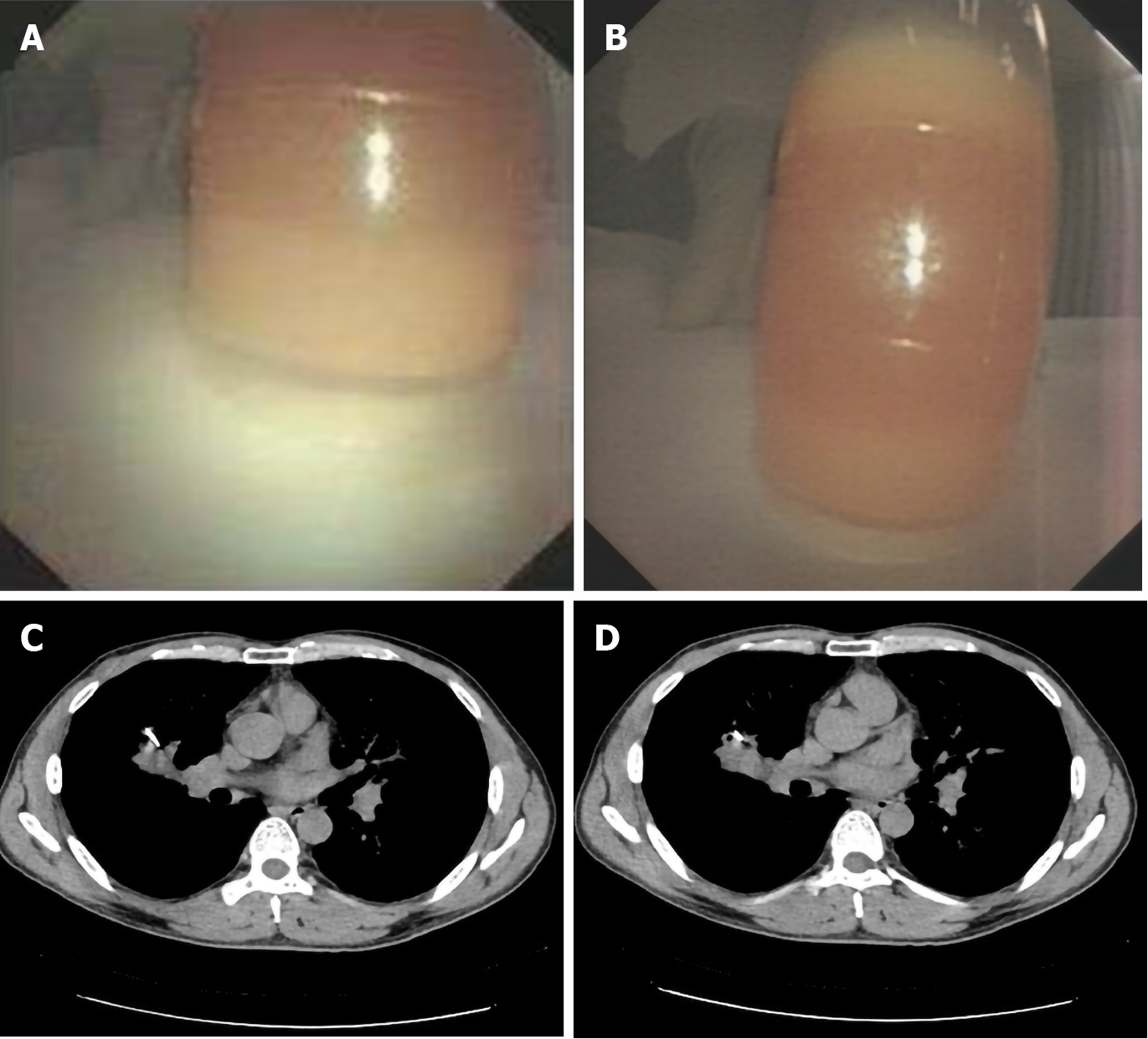
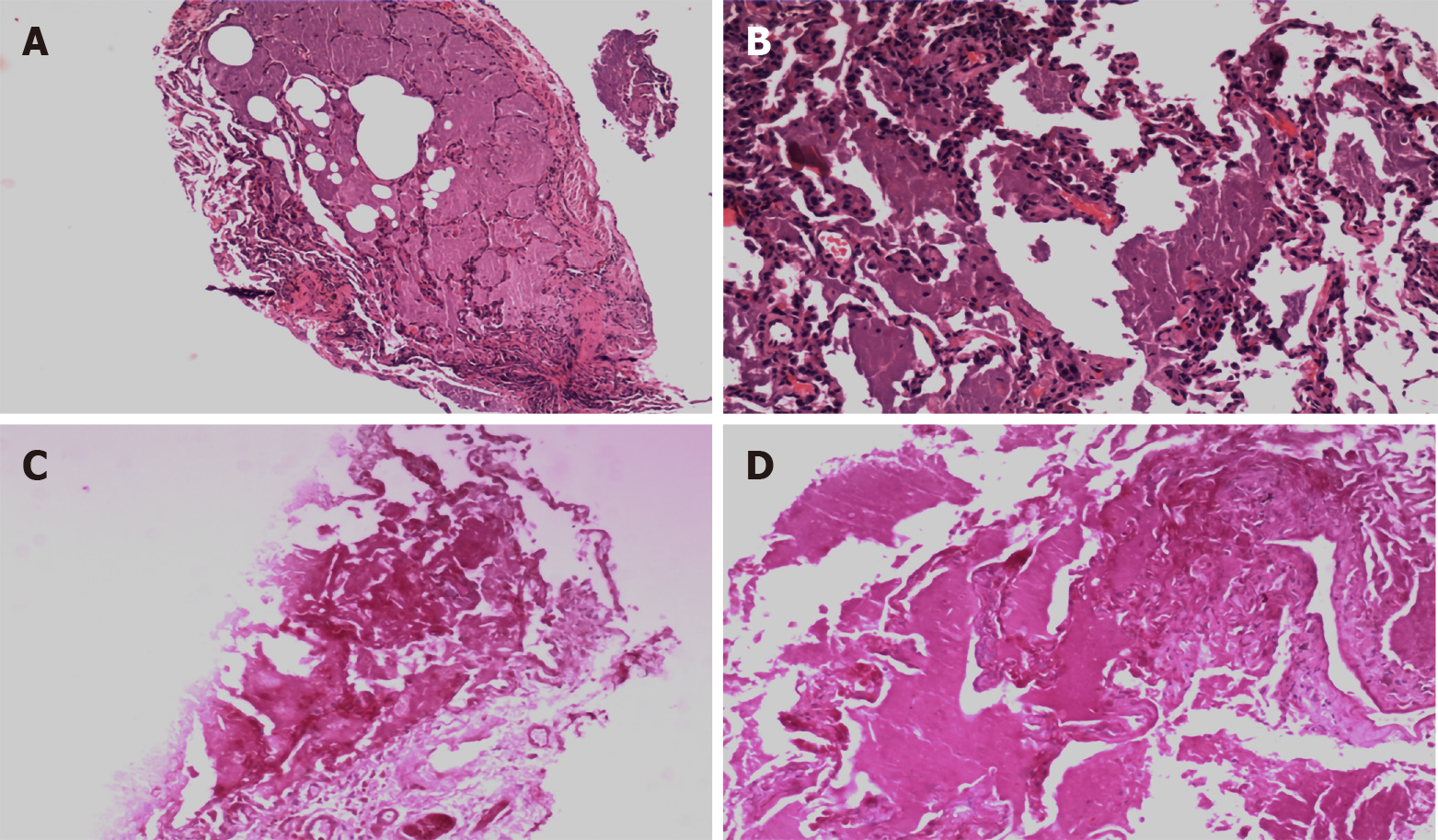
After evaluating the patient for any possible contraindications, a series of bronchoscopy-based diagnostic analyses, including bronchoalveolar lavage and transbronchial lung biopsy (TBLB, lower left lobe), were conducted on August 8, 2018. The lavage fluid appeared white and turbid (Figure 2A and B), and the composition of the right lung lesion remained to be established. CT-guided lung biopsy was subsequently conducted successfully on August 17, 2018 (Figure 2C and D). The TBLB results revealed chronic inflammation accompanied by alveolar cavity expansion in the lower left lung lobe, with evidence of mucinous exudation, peripheral fibrous tissue hyperplasia, chronic inflammatory changes, and the presence of a pink mucoid substance filling a portion of the alveolar cavity (Figure 3A and B). In addition, PAS staining was positive (Figure 3C and D), consistent with a diagnosis of PAP.
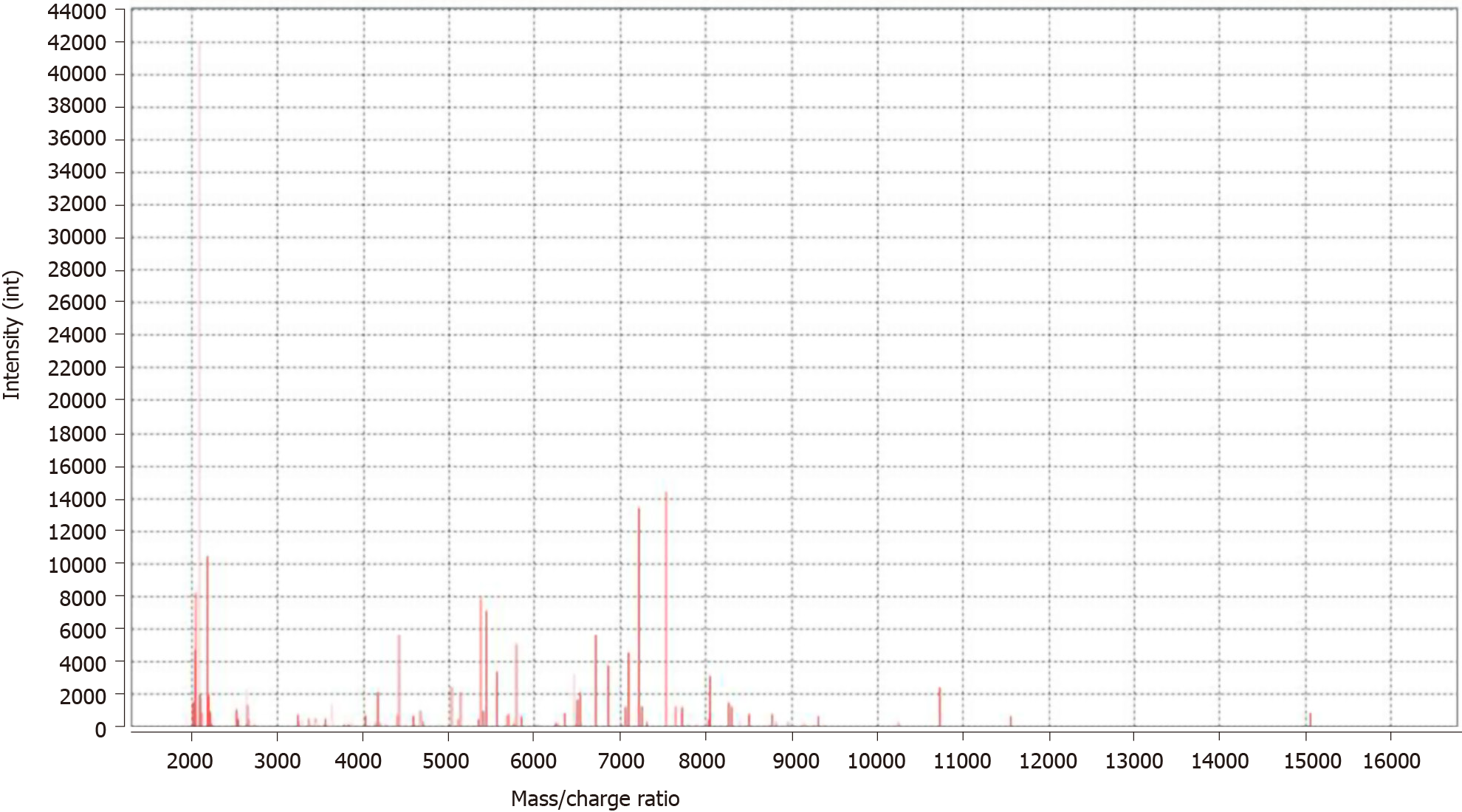
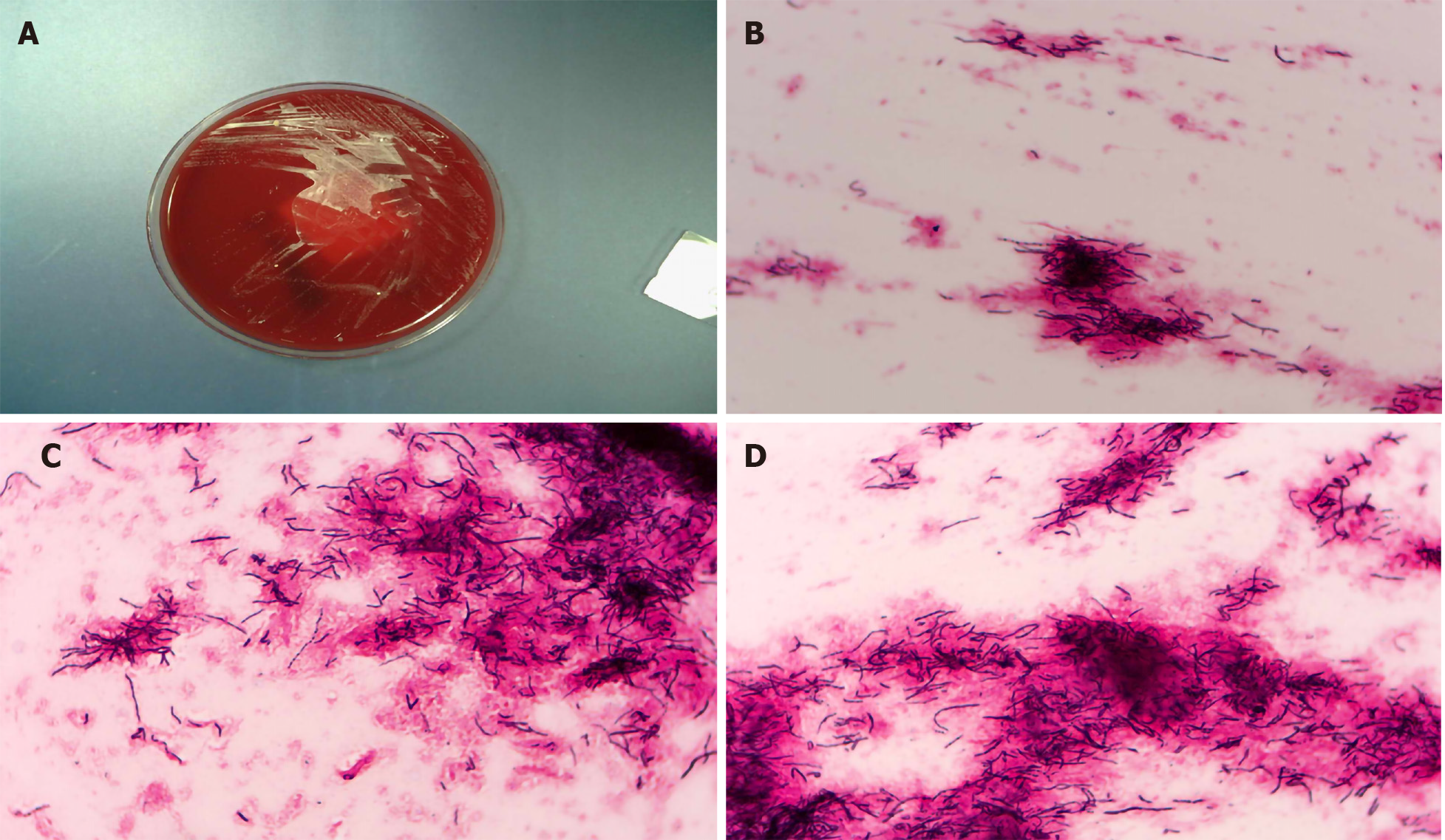
The overall biopsy results suggested that the observed chronic inflammation was associated with alveolar narrowing, neutrophil infiltration in the focal area, and chronic inflammatory cell infiltration of the regions of pulmonary interstitial fibrous tissue hyperplasia. Mass spectroscopy (MS) analysis of the lung biopsy culture from the middle right lung lobe identified Nocardia infection (Vitek MS automated MALDI-TOF-MS instrument; Biomérieux, Marcy-IÉtiole, France) (Figure 4). Microscopic analysis confirmed cultural characteristics of Nocardia in the lung biopsy culture (Figure 5). Drug-susceptibility testing indicated sensitivity to sulfamethoxazole (Table 2).
| Drug | Sensibility | Result in μg/mL | Method |
| Amoxicillin | S | 1 | MIC |
| Ceftriaxone sodium | S | 1 | MIC |
| Imipenem | S | 2 | MIC |
| Clarithromycin | R | > 64 | MIC |
| Linezolid | S | 1 | MIC |
| Minocycline | S | 1 | MIC |
| Ciprofloxacin | S | 8 | MIC |
| Moxifloxacin | R | 4 | MIC |
| Tobramycin | S | 1 | MIC |
| Amikacin | S | 1 | MIC |
| Sulfamethoxazole | S | 0.5 | MIC |
The serum of this patient was detected by enzyme-linked immunosorbent assay, and the results indicated elevated levels of anti-GM-CSF antibodies.
The patient was tentatively diagnosed with primary PAP complicated with nocardiosis.
The patient received a 6-mo treatment course with sulfamethoxazole (September 2018 to April 2019).
The patient attended regular follow-up visits. Pulmonary function testing performed in April 2019 provided findings similar to those in August 2018. However, in December 2019, the findings improved substantially, especially for forced vital capacity (FVC), FVC/predictive value, diffusing capacity of the lungs single-breath (DLCO SB), and DLCO SB/predictive value (Table 1). Chest CT imaging in April 2019 (Figure 1E-H) revealed further improvements, particularly in the consolidation in the middle lobe of the right lung, but the alveolar protein deposition remained largely unchanged. Chest CT imaging conducted in December 2019 (Figure 1I-L) showed the long-awaited improvements in alveolar protein deposition.
The patient's symptoms were gradually relieved over the course of follow-up. Details of the effectiveness of the anti-nocardia treatment, illustrated by findings from before and after treatment, are summarized in Table 3. As of October 2020, the patient remained in stable condition and had not undergone whole-lung lavage.
| August 2018 | April 2019 | December 2019 | |
| Dyspnea index | 2 | 2 | 0 |
| Supplemental O2 in L/min | 5 | 3 | 0 |
| PaO2 in mmHg | 50.7 | 62.6 | 95.8 |
| SaO2 in mmHg | 86.1 | 91.5 | 97 |
PAP is a rare disease characterized by alveolar accumulation of surfactant, composed of proteins and lipids, that is due to defective surfactant clearance by the alveolar macrophages. Among the three forms of PAP[21-23], primary PAP accounts for the majority of cases (85%-90%). Its pathomechanism is a loss of GM-CSF signaling due to elevated GM-CSF antibody levels or genetic mutations in the receptors for GM-CSF that inhibit or prevent GM-CSF signaling. Loss of GM-CSF signaling prevents differentiation of macrophages in the lung, and mature macrophages are imperative for appropriate surfactant levels in the lungs. All primary PAP patients demonstrate circulating, neutralizing anti-GM-CSF autoantibodies[24-26]. Secondary PAP, on the other hand, is an entity that occurs in the presence of other diseases, such as acute myelogenous leukemia, acute lymphocytic leukemia, chronic myelogenous leukemia, or infections (e.g., nocardiosis and tuberculosis). The congenital form of PAP results from very rare gene mutations. Typically, these cases manifest in patients without any history of relevant disease or a positive GM-CSF antibody testing result.
Our patient, described herein, was considered to have primary PAP. The current standard of care for all forms of PAP is whole-lung lavage. However, this procedure is associated with a wide range of complications, with the most frequent being low oxygen saturation, convulsions, pneumothorax, pleural effusion, and fever; the latter of these may indicate an infection complication. Our patient did not undergo whole-lung lavage because of our concerns about introducing a secondary or aggravated infection. Although PAP can wax/wane or even spontaneously improve on its own, we were surprised to find that during follow-up the patient’s PAP became significantly alleviated after an active anti-Nocardia treatment course. Importantly, our patient has been able to avoid undergoing whole-lung lavage to date.
Cases of nocardiosis in cows and humans were first described in 1888 and 1890[27], respectively. Cell-based immune responses are the primary means of combatting these Nocardia infections, and PAP can also arise as a consequence of pulmonary infections, including nocardiosis[28,29]. Pulmonary nocardiosis always manifests on CT as lung consolidation, presenting a solitary or, more often, multiple lung nodules of various sizes[30]. Therefore, in cases of PAP associated with such pulmonary manifestations, it is necessary that the clinical care team be alert to the possibility of a Nocardia infection. It has been reported that patients with PAP are prone to pulmonary infection (e.g., fungal infection and tuberculosis), which may be related to the impaired alveolar surface clearance mechanism leading to decreased immunity of the body.
Because of the decreased immunity of the body caused by the impaired alveolar surface clearance mechanism, we speculated that our patient’s nocardiosis was likely secondary to the PAP incidence. To date, there have been few reported cases of PAP associated with nocardiosis. In one such reported case[31], the patient’s condition improved significantly following active treatment. Owing to the active anti-Nocardia treatment, our patient has been able to avoid whole-lung lavage while obtaining a substantial improvement in his PAP symptoms.
In summary, the present case emphasizes the importance of evaluating PAP patients for rare pathogenic bacterial infections, such as Nocardia infection. Active anti-Nocardia treatment may be sufficient to improve the symptoms in patients who suffer from PAP associated with Nocardia infection, thereby decreasing the likelihood that a patient will need undergo the inherently risky whole-lung lavage procedure.
We thank the patient and his family and all those who contributed to this report.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta N S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Nekooie-Marnany N, Deswarte C, Ostadi V, Bagherpour B, Taleby E, Ganjalikhani-Hakemi M, Le Voyer T, Rahimi H, Rosain J, Pourmoghadas Z, Sheikhbahaei S, Khoshnevisan R, Petersheim D, Kotlarz D, Klein C, Boisson-Dupuis S, Casanova JL, Bustamante J, Sherkat R. Impaired IL-12- and IL-23-Mediated Immunity Due to IL-12Rβ1 Deficiency in Iranian Patients with Mendelian Susceptibility to Mycobacterial Disease. J Clin Immunol. 2018;38:787-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Inoue Y, Trapnell BC, Tazawa R, Arai T, Takada T, Hizawa N, Kasahara Y, Tatsumi K, Hojo M, Ichiwata T, Tanaka N, Yamaguchi E, Eda R, Oishi K, Tsuchihashi Y, Kaneko C, Nukiwa T, Sakatani M, Krischer JP, Nakata K; Japanese Center of the Rare Lung Diseases Consortium. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med. 2008;177:752-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 320] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 3. | Suzuki T, Sakagami T, Young LR, Carey BC, Wood RE, Luisetti M, Wert SE, Rubin BK, Kevill K, Chalk C, Whitsett JA, Stevens C, Nogee LM, Campo I, Trapnell BC. Hereditary pulmonary alveolar proteinosis: pathogenesis, presentation, diagnosis, and therapy. Am J Respir Crit Care Med. 2010;182:1292-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Seymour JF, Presneill JJ, Schoch OD, Downie GH, Moore PE, Doyle IR, Vincent JM, Nakata K, Kitamura T, Langton D, Pain MC, Dunn AR. Therapeutic efficacy of granulocyte-macrophage colony-stimulating factor in patients with idiopathic acquired alveolar proteinosis. Am J Respir Crit Care Med. 2001;163:524-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 134] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Venkateshiah SB, Yan TD, Bonfield TL, Thomassen MJ, Meziane M, Czich C, Kavuru MS. An open-label trial of granulocyte macrophage colony stimulating factor therapy for moderate symptomatic pulmonary alveolar proteinosis. Chest. 2006;130:227-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Robinson TE, Trapnell BC, Goris ML, Quittell LM, Cornfield DN. Quantitative analysis of longitudinal response to aerosolized granulocyte-macrophage colony-stimulating factor in two adolescents with autoimmune pulmonary alveolar proteinosis. Chest. 2009;135:842-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Patiroglu T, Akyildiz B, Patiroglu TE, Gulmez IY. Recurrent pulmonary alveolar proteinosis secondary to agammaglobulinemia. Pediatr Pulmonol. 2008;43:710-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Uchida K, Nakata K, Suzuki T, Luisetti M, Watanabe M, Koch DE, Stevens CA, Beck DC, Denson LA, Carey BC, Keicho N, Krischer JP, Yamada Y, Trapnell BC. Granulocyte/macrophage-colony-stimulating factor autoantibodies and myeloid cell immune functions in healthy subjects. Blood. 2009;113:2547-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Choi HK, Park CM, Goo JM, Lee HJ. Pulmonary alveolar proteinosis vs exogenous lipoid pneumonia showing crazy-paving pattern: Comparison of their clinical features and high-resolution CT findings. Acta Radiol. 2010;51:407-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Johkoh T, Itoh H, Müller NL, Ichikado K, Nakamura H, Ikezoe J, Akira M, Nagareda T. Crazy-paving appearance at thin-section CT: spectrum of disease and pathologic findings. Radiology. 1999;211:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 193] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Greenhill SR, Kotton DN. Pulmonary alveolar proteinosis: a bench-to-bedside story of granulocyte-macrophage colony-stimulating factor dysfunction. Chest. 2009;136:571-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Lison D, Delos M. Pulmonary alveolar proteinosis in workers at an indium processing facility. Am J Respir Crit Care Med. 2010;182:578; author reply 578-578; author reply 579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Cheng SL, Chang HT, Lau HP, Lee LN, Yang PC. Pulmonary alveolar proteinosis: treatment by bronchofiberscopic lobar lavage. Chest. 2002;122:1480-1485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Brach BB, Harrell JH, Moser KM. Alveolar proteinosis. Lobar lavage by fiberoptic bronchoscopic technique. Chest. 1976;69:224-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Borie R, Debray MP, Laine C, Aubier M, Crestani B. Rituximab therapy in autoimmune pulmonary alveolar proteinosis. Eur Respir J. 2009;33:1503-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006;19:259-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 692] [Cited by in RCA: 781] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 17. | Conville PS, Brown-Elliott BA, Smith T, Zelazny AM. The Complexities of Nocardia Taxonomy and Identification. J Clin Microbiol. 2018;56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 137] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 18. | Le Coustumier EM, Denes E, Martin C, Weinbreck P. [Nocardiosis: A retrospective case series of 19 patients]. Rev Med Interne. 2017;38:81-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Oszoyoglu AA, Kirsch J, Mohammed TL. Pulmonary nocardiosis after lung transplantation: CT findings in 7 patients and review of the literature. J Thorac Imaging. 2007;22:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Yildiz O, Doganay M. Actinomycoses and Nocardia pulmonary infections. Curr Opin Pulm Med. 2006;12:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Wells AU. The clinical utility of bronchoalveolar lavage in diffuse parenchymal lung disease. Eur Respir Rev. 2010;19:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Prakash UB, Barham SS, Carpenter HA, Dines DE, Marsh HM. Pulmonary alveolar phospholipoproteinosis: experience with 34 cases and a review. Mayo Clin Proc. 1987;62:499-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 129] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Huizar I, Kavuru MS. Alveolar proteinosis syndrome: pathogenesis, diagnosis, and management. Curr Opin Pulm Med. 2009;15:491-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Bonfield TL, Russell D, Burgess S, Malur A, Kavuru MS, Thomassen MJ. Autoantibodies against granulocyte macrophage colony-stimulating factor are diagnostic for pulmonary alveolar proteinosis. Am J Respir Cell Mol Biol. 2002;27:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 79] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 25. | Thomassen MJ, Yi T, Raychaudhuri B, Malur A, Kavuru MS. Pulmonary alveolar proteinosis is a disease of decreased availability of GM-CSF rather than an intrinsic cellular defect. Clin Immunol. 2000;95:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Bonfield TL, Kavuru MS, Thomassen MJ. Anti-GM-CSF titer predicts response to GM-CSF therapy in pulmonary alveolar proteinosis. Clin Immunol. 2002;105:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Fatahi-Bafghi M. Nocardiosis from 1888 to 2017. Microb Pathog. 2018;114:369-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 106] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 28. | Lebeaux D, Morelon E, Suarez F, Lanternier F, Scemla A, Frange P, Mainardi JL, Lecuit M, Lortholary O. Nocardiosis in transplant recipients. Eur J Clin Microbiol Infect Dis. 2014;33:689-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 29. | Filice GA. Nocardiosis in persons with human immunodeficiency virus infection, transplant recipients, and large, geographically defined populations. J Lab Clin Med. 2005;145:156-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Kanne JP, Yandow DR, Mohammed TL, Meyer CA. CT findings of pulmonary nocardiosis. AJR Am J Roentgenol. 2011;197:W266-W272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Yamaguchi S, Takayanagi N, Tokunaga D, Sugita Y, Kawabata Y. [A case of pulmonary alveolar proteinosis which initially deteriorated rapidly with exacerbation of pulmonary nocardiosis, responded promptly to treatment of the pulmonary nocardiosis]. Nihon Kokyuki Gakkai Zasshi. 2010;48:580-583. [PubMed] |