Published online Apr 26, 2021. doi: 10.12998/wjcc.v9.i12.2751
Peer-review started: December 24, 2020
First decision: January 17, 2021
Revised: January 29, 2021
Accepted: February 24, 2021
Article in press: February 24, 2021
Published online: April 26, 2021
Processing time: 111 Days and 18.8 Hours
In transradial intervention procedures, poor back-up support and noncoaxial alignment of the guide catheter (GC) may result in failure of the balloon or stent to reach the targeted lesion. Methods to provide extra back-up support using the original GC and wire can improve procedural success with reduced complications. A rapid exchange guide extension catheter provides convenient and efficient back-up support while preserving the initial GC and inserted wire.
To evaluate the efficacy and safety of rapid exchange extension catheter in the treatment of type B2/C nonocclusive coronary lesions via the radial access.
A total of 135 patients with type B2/C nonocclusive lesions who were treated via the transradial approach were enrolled in the study. The clinical characteristics, indications for use of the rapid exchange extension catheter, and procedural details and results were reviewed and analyzed. All procedure-related complications and major adverse cardiovascular events were recorded during the in-hospital stay and follow-up period.
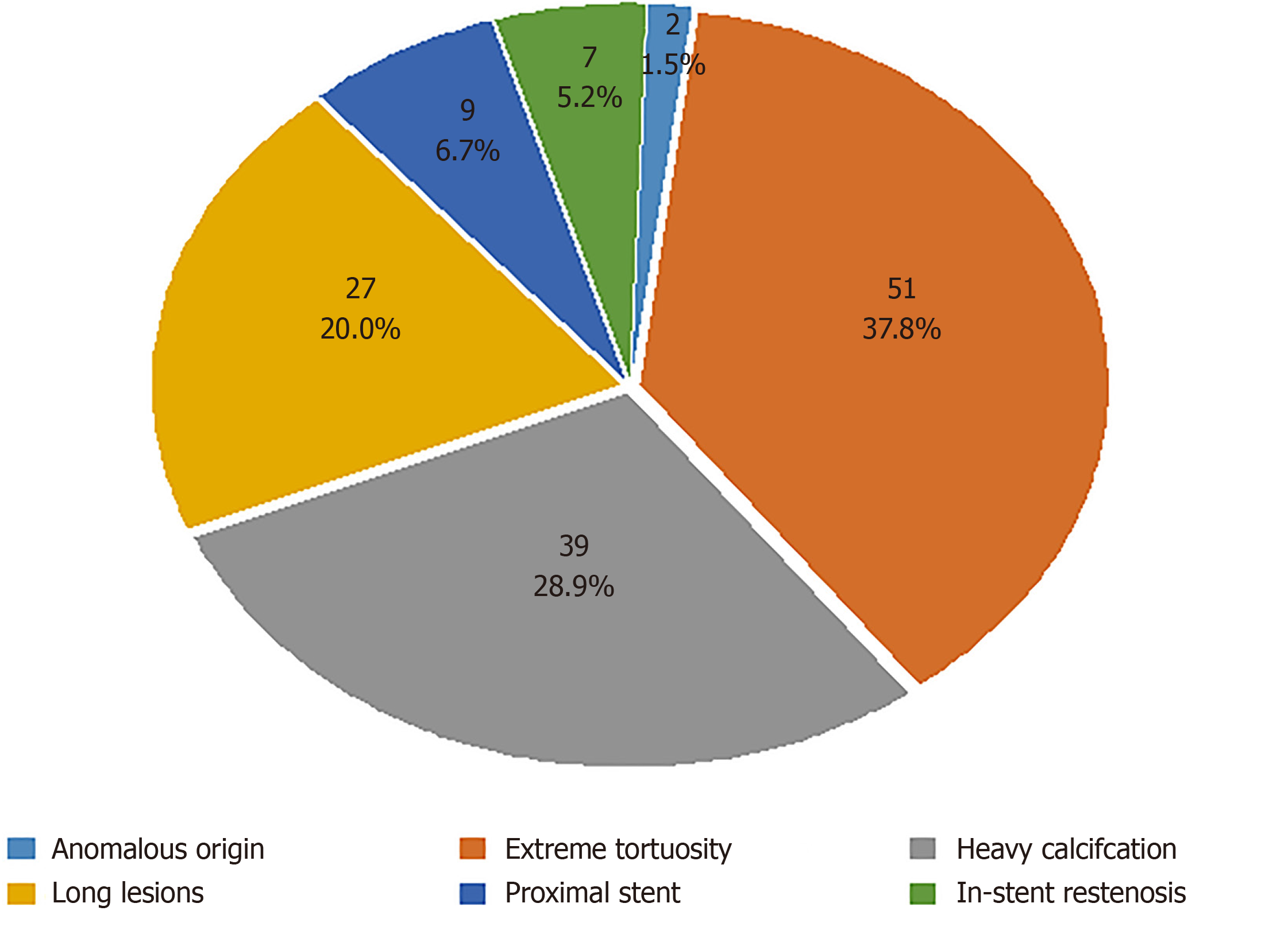
The most common indication for the use of a rapid exchange extension catheter was vascular tortuosity (37.8%), followed by heavy calcification (28.9%), long lesions (20.0%), proximal stent (6.7%), in-stent restenosis (5.2%), and coronary origin anomalies (1.5%). The following technologies failed in passing targeted lesions before delivering the rapid exchange catheter: Multiple predilatation technique (57%), buddy wire technique (33.4%), balloon anchoring technique (5.9%), and cutting balloon modification (3.7%). The mean depth of the extension catheter intubation was 20.56 ± 13.05 mm, and the mean rapid exchange catheter service time was 18.9 ± 9.7 min. The mean length and diameter of stents were 33.5 ± 14.4 mm and 2.75 ± 0.45 mm, respectively. The total rate of technique success (balloon or stent successful crossing of the target lesion with this technique) was 94.8%.
The rapid exchange extension catheter technique showed acceptable safety and efficacy in the transradial coronary interventions of type B2/C nonocclusive coronary lesions. We recommend this technique to assist in complex lesion intervention via radial access.
Core Tip: Transradial intervention (TRI) has been widely used due to its advantages compared with the transfemoral approach. In TRI, poor back-up support may result in failure of the balloon or stent to reach the targeted lesion. A rapid exchange guide extension catheter provides convenient and efficient back-up support in the TRI procedures. The findings of our study revealed the efficacy and safety of the rapid exchange extension catheter for the balloon and stent delivery in the treatment of type B2/C nonocclusive coronary lesions. The rapid exchange extension catheter technique is a useful approach for complex coronary lesions via the radial access.
- Citation: Wang HC, Lu W, Gao ZH, Xie YN, Hao J, Liu JM. Application of a rapid exchange extension catheter technique in type B2/C nonocclusive coronary intervention via a transradial approach. World J Clin Cases 2021; 9(12): 2751-2762
- URL: https://www.wjgnet.com/2307-8960/full/v9/i12/2751.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i12.2751
The first transradial catheterization approach to coronary angiography was reported in 1989. In recent years, transradial intervention (TRI) has been increasingly used as the first choice for percutaneous coronary intervention (PCI) in many hospitals in China and elsewhere around the world because it has better compliance and few bleeding complications and requires a shorter hospital stay than transfemoral access[1-5]. However, operators prefer femoral access when dealing with complex coronary lesions, which require more backup support and devices. The size of the radial artery limits the guide catheter (GC) to a size no larger than 7F. Furthermore, it also has intrinsic weaknesses, including inadequate backup support and poor coaxiality due to different anatomical characteristics of the support point angulation.
In TRI procedures, the balloon or stent may fail in reaching the targeted lesion area because of poor backup support, and an improper procedure may even cause stent deformity or detachment[6,7]. Therefore, methods to further improve backup support using the original GC and wire via the radial approach have been a hot topic. The rapid exchange guide extension catheter is a new-generation extension mother-child catheter system. This device provides convenient and efficient back-up support in the implementation of 6F GCs while preserving the initially inserted wire to avoid the risk of entering the vascular compartment in cases where the wire is reinserted[8].
The purpose of this study was to describe our clinical experience with a rapid exchange extension catheter for back-up support and balloon and stent delivery in the treatment of type B2/C nonocclusive coronary lesions via the radial access at a single center in China.
Between January 2018 and September 2019, a total of 1401 consecutive patients underwent PCI, among whom the rapid exchange extension catheter (Expressman™, APT Medical, China) was used in 157 patients at The Second Hospital of Hebei Medical University, Shijiazhuang, China. Among the 157 patients, 4 underwent the transfemoral route, 18 had chronic total occlusion (CTO) lesions, and the remaining 135 with type B2/C nonocclusive coronary lesions underwent transradial coronary interventions. Patient clinical characteristics were reviewed and analyzed, including age, sex, smoking status, hypertension, diabetes, hyperlipidemia, myocardial infarction, coronary artery bypass graft history, clinical presentation, and indications for coronary angiography. All patients provided written informed consent after approval by the Ethics Committee.
Each target lesion was classified as type B2 or C according to the definitions established by the American Heart Association/American College of Cardiology[9]. Indications for the use of the rapid exchange extension catheter included anomalous origin of the coronary artery, extreme tortuosity, heavy calcification, long lesions, or in-stent restenosis. In case of multiple indications, the key point leading to extension catheter use was listed as primary. A tortuous lesion was defined as having at least three 45-degree or greater bends in a vessel direction along the main trunk during the diastolic period[9]. Calcification was identified based on density as visualized in the wall of the vessel before injecting a contrast agent[10].
Transradial PCI techniques with a rapid exchange extension catheter were performed by one experienced interventional operator following standard clinical protocols with radial artery access and a 6F GC and radial sheath. The rapid exchange extension catheter was used when the balloon or stent could not be delivered to the target lesion after high-pressure balloon predilatation without the need to change the original guiding catheter. Technique success was defined as the balloon or stent successfully passing through the target lesion with rapid exchange extension catheter support. PCI success was defined as a successful stent implantation or drug-coated balloon (DCB) therapy in the targeted lesion area with a residual stenosis < 20% and TIMI grade 3 flow. Angiographic outcome (target lesion, and type and character of lesion, such as anomalous origin, tortuosity, calcification, long lesions, and in-stent restenosis) and procedural data (type of guiding catheter, guidewire, stent, preprocess for the lesion, and depth of intubation of the extension catheter) were recorded.
Dual antiplatelet therapy with aspirin and clopidogrel or ticagrelor was administered orally before and after performing PCI. Unfractionated heparin (70-100 IU/kg) was administered during the PCI procedure after achieving arterial access. Patients with a higher blood risk were treated with bivalirudin (intravenous infusion of 0.75 mg/kg was started and maintained at 1.75 mg/kg per hour until 4 h after surgery). If there are no contraindications, statins and other secondary prophylactic drugs should be administered. Surgical safety was defined as the absence of periprocedural complications (perforation, dissection, stent dislodgement, and fracture of the extension catheter). All procedure-related complications and major adverse cardiovascular events (MACEs) (including all-cause death, recurrence of myocardial infarction, and repeated revascularization) were recorded during the in-hospital stay and follow-up period of 1 mo.
Analyses were performed using SPSS statistical software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, United States). Continuous variables are expressed as the mean ± SD, and categorical variables are expressed as numbers and percentages (%). Non-normally distributed continuous variables are expressed as the median and interquartile range. Categorical data were compared using a chi-square test or Fisher’s exact test. Relative risks are reported with 95% confidence intervals. P < 0.05 was considered statistically significant.
Among the 1401 enrolled patients, 157 were treated with a rapid exchange extension catheter, and the utilization rate was 11.2%. Excluding 18 patients with CTO, the catheter utilization rate was 97.1% (135 cases) via the transradial approach and 2.9% (4 cases) via the transfemoral route in nonocclusive lesion patients. Baseline clinical characteristics of the patients are presented in Table 1. The mean age was 62.8 ± 9.5 years, and the 104 males (77.0%) outnumbered the 31 females (23.0%). Hypertension was the most common risk factor (n = 102; 75.6%), followed by diabetes mellitus (n = 59; 43.7%) and hypercholesterolemia (n = 14; 10.4%). The most common clinical indication was unstable angina (n = 94; 69.6%), followed by ST-segment elevation myocardial infarction (n = 25; 18.5%) and non-ST-segment elevation myocardial infarction (n = 16; 11.9%) (Table 1).
| Clinical characteristic | n | % |
| Mean age (yr) | 62.8 ± 9.5 | |
| Male | 104 | 77.0 |
| Female | 31 | 23.0 |
| BMI (m/kg2) | 26.2 ± 2.9 | |
| Creatinine/(μmol/L) | ||
| Previous | 77.5 ± 27.2 | |
| Postoperation | 82.8 ± 30.1 | |
| Risk factors | ||
| Hypertension | 102 | 75.6 |
| Diabetes mellitus | 59 | 43.7 |
| Hypercholesterolemia | 14 | 10.4 |
| Angiography indication | ||
| Unstable angina | 94 | 69.6 |
| STEMI | 25 | 18.5 |
| NSETMI | 16 | 11.9 |
Technique success (successful crossing of the target lesion) was achieved with this technique in 128 procedures (success rate 94.8%); the rate of PCI success was 92.6% (125 cases, including 1 case with DCB therapy). Three cases did not undergo stent implantation due to small target vessels after balloon pass and were treated by PTCA alone. Among the 7 patients who failed with this technique, coronary artery bypass grafting (CABG) was performed in 5 patients; the other 2 cases who refused CABG treatment had refractory angina despite optimal drug therapy.
As shown in Figure 1, the most common indication for the use of a rapid exchange extension catheter was vascular extreme tortuosity (51 cases, accounting for 37.8%), followed by heavy calcification (39 cases, 28.9%), long lesions (27cases, 20.0%), proximal stent (9 cases, 6.7%), in-stent restenosis (7 cases, 5.2%), and coronary origin anomalies (2 cases, 1.5%). The right coronary artery (RCA) was the most commonly intervened vessel (43.0%), followed by the left anterior descending artery (LAD, 33.3%) and the left circumflex artery (LCX, 23.7%). Among the RCA lesions, 52 cases were treated with a rapid exchange extension catheter combined with a 6F GC of JR (38.5%), and the remaining 6 cases were combined with SAL (4.4%). In LAD lesions, a JL GC was used in 9 (6.7%) cases, and EBU was used in 36 (26.7%) cases; among LCX lesions, there were 5 (3.7%) cases of JL and 27 (20.0%) cases of EBU (Table 2).
| Target vessel | n (%) | Type of GC | n (%) |
| RCA | 58 (43.0) | JR | 52 (38.5) |
| SAL | 6 (4.4) | ||
| LAD | 45 (33.3) | JL | 9 (6.7) |
| EBU | 36 (26.7) | ||
| LCX | 32 (23.7) | JL | 5 (3.7) |
| EBU | 27 (20.0) |
Most of the interventions were performed through the right radial artery (128 cases; 94.8%); we attempted 2 cases successfully via the distal radial artery. The majority of operations using the rapid exchange extension catheter had difficulty in stent delivery (96 cases; 71.1%), and 4 cases had difficulty in posterior expansion balloon delivery after stent implantation. The technologies that failed in passing target lesions before delivering the rapid exchange extension catheter included the multiple predilatation technique (77 cases; 57%), buddy wire technique (45 cases; 33.4%), balloon anchoring technique (8 cases; 5.9%), and cutting balloon modification (5 cases; 3.7%). The estimated mean depth of extension catheter intubation into the target vessel was 20.56 ± 13.05 mm, and the mean rapid exchange extension catheter service time was 18.9 ± 9.7 min. The mean length and mean diameter of the stents were 33.5 ± 14.4 mm and 2.75 ± 0.45 mm, respectively (Table 3).
| Procedural characteristic | n (%) or mean ± SD |
| Procedural results | |
| Technique success | 128 (94.8) |
| PCI success | 125 (92.6) |
| Stent implantation | 124 (91.9) |
| DCB therapy | 1 (0.7) |
| Artery path | |
| Right radial artery | 128 (94.8) |
| Left radial artery | 5 (3.7) |
| Distal radial artery | 2 (1.5) |
| Indication for using a rapid exchange extension catheter | |
| Difficult balloon delivery | 35 (25.9) |
| Difficult stent delivery | 96 (71.1) |
| Difficult posterior expansion balloon | 4 (3.0) |
| Preprocess lesion before delivering the rapid exchange catheter | |
| Multiple predilatation | 77 (57.0) |
| Buddy wire technique | 45 (33.4) |
| Balloon anchoring technique | 8 (5.9) |
| Cutting balloon modification | 5 (3.7) |
| Depth of extension catheter intubation (mm) | 25.3 ± 15.4 |
| Rapid exchange catheter service time1 (min) | 18.9 ± 9.7 |
| PCI operation time2 (min) | 35.8 ± 16.6 |
| Mean length of stents (mm) | 33.5 ± 14.4 |
| Mean diameter of stents (mm) | 2.75 ± 0.45 |
| Length of DCB (mm) | 30.0 |
| Diameter of DCB (mm) | 3.0 |
| Contrast dose (mL) | 162.2 ± 38.3 |
| Perioperative dual antiplatelet | |
| Aspirin + clopidogrel | 77 (57.0) |
| Aspirin + ticagrelor | 58 (43.0) |
| Perioperative anticoagulant | |
| Unfractionated heparin | 98 (72.6) |
| Bivalirudin | 37 (27.4) |
Regarding safety, no perforation caused by the guide wire, air embolism, acute stent thrombosis, or rapid exchange extension catheter fracture occurred. Proximal vessel dissections occurred in 9 patients after balloon predilatation, though these occurrences were not related to the insertion of the extension catheter. Stents were deformed in 6 cases while crossing the collar segment of the rapid exchange extension catheter, and only 1 stent was stripped off its delivery balloon. Pressure damping was observed in 27 patients (accounting for 20.0%) and was relieved when the extension catheter was withdrawn. No case of sustained pressure damping that required abandoning rapid exchange extension catheter usage was observed. Five (3.7%) cases had perioperative gingival or mucosal bleeding. No major bleeding, stent thrombosis, or MACE occurred in any of the enrolled patients during the hospitalization or the 1-month follow-up period. The data are summarized in Table 4.
| Adverse event | n (%) |
| Intraoperative complication | |
| Perforation | 0 |
| Dissection | 9 (6.7) |
| Thrombosis | 0 |
| Air embolism | 0 |
| Pressure damping | 27 (20.0) |
| Stent deformation or stripping | 6 (4.4) |
| Extension catheter fracture | 0 |
| Perioperative complication | |
| Bleeding | 5 (3.7) |
| Major bleeding | 0 |
| Stent thrombosis | 0 |
| MACEs during hospitalization | |
| Recurrence of myocardial infarction | 0 |
| Repeated revascularization | 0 |
| All-cause death | 0 |
| MACEs in the one-month follow-up | |
| Recurrence of myocardial infarction | 0 |
| Repeated revascularization | 0 |
| All-cause death | 0 |
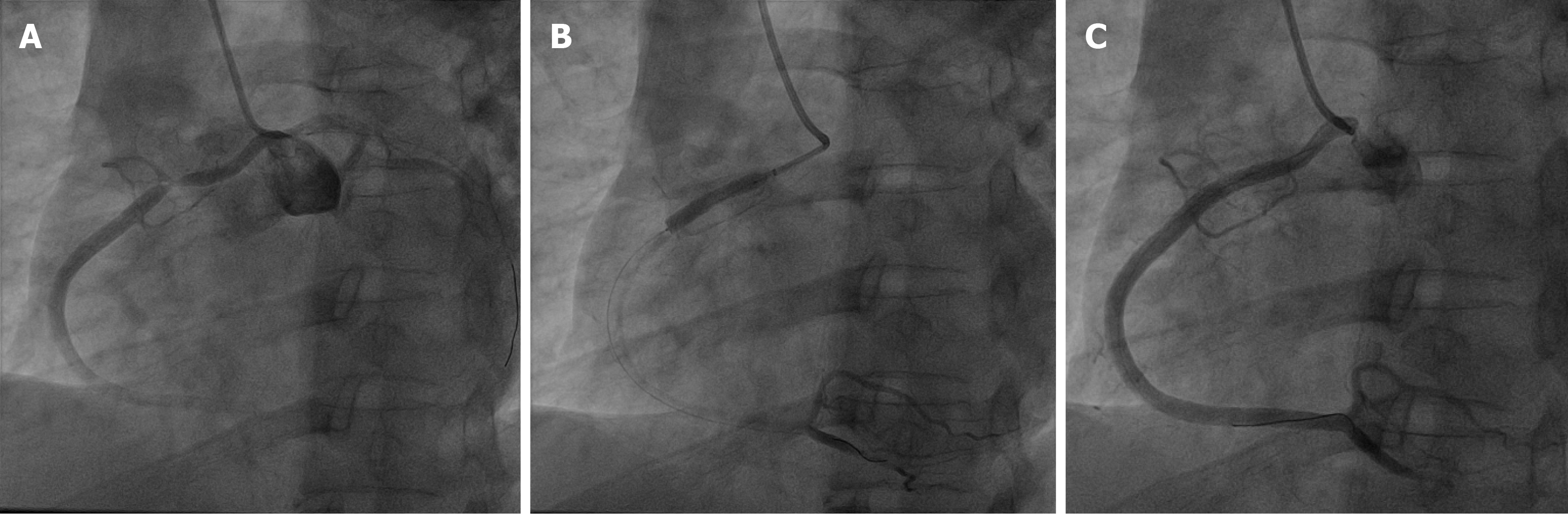
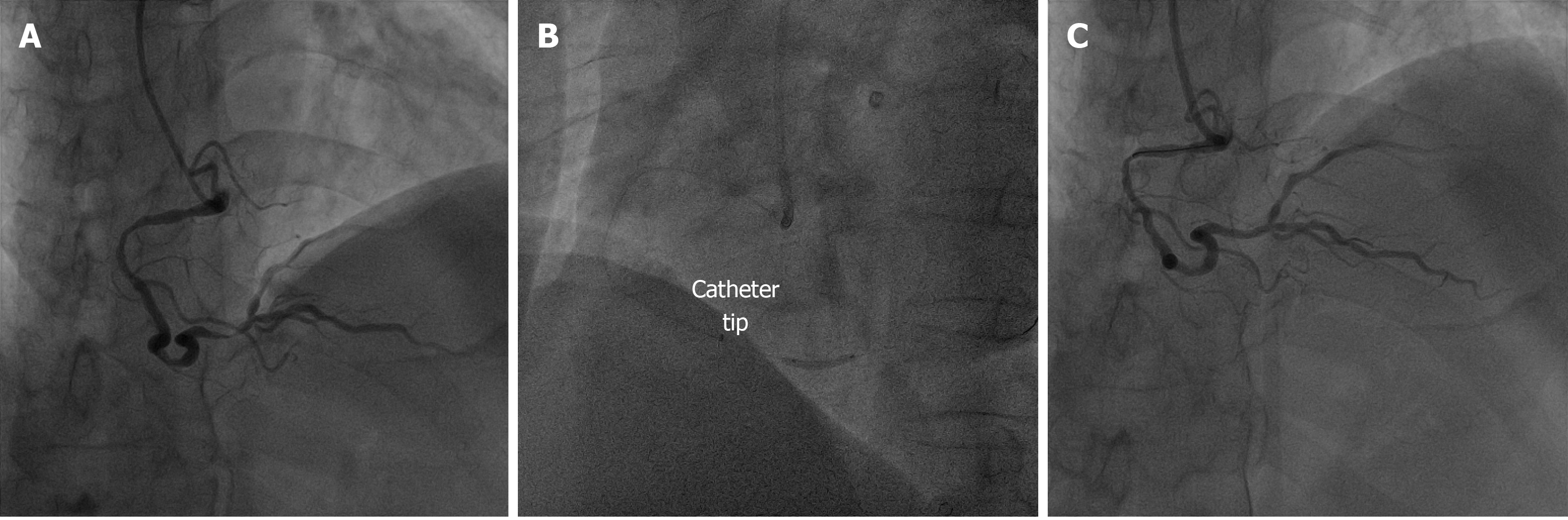
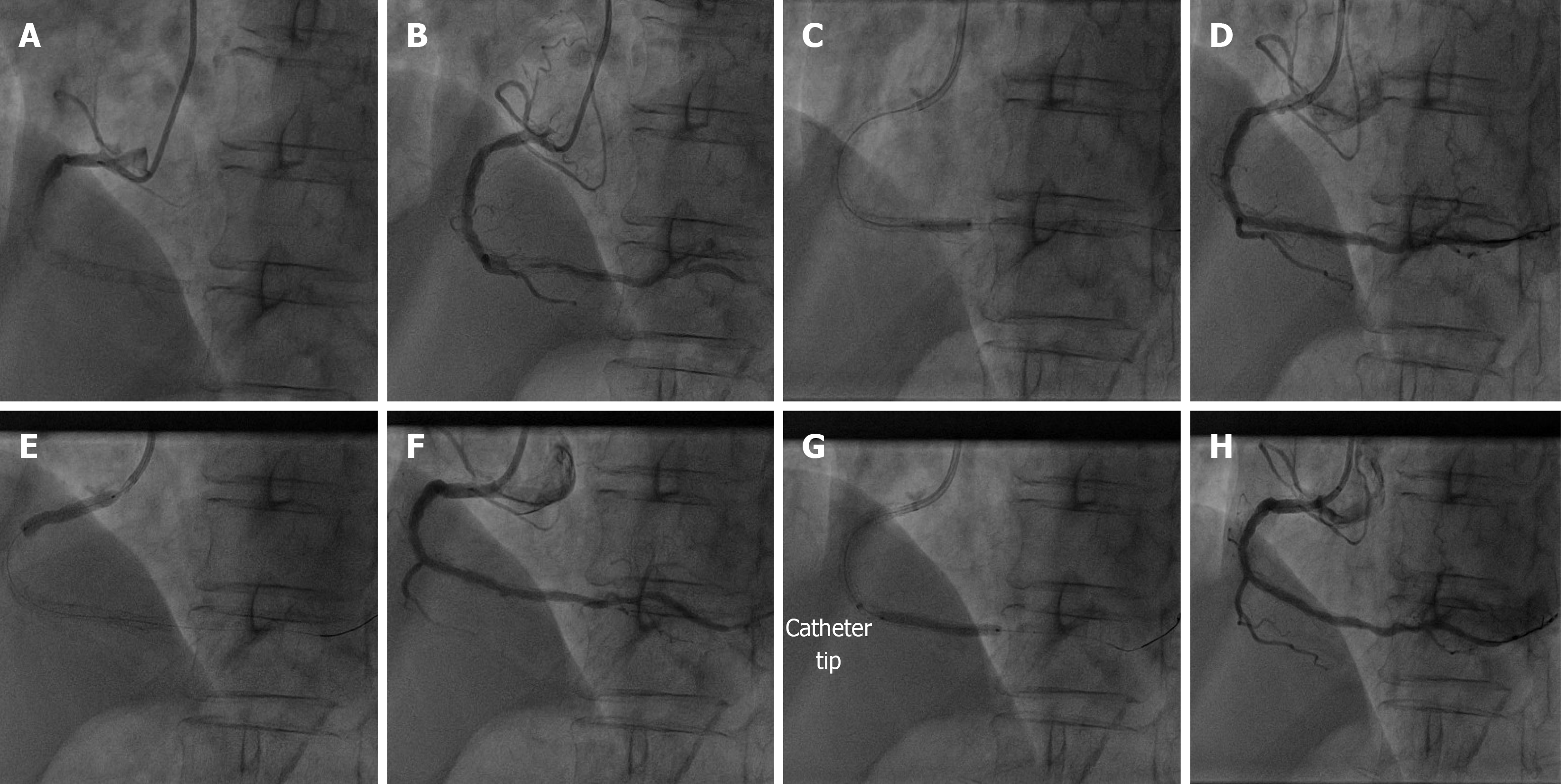
Several cases of the application of rapid exchange extension catheter are reported (Figures 2-4).
With the dramatic development of surgical techniques and equipment, TRI has been widely used due to its advantages compared with the transfemoral approach, including decreased incidence of complications, earlier patient mobilization, and improved patient comfort[11,12]. The proper PCI strategy with appropriate coronary hardware is crucial to ensure the success of the PCI procedure. The development and application of coronary interventional devices are important factors in improving the success rate of PCI[13]. GC extension systems have been one of the most powerful approaches to providing additional back-up support with minimal trauma to the proximal coronary artery[14-16]. The PCI procedural success rate with the use of GC extension systems ranges from 93% to 98%[17,18].
Complex coronary anatomical features, including severe calcification, extreme vessel tortuosity, CTOs, and coronary anomalies often render PCI challenging and time-consuming[19-23]. TRI procedures may result in failure of the balloon or stent to reach the targeted lesion area in these cases because of inadequate backup support and poor coaxiality[24]. These problems can be circumvented by upsizing different GCs, the use of buddy wires, strong support wires, anchoring balloons, deep insertion of the GC, or commonly using a mother-child catheter[25-27]. The rapid exchange guide extension catheter is a new-generation extension mother-child catheter system. This extension catheter has a 35-cm catheter with a hydrophilic coating, a larger inner diameter that has more room to deliver an intervention device, and a smaller outer diameter that reduces GC interference. It was developed to provide adequate back-up support and to facilitate device delivery to cross through the target lesion in complex coronary interventions[28,29]. The results of the present research show that the rapid exchange extension catheter technique is a useful approach for complex coronary lesions.
The key technique in the application of the rapid exchange extension catheter is deep insertion to garner more support. The mean depth of intubation in our research was 25.3 ± 15.4 mm, which is similar to that reported by Kumar et al[30]. Deeper intubation of the extension device may cause pressure damping during the operation, after which pressure returns to normal after retracting the catheter. In our study, the time from the extension catheter entering the coronary artery to returning to GC after stent implantation was recorded. The mean time was 18.9 ± 9.7 min, and the mean PCI operation time was 35.8 ± 16.6 min. These data indicate that the application of the rapid exchange extension catheter does not increase the operative time of complex lesions via transradial access. The PCI success rate with this technique and the data for average diameter/length of stents were similar to those reported by Ma et al[31]. In addition, we successfully intervened in a case of in-stent restenosis treated with DCB using the rapid exchange extension catheter (Figure 4). The use of this technique facilitated the delivery of the long and bulky DCB (3.0 mm × 30 mm) atraumatically through the target lesion to the distal vessel segment. The results of our study highlight the feasibility and safety of using the rapid exchange extension catheter in transradial coronary interventions, achieving a high technique success rate with few complications when treating type B2/C nonocclusive coronary lesions.
Although this technique has many advantages, it is worth noting that caution is warranted. We should avoid twisting the rapid exchange extension catheter while pushing the equipment forward. Additionally, care must be taken to avoid forceful manipulation to prevent injury to the coronary artery. Previous studies have reported that coronary dissection is a common complication caused by deep intubation or forceful injection of contrast agent. While withdrawing the extension catheter, it is possible to unintentionally remove the guidewire from the coronary artery, and attention should be paid to the distal guidewire end[32]. Such events were not observed in our research study. Carefulness and slow operating speed play key roles in preventing these adverse events. In addition, the soft, flexible, and atraumatic tip of the rapid exchange extension catheter was designed to minimize the risk of injuring the vessel.
The findings of the present real-world study revealed the effectiveness and safety of the rapid exchange extension catheter for back-up support and balloon and stent delivery in the treatment of complex coronary artery lesions. The application of this technique can shorten the total fluoroscopy time and reduce the contrast agent dose. Therefore, we believe that it is also suitable for patients with renal insufficiency.
In this single-center study, the rapid exchange extension catheter technique showed acceptable safety and efficacy in the transradial coronary interventions of type B2/C nonocclusive coronary lesions. We recommend this technique to assist in complex lesion interventions via the radial approach, thereby ensuring overall procedural success with reduced complications.
Transradial intervention (TRI) has been widely used due to its advantages compared with the transfemoral approach. In TRI, poor back-up support may result in failure of the balloon or stent to reach the targeted lesion.
Methods to provide extra back-up support may improve procedural success with reduced complications. A rapid exchange guide extension catheter can provide the convenient and efficient back-up support in the TRI procedures.
The purpose of our study was to evaluate the efficacy and safety of rapid exchange extension catheter in the treatment of complex coronary lesions via the radial access.
A total of 135 patients with type B2/C nonocclusive lesions underwent transradial coronary interventions in the study. The clinical characteristics, indications for use of the rapid exchange extension catheter, procedural details, procedure-related complications, and major adverse cardiovascular events were recorded and analyzed.
Technique success (successful crossing of the target lesion with this technique) rate was up to 94.8%. The most common indication for the use of a rapid exchange extension catheter was vascular tortuosity, followed by heavy calcification, long lesions, proximal stent, in-stent restenosis, and coronary origin anomalies. The following technologies failed in passing targeted lesions before delivering the rapid exchange catheter: Multiple predilatation technique, buddy wire technique, balloon anchoring technique, and cutting balloon modification. The rapid exchange extension catheter technique showed effectiveness for the balloon and stent deliver in the transradial coronary interventions of type B2/C nonocclusive coronary lesions.
The findings of our study revealed the efficacy and safety of a rapid exchange extension catheter in the treatment of type B2/C nonocclusive coronary lesions. The rapid exchange extension catheter technique is a useful approach for complex coronary lesions via the radial access.
Our study was designed as a retrospective study and was performed at a single study center. Potential patient selection bias and influence by operator experience might have affected the accuracy and efficacy. Larger, multicenter, randomized controlled studies are warranted.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berger BM S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, Budaj A, Niemelä M, Valentin V, Lewis BS, Avezum A, Steg PG, Rao SV, Gao P, Afzal R, Joyner CD, Chrolavicius S, Mehta SR; RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1409] [Cited by in RCA: 1470] [Article Influence: 105.0] [Reference Citation Analysis (0)] |
| 2. | Pasceri V, Patti G, Pelliccia F, Gaudio C, Speciale G, Mehran R, Dangas GD. Complete Revascularization During Primary Percutaneous Coronary Intervention Reduces Death and Myocardial Infarction in Patients With Multivessel Disease: Meta-Analysis and Meta-Regression of Randomized Trials. JACC Cardiovasc Interv. 2018;11:833-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Huff CM, Kapadia S, Rao SV. Mechanisms by which transradial approach may reduce mortality in ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2014;7:621-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Rigatelli G, Zuin M, Ngo TT, Nguyen HT, Nanjundappa A, Talarico E, Duy LCP, Nguyen T. Intracoronary Cavitation as a Cause of Plaque Rupture and Thrombosis Propagation in Patients with Acute Myocardial Infarction: A Computational Study. J Transl Int Med. 2019;7:69-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Peng X, Wei C, Li HZ, Li HX, Bai SZ, Wang LN, Xi YH, Yan J, Xu CQ. NPS2390, a Selective Calcium-sensing Receptor Antagonist Controls the Phenotypic Modulation of Hypoxic Human Pulmonary Arterial Smooth Muscle Cells by Regulating Autophagy. J Transl Int Med. 2019;7:59-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Carlino M, Azzalini L, Colombo A. A novel maneuver to facilitate retrograde wire externalization during retrograde chronic total occlusion percutaneous coronary intervention. Catheter Cardiovasc Interv. 2017;89:E7-E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Singh S, Singh M, Grewal N, Khosla S. Transradial vs Transfemoral Percutaneous Coronary Intervention in ST-Segment Elevation Myocardial Infarction: A Systemic Review and Meta-analysis. Can J Cardiol. 2016;32:777-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Yew KL. Guidezilla guide extension catheter enhances the delivery of bioresorbable vascular scaffold in an anomalous coronary artery. Int J Cardiol. 2016;223:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Turgut O, Yilmaz A, Yalta K, Yilmaz BM, Ozyol A, Kendirlioglu O, Karadas F, Tandogan I. Tortuosity of coronary arteries: an indicator for impaired left ventricular relaxation? Int J Cardiovasc Imaging. 2007;23:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Moussa I, Ellis SG, Jones M, Kereiakes DJ, McMartin D, Rutherford B, Mehran R, Collins M, Leon MB, Popma JJ, Russell ME, Stone GW. Impact of coronary culprit lesion calcium in patients undergoing paclitaxel-eluting stent implantation (a TAXUS-IV sub study). Am J Cardiol. 2005;96:1242-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Rashid M, Lawson C, Potts J, Kontopantelis E, Kwok CS, Bertrand OF, Shoaib A, Ludman P, Kinnaird T, de Belder M, Nolan J, Mamas MA. Incidence, Determinants, and Outcomes of Left and Right Radial Access Use in Patients Undergoing Percutaneous Coronary Intervention in the United Kingdom: A National Perspective Using the BCIS Dataset. JACC Cardiovasc Interv. 2018;11:1021-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Ranwa BL, Priti K. Transulnar versus Transradial Access as a Default Strategy for Percutaneous Coronary Intervention. Heart Views. 2019;20:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Li P, Ruan JW, Liu M, Li SY, Wang ZD, Xie WC. Thrombus aspiration catheter improve the myocardial reperfusion of STEMI patients with high thrombus load during the emergency PCI operation. J Cardiothorac Surg. 2019;14:172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Duong T, Christopoulos G, Luna M, Christakopoulos G, Master RG, Rangan BV, Roesle M, Banerjee S, Brilakis ES. Frequency, Indications, and Outcomes of Guide Catheter Extension Use in Percutaneous Coronary Intervention. J Invasive Cardiol. 2015;27:E211-E215. [PubMed] |
| 15. | Chen Y, Shah AA, Shlofmitz E, Khalid N, Musallam A, Khan JM, Iantorno M, Gajanana D, Rogers T, Hashim H, Bernardo NL, Waksman R. Adverse Events Associated with the Use of Guide Extension Catheters during Percutaneous Coronary Intervention: Reports from the Manufacturer and User Facility Device Experience (MAUDE) database. Cardiovasc Revasc Med. 2019;20:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Sharma D, Shah A, Osten M, Ing D, Barolet A, Overgaard CB, Džavík V, Seidelin PH. Efficacy and Safety of the GuideLiner Mother-in-Child Guide Catheter Extension in Percutaneous Coronary Intervention. J Interv Cardiol. 2017;30:46-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Chen T, Xu W, Cai Y, Wang Q, Guo J, Chen Y. Safety and Efficacy of Guidezilla Extension Catheter for the Percutaneous Treatment of Complex Coronary Lesions. Heart Surg Forum. 2020;23:E147-E150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Chan PH, Alegria-Barrero E, Foin N, Paulo M, Lindsay AC, Viceconte N, Di Mario C. Extended use of the GuideLiner in complex coronary interventions. EuroIntervention. 2015;11:325-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Ma J, Hou L, Qian J, Ge L, Zhang F, Chang S, Xu R, Qin Q, Ge J. The safety and feasibility of guidezilla catheter in complex coronary interventions and an observational study. Medicine (Baltimore). 2017;96:e8172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Tanaka H, Tsuchikane E, Muramatsu T, Kishi K, Muto M, Oikawa Y, Kawasaki T, Hamazaki Y, Fujita T, Katoh O. A Novel Algorithm for Treating Chronic Total Coronary Artery Occlusion. J Am Coll Cardiol. 2019;74:2392-2404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 21. | Shavadia JS, Vo MN, Bainey KR. Challenges With Severe Coronary Artery Calcification in Percutaneous Coronary Intervention: A Narrative Review of Therapeutic Options. Can J Cardiol. 2018;34:1564-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Parekh P, Agrawal N, Vasavada A, Vinchurkar M. Extreme coronary artery tortuosity in association with tortuosity of the systemic arteries: a rare and challenging situation for the interventionist. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Phadke M, Ambardekar K, Shaikh Z, Mahajan AU, Nathani PJ. Study of the Prevalence of Congenital Coronary Anomalies of Origin from the Opposite or Non-coronary Sinus in patients undergoing Invasive Coronary Angiography. J Assoc Physicians India. 2020;68:28-32. [PubMed] |
| 24. | Allende-Carrera R, Viana-Rojas JA, Saldierna-Galván A, López-Quijano JM, Rivera-Arellano JJ, Leiva-Pons JL, Carrillo-Calvillo J. Feasibility of single catheter intervention for multivessel coronary artery disease using transradial approach. Arch Cardiol Mex. 2019;89:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Mahmood A, Banerjee S, Brilakis ES. Applications of the distal anchoring technique in coronary and peripheral interventions. J Invasive Cardiol. 2011;23:291-294. [PubMed] |
| 26. | Chen CY, Huang YY, Tang L, Hu XQ, Fang ZF, Zhou SH. Guidezilla extension catheter for percutaneous interventional therapy of complex lesions via a transradial approach: Case series from a single-center experience. Cardiol J. 2018;25:171-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Mitomo S, Demir OM, Latib A, Colombo A. Buddy-wire technique during rotational Atherectomy: Simple and effective solution to achieve strong back-up support. Catheter Cardiovasc Interv. 2019;93:436-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Yew KL, Kang Z. Guidezilla guide extension catheter facilitated the delivery of long and bulky In.Pact Falcon drug-coated balloon for the treatment of chronic total occlusion lesion. Int J Cardiol. 2015;201:220-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Waggoner T, Desai H, Sanghvi K. A unique complication of the GuideZilla guide extension support catheter and the risk of stent stripping in interventional & endovascular interventions. Indian Heart J. 2015;67:381-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Kumar P, Aggarwal P, Sinha SK, Khanra D, Razi M, Sharma AK, Thakur R, Pandey U, Krishna V. The Safety and Efficacy of Guidezilla Catheter (Mother-in-Child Catheter) in Complex Coronary Interventions: An Observational Study. Cardiol Res. 2019;10:336-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Ma M, Diao KY, Liu XJ, He Y. Early clinical experience with Guidezilla for transradial interventions in China. Sci Rep. 2018;8:5444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Roth C, Berger R, Scherzer S, Krenn L, Gangl C, Dalos D, Delle-Karth G, Neunteufl T. Comparison of magnetic wire navigation with the conventional wire technique for percutaneous coronary intervention of chronic total occlusions: a randomised, controlled study. Heart Vessels. 2016;31:1266-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |