Published online Apr 26, 2021. doi: 10.12998/wjcc.v9.i12.2811
Peer-review started: September 9, 2020
First decision: December 14, 2020
Revised: December 27, 2020
Accepted: February 22, 2021
Article in press: February 22, 2021
Published online: April 26, 2021
Processing time: 218 Days and 3.6 Hours
Primary carcinoma ex pleomorphic adenoma arising from the tracheobronchial system is rarely reported.
We present a patient with primary carcinoma ex pleomorphic adenoma of the bronchus and review the associated literature for further comparison, including age, clinical manifestations, and diagnostic process. This patient had no history of neoplasms of the salivary gland.
Positron emission tomography played an important role in the staging work-up of primary carcinoma of ex pleomorphic adenoma. Long-term follow-up was necessary for further prognosis analysis.
Core Tip: Positron emission tomography plays an important role in defining the size of the malignant component of primary carcinoma ex pleomorphic adenoma and affects its clinical staging.
- Citation: Yang CH, Liu NT, Huang TW. Role of positron emission tomography in primary carcinoma ex pleomorphic adenoma of the bronchus: A case report. World J Clin Cases 2021; 9(12): 2811-2815
- URL: https://www.wjgnet.com/2307-8960/full/v9/i12/2811.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i12.2811
Carcinoma ex pleomorphic adenoma (Ca ex PA) is a carcinoma arising from a primary or recurrent benign pleomorphic adenoma. Ca ex PA is uncommon, and it has a prevalence rate of 5.6 cases per 100000 malignant neoplasms and a yearly incidence rate of 0.17 tumors per 1 million persons. Cancer predominantly presents in the sixth to eighth decades of life and is slightly more common in females[1]. Although rarely reported, primary Ca ex PA can arise only from the respiratory tract and manifests respiratory symptoms. Only 11 cases have been reported since 1988[2].
Due to its rarity, there is no consensus on the diagnostic protocol for Ca ex PA. It is difficult to discuss radiologic features, particularly features of positron emission tomography (PET). The case reported herein only developed hemoptysis without cough or other respiratory symptoms. This patient is the youngest adult among the patients with Ca ex PA reported to date.
Blood-tinged sputum was observed in June 2018, which progressed to bloody sputum 2 mo later.
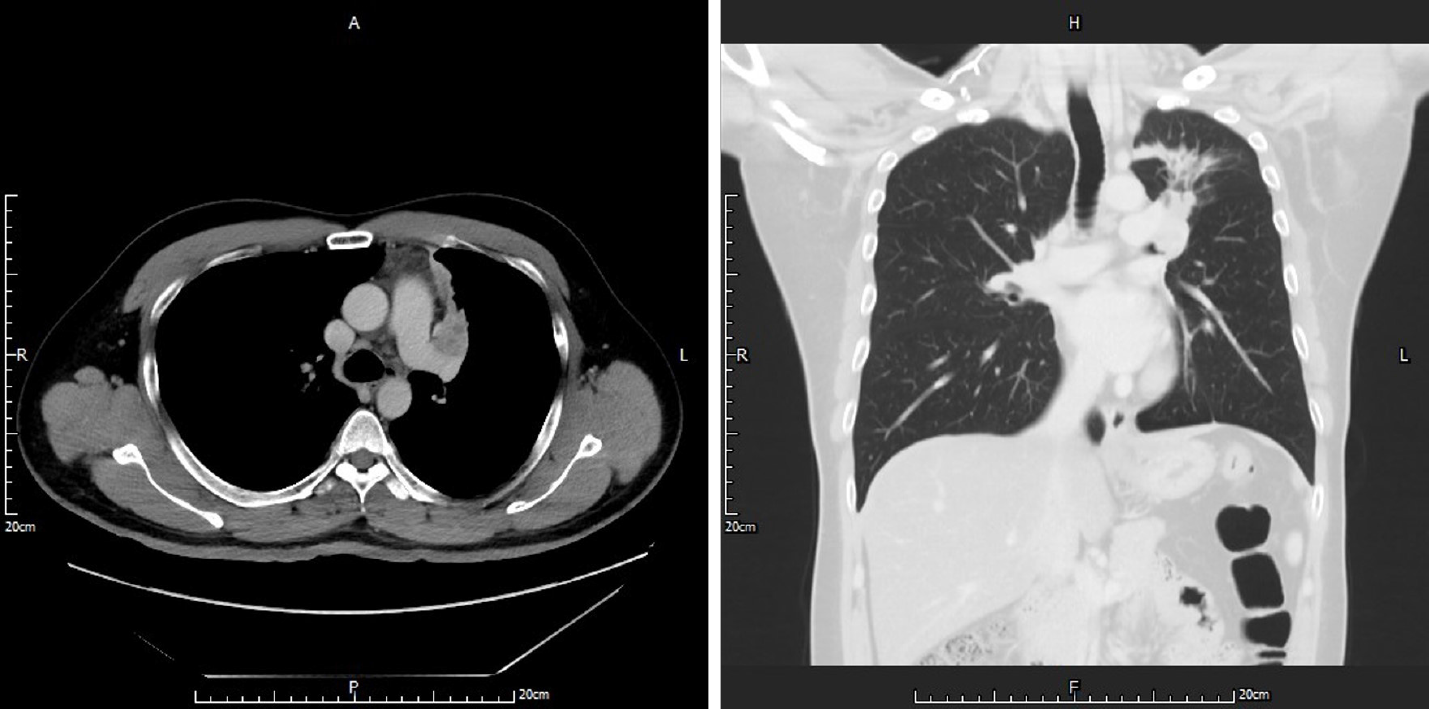
The 40-year-old married man noticed blood-tinged sputum beginning in June 2018, which progressed to bloody sputum 2 mo later. Therefore, he visited a district hospital where chest computed tomography (CT) showed an irregular mass over the left upper lobe of the lung with suspected pulmonary vessel invasion. In addition, endobronchial lesions caused obstructive pneumonitis and partial atelectasis of the left upper lobe of the lung (Figure 1). Bronchoscopy with cytology and biopsy was performed, and the pathological report demonstrated carcinoid tumors of the lung. Due to the impression of a carcinoid tumor of the bronchus of the left upper lobe of the lung, cT4NxMx, stage IIIA at least, he was referred to our medical center for further staging work-up and pre-operative evaluation.
The patient had no systematic disease or surgical history.
He was a non-smoker and did not consume alcohol. His family history was unremarkable.
The patient was considered to have a moderate nutritional status with good performance. Body weight was 80.9 kg, body temperature was 36.3 °C; respiration rate was 12 breaths/min, and heart rate was 72 bpm. Neck and head showed no palpable masses or nodules. Back and spine demonstrated no knocking tenderness.
Chest and lungs examination: No chest wall deformity, no accessory muscle respiration, and no surgical scars were observed. Auscultation showed symmetrical and free expansion, and coarse breathing sounds in the left upper field. Percussion revealed no abnormal dullness. Palpation showed symmetrical and free expansion, no tender points, and no palpable masses. The abdomen revealed normoactive bowel sounds, and was soft without tenderness.
Routine blood tests and blood biochemistry showed no significant abnormalities. Serum levels of tumor markers including carcinoembryonic antigen and squamous-cell-carcinoma antigen were within the normal range.
Chest CT showed an irregular mass over the left upper lobe of the lung with suspected pulmonary vessel invasion. In addition, endotracheal lesions caused obstructive pneumonitis and partial atelectasis of the left upper lobe of the lung.
Contrast-enhanced magnetic resonance imaging of the brain showed no evidence of metastasis. Abdominal sonography showed no evidence of intra-abdominal metastasis.
PET showed: (1) A focally intense fluorodeoxyglucose-avid lesion near the left upper lobe bronchus (maximal standard uptake value = 7.1; metabolic size: 2.0 cm) was seen, compatible with lung cancer (cT2 at least, involving the bronchus); and (2) No metastasis/malignancy associated abnormal fluorodeoxyglucose uptake was noted (Figure 2). Bronchoscopy showed an endobronchial tumor.
Ca ex PA of the left upper lobe of the lung, pT2aN0M0, stage IB.
Video-assisted thoracic surgery with lobectomy was performed. One endobronchial, firm and solid tumor measuring 2.2 cm in diameter without a satellite tumor nodule was found in the main bronchus with bronchial cartilage invasion. Due to the clinically close margin, he was treated with a series of concurrent chemo-radiotherapy after surgery.
Follow-up examinations 1 year after surgery showed no disease recurrence or metastasis. Although the serum carcinoembryonic antigen level was within normal limits at initiation, it continued to decline.
Primary Ca ex PA of the trachea and bronchi is extremely rare. Only 11 cases have been reported. A comparison with our case was made and the results are as follows:
The average age at operation was 59 years and ranged from 44 years to 71 years. Most of the patients were in their sixties[2]. Our patient at 40 years old is the youngest adult to date to be diagnosed and surgically managed.
Symptoms might not be important clues for diagnosis. Although dyspnea and cough seem to be common, our case presented with only hemoptysis.
Chest CT showed mild atelectasis and mild obstructive pneumonitis of the left upper lobe of the lung caused by endobronchial partial obstruction. A description of the radiologic manifestations of Ca ex PA is rare. This should be included in the differential diagnosis when an endobronchial lesion with a lung mass is noted.
It is difficult to determine the malignant tumor size from the whole mass; thus initially, the clinical stage was cT4N0M0 as revealed by contrast-enhanced thoracic CT, with probable invasion of the pulmonary arterial branch. However, PET showed only 2 cm of metabolic tumor volume without evidence of lymphadenopathy or distant metastasis. Therefore, surgical intervention was an option. PET plays an important role in both the detection of lymphadenopathy and distant metastasis of lung cancer. In addition, it can measure the true size of the malignant component of this type of tumor. The pathology report showed that the malignant component of the tumor was 2.2 cm in diameter without lymph-vascular invasion, compatible with a T2a lesion.
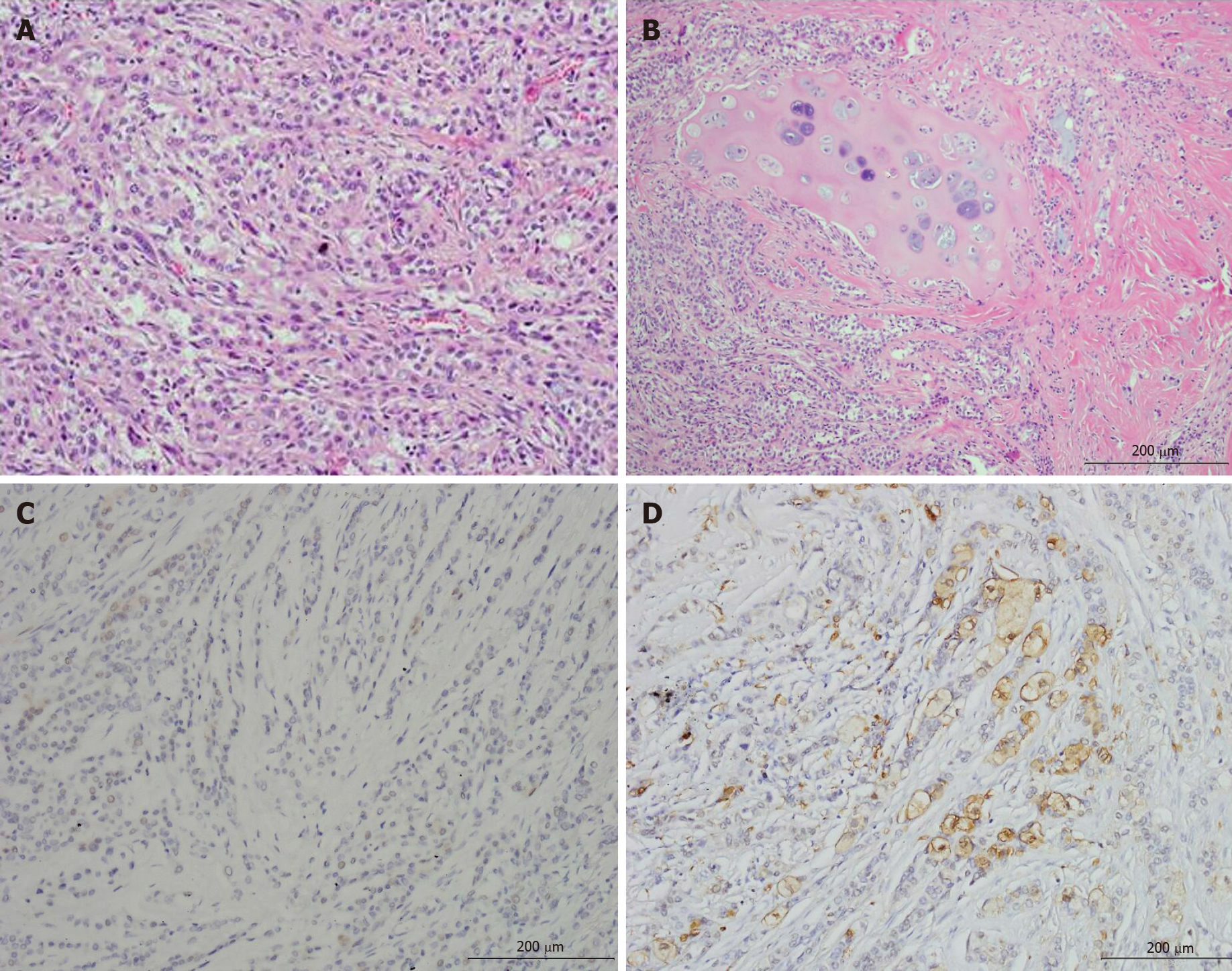
The malignant component of Ca ex PA demonstrated a wide spectrum of histologic differentiation that needs to be recognized as such in order not to be dismissed as a non-small cell carcinoma or poorly differentiated carcinoma. They usually show myoepithelial differentiation, but not adenocarcinoma or salivary duct carcinoma, as commonly seen in tumors arising in the salivary glands[3]. Most likely due to the limitation of inappropriate endobronchial specimens taken during bronchoscopy, the gross morphology of the tumor, hemoptysis as the only symptom and its acute onset, and the patient’s age, the initial impression was a carcinoid lung tumor. However, the final pathology from lobectomy showed a subepithelial solid tumor composed of obvious epithelial cells forming a duct-like structure (Figure 3A), occasional mucin production, and a focal myoepithelial cell component (reactive to S-100 protein, Figure 3D) with clear cytoplasm, accompanied by chondromyxoid and hyalinizing matrix with bronchial cartilage invasion (Figure 3B). Negative reactivity to chromogranin A and weakly positive reactivity to synaptophysin in tumor cells indicated that a carcinoid lung tumor was unlikely. Therefore, the final diagnosis was Ca ex PA (Figure 3).
Here, we report a case of primary Ca ex PA arising from the main bronchus of the left upper lobe of the lung. Additionally, we show that PET may provide some information on the resectability and true size of the malignant component of this type of tumor. Long-term follow-up for analysis of prognosis is necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Guo B, Koumarianou A S-Editor: Gao CC L-Editor: Webster JR P-Editor: Liu JH
| 1. | Antony J, Gopalan V, Smith RA, Lam AK. Carcinoma ex pleomorphic adenoma: a comprehensive review of clinical, pathological and molecular data. Head Neck Pathol. 2012;6:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 161] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 2. | Xu JJ, Wang JW, Zhang MM. Primary carcinoma ex pleomorphic adenoma of the bronchus: report of two cases and review of the literature. Int J Clin Exp Med. 2017;10:3860-3863. |
| 3. | Weissferdt A, Moran CA. Pulmonary salivary gland-type tumors with features of malignant mixed tumor (carcinoma ex pleomorphic adenoma): a clinicopathologic study of five cases. Am J Clin Pathol. 2011;136:793-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |