Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2576
Peer-review started: December 8, 2020
First decision: December 30, 2020
Revised: January 11, 2021
Accepted: February 4, 2021
Article in press: February 4, 2021
Published online: April 16, 2021
Processing time: 114 Days and 23.7 Hours
Immunoglobulin D (IgD) multiple myeloma (MM) is a rare subtype of MM and commonly occurs in younger subjects but at a later stage of the International Staging System (ISS) when admitted. As a special type of IgD myeloma, IgD-λ/λ biclonal MM is rarer. Its serum protein electrophoresis and serum immuno-fixation electrophoresis (IFE) might find no anomalies even if the bone marrow (BM) examination is performed. Thus, it is easy to miss the diagnosis.
A 62-year-old man diagnosed as IgD-λ/λ myeloma (ISS stage III) was admitted with fatigue and weight loss. The physical examination suggested an anemic face, a few moist rales at the left lung base, and mild concave edema in both lower extremities. Laboratory examinations showed the elevated creatinine levels, β2-microglobulin, lactic dehydrogenase, and erythrocyte sedimentation rate, while the decreased neutrophils, granulocytes, and hemoglobin. In the serum protein electrophoresis, there appeared two inconspicuous M-spikes. Serum IFE indicated an over-representation of lambda light chain and yielded two monoclonal bands in λ region, but only one corresponding heavy chain band in the antisera to IgD region. The BM histology and BM cytology both supported the diagnosis of IgD-λ/λ myeloma.
This case highlights the differential clinical manifestations and laboratory findings of IgD-λ/λ myeloma to help minimize the chance of misdiagnosis.
Core Tip: Immunoglobulin D (IgD)-λ/λ myeloma is extremely rare and has a later International Staging System stage at diagnosis. The median survival time is shorter than that of other subtypes, and renal insufficiency is prone to occur at the time of diagnosis. Furthermore, the laboratory examination tends to consider IgD-λ/λ myeloma as other isotypes in that its serum immunofixation electrophoresis shows two bands in the λ region but no responding heavy chain band. Therefore, more complete serum immunofixation electrophoresis should be conducted to reduce the rate of missed diagnoses.
- Citation: He QL, Meng SS, Yang JN, Wang HC, Li YM, Li YX, Lin XH. Immunoglobulin D-λ/λ biclonal multiple myeloma: A case report. World J Clin Cases 2021; 9(11): 2576-2583
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2576.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2576
Immunoglobulin (Ig) D multiple myeloma (MM) is a rare disease, accounting for 2.0% to 2.5% of all MM cases, but the incidence has presented an increasing tendency in recent years[1]. In addition to the typical clinical manifestation of “CRAB” (hypercalcemia, renal insufficiency, anemia, or bone lesions), IgD MM is frequently accompanied by infection, fatigue, weight loss, etc.[2,3]. IgD MM is classified into two types, kappa (κ) and lambda (λ); the type λ occupies a dominant position and the IgD κ is rare[4]. The majority of MM are monoclonal; only precious few MM are biclonal, which almost all belong to the heavy chain type, such as IgG/IgA, IgG/IgM, and IgG/IgG[5]. Thus, the infrequent type of light chain biclonal MM, and the IgD-λ/λ biclonal MM, are extremely rare. At present, only a few cases have been reported[6,7].
Compared to the other subtypes of MM, IgD MM is often more common in younger individuals and has a higher incidence of renal failure, a more advanced stage by the international staging system (ISS), and a worse prognosis[8,9]. The laboratory examination frequently presents higher levels of creatinine concentration, lactic dehydrogenase (LDH), β2-microglobulin, and C-reactive protein (CRP) than other MM subtypes[9,10]. The M-spike in serum electrophoresis is not obvious due to the low levels of serum IgD concentration[4,10]. Similarly, the serum protein electrophoresis of IgD-λ/λ MM shows two subtle M-spikes and two bands appear in the serum immunofixation electrophoresis (IFE). Then, combined with the identification of bone marrow (BM) histology, immunohistochemistry, and immunophenotype of myeloma cells, the patients could be diagnosed as IgD-λ/λ myeloma[5,11]. In view of the low levels of serum IgD content and that immune serum anti-IgD is not routinely used in many laboratories, the diagnosis of type IgD-λ/λ myeloma is prone to be missed or confused with a type of light chain myeloma or monoclonal myeloma[12].
In this paper, we report the clinical case of a patient with IgD-λ/λ MM, who presented overexpression of IgD λ and free light chain (FLCs) λ with two bands in serum IFE, in order to summarize the clinical features and laboratory examination to help clinicians enhance the early diagnosis of IgD-λ/λ.
Fatigue and weight loss for more than 1 mo.
A 62-year-old male farmer was hospitalized for fatigue and weight loss for more than 1 mo, without fever or bone pain. The peripheral blood examination in a local hospital indicated severe anemia with a hemoglobin level of 54 g/L and a potentially malignant tumor from the blood system. Therefore, he was admitted to Huaihe Hospital of Henan University.
No particular previous medical history.
The patient had no history of exposure to industrial poisons or radioactive substances, and was not smoking or drinking alcohol. The family history was unremarkable.
The patient presented an anemic face; the percussion of the lungs presented a little dullness, a few moist rales were heard at the left lung base, and mild concave edema was seen in both lower extremities.
Laboratory evaluation at the Huaihe Hospital of Henan University showed a medium degree of anemia with a hemoglobin level of 61 g/L. Further blood examination indicated renal dysfunction and elevated erythrocyte sedimentation rate and N-terminal pro-brain natriuretic peptide (NT-PROBNP) (Table 1). The other laboratory findings, including blood coagulation functions, stool for routine, blood lipids, and blood sugar, were normal.
| Item | Result | Reference range |
| Peripheral blood | ||
| White blood cells (× 109/L) | 4.30 | 4-10 |
| Neutrophils (× 109/L) | 2.89 | 3.5-5.5 |
| Red blood cells (× 1012/L) | 1.81 | 4.0-5.5 |
| Hemoglobin (g/L) | 61 | 120-160 |
| Erythrocyte sedimentation rate (mm/1st h) | 150 | 0-20 |
| Anemia project | ||
| Folic acid (ng/mL) | 4.9 | ≥ 6.59 |
| Vitamin B12 (pg/mL) | 320.00 | 180.00-900.00 |
| Ferritin (ng/mL) | 636.60 | 11.00-306.8 |
| Urine analysis | ||
| Urine protein | +- | - |
| Urine sugar | - | - |
| White blood cells | +- | - |
| Blood | - | - |
| Urinary sediment | Normal | |
| Biochemistry | ||
| Aspertate aminotransferase (U/L) | 28 | 8-40 |
| Alanine aminotransferase (U/L) | 12 | 0-40 |
| Alkaline phosphatase (U/L) | 50 | 40-100 |
| Blood urea nitrogen (mmol/L) | 23.97 | 2.9-8.2 |
| Creatinine (μmol/L) | 874 | 35-80 |
| Uric acid (μmol/L) | 732 | 155-357 |
| Albumin (g/L) | 32.5 | 34-48 |
| Total protein (g/L) | 63 | 60-80 |
| Lactate dehydrogenase (U/L) | 148 | 109-245 |
| N-terminal pro-brain natriuretic peptide (pg/mL) | 9670.00 | 0-125 |
| C-reactive protein (mg/L) | 4.1 | 0-8.2 |
| Ca (mmol/L) | 2.27 | 2.0-2.5 |
| P (mmol/L) | 1.84 | 0.9-1.34 |
| Fe (μmol/L) | 17.4 | 11-30 |
| Serological test | ||
| β2-microglobulin (μg/mL) | > 13.77 | 0.9-2.7 |
| IgM (mg/dL) | 5.55 | 46-304 |
| IgA (mg/dL) | < 6.67 | 82-453 |
| IgG (mg/dL) | 264.00 | 751-1560 |
| LC (mg/dL) | 134.00 | 629-1350 |
| λ-LC (mg/dL) | 1910.00 | 313-723 |
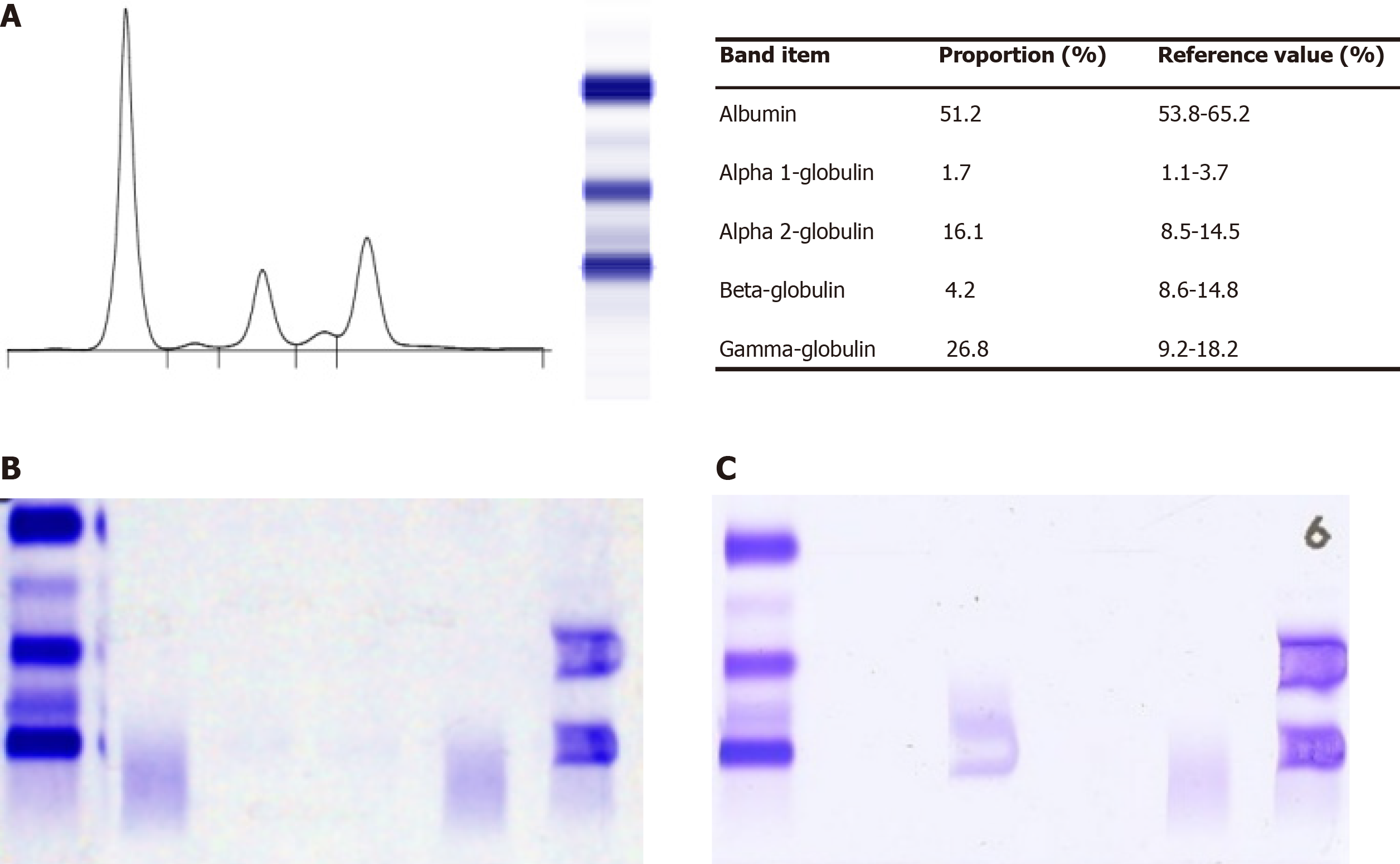
Serum protein electrophoresis on agarose gel suggested an elevation of α2-globulin and γ-globulin, and two slight M-spikes appeared and a band within the γ fraction (the other band within α2 fraction was obscure) was seen. To categorize the M protein, we conducted serum IFE, which consisted of antisera to IgA, IgM, IgG, κ, and λ, and the results yielded two monoclonal bands in the λ region without corresponding heavy chain bands, corresponding to the distinct elevation of serum λ FLC (Figure 1). Thus, we highly suspected the possibility of type IgD or IgE or FLC M protein component. Subsequently, we implemented a second serum IFE with antisera to IgD, IgE, κ, and λ. The results showed two monoclonal bands in antisera to λ but only one corresponding heavy chain band in antisera to IgD, which indicated a diagnosis of IgD-λ/λ myeloma by correlating the clinical manifestation and laboratory examinations.
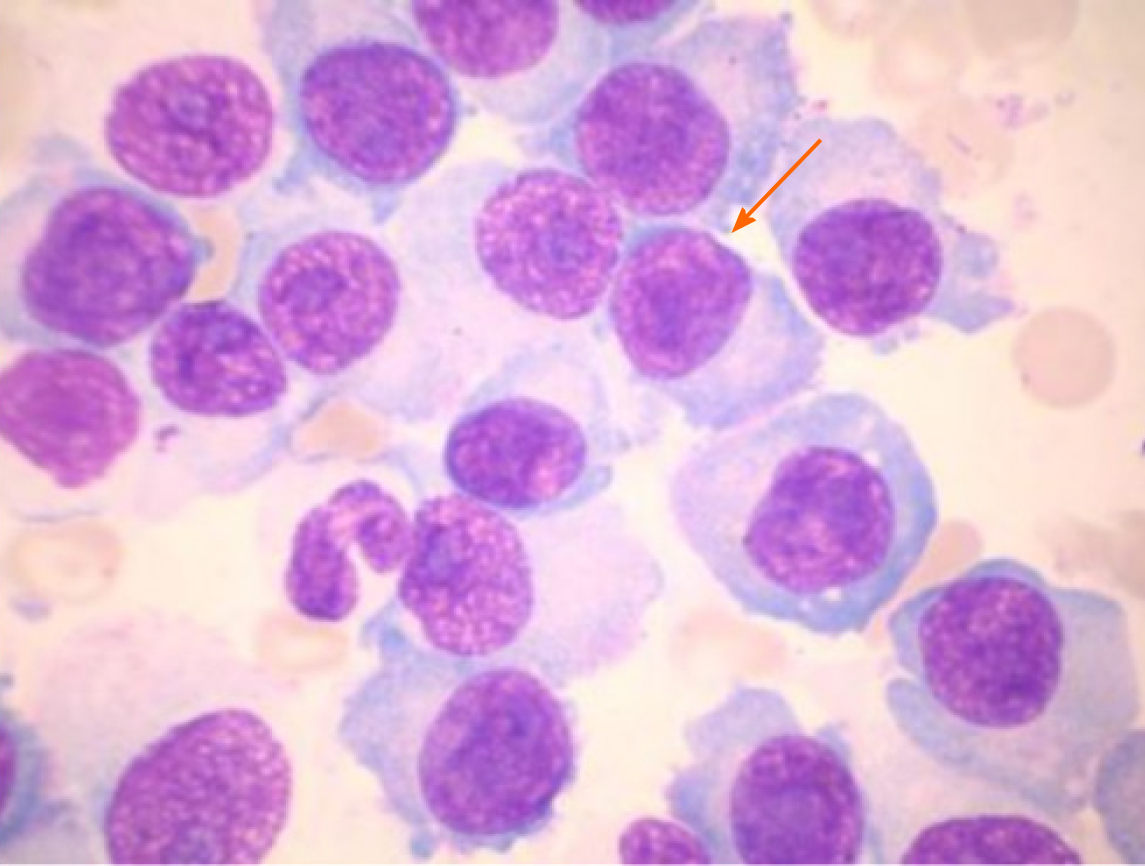
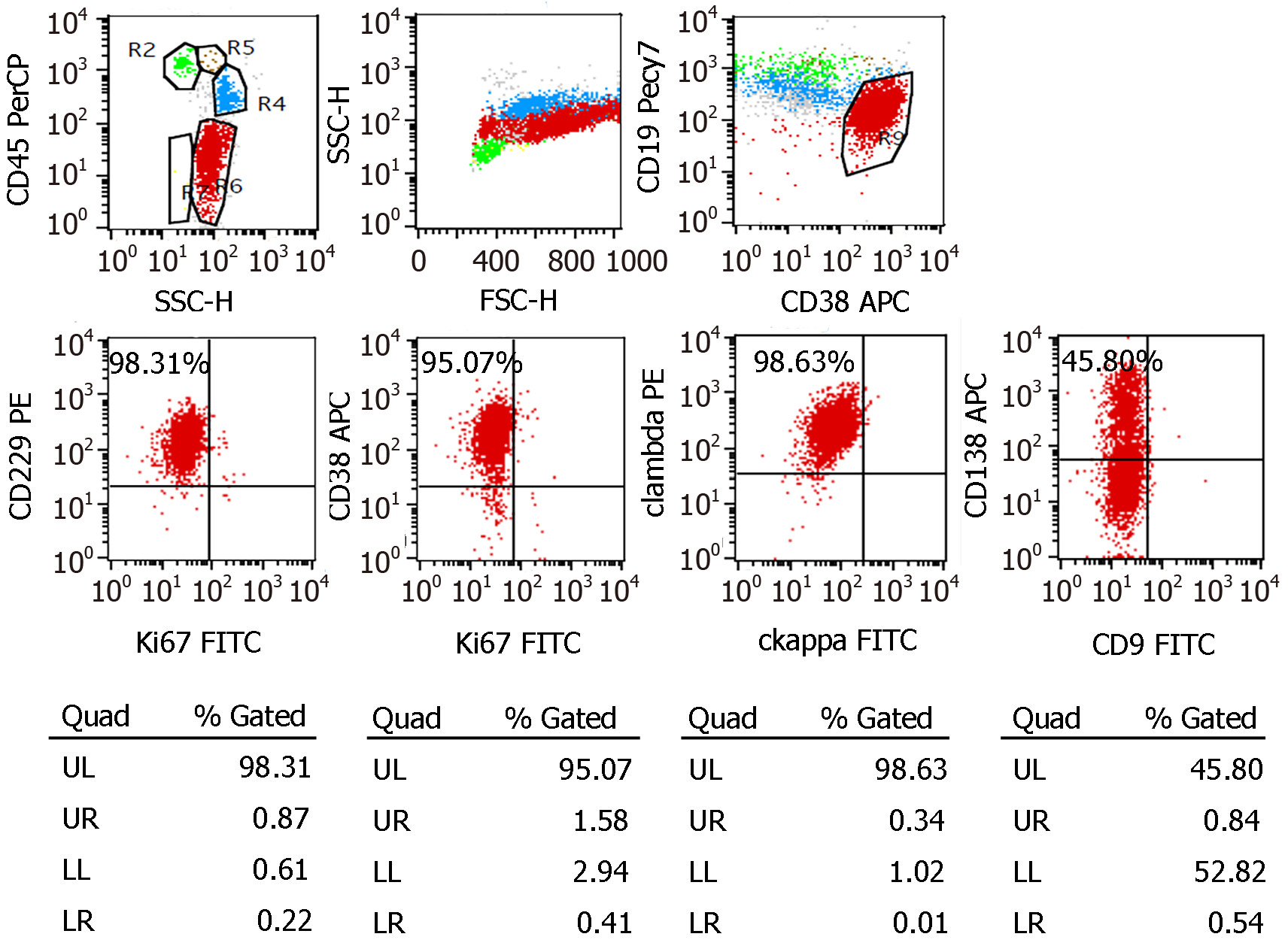
BM cytomorphologic (anterior superior spine) examination found a marked increment of plasma cells, mainly immature plasma cells, which accounted for 82% of the BM nucleated cells (Figure 2). Flow cytometry suggested positivity of monoclonal plasma cells (70.12% of total nucleated red blood cells) with the following immunophenotype: CD38, cytoplasmic lambda, and CD229. All of the monoclonal plasma cells expressed CD229, CD38, and cytoplasmic lambda and partly expressed CD138 (Figure 3). Undoubtedly, BM cytomorphologic examination and flow cytometry supported the diagnosis of plasma cell myeloma. Furthermore, analysis of chromosome karyotype was as follows: 46,XY;46,Y,t(X;4)(p11.2;q21), no abnormal cloning. Gene analysis of the blood tumor mutant group was mainly normal.
Combined with the clinical, and laboratory data above, the patient was diagnosed with stage ISS III myeloma.
IgD-λ/λ MM with renal failure (late stage of uremia).
The patient was treated with BCD chemotherapy (bortezomib plus cyclophosphamide and dexamethasone) for approximately two cycles. The specific method of drug use was as follows: Bortezomib: 1.3 mg/(m2·d) mixed in 0.9% sodium chloride injection (1 mL), which was given subcutaneously on the 1st, 4th, 8th, and 11th days; cyclophosph
For the anemic condition, treatment with blood transfusions (suspended red blood cells with white blood cells removed) was given many times.
As for the renal failure, given the influence of hemodialytic treatment on the patient, symptomatic treatment, such as lowering creatine and protecting renal function, was used; however, the effect was minimal.
At the last follow-up, 5 mo after discharge, the anemic condition had been improved significantly, and the patient was free from the symptom of fatigue, but his renal function continued to deteriorate. Unfortunately, the patient died from a lung infection in the ensuing 2 mo. In this case, the median survival period for the patient with MM (ISS III) tended to be shorter than that for those with the other subtypes of myeloma, which is consistent with most studies[3,8,10].
MM is a malignant tumor characterized by BM infiltration of clonal plasma cells[13]. The abnormal immunoglobulin appears in circulation and can cause damage to related organs or tissues by monoclonal immunoglobulins or their fragments[13]. Hematological examination tends to find anemia, hypercalcemia, elevated β2-microglobulin and LDH, and decreased neutrophils, granulocytes, and hemoglo
For IgD myeloma, the laboratory examination frequently presents higher levels of creatinine concentration, LDH, β2-microglobulin, and CRP than all other subtypes[9,10]. Theoretically, two ‘spikes’ could appear in the serum protein electrophoresis and two bands correspondingly appear in the serum IFE[11,12]. Nevertheless, generally it could not be seen due to the low levels of serum IgD[12]. In view of the infrequency of IgD myeloma, most hospitals or laboratories do not set the antisera to IgD as standard diagnostic items of serum IFE[12]. Moreover, the concentration of IgD is very low, even for IgD myeloma, and the elevation of monoclonal immunoglobulin in serum is so slight that it results in no visible M band and an inconspicuous monoclonal spike on serum electrophoresis[3]. Thus, the diagnosis of type IgD-λ/λ myeloma is apt to be missed or confused with light chain myeloma or monoclonal myeloma.
As in this patient, the ALB (32.5 g/L) decreased slightly, and TP (63.0 g/L) and globulin were within the normal range. The concentrations of IgM, IgA, IgG, IgE, and κ-LC were decreased in the serum IFE while IgD and λ-LC were significantly increased, but the corresponding M peak of serum protein electrophoresis was not visible, which is apt to be missed or misdiagnosed as light chain type MM. To improve the diagnostic level of IgD myeloma, the IgD examination is supposed to be included in the item of serum IFE for patients with MM. In light of the additional costs, the antisera to IgD can be applied when the subject is highly suspected to have MM, but there is no significant abnormality in the serum protein electrophoresis and routine IFE. Moreover, the laboratory examinations should be combined with the clinical manifestations and other examinational findings, such as BM cytology or BM biopsy.
Owing to the infrequency of IgD-λ/λ myeloma mentioned previously[6], its misdiagnosis rate is high. Thus, it is necessary to perform a full set of IFE when two bands in FLC fraction are found but no corresponding heavy chain is present. Consistently, there have been several studies[10,12] suggesting that the antisera to IgD IFE should be included in the routine diagnostic examination of myeloma in tertiary hospitals and medical laboratory centers.
As a first-line drug, bortezomib has been reported to prolong the survival time of patients with myeloma effectively[14]. One study has showed that the response to the bortezomib chemotherapy might be better in younger patients[15]. In addition, IgD MM is common in younger individuals, but the median duration of survival is shorter than in the other isotype[15,16], which indicates that the prognosis of patients with bortezomib chemotherapy might be more closely related to the type of MM than to the age of MM. In this case, the patient with IgD-λ/λ myeloma was alive for only 7 mo since showing symptoms, which might have been the result of the interrupted chemotherapy treatment or the even worse prognosis of double-clonal IgD myeloma than monoclonal IgD myeloma. We could guess that the double-clonal IgD myeloma might have a more aggressive course than monoclonal IgD myeloma and other isotypes. Of course, such a small sample was not tempting enough to support this inference. The specific reason remained unclear and needs further study. In view of the limited number of case reports on IgD-λ/λ myeloma worldwide, we present this case, hoping to provide a deeper understanding of the clinical features and laboratory findings of IgD-λ/λ myeloma, to increase the diagnosis rate in the same type of patients and to develop a more appropriate treatment plan.
In conclusion, the incidence of IgD myeloma is very low[1], and compared to the other types of MM, besides the “CRAB” symptoms, the patients frequently have higher levels of creatinine, LDH, β2-microglobulin, CRP content, and renal failure[2]. Moreover, a later disease stage with a more aggressive course of the disease, as well as younger age, have been noticed at diagnosis of IgD myeloma[8,16]. On the basis of identification of BM histology, immunohistochemistry and immunophenotype of myeloma cells, combined with serum protein electrophoresis and IFE, could be able to diagnose IgD myeloma[5,11]. However, the majority of laboratories have not established the immune serum anti-IgD as the general procedure[12]; thus, IgD-λ/λ myeloma is often misdiagnosed or neglected. To improve the diagnosis rate, this examination should be performed to exclude IgD-λ/λ myeloma when finding light chain myeloma while without any corresponding heavy chain. In addition, bortezomib is still an effective first-line treatment for IgD myeloma[15]; however, more appropriate drugs and treatments should be studied due to its worse treatment effect and prognosis than other isotypes.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li SC S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Zagouri F, Kastritis E, Symeonidis AS, Giannakoulas N, Katodritou E, Delimpasi S, Repousis P, Terpos E, Dimopoulos MA; Greek Myeloma Study Group. Immunoglobulin D myeloma: clinical features and outcome in the era of novel agents. Eur J Haematol. 2014;92:308-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351:1860-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1078] [Cited by in RCA: 1070] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 3. | Bladé J, Lust JA, Kyle RA. Immunoglobulin D multiple myeloma: presenting features, response to therapy, and survival in a series of 53 cases. J Clin Oncol. 1994;12:2398-2404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 132] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Djidjik R, Lounici Y, Chergeulaïne K, Berkouk Y, Mouhoub S, Chaib S, Belhani M, Ghaffor M. IgD multiple myeloma: Clinical, biological features and prognostic value of the serum free light chain assay. Pathol Biol (Paris). 2015;63:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Dash NR, Mohanty B. Multiple myeloma: a case of atypical presentation on protein electrophoresis. Indian J Clin Biochem. 2012;27:100-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Wang XJ, Zhang Z, Yu JX, Li YY, Zhao MS, Yin LF. Mutiple Myeloma with Double Clones of IgD-λ+λ: Two Cases Report. Kunming Yike Daxue Xuebao. 2017;38:124-128. |
| 7. | Rabrenović V, Mijušković Z, Marjanović S, Rabrenović M, Jovanović D, Antić S, Ignjatović L, Petrović M, Pilcević D. Kidney failure as an unusual initial presentation of biclonal gammopathy (IgD multiple myeloma associated with light chain disease)--a case report. Vojnosanit Pregl. 2015;72:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Kim MK, Suh C, Lee DH, Min CK, Kim SJ, Kim K, Moon JH, Yoon SS, Lee GW, Kang HJ, Kim SH, Choi CW, Eom HS, Kwak JY, Kim HJ, Mun YC, Bang SM, Lee K, Shin HJ, Lee JH; Korean Multiple Myeloma Working Party. Immunoglobulin D multiple myeloma: response to therapy, survival, and prognostic factors in 75 patients. Ann Oncol. 2011;22:411-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Reece DE, Vesole DH, Shrestha S, Zhang MJ, Pérez WS, Dispenzieri A, Milone GA, Abidi M, Atkins H, Bashey A, Bredeson CN, Boza WB, Freytes CO, Gale RP, Gajewski JL, Gibson J, Hale GA, Kumar S, Kyle RA, Lazarus HM, McCarthy PL, Pavlovsky S, Roy V, Weisdorf DJ, Wiernik PH, Hari PN. Outcome of patients with IgD and IgM multiple myeloma undergoing autologous hematopoietic stem cell transplantation: a retrospective CIBMTR study. Clin Lymphoma Myeloma Leuk. 2010;10:458-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 10. | Benchekroun L, Ouzzif Z, Bouabdillah M, Jaouhar N, Aoufir F, Aoufi F, Chabraoui L. [Multiple myeloma with D immunoglobulin]. Ann Biol Clin (Paris). 2011;69:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Misra A, Mishra J, Chandramohan J, Sharma A, Raina V, Kumar R, Soni S, Chopra A. Old but Still Relevant: High Resolution Electrophoresis and Immunofixation in Multiple Myeloma. Indian J Hematol Blood Transfus. 2016;32:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 12. | Robier C, Piribauer M, Beham-Schmid C, Aubell K, Neubauer M. IgD-λ myeloma with extensive free light-chain excretion: a diagnostic pitfall in the identification of monoclonal gammopathies. Clin Chem Lab Med. 2017;55:e137-e139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Kumar SK, Rajkumar V, Kyle RA, van Duin M, Sonneveld P, Mateos MV, Gay F, Anderson KC. Multiple myeloma. Nat Rev Dis Primers. 2017;3:17046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 817] [Article Influence: 102.1] [Reference Citation Analysis (0)] |
| 14. | Xu YL, Zhao WH, Tang ZY, Li ZQ, Long Y, Cheng P, Luo J. Guillain-Barré syndrome in a patient with multiple myeloma after bortezomib therapy: A case report. World J Clin Cases. 2019;7:2905-2909. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Lu J, Lu J, Chen W, Wang J, Huo Y, Hou J, Huang X. More frequent IgD and reduced CD200 expression in Chinese patients younger than 50 years old with multiple myeloma: a multicenter analysis. Drug Des Devel Ther. 2016;10:3673-3679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Modi J, Kamal J, Eter A, El-Sayegh S, El-Charabaty E. Immunoglobulin D Multiple Myeloma With Rapidly Progressing Renal Failure. J Clin Med Res. 2015;7:653-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |