Published online May 6, 2020. doi: 10.12998/wjcc.v8.i9.1592
Peer-review started: December 16, 2019
First decision: February 20, 2020
Revised: March 4, 2020
Accepted: April 15, 2020
Article in press: April 15, 2020
Published online: May 6, 2020
Processing time: 135 Days and 22.3 Hours
Although long-term retention of a ventilation tube is required in many ear diseases, spontaneous removal of conventional ventilation tube is observed in patients within 3 to 12 mo. To address this issue, we aimed to determine a new method for long-term retention of the ventilation tube.
To explore the value of removing the biofilm for long-term retention of tympanostomy ventilation tubes.
A case-control study design was used to evaluate the safety and effectiveness of long-term tube retention by directly removing the biofilm (via surgical exfoliation) in patients who underwent myringotomy with ventilation tube placement. The patients were randomly divided into two groups: Control group and treatment group. Patients in the treatment group underwent regular biofilm exfoliation surgery in the clinic, whereas those in the control group did not have their biofilm removed. Only conventional ventilation tubes were placed in this study. Outcome measures were tube position and patency. Tube retention time and any complications were documented.
Eight patients with biofilm removal and eight patients without biofilm removal as a control group were enrolled in the study. The tympanostomy tube retention time was significantly longer in the treatment group (43.5 ± 26.4 mo) than in the control group (9.5 ± 6.9 mo) (P = 0.003). More tympanostomy tubes were found to be patent and in correct position in the treatment group during the follow-up intervals than in the control group (P = 0.01).
Despite the use of short-term ventilation tubes, direct biofilm removal can be a well-tolerated and effective treatment for long-term tube retention of tympanostomy ventilation tubes in patients who underwent myringotomy.
Core tip: Long-term ventilation tube retention is necessary in many diseases, such as refractory otitis media with effusion and eustachian tube dysfunction, as well as with the use of Meniett therapy for Ménière disease. However, conventional ventilation tubes are expelled spontaneously within 3 to 12 mo because of tube extrusion or obstruction. Therefore, patients have to undergo two or more myringotomy with ventilation tube placement procedures, along with the risks of anesthesia and surgery, excessive injury to the tympanic membrane and external auditory canal, medical care costs, and impact on school or work. The biofilm plays a crucial role in the development of extrusion or obstruction after myringotomy with ventilation tube placement. It was revealed that, despite the use of short-term tube, biofilm removal has been proven to be a safe and effective treatment for long-term tube retention.
- Citation: Ma Q, Wang H, Chen ZN, Wu YQ, Yu DZ, Wang PJ, Shi HB, Su KM. Removal of biofilm is essential for long-term ventilation tube retention. World J Clin Cases 2020; 8(9): 1592-1599
- URL: https://www.wjgnet.com/2307-8960/full/v8/i9/1592.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i9.1592
Myringotomy with ventilation tube placement (M&T) was first described by Viennese otologist Politzer in 1868 for the treatment of otitis media catarrhalis and was popularized by Armstrong in 1954[1]. Since then, the basic principles of myringotomy with tube placement have remained unchanged, although various surgical procedures have been developed. M&T plays an important role in the treatment of refractory otitis media with effusion (ROME) and eustachian tube dysfunction by maintaining continuous ventilation and pressure balance and promoting secretion drainage in the middle ear[2]. Ninety percent of children develop otitis media at least once before the age of 2 years; thus, M&T is the most common outpatient operation for children younger than 15 years[3].
In cases of ROME and eustachian tube dysfunction, as well as with the use of Meniett therapy for Ménière disease, the ventilation tube needs to be retained for a relatively long time. However, conventional ventilation tube is expelled spontaneously within 3 to 12 mo because of tube extrusion or obstruction[4], and in such cases, patients have to undergo two or more M&T procedures. Although M&T is a minimally invasive procedure, there is a need to minimize the number of operations for long-term maintenance of an indwelling tube, considering the risks of anesthesia and surgery, excessive injury to the tympanic membrane and external auditory canal, medical care costs, and impact on school or work[5].
Many “permanent” tubes have been developed in an attempt to provide longer-lasting middle ear ventilation, but such tubes are still subject to problems with unplanned extrusion[6]. In this study, we aimed to identify a safe and effective method for long-term retention with the conventional ventilation tube in patients requiring an indwelling tube.
Sixteen consecutive adult patients who underwent M&T and required an indwelling tube over a long period were recruited from the Sixth People’s Hospital (Affiliated to Shanghai Jiaotong University) between January 2011 and September 2019. The patients were randomly divided into two groups: Control group and treatment group. During the same period, patients in the treatment group underwent regular biofilm exfoliation surgery in the clinic, whereas those in the control group did not have their biofilm removed. General characteristics, such as age, sex, follow-up interval, and retention time, were collected (Table 1). All patients provided written informed consent in accordance with the Declaration of Helsinki[7]. The study protocol was reviewed and approved by the Ethics Committee of Shanghai Sixth People’s Hospital (YS-2018-101).
| No. | Sex/age (yr) | Diagnosis | Follow-up intervals (mo) | Retention time (mo) |
| 1 | F/72 | MD | 2 | 24 |
| 2 | M/37 | MD | 12 | 84 |
| 3 | F/42 | MD | 1 | 12 |
| 4 | M/55 | ROME | 6 | 24 |
| 5 | M/60 | ROME | 6 | 24 |
| 6 | F/39 | MD | 1.5 | 42 |
| 7 | M/25 | MD | 12 | 72 |
| 8 | M/51 | MD | 12 | 60 |
| 9 | F/55 | ROME | / | 24 |
| 10 | M/63 | ROME | / | 9 |
| 11 | M/79 | ROME | / | 5 |
| 12 | F/46 | ROME | / | 8 |
| 13 | M/64 | ROME | / | 12 |
| 14 | F/49 | ROME | / | 4 |
| 15 | F/75 | ROME | / | 2 |
| 16 | F/40 | ROME | / | 12 |
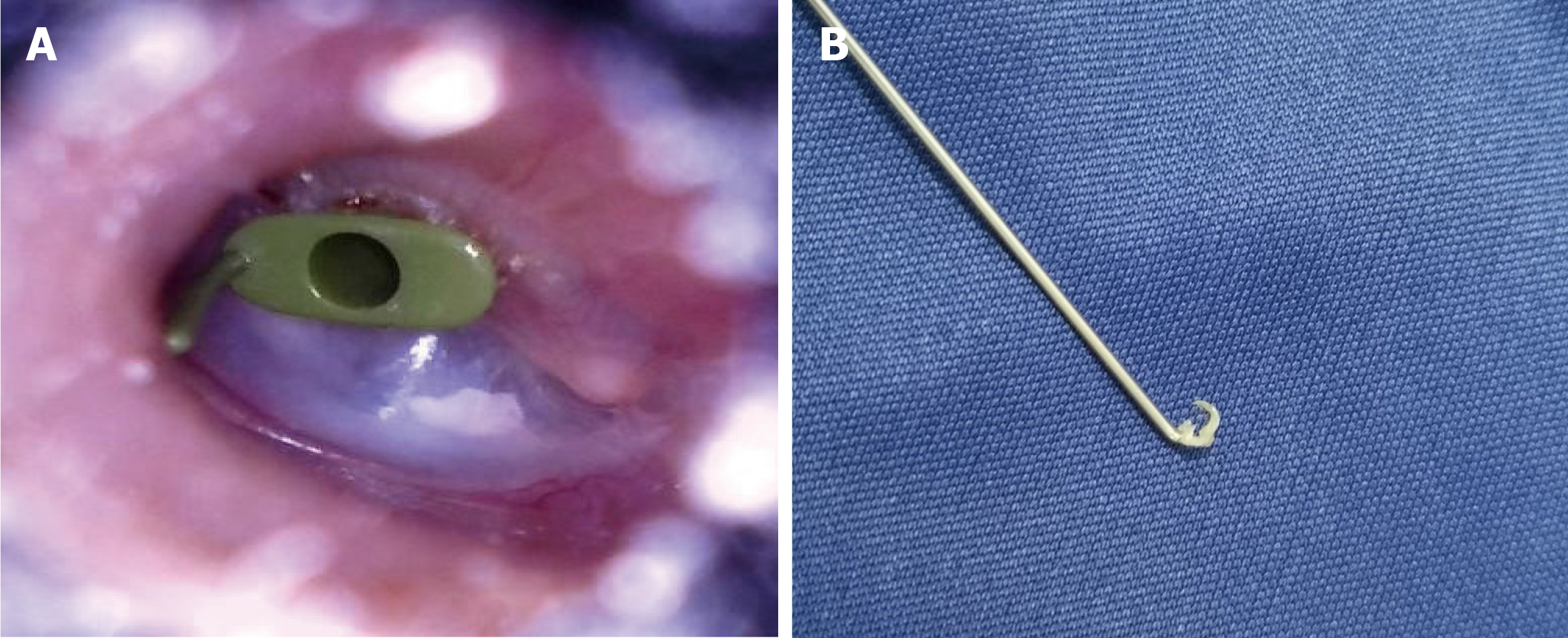
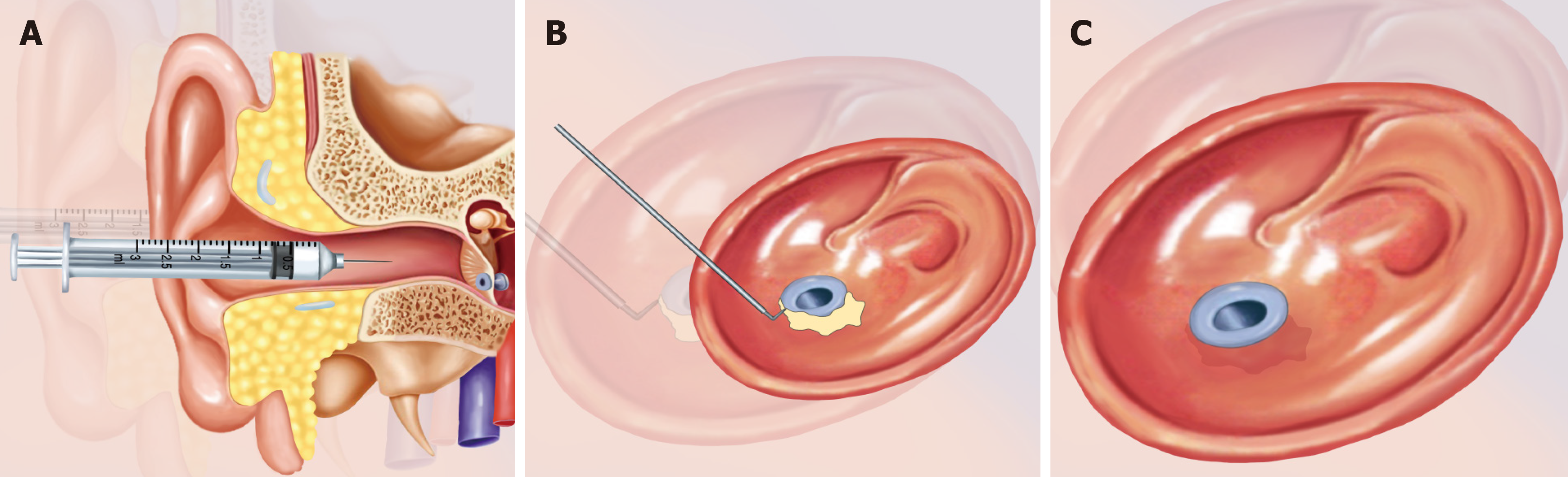
All patients underwent M&T. Only conventional ventilation tubes were used in this study (Medtronic, United States) and retained for more than 1 year depending on the needs of treatment. Follow-up intervals were 4 wk, 8 wk, 6 mo, and 1 year after M&T, which were mainly conducted to examine the state of the ventilation tube and the treatment effects for primary diseases. The follow-up period was determined according to the speed of accumulation of the exfoliated epithelium (biofilm), which was mostly located at the vertical junction of the circular edge of the indwelling tube (Figure 1). For regular biofilm exfoliation surgery, the biofilm of the ventilation tube was immersed in ofloxacin ear drops for 20-30 min. Then, under a microscope, the biofilm was cut off and cleared with an improvised miniature suction or hook. Finally, the migrated tube was reset (Figure 2). The control group did not undergo biofilm removal.
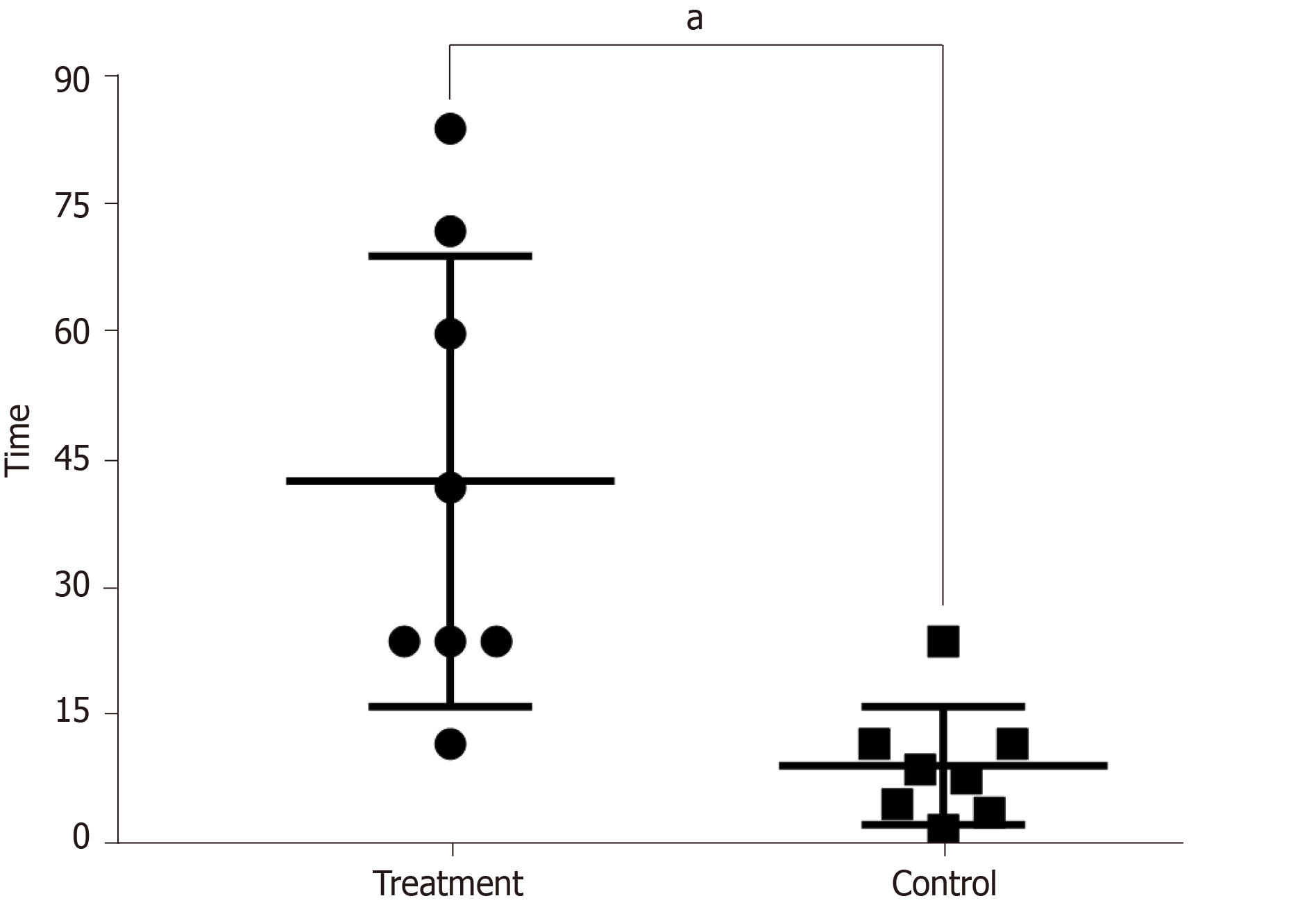
Tube position and patency were the outcome measures. Patency was defined as < 50% blockage in the ventilation tube; position was indicated by a distance < 0.3 cm between the ventilation tube and the tympanic membrane. Any complications, such as obstruction, granulomatosis, myringosclerosis, retraction, cholesteatoma, and tympanic membrane perforation, were documented. The tube retention time was calculated in the control and treatment groups (Figure 3).
SPSS for Windows version 22.0 (IBM, United States) was used for data analyses. Independent t-test was used to compare mean difference between the two values, and a Chi-square test (χ2) was used for the comparison of two or more rates. A P value < 0.05 was considered statistically significant.
A total of 16 participants (56.3% men and 43.7% women) with a mean age of 53.3 ± 15.0 years (Table 1) were enrolled in the study. The treatment and control groups included eight patients each. The reason for long-term ventilation tube retention included MD and ROME (Table 1).
Univariate analysis revealed that the retention time of the tympanostomy tube was significantly longer in the treatment group (43.5 ± 26.4 mo) than in the control group (9.5 ± 6.9 mo) (P = 0.003). No statistically significant difference in sex (P = 0.619) or age (P = 0.140) was found between the treatment and control groups (Table 2).
| Total (n = 16) | Treatment (n = 8) | Control (n = 8) | P value | |
| Sex | 0.619 | |||
| Male | 9 (56.25) | 5 (62.5) | 3 (37.5) | |
| Female | 7 (43.75) | 3 (37.5) | 5 (62.5) | |
| Age (yr) | 53.3 ± 15.0 | 47.6 ± 14.9 | 58.9 ± 13.9 | 0.140 |
More tympanostomy tubes were found to be in position and patent in the treatment group in the follow-up intervals compared with those in the control group (P = 0.01). During the course of tube retention, there was no complication in either group (Table 3).
| Total | Treatment | Control | P value | ||
| Position | 0.010 | ||||
| Yes | 8 | 7 | 7 | ||
| No | 8 | 1 | 1 | ||
| Patency | 0.010 | ||||
| Yes | 8 | 7 | 7 | ||
| No | 8 | 1 | 1 | ||
In this study, we identified a safe and effective method for long-term retention of conventional ventilation tube in patients requiring an indwelling tube. The treatment group had longer tympanostomy tube retention time than the control group.
Long-term ventilation tube retention is necessary in many diseases. Otitis media with effusion is more common in children with cleft palate or cleft lip and palate, with incidence rates of 70%-90%[8]. Although M&T is expected to alleviate tympanic effusion, the rate of reimplantation is 21.9%, owing to recurrent attacks or premature extrusion caused by middle ear inflammation[9]. Because of persistent eustachian tube dysfunction in persons with Down syndrome, middle ear aeration via tympanostomy tubes may be required throughout the preschool years to prevent otologic and developmental complications associated with otitis media with effusion. However, in 38.4% of the patients, the tube needs to be replaced because of repeated removal, and the average number of tube replacements per individual is 3.5[10]. Yaman et al[11] showed that the longer the tympanostomy tube retention time, the lower the recurrence rate of ROME. Comparison of three groups in their study showed higher recurrence rates with a retention time < 6 mo (36.54%) than with retention times between 6 and 12 mo (17.74%) and > 12 mo (9.1%).
Biofilm removal is essential for long-term ventilation tube retention in Meniett therapy. The Meniett device is a safe, nondestructive treatment for patients refractory to medical therapy for Meniere disease[12]. It does not function in the presence of an intact tympanic membrane, requiring the maintenance of a patent myringotomy tube. In Mattox’s study, in eight patients using the device between 3 and 5.25 years, there were 29 separate conventional tube insertions or 3.6 tube insertions per patient[13]. With the same therapy, our six patients with Meniere disease had six separate conventional tube insertions or one tube insertion per patient during an average of 4 years of treatment. Therefore, our new method for long-term ventilation tube retention appears to be a suitable alternative to repeated tympanostomy tube placement in selected patients.
The biofilm plays a crucial role in the development of complications after M&T. Otorrhea and obstruction are the two most common complications after tympanic membrane catheterization. In one study, the risk of otorrhea ranged from 0.5% to 11%, and the incidence of tube obstruction ranged from 6.9% to 36%[14]. There is growing evidence to support the role of biofilms in the development of complications after M&T. Previous reports have described strategies to inhibit the development of bacterial biofilms in tympanostomy tubes. Among these strategies are antibiotic-coated tympanostomy tubes, silver oxide–impregnated tympanostomy tubes[15], polyvinylpyrrolidone-coated silicone tympanostomy tubes[16], phosphorylcholine antibacterial coating, and ion-bombarded silicone and fluoroplastic tympanostomy tubes[17]. Each of these strategies has its own limitations. Antibiotic coatings are likely to cause an increase in antibiotic resistance; silver oxide–impregnated and phosphorylcholine antibacterial-coated tympanostomy tubes do not inhibit biofilm formation; and ion-bombarded tympanostomy tubes do not completely inhibit bacterial attachment[18]. Since the role of biofilm in the development of complications is clear, our treatment should also be effective in theory.
An obvious shortcoming of our study is its retrospective nature. Although this study investigated several factors that might affect tube retention time, not all potential variables were included. Considering the small sample size, further study is necessary to determine whether biofilm removal is a suitable alternative to repeated tympanostomy tube placement in selected patients. In conclusion, despite the use of short-term tube, biofilm removal has been proven to be a safe and effective treatment for long-term tube retention.
Myringotomy with ventilation tube placement (M&T) plays an important role in the treatment of refractory otitis media by maintaining continuous ventilation and pressure balance and promoting secretion drainage in the middle ear. Long-term ventilation tube retention is necessary in many diseases, such as refractory otitis media with effusion and eustachian tube dysfunction, as well as with the use of Meniett therapy for Ménière disease. However, conventional ventilation tubes are expelled spontaneously within 3 to 12 mo because of tube extrusion or obstruction. Therefore, patients have to undergo two or more M&T procedures, which have the concomitant risks of anesthesia and surgery, excessive injury to the tympanic membrane and external auditory canal, medical care costs, and impact on school or work.
The biofilm plays a crucial role in the development of extrusion or obstruction after M&T. Previous reports described strategies designed to inhibit the development of bacterial biofilms on tympanostomy tubes, such as antibiotic-coated, ion-bombarded silicone, and fluoroplastic tympanostomy tubes, which had been proved to be incapable of completely inhibiting bacterial attachment. However, studies about biofilms are still lacking, and it is uncertain whether directly removing the biofilm can be a well-tolerated and effective treatment for long-term tube retention of tympanostomy ventilation tubes.
In this study, directly removing the biofilm was performed to maintain tube position and patency as well as control complications. Our study aimed to explore the value of directly removing the biofilm for long-term ventilation tube retention.
A case-control study design was used to evaluate the safety and effectiveness of long-term tube retention by directly removing the biofilm (via surgical exfoliation) in patients who underwent M&T. Patients in the treatment group underwent regular biofilm exfoliation surgery in the clinic, whereas the control group did not undergo biofilm removal. Only conventional ventilation tubes were placed in this study. Outcome measures were tube position and patency. Tube retention time and any complications were documented.
In this study, we identified a safe and effective method for long-term retention of conventional ventilation tube in patients requiring an indwelling tube. Tympanostomy tube retention time was longer in the treatment group than in the control group. More tympanostomy tubes were found to be in position and patent in the treatment group in the follow-up intervals than in the control group. Furthermore, during the course of tube retention, there was no complication in either group.
Biofilm removal has been proven to be a safe and effective treatment for long-term tube retention, even with the use of short-term tube. It is expected to provide a new treatment method for many diseases that necessitate long-term ventilation tube retention.
Considering the small sample size, further study is needed to determine whether biofilm removal is a suitable alternative to repeated tympanostomy tube placement in selected patients.
Manuscript source: Invited Manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chhabra N, Ozcan C S-Editor: Wang J L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Paradise JL, Bluestone CD. Consultation with the specialist: tympanostomy tubes: a contemporary guide to judicious use. Pediatr Rev. 2005;26:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Smith N, Greinwald J. To tube or not to tube: indications for myringotomy with tube placement. Curr Opin Otolaryngol Head Neck Surg. 2011;19:363-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Schraff SA. Contemporary indications for ventilation tube placement. Curr Opin Otolaryngol Head Neck Surg. 2008;16:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Principi N, Marchisio P, Esposito S. Otitis media with effusion: benefits and harms of strategies in use for treatment and prevention. Expert Rev Anti Infect Ther. 2016;14:415-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Huyett P, Sturm JJ, Shaffer AD, Kitsko DJ, Chi DH. Second tympanostomy tube placement in children with recurrent acute otitis media. Laryngoscope. 2018;128:1476-1479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Poe DS, Metson RB, Kujawski O. Laser eustachian tuboplasty: a preliminary report. Laryngoscope. 2003;113:583-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-2194. [PubMed] [DOI] [Full Text] |
| 8. | Flynn T, Möller C, Jönsson R, Lohmander A. The high prevalence of otitis media with effusion in children with cleft lip and palate as compared to children without clefts. Int J Pediatr Otorhinolaryngol. 2009;73:1441-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 153] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Huang CY, Wu CS, Tang CH, Wang MC, Kuo TY, Tu TY. Palatoplasty decreases the re-insertion rate of middle ear ventilation tube in cleft palate children-A population-based birth cohort study. Acta Otolaryngol. 2016;136:768-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Bernardi GF, Pires CTF, Oliveira NP, Nisihara R. Prevalence of pressure equalization tube placement and hearing loss in children with down syndrome. Int J Pediatr Otorhinolaryngol. 2017;98:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Yaman H, Yilmaz S, Guclu E, Subasi B, Alkan N, Ozturk O. Otitis media with effusion: recurrence after tympanostomy tube extrusion. Int J Pediatr Otorhinolaryngol. 2010;74:271-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Ahsan SF, Standring R, Wang Y. Systematic review and meta-analysis of Meniett therapy for Meniere's disease. Laryngoscope. 2015;125:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Mattox DE, Reichert M. Meniett device for Ménière's disease: use and compliance at 3 to 5 years. Otol Neurotol. 2008;29:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Wang JC, Hamood AN, Saadeh C, Cunningham MJ, Yim MT, Cordero J. Strategies to prevent biofilm-based tympanostomy tube infections. Int J Pediatr Otorhinolaryngol. 2014;78:1433-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Vlastarakos PV, Nikolopoulos TP, Maragoudakis P, Tzagaroulakis A, Ferekidis E. Biofilms in ear, nose, and throat infections: how important are they? Laryngoscope. 2007;117:668-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Antonelli PJ, Sampson EM, Ojano-Dirain C. Biofilm formation on silicone tympanostomy tubes with polyvinylpyrrolidone coating. Arch Otolaryngol Head Neck Surg. 2011;137:19-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Licameli G, Johnston P, Luz J, Daley J, Kenna M. Phosphorylcholine-coated antibiotic tympanostomy tubes: are post-tube placement complications reduced? Int J Pediatr Otorhinolaryngol. 2008;72:1323-1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Wang JC, Tran PL, Hanes R, Cordero J, Marchbanks J, Reid TW, Colmer-Hamood JA, Hamood AN. Inhibition of otopathogenic biofilms by organoselenium-coated tympanostomy tubes. JAMA Otolaryngol Head Neck Surg. 2013;139:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |