Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2367
Peer-review started: December 1, 2020
First decision: December 21, 2020
Revised: December 23, 2020
Accepted: January 26, 2021
Article in press: January 26, 2021
Published online: April 6, 2021
Processing time: 118 Days and 20.6 Hours
Nocardia cyriacigeorgica (N. cyriacigeorgica) infection is uncommon in clinical practice. Pulmonary sequestration complicated with N. cyriacigeorgica has not been reported in the literature. Here, we present a case of pulmonary se-questration complicated with N. cyriacigeorgica infection in an immunocom-petent woman.
A 37-year-old woman complaining of a recurrent cough was admitted to our hospital. Pulmonary sequestration in the lower lobe of the left lung was diagnosed by enhanced computed tomography. Bronchoalveolar lavage fluid was then collected, which showed gram positive bacilli with weakly positive modified acid-fast staining. The pathogen was identified as N. cyriacigeorgica after bacterial culture and mass spectrometry analysis. The patient was diagnosed with pulmonary sequestration complicated with N. cyriacigeorgica infection, and her symptoms quickly improved following anti-infective therapy.
Nocardiosis is considered to be an opportunistic infection. This is the first report of pulmonary sequestration complicated with N. cyriacigeorgica infection in a patient with normal immunity.
Core Tip: Nocardia cyriacigeorgica (N. cyriacigeorgica) infection is uncommon in clinical practice. There are few reports of Nocardia infection in patients with pulmonary sequestration. We report an immunocompetent young woman who was diagnosed with pulmonary sequestration by enhanced computed tomography. Bronchoalveolar lavage was performed for further pathogenic examination, which revealed N. cyriacigeorgica infection in the lesion. This is the first case of pulmonary sequestration complicated with N. cyriacigeorgica infection reported in the literature.
- Citation: Lin J, Wu XM, Peng MF. Nocardia cyriacigeorgica infection in a patient with pulmonary sequestration: A case report. World J Clin Cases 2021; 9(10): 2367-2372
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2367.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2367
Nocardia is an opportunistic pathogen, which is frequently seen in immunosuppressed individuals[1-3]. More than 50 Nocardia species have been identified[1,4], including Nocardia asteroides, Nocardia brasiliensis, Nocardia farcinica, and Nocardia otitidiscaviarum, which are the main species causing disease in humans, and Nocardia cyriacigeorgica (N. cyriacigeorgica) is a relatively rare pathogen[5]. N. cyriacigeorgica infection has been reported in organ transplant recipients, long-term glucocorticoid users, and patients with several chronic pulmonary diseases[2,5-8]. There are few reports of Nocardia infection in patients with pulmonary sequestration. Here, we report a case of pul-monary sequestration complicated with N. cyriacigeorgica infection diagnosed in our hospital.
A 37-year-old woman was admitted to our hospital on September 15, 2020 due to recurrent cough for more than 10 mo.
The patient developed a paroxysmal cough accompanied by a small amount of white sputum 10 mo ago. She had no chills, fever, chest pain, hemoptysis, or shortness of breath. She received symptomatic treatment such as anti-infection at a local hospital but her symptoms persisted during this period. The above symptoms recurred 1 mo ago with a little yellow sputum. Fever and hemoptysis were absent. The patient was admitted to our hospital for further treatment.
The patient was thin and weighed only 40 kg (Body mass index: 15.6). Her temperature was 37.4 °C, pulse rate was 99 bpm, respiratory rate was 19 breaths/min, and blood pressure was 100/63 mmHg. No clubbing of fingers, icterus, or generalized lymphadenopathy were observed. Clinical examinations of the cardiovascular, gastrointestinal, and nervous systems were normal, but crackles were found in the lower lobe of the left lung during lung auscultation.
Laboratory studies showed normal white blood cells (8.6 × 109/L), and the neutrophil ratio was 83.0%. Erythrocyte sedimentation rate was 26 mm/h (normal value < 15 mm/h), and high-sensitivity C-reactive protein was 8.2 mg/L (normal value < 8.0 mg/L). Arterial partial pressure of oxygen was 91 mmHg (partial pressure of oxygen/fraction of inspiration O2 433.3 mmHg), and arterial partial pressure of carbon dioxide was 41 mmHg. The 1,3-β-D-glucan test and galactomannan test were both negative.
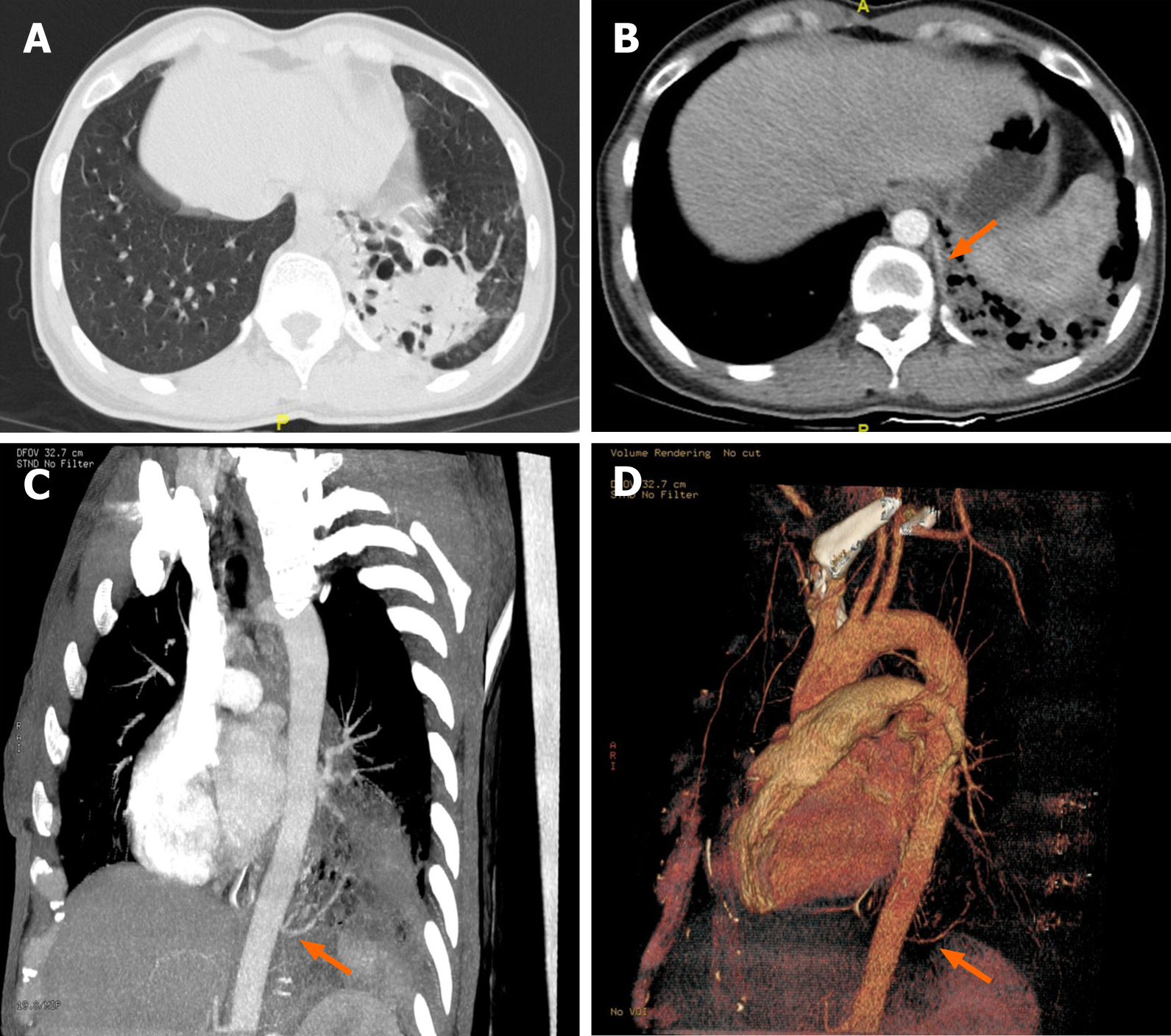
Enhanced computed tomography images revealed a honeycomb lesion in the lower lobe of the left lung, and an enhanced vascular shadow was seen in the descending aorta, which was consistent with pulmonary sequestration (Figure 1).
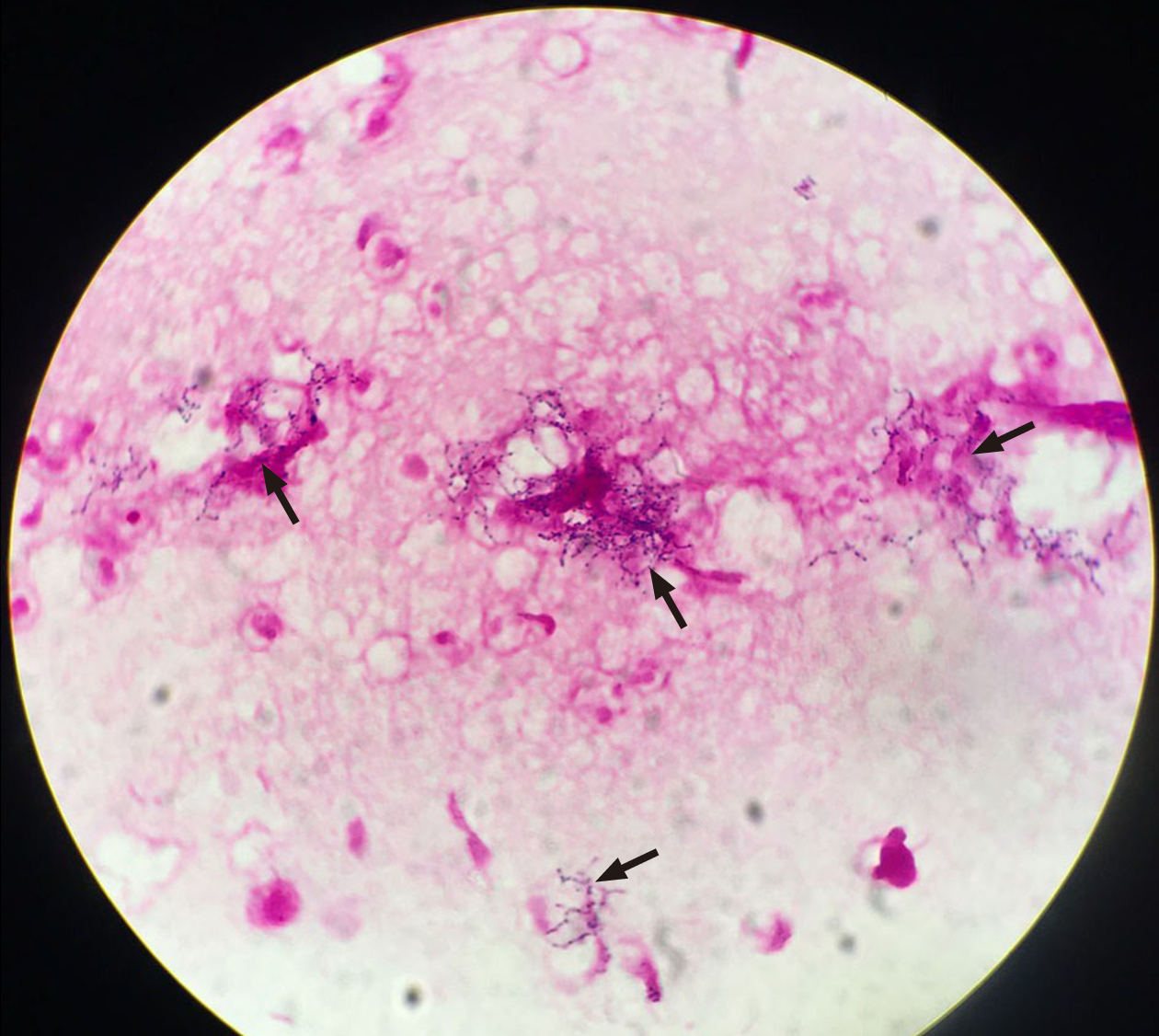
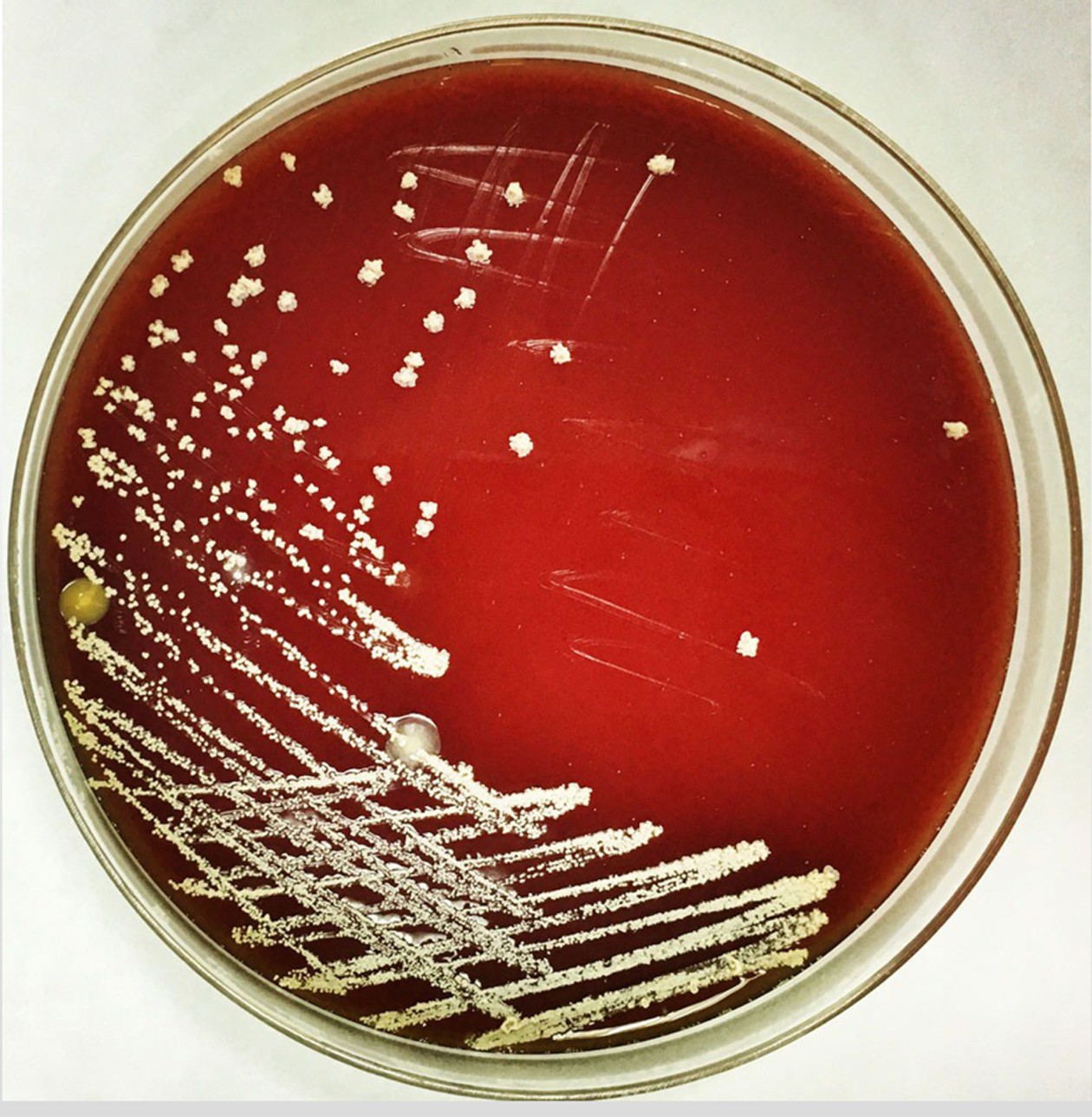
We also performed bronchoscopic alveolar lavage in the posterior basal segment of the left lower lobe. Gram-positive bacilli were detected in the bronchoalveolar lavage fluid (BALF) (Figure 2). The modified acid-fast staining of BALF was weakly positive, and the possible presence of Nocardia species was considered. Following culture of BALF, N. cyriacigeorgica was identified (Figure 3), which was confirmed by matrix-assisted laser desorption ionization-time of flight mass spectrometry (matrix-assisted laser desorption/ ionization-time of flight; VITEK MS, bioMérieux, Craponne, France) (Supplementary Figure 1).
The patient was diagnosed with pulmonary sequestration in the lower lobe of the left lung complicated by N. cyriacigeorgica infection.
She was started on treatment with trimethoprim-sulfamethoxazole (TMP-SMX) (4.32 g/d) and amikacin (0.4 g/d).
Her symptoms gradually improved, and she was discharged on September 25, 2020.
Nocardia is an aerobic, gram-positive, and modified acid-fast stain-positive bacillus that belongs in Actinomycetes. It is widely found in natural environments and frequently causes opportunistic infections in patients with impaired immunity, but one-third of infections can also be seen in patients with normal immunity[1]. N. cyriacigeorgica, an uncommon type of Nocardia, was first described in 2001, and was subsequently reported in Europe, Asia, and North America[9]. Microscopic examination revealed typical bacilli, and positive modified acid-fast staining was helpful for the diagnosis. The identification of Nocardia species by mass spectrometry after bacterial culture is the “gold standard” for determining different subtypes of Nocardia[8,10]. Sputum is the most commonly used respiratory tract specimen for Nocardia isolation[2,3,8,10], and BALF or fine needle aspiration biopsy is sometimes used as an invasive method to obtain specimens[3]. BALF has the advantages of simple operation and collection, the specimens are relatively less contaminated, and the results are relatively reliable. Percutaneous lung puncture biopsy is generally not the first choice for the risk of pneumothorax or bleeding. In our case, Nocardia was initially suspected when gram-positive bacilli were found in BALF smears. The pathogen was identified as N. cyriacigeorgica after bacterial culture and mass spectrometry analysis. Thus, the clinical evidence was conclusive.
Nocardia infection usually occurs due to exogenous inhalation or direct invasion through injured skin; therefore, the lungs and skin are the most common organs involved. Disseminated nocardiosis is frequently seen in immunocompromised patients[1,11], and mortality is high when the brain is involved[5]. In patients without cellular immune deficiency, the use of systemic glucocorticoids in chronic obstructive pulmonary disease is considered to cause pulmonary nocardiosis[1]. In addition to chronic obstructive pulmonary disease, there are reports in the literature that patients with structural lung diseases such as bronchiectasis, allergic bronchopulmonary aspergillosis, and nontuberculous mycobacterial pulmonary disease can also be complicated with N. cyriacigeorgica infection[2,8,12]. Pulmonary sequestration is a rare congenital pulmonary malformation where part of the lung tissue is directly supplied by the systemic circulation, which forms a cystic mass[13]. This part of the lung tissue is prone to recurrent localized infections[14]. Therefore, pulmonary sequestration is also a “special” structural lung disease. Kilpatrick et al[15] reported the first case of pulmonary sequestration complicated with Nocardia infection in 1976, but it was impossible to distinguish N. brasiliensis from N. asteroides due to technical limitations at that time. Shibli et al[16] and colleagues reported another case with N. asteroides infection and pulmonary sequestration in 2002. Foucrier et al[17] reported the imaging findings of another case of pulmonary sequestration with Nocardia infection (the article did not mention the type of Nocardia species). This is the first report of pulmonary sequestration complicated with N. cyriacigeorgica infection in a young immu-nocompetent woman.
Nocardiosis involves chronic suppurative inflammation, and TMP-SMX is the first choice for treatment. Critically ill patients often require combination therapy. The drugs that can be combined include aminoglycosides, carbapenems, quinolones, etc., and the course of treatment usually lasts more than 6 mo. Patients with central nervous system involvement may need a longer course of treatment[1]. The clinical symptoms in our patient were relatively mild and improved after treatment with TMP-SMX combined with amikacin. Pulmonary sequestration itself was considered to have surgical indications after thoracic surgery consultation. However, the patient was recommended to choose the timing of surgery after adequate anti-infective treatment due to the presence of N. cyriacigeorgica infection.
In summary, we report a case of pulmonary sequestration complicated by with N. cyriacigeorgica infection in an immunocompetent female patient. The pathogen was confirmed by BALF examination. In addition to common bacteria, rare pathogens such as Nocardia should be considered in patients with pulmonary sequestration.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Parra-Medina R S-Editor: Zhang L L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Wilson JW. Nocardiosis: updates and clinical overview. Mayo Clin Proc. 2012;87:403-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 483] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 2. | Yagi K, Ishii M, Namkoong H, Asami T, Fujiwara H, Nishimura T, Saito F, Kimizuka Y, Asakura T, Suzuki S, Kamo T, Tasaka S, Gonoi T, Kamei K, Betsuyaku T, Hasegawa N. Pulmonary nocardiosis caused by Nocardia cyriacigeorgica in patients with Mycobacterium avium complex lung disease: two case reports. BMC Infect Dis. 2014;14:684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Chen J, Zhou H, Xu P, Zhang P, Ma S, Zhou J. Clinical and radiographic characteristics of pulmonary nocardiosis: clues to earlier diagnosis. PLoS One. 2014;9:e90724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Schlaberg R, Huard RC, Della-Latta P. Nocardia cyriacigeorgica, an emerging pathogen in the United States. J Clin Microbiol. 2008;46:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Benek HB, Akcay E, Yilmaz H, Yis R, Yurt A. Nocardia cyriacigeorgica brain abscess with Pemphigus vulgaris: first report. Br J Neurosurg. 2020: 1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Freiberg JA, Saharia KK, Morales MK. An unusual case of Nocardia cyriacigeorgica presenting with spinal abscesses in a renal transplant recipient and a review of the literature. Transpl Infect Dis. 2019;21:e13025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Akcaglar S, Yilmaz E, Heper Y, Alver O, Akalin H, Ener B, Tore O, Ersoy C, Imamoglu S. Nocardia cyriacigeorgica: pulmonary infection in a patient with Basedow-Graves disease and a short review of reported cases. Int J Infect Dis. 2008;12:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Wu J, Wu Y, Zhu Z. Pulmonary infection caused by Nocardia cyriacigeorgica in a patient with allergic bronchopulmonary aspergillosis: A case report. Medicine (Baltimore). 2018;97:e13023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Yassin AF, Rainey FA, Steiner U. Nocardia cyriacigeorgici sp. nov.. Int J Syst Evol Microbiol. 2001;51:1419-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Liu C, Feng M, Zhu J, Tao Y, Kang M, Chen L. Severe pneumonia due to Nocardia otitidiscaviarum identified by mass spectroscopy in a cotton farmer: A case report and literature review. Medicine (Baltimore). 2017;96:e6526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Martínez R, Reyes S, Menéndez R. Pulmonary nocardiosis: risk factors, clinical features, diagnosis and prognosis. Curr Opin Pulm Med. 2008;14:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Ercibengoa M, Càmara J, Tubau F, García-Somoza D, Galar A, Martín-Rabadán P, Marin M, Mateu L, García-Olivé I, Prat C, Cilloniz C, Torres A, Pedro-Botet ML, Ardanuy C, Muñoz P, Marimón JM. A multicentre analysis of Nocardia pneumonia in Spain: 2010-2016. Int J Infect Dis. 2020;90:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Chaves JJ, Nieto FP, Gómez-Gómez M, Rodríguez DF, García-Concha D, Parra-Medina R. Pulmonary Sequestration Associated with Actinomycosis: A Case Report. Antibiotics (Basel). 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Elia S, Alifano M, Gentile M, Somma P, D'Armiento FP, Ferrante G. Infection with Mycobacterium tuberculosis complicating a pulmonary sequestration. Ann Thorac Surg. 1998;66:566-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Kilpatrick GR Jr, Koontz CH, Nelson RA. Nocardia infection in a bronchopulmonary sequestration. Chest. 1976;69:786-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Shibli M, Connery C, Shapiro JM. Intralobar and extralobar bronchopulmonary sequestration complicated by Nocardia asteroides infection. South Med J. 2003;96:78-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Foucrier A, Woerther PL, Le Dorze M, Ruimy R, Laissy JP, Castier Y, Mourvillier B. Pulmonary sequestration syndrome diagnosed from a Nocardia infection. Am J Respir Crit Care Med. 2012;186:288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |