Published online Apr 26, 2021. doi: 10.12998/wjcc.v9.i12.2845
Peer-review started: November 16, 2020
First decision: December 30, 2020
Revised: January 13, 2021
Accepted: February 22, 2021
Article in press: February 22, 2021
Published online: April 26, 2021
Processing time: 147 Days and 20.4 Hours
Glioblastoma is the most common type of brain tumor and is invariably fatal, with a mean survival time of 8-15 mo for recently diagnosed tumors, and a 5-year survival rate of only 7.2%. The standard treatment for newly diagnosed glioblastoma includes surgery followed by concurrent chemoradiotherapy and further adjuvant temozolomide. However, the prognosis remains poor and long-term survival is rare. This report aimed to demonstrate a new therapeutic strategy for the treatment of glioblastoma.
A patient was referred to the Department of Neurosurgery with an intracranial space-occupying lesion with a maximum diameter of approximately 5 cm. The tumor was compressing functional areas, and the patient accordingly underwent partial resection and concurrent chemoradiotherapy. The imaging and pathological findings were consistent with a diagnosis of glioblastoma with oligodendroglioma differentiation (World Health Organization IV). The patient was finally diagnosed with glioblastoma. However, the patient discontinued treatment due to intolerable side effects, and was prescribed Kangliu pill (KLP) 7.5 g three times/d, which he has continued to date. Significant shrinkage of the tumor (maximum diameter reduced from about 3.5 to about 2 cm) was found after 3 mo of KLP therapy, and the tumor was further reduced to about 1 cm after 3 years. The patient’s symptoms of headache, limb weakness, and left hemiplegia were relieved, with no side effects.
KLP has been a successful intervention for glioblastoma, and the current case indicates that traditional Chinese medicine may offer effective alternative therapies for glioblastoma.
Core Tip: Glioblastoma is the most common type of malignant primary brain cancer. The standard treatment for newly diagnosed glioblastoma includes surgery followed by concurrent chemoradiotherapy and further adjuvant temozolomide. However, patients usually have a poor prognosis and high recurrence rate, and may develop drug resistance and serious adverse reactions to chemotherapy. Some recent studies suggested that traditional Chinese medicine may have a good therapeutic effect in patients with glioblastoma, and it is generally used as an adjunct therapy for various stages of tumors in clinical practice. We report a patient with glioblastoma who abandoned chemoradiotherapy due to intolerance, and subsequently received the Chinese patent medicine Kangliu pill without any other treatment. Three months after the start of treatment, the patient had a partial response, which persisted for more than 3 years. This surprising discovery indicates that the Chinese patent medicine Kangliu pill may provide a new option for the treatment of glioblastoma.
- Citation: Sun G, Zhuang W, Lin QT, Wang LM, Zhen YH, Xi SY, Lin XL. Partial response to Chinese patent medicine Kangliu pill for adult glioblastoma: A case report and review of the literature. World J Clin Cases 2021; 9(12): 2845-2853
- URL: https://www.wjgnet.com/2307-8960/full/v9/i12/2845.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i12.2845
Glioblastoma (GBM) is the most common type of malignant primary brain cancer with the lowest survival rate, representing approximately 48% of all primary malignant central nervous system tumors[1,2]. GBM is one of the most devastating brain tumors, and is highly heterogeneous and invasive, with a high incidence rate. The overall annual incidence rate of glioma is high, at 9.23 cases per 100000 individuals in the United States, with GBM accounting for about half of all these cases[2]. Patients diagnosed with GBM usually have a dismal prognosis and poor quality of life. Currently, the best outcome is a modest 14.6-mo median survival following surgical resection, radiotherapy, and/or chemotherapy with temozolomide (TMZ)[3]. However, the survival outcomes are generally very poor, with a mean survival rate of recurring GBM of just 3-9 mo[4] and a 5-year survival rate of 7.2%[5]. This poor prognosis is mostly due to the tumor’s therapeutic resistance and to tumor relapse after surgical removal[6]. Despite extensive efforts, little progress has been made in prolonging the survival of patients with GBM[7]. Thus, there is an urgent need to explore effective treatment strategies and drugs to improve the prognosis of patients with GBM. Traditional Chinese medicine (TCM) has recently gained wide attention due to its therapeutic effects and few side effects in patients with GBM, with increasing numbers of TCMs demonstrating antitumor effects against GBM. For example, toosendanin inhibited GBM cell proliferation and induced apoptosis in vitro and in vivo[8]. Celastrol sensitized glioma cells to the apoptosis-induced ligand TRAIL via the death receptor pathway, indicating a promising tumor-killing therapeutic strategy with high efficacy and low toxicity[9]. The aqueous extract of Pingliu Keli strongly inhibited cell proliferation and induced apoptosis in SHG-44 cells[10], and Jinlong capsules partly regulated the mTOR/S6 pathway to inhibit glioblastoma cell migration and invasion in vitro[11]. Kangliu pill (KLP) is a Chinese patent medicine consisting of 18 types of traditional Chinese medicine: Smilax glabra Roxb. (Tufuling) (Voucher Number: 140105), Panax notoginseng (Burkill) F. H. Chen (Sanqi) (Voucher Number: 140815), Scleromitrion diffusum (Willd.) R. J. Wang (Baihuasheshecao) (Voucher Number: 140702), Scutellaria barbata D. Don (Banzhilian) (Voucher Number: 140912), calcined Alumen (Kufan) (Voucher Number: 140201), Reynoutria multiflora (Thunb.) Moldenke (Zhiheshouwu) (Voucher Number: 140705), Aquilaria sinensis (Lour.) Spreng. (Baimuxiang) (Voucher Number: 140615), Monetaria annulus (Linnaeus) (Baibeichi) (Voucher Number: 140216), Solanum lyratum Thunb. (Baiying) (Voucher Number: 140708), Fritillaria cirrhosa D. Don (Chuanbeimu) (Voucher Number: 140207), Stemona japonica (Blume) Miq. (Baibu) (Voucher Number: 140211), Eriobotrya japonica (Thunb.) Lindl. (Pipaye) (Voucher Number: 140416), Aster tataricus L.f. (Ziwan) (Voucher Number: 140409), stir-baked Crataegus pinnatifida Bunge (Jiaoshanzha) (Voucher Number: 140809), stir-baked Hordeum vulgare L. (Jiaomaiya) (Voucher Number: 140512), stir-baked Massa Medicata Fermentata (Jiaoshenqu) (Voucher Number: 140608), Platycodon grandiflorus (Jacq.) A. DC. (Jiegeng) (Voucher Number: 140713), and Succinium (Hupo) (Voucher Number: 140914). KLP has been used for 40 years and has been shown to reduce temperature and achieve detoxification, as well as promote blood circulation and resolve blood stasis[12-15]. Preclinical studies showed that KLP promoted GBM cell apoptosis by adjusting the ratio of Bcl-2/Bax, suggesting that its inhibitory effect could be related to the induction of glioma cell apoptosis[12,13]. In addition, researchers have identified the main components of KLP and determined quality standards[14,15].
A clinical study also found that KLP exerted antitumor effects against malignant gliomas[16]. Here we report a patient with GBM who experienced a remarkable response to KLP.
The protocols in this case were conducted in strict accordance with the clinical trial guidelines of the Ministry of Science and Technology of the People’s Republic of China and the study was approved by the Ethics Committee of Xuanwu Hospital of Capital Medical University. The specimens of Chinese herbal medicine have been stored in the Pharmacy Department of Xuanwu Hospital of Capital Medical University for future reference, and were identified and independently verified by Professor Jing-Xia Wang from the Chinese Medicine Department of Beijing University of Chinese Medicine.
A 27-year-old man was referred to the Department of Neurosurgery with an intracranial space-occupying lesion on February 21, 2016.
Eight months before the current referral, the patient had experienced left upper limb convulsions, urinary incontinence, nausea, vomiting, and loss of consciousness with no apparent cause, which were relieved after a few minutes. He did not receive any treatment at that time. However, his headache, limb weakness, and left hemiplegia returned 4 mo later. The symptoms were partially relieved by symptomatic supportive treatment, including carbamazepine 400 mg twice/d orally; however, the patient stopped carbamazepine of his own accord due to aggravated limb weakness.
The patient had no previous medical history.
The patient had no personal and family history.
The patient’s temperature was 36.7°C, his heart rate was 70 bpm, his respiratory rate was 18 breaths/min, and his blood pressure was 110/70 mmHg. Clinical neurological examination revealed normal right limb muscle strength, but his left limbs were slightly weaker than his right limbs. His mental functions were normal, with no other pathological signs.
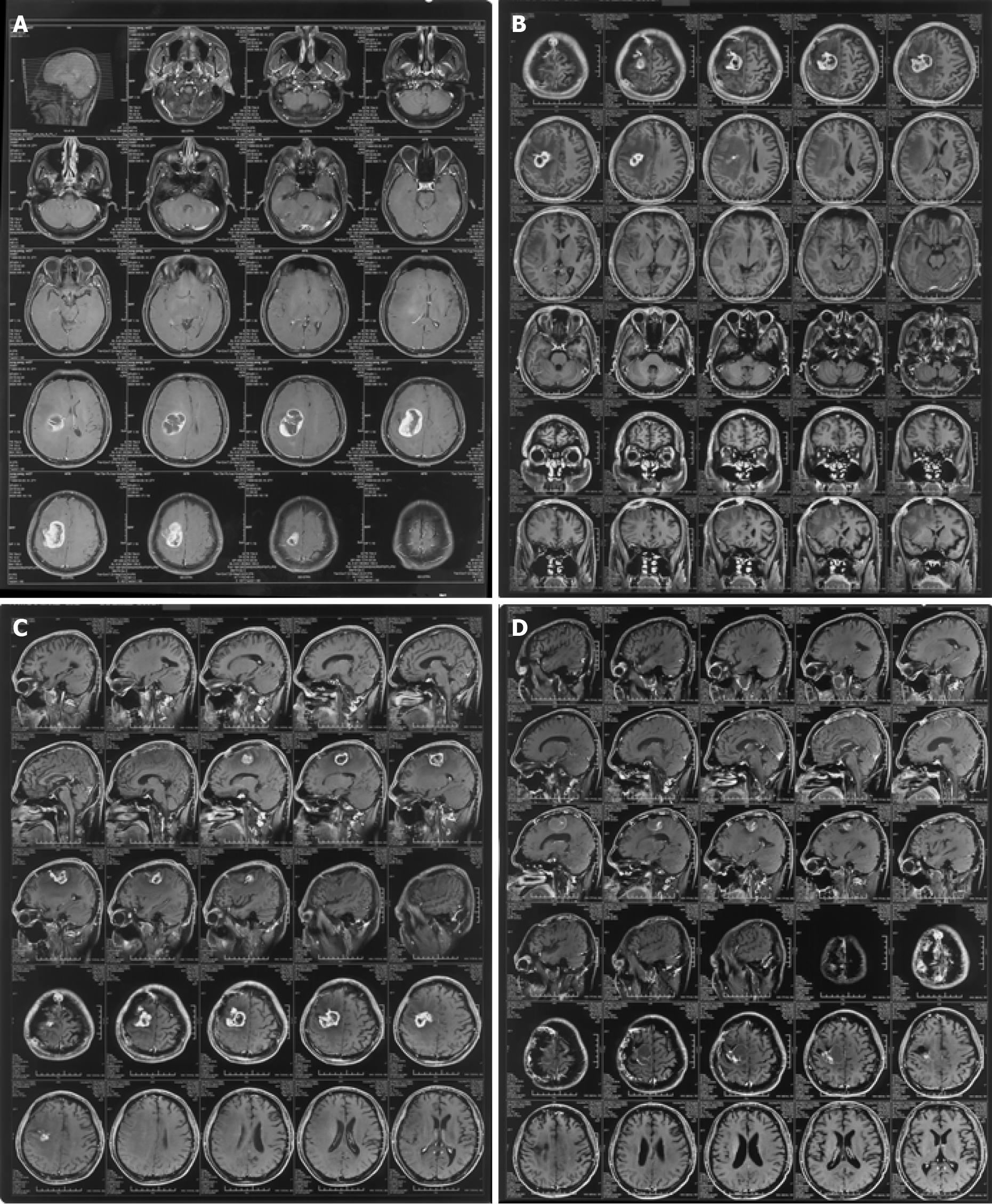
Computed tomography examination in a local hospital showed no obvious abnormalities, but magnetic resonance imaging indicated a space-occupying lesion in the right frontal lobe. The patient did not receive any treatment at that time. However, headache, limb weakness, and left hemiplegia returned 4 mo later, and repeat computed tomography suggested a right frontal parietal lobe cerebral hemorrhage. He presented to the hospital for re-examination on February 18, 2016. Cranial magnetic resonance imaging showed that the right frontal-parietal lobe was occupied by a mass, with a maximum diameter of about 5 cm, irregular enhancement of the parenchyma ring, and the necrotic center was not enhanced, indicating a possible high-grade glioma (Figure 1A).
The patient should undergo surgical treatment with right frontal craniotomy and resection of the brain tumor.
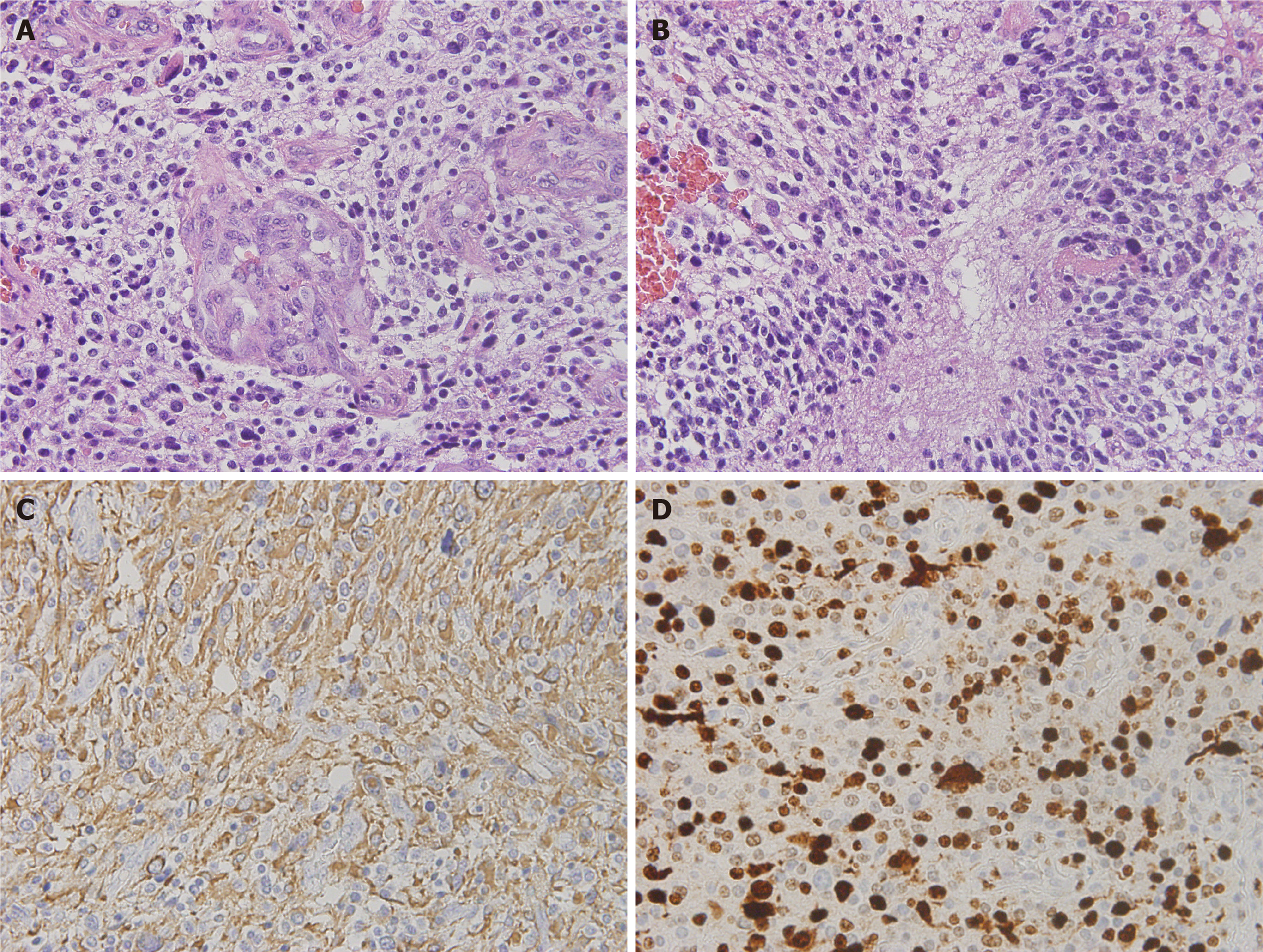
Under the microscope, the specimens submitted for examination showed diffuse growth of tumor cells, with short spindle-shaped nuclei in some areas and round-shaped nuclei in some areas. The cytoplasm was empty and bright, with vascular endothelial proliferation and palisade necrosis (Figure 2). Combined with the immunohistochemical results, these findings were consistent with the diagnosis of glioblastoma with oligodendroglioma differentiation (World Health Organization IV).
The patient discontinued concurrent chemoradiation due to intolerable side effects, and he should therefore be prescribed KLP 7.5 g three times/d.
The final diagnosis of the presented case was glioblastoma.
There was a clear indication for surgery, with no contraindications in the preoperative examination, and the patient underwent partial resection on February 23, 2016. The postoperative pathological report confirmed GBM. After surgery, the patient started concurrent chemoradiation therapy until April 2016, with 75 mg/m2 TMZ once daily for 45 d combined with focal radiotherapy of 60 Gy administered in 30 fractions. However, he opted to discontinue the chemoradiotherapy due to intolerable adverse reactions, including nausea, vomiting, and loss of appetite. Two months later, the patient attended the hospital for postoperative review (Figure 1B) and was prescribed KLP 7.5 g three times/d.
After taking KLP for nearly 3 mo, the tumor had shrunk significantly (from about 3.5 to about 2 cm) (Figure 1C), and he therefore continued to take KLP as prescribed for the next 3 years. A subsequent examination showed that the tumor had shrunk to about 1 cm after 3 years (Figure 1D). No adverse reactions were detected throughout the course of KLP treatment, and the patient’s symptoms of headache, limb weakness, and left hemiplegia were relieved (Table 1).
| Relevant past medical history and interventions | |||
| No relevant past medical history | |||
| Date | Summaries from Initial and follow-up visits | Diagnostic testing | Interventions |
| June 2015 | Left upper limb convulsions, urinary incontinence, nausea, vomiting, and loss of consciousness with no apparent cause | CT examination in a local hospital showed no obvious abnormality, but MRI indicated a space-occupying lesion in the right frontal lobe | Without any treatment |
| October 2015 | Headache, limb weakness, and left hemiplegia | Repeat CT suggested a right frontal parietal lobe cerebral hemorrhage | Symptomatic supportive treatment, including carbamazepine 400 mg twice/d orally. However, the patient stopped carbamazepine of his own accord due to aggravated limb weakness |
| February 2016 | Final diagnosis: glioblastoma, maximum diameter about 5 cm | Cranial MRI showed that the right frontal parietal lobe was occupied by a mass, identified as a possible high-grade glioma. Hematoxylin-eosin staining showed that the tumor cells diffused and infiltrated. Cells were heteromorphic with mitotic figures, microvessel hyperplasia and palisade necrosis. Tumor cells were immunopositive for glial fibrillary acidic protein immunostaining, and about 70% of tumor cells were positive for Ki-67 | Partial resection and concurrent chemoradiation therapy until April 2016, with 75 mg/m2 TMZ once daily for 45 d combined with focal radiotherapy of 60 Gy administered in 30 fractions |
| April 2016 | Intolerable ADRs, including nausea, vomiting, and loss of appetite | None | Discontinued the chemoradiotherapy |
| June 2016 | Postoperative review: maximum diameter about 3.5 cm | Enhanced right frontal parietal lobe space-occupying lesion, maximum diameter about 3.5 cm | Kangliu Pill 7.5 g three times/d |
| October 2016 | Maximum diameter from about 3.5 to about 2 cm | Enhanced lesion at the junction of the right frontal and parietal lobes, maximum diameter about 2 cm | Continue Kangliu pill 7.5 g three times/d |
| April 2019 | Maximum diameter about 1 cm | Enhanced lesion at the junction of the right frontal and parietal lobes, maximum diameter about 1 cm | Continue Kangliu pill 7.5 g three times/d |
| Final outcome | |||
| The patient’s symptoms of headache, limb weakness, and left hemiplegia were relieved, with no side effects | |||
GBM, which accounts for the majority of gliomas (57.7%)[5], is characterized histologically by appreciable cellularity with mitotic activity, vascular proliferation, and necrosis. The standard treatment for newly diagnosed GBM includes surgery followed by concurrent chemoradiotherapy and further adjuvant TMZ. The benefits of TMZ may derive from O-6-methylguanine-deoxyribonucleic acid methyltransferase promoter methylation, which silences epigenetic genes[17]. TMZ is associated with toxicities including myelosuppression and nausea, and especially thrombocytopenia and neutropenia, particularly during adjuvant therapy. GBM usually recurs within 6 mo after standard concurrent chemoradiotherapy[18]. The humanized vascular endothelial growth factor monoclonal antibody bevacizumab has been shown to improve progression-free but not overall survival in patients with GBM[19]. Tumor-treating fields, delivering low-intensity, is approved for adjuvant TMZ therapy based on the progression-free and overall survival benefits[20]. However, despite Food and Drug Administration approval, the evidence for and use of tumor-treating fields remain controversial. Extensive research efforts have also been made in the fields of immunotherapy and targeted therapy, but few encouraging outcomes have been observed[18]. Overall, despite advances in multimodality therapy, the prognosis of patients with GBM thus remains poor and long-term survival is rare. There is accordingly a need to identify more effective therapies for GBM.
In the current case, the tumor location and the intense side effects meant that total resection with chemoradiotherapy was impossible, and KLP was therefore prescribed. Surprisingly, the patient experienced a remarkable response to KLP therapy, with a reduction in tumor size from about 3.5 cm to about 1 cm. This therapeutic effect might have been related to the anti-tumor effects of the main components of KLP, such as Smilax glabra Roxb. (Tufuling), Panax notoginseng (Burkill) F. H. Chen (Sanqi), Scleromitrion diffusum (Willd.) R. J. Wang (Baihuasheshecao), and Scutellaria barbata D. Don (Banzhilian). Smilax glabra Roxb. (Tufuling) is a natural dietary supplement widely used in food-making and health care, based on its abilities to detoxify and reduce temperature[21]. Previous studies revealed that it also had an anti-tumor function in counteracting the invasiveness of a subset of cancer cells by suppressing the transforming growth factor-β1 pathway[22]. Panax notoginseng (Burkill) F. H. Chen (Sanqi), which has been applied for medical uses for over four centuries, includes saponins that can be effective in the treatment of cancer, partly by modulating the Met/miR-222 axis[23]. Scleromitrion diffusum (Willd.) R.J. Wang (Baihuasheshecao) was shown to suppress GBM growth in vitro by inducing mitochondria-mediated apoptosis via Akt/ERK signaling[24]. Scutellaria barbata D. Don (Banzhilian) is used as an immunomodulatory and anti-tumor agent in TCM, and its extracts have exhibited growth-inhibitory effects in various cancers in vitro and/or in vivo[25]. Recent studies have provided a preliminary understanding of the mechanism of traditional Chinese medicine in regulating the permeability of the blood-brain barrier. Some studies found that astilbin in Smilax glabra Roxb. (Tufuling) enters the brain tissue through the blood-brain barrier, at a low concentration, but with a long duration[26]. Notoginseng saponins R1 and ginsenoside Rg1 in Panax notoginseng (Burkill) F. H. Chen (Sanqi) could penetrate the blood-brain barrier and enter the cerebrospinal fluid in rats[27]. Few studies have investigated the ability of Scleromitrion diffusum (Willd.) R. J. Wang and Scutellaria barbata D. Don to affect blood-brain barrier permeability, but we speculate that other components in KLP may also play a role in assisting the main components to enter the blood-brain barrier. TCMs act on the human body through multiple channels and targets; however, the mechanism of KLP is still unclear.
TCMs have demonstrated visible effects in relieving clinical symptoms, prolonging survival, and preventing recurrence of GBM, and even reducing the toxicity of chemotherapy[28-31]. In addition, they have dual immunomodulatory effects of immune promotion and suppression, which can dramatically enhance the patient’s immune function and improve their quality of life. TCMs are thus widely used as adjuvant therapy in all cancer stages, especially for the palliative treatment of advanced and refractory tumors. Progress in related technologies has allowed researchers to investigate the mechanisms of TCMs in relation to glioma treatment at the molecular level, and increasing evidence has confirmed their effectiveness and reliability[31]. TCMs may thus offer new therapeutic strategies for the treatment of glioma.
Western medicine is usually considered to be the first choice of drug therapy for GBM in clinical practice. However, TMZ treatment was not suitable for the current patient and the TCM KLP was administered as an alternative. Compared with other therapies, KLP has the advantages of lower cost, comprehensive efficacy, and few side effects, and should thus be considered as a recommended option for the treatment of GBM. However, although this report demonstrated the potential suitability of TCM as an alternative therapy for GBM, the detailed mechanisms responsible for its effects remain complex and unknown. Extensive further research and more clinical trials are therefore required to confirm the efficacy and mechanisms of TCMs.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li H S-Editor: Zhang L L-Editor: Webster JR P-Editor: Li JH
| 1. | Poon CC, Sarkar S, Yong VW, Kelly JJP. Glioblastoma-associated microglia and macrophages: targets for therapies to improve prognosis. Brain. 2017;140:1548-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 163] [Article Influence: 20.4] [Reference Citation Analysis (1)] |
| 2. | Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011-2015. Neuro Oncol. 2018;20:iv1-iv86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1156] [Cited by in RCA: 1557] [Article Influence: 259.5] [Reference Citation Analysis (0)] |
| 3. | Jacob F, Salinas RD, Zhang DY, Nguyen PTT, Schnoll JG, Wong SZH, Thokala R, Sheikh S, Saxena D, Prokop S, Liu DA, Qian X, Petrov D, Lucas T, Chen HI, Dorsey JF, Christian KM, Binder ZA, Nasrallah M, Brem S, O'Rourke DM, Ming GL, Song H. A Patient-Derived Glioblastoma Organoid Model and Biobank Recapitulates Inter- and Intra-tumoral Heterogeneity. Cell 2020; 180: 188-204. e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 655] [Article Influence: 131.0] [Reference Citation Analysis (0)] |
| 4. | Anjum K, Shagufta BI, Abbas SQ, Patel S, Khan I, Shah SAA, Akhter N, Hassan SSU. Current status and future therapeutic perspectives of glioblastoma multiforme (GBM) therapy: A review. Biomed Pharmacother. 2017;92:681-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 188] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 5. | Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013-2017. Neuro Oncol. 2020;22:iv1-iv96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 637] [Cited by in RCA: 1261] [Article Influence: 315.3] [Reference Citation Analysis (0)] |
| 6. | Yi GZ, Huang G, Guo M, Zhang X, Wang H, Deng S, Li Y, Xiang W, Chen Z, Pan J, Li Z, Yu L, Lei B, Liu Y, Qi S. Acquired temozolomide resistance in MGMT-deficient glioblastoma cells is associated with regulation of DNA repair by DHC2. Brain. 2019;142:2352-2366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 7. | Alexander BM, Cloughesy TF. Adult Glioblastoma. J Clin Oncol. 2017;35:2402-2409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 370] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 8. | Cao L, Qu D, Wang H, Zhang S, Jia C, Shi Z, Wang Z, Zhang J, Ma J. Toosendanin Exerts an Anti-Cancer Effect in Glioblastoma by Inducing Estrogen Receptor β- and p53-Mediated Apoptosis. Int J Mol Sci. 2016;17. [PubMed] [DOI] [Full Text] |
| 9. | Cha Z, Cheng J, Xiang H, Qin J, He Y, Peng Z, Jia J, Yu H. Celastrol enhances TRAIL-induced apoptosis in human glioblastoma via the death receptor pathway. Cancer Chemother Pharmacol. 2019;84:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Cao P, Cai X, Lu W, Zhou F, Huo J. Growth Inhibition and Induction of Apoptosis in SHG-44 Glioma Cells by Chinese Medicine Formula "Pingliu Keli". Evid Based Complement Alternat Med. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Shi J, Zhang W, He L, Kong F, Pan M, Guo J, Xu X, Wang H, Wang Y. Jinlong capsule inhibits migration and invasion in human glioblastoma cells via the modulation of mTOR/S6 signaling pathway. Drug Des Devel Ther. 2019;13:1023-1032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Feng Y, Zhang P, Chen F, Zhuang W, Lin X. Research on mechanism of action of Chinese medicine compound optimization Kangliuwan on BALB/c nude mice transplantation tumor model of U87. Huanqiu Zhongyiyao. 2018;10:1515-1519. [DOI] [Full Text] |
| 13. | Wang H, Feng Y, Chen F, Zhang P, Lin X. Influence of KangLiu pills on the expressions of apoptosis factors of nude mice with glioma. Xibu Zhongyiyao. 2019;4:8-11. [DOI] [Full Text] |
| 14. | Feng YN, Chen F, Zhang P, Zhuang W, Lin XL. Quality standard for KangLiuWan. Huanqiu Zhongyiyao Zazhi. 2017;5:527-531. [DOI] [Full Text] |
| 15. | Chen F, Lin XL, Xi HW, Zhuang W, Li XL. Simultaneous determination of notoginsenoside R1, ginsenoside Rg1 and ginsenoside Rb1 in Chinese formula KLW by UPLC-MS-MS. Zhongguo Shiyan Fangjixue. 2013;16:156-159. [DOI] [Full Text] |
| 16. | Zhuang W, Lin XL, Jiang DC, Lin QT, Wang YQ, Guo JX, Zhang P, Chen F, Xu G, Wu XG. Efficacy of KLW-1 in treatment of patients with malignant gliomas. Zhongguo Xinyao Zazhi. 2011;19:1894-1897. |
| 17. | Schreck KC, Grossman SA. Role of Temozolomide in the Treatment of Cancers Involving the Central Nervous System. Oncology (Williston Park). 2018;32:555-560, 569. [PubMed] |
| 18. | Tan AC, Ashley DM, López GY, Malinzak M, Friedman HS, Khasraw M. Management of glioblastoma: State of the art and future directions. CA Cancer J Clin. 2020;70:299-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 576] [Cited by in RCA: 1218] [Article Influence: 243.6] [Reference Citation Analysis (0)] |
| 19. | Gerstner ER, Emblem KE, Chang K, Vakulenko-Lagun B, Yen YF, Beers AL, Dietrich J, Plotkin SR, Catana C, Hooker JM, Duda DG, Rosen B, Kalpathy-Cramer J, Jain RK, Batchelor T. Bevacizumab Reduces Permeability and Concurrent Temozolomide Delivery in a Subset of Patients with Recurrent Glioblastoma. Clin Cancer Res. 2020;26:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 20. | Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, Toms S, Idbaih A, Ahluwalia MS, Fink K, Di Meco F, Lieberman F, Zhu JJ, Stragliotto G, Tran D, Brem S, Hottinger A, Kirson ED, Lavy-Shahaf G, Weinberg U, Kim CY, Paek SH, Nicholas G, Bruna J, Hirte H, Weller M, Palti Y, Hegi ME, Ram Z. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA. 2017;318:2306-2316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1175] [Cited by in RCA: 1738] [Article Influence: 217.3] [Reference Citation Analysis (0)] |
| 21. | Hua S, Zhang Y, Liu J, Dong L, Huang J, Lin D, Fu X. Ethnomedicine, Phytochemistry and Pharmacology of Smilax glabra: An Important Traditional Chinese Medicine. Am J Chin Med. 2018;46:261-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 22. | She T, Zhao C, Feng J, Wang L, Qu L, Fang K, Cai S, Shou C. Sarsaparilla (Smilax Glabra Rhizome) extract inhibits migration and invasion of cancer cells by suppressing TGF-β1 pathway. PLoS One. 2015;10:e0118287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Yang Q, Wang P, Cui J, Wang W, Chen Y, Zhang T. Panax notoginseng saponins attenuate lung cancer growth in part through modulating the level of Met/miR-222 axis. J Ethnopharmacol. 2016;193:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Zhang Y, Xie RF, Xiao QG, Li R, Shen XL, Zhu XG. Hedyotis diffusa Willd extract inhibits the growth of human glioblastoma cells by inducing mitochondrial apoptosis via AKT/ERK pathways. J Ethnopharmacol. 2014;158 Pt A:404-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Li L, Xu X, Wu L, Zhu H, He Z, Zhang B, Chi Y, Song G. Scutellaria barbata polysaccharides inhibit tumor growth and affect the serum proteomic profiling of hepatoma H22bearing mice. Mol Med Rep. 2019;19:2254-2262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Li YQ, Gu J, Huan Z, Qiu J, Li YL, Deng CG. Tissue distribution of astilbin in mice. Yaoxue Shijian Zazhi. 2013;03:201-203. [DOI] [Full Text] |
| 27. | Zhao C, Guo H, Xu YY, Wang SX, Chai LJ, Yuan Q, Hu LM. Study of Xueshuantong injection on permeability of the blood brain barrier. Zhongguo Linchuang Yaolixue Zazhi. 2017;03:235-238. [DOI] [Full Text] |
| 28. | Chen ZZ, Lu Y, Du SY, Shang KX, Cai CB. Influence of borneol and muscone on geniposide transport through MDCK and MDCK-MDR1 cells as blood-brain barrier in vitro model. Int J Pharm. 2013;456:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Guo Y, Wang P. Chemo-sensitization effect of borneol combined with paclitaxel on brain glioma cell lines. Yatai Chuantong Yiyao. 2018;9:9-11. [DOI] [Full Text] |
| 30. | Wang H, Guo X, Wu G, Chen L. Combination of tetrandrine and paclitaxel overcomes multidrug resistance on C6/MDR glioma cells. Zhongcaoyao Zazhi. 2018;11:2584-2590. [DOI] [Full Text] |
| 31. | Wang J, Qi F, Wang Z, Zhang Z, Pan N, Huai L, Qu S, Zhao L. A review of traditional Chinese medicine for treatment of glioblastoma. Biosci Trends. 2020;13:476-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |