Published online Apr 26, 2020. doi: 10.12998/wjcc.v8.i8.1554
Peer-review started: March 5, 2020
First decision: April 1, 2020
Revised: April 8, 2020
Accepted: April 11, 2020
Article in press: April 11, 2020
Published online: April 26, 2020
Processing time: 50 Days and 1.7 Hours
Coronavirus disease 2019 (COVID-19) is a major public health emergency with obvious characteristics of human-to-human transmission, and there are infective asymptomatic carriers. Early identification and proper management of patients with COVID-19 are important. Features in chest computed tomography (CT) can facilitate identifying newly infected individuals. However, CT findings of some lung contusions are similar to those of COVID-19, as shown in the present case.
A 46-year-old woman was admitted to hospital for backache and foot pain caused by a fall injury 1 d before hospitalization. She was suspected of having COVID-19, since there was a confirmed COVID-19 case near her residence. But she had no fever, cough, chest tightness, difficult breathing, nausea, vomiting, or diarrhea, etc. On physical examination, the lower posterior chest of both sides showed dullness on percussion and moist rales at the end of inspiration on auscultation. The white blood cell count and lymphocyte count were 10.88 × 109/L and 1.04 × 109/L, respectively. CT performed on February 7, 2020 revealed that both lungs were scattered with patchy ground-glass opacity. The patient was diagnosed with pulmonary contusion with thoracic spinal fracture (T12), calcaneal fracture, and pelvic fracture. On day 9 after conservative treatment, her condition was alleviated. On review of the chest CT, the previous shadows were significantly reduced.
Differential diagnosis of lung contusion and COVID-19 must be emphasized. Both conditions require effective prompt actions, especially COVID-19.
Core tip: A 46-year-old female trauma patient had pulmonary contusion that showed similar computed tomography findings to coronavirus disease 2019 (COVID-19) 1 d after injury. Her epidemiological history highly suggested COVID-19. However, the patient was not tested for COVID-19, and the imaging features improved after conservative treatment. This report suggests that in view of the risk of COVID-19, all trauma patients should undergo epidemiological investigations and chest computed tomography examinations, and strict and standardized processing procedures are needed.
- Citation: Chen LR, Chen ZX, Liu YC, Peng L, Zhang Y, Xu Q, Lin Q, Tao YM, Wu H, Yin S, Hu YJ. Pulmonary contusion mimicking COVID-19: A case report. World J Clin Cases 2020; 8(8): 1554-1560
- URL: https://www.wjgnet.com/2307-8960/full/v8/i8/1554.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i8.1554
Since December 2019, a new type of coronavirus pneumonia that occurred in Wuhan, Hubei Province, China has spread rapidly in China, and it is likely to spread worldwide[1-3]. The World Health Organization defined the new coronavirus pneumonia as a public health emergency of international concern on January 30, 2020, and officially named the new disease coronavirus disease 2019 (COVID-19) on February 11, 2020.
COVID-19 is currently a major public health emergency with obvious characteristics of human-to-human transmission and probable clustering onset, and there are infective asymptomatic carriers[4,5]. It also can result in severe and even fatal respiratory diseases such as acute respiratory distress syndrome[6]. Due to its transmissibility and severity, there is possible sustained transmission of COVID-19 beyond China[7]. Early identification and proper management of patients with COVID-19 are important. Characteristics on chest computed tomography (CT), clinical features, and epidemiological history can facilitate identifying new cases of COVID-19[8-10].
Pulmonary contusion is the most common complication of blunt chest injury[11], and is defined as alveolar consolidation or ground-glass opacity (GGO)[12]. Some trauma patients with pulmonary contusion may show similar CT images to patients with COVID-19, which could confuse the clinical diagnosis and treatment, and even result in serious situations if precautions were not taken when COVID-19 was diagnosed.
In the present paper, we report a trauma patient with pulmonary contusion whose CT imaging showed similar features to those of COVID-19, and we provide suggestions on management for trauma patients during the COVID-19 epidemic.
A 46-year-old woman was admitted to hospital due to backache and foot pain for 1 d caused by a fall injury.
The patient accidentally fell from a height of 3 m due to mental abnormality. After the injury, she felt persistent pain in the lower back, pelvis, and calcaneus, accompanied by a sense of swelling, restricted movement of the lower back and feet, and no local skin rupture or bleeding. At that time, there was no fever, cough, chest tightness, or difficult breathing and no discomfort such as nausea, vomiting, or diarrhea. She presented to hospital after 1 d due to severe pain.
She had a history of mental disorder 1 year ago and took medication intermittently. She had no history of cardiovascular disease, hypertension, or diabetes. Since December 2019, there had been no history of residence in Wuhan or Hubei Province, and no contact with diagnosed or suspected COVID-19 patients, but there was a confirmed case near her residence.
The vital signs were stable on admission. The patient’s temperature was 36.6 °C. Bruises were seen in the back and calcaneus without skin rupture. The lower posterior chest of both sides showed dullness on percussion and moist rales at the end of inspiration on auscultation.
The laboratory findings showed slightly elevated white blood cell count (10.88 × 109/L) and lowered lymphocyte count (1.04 × 109/L) on February 8, 2020. All other values including coagulation, albumin, alanine aminotransferase, and aspartate aminotransferase were within normal limits. However, on review of blood test on February 9, 2020, the white blood cell count and lymphocyte count were 8.39 × 109/ L and 1.29 × 109/ L, respectively.
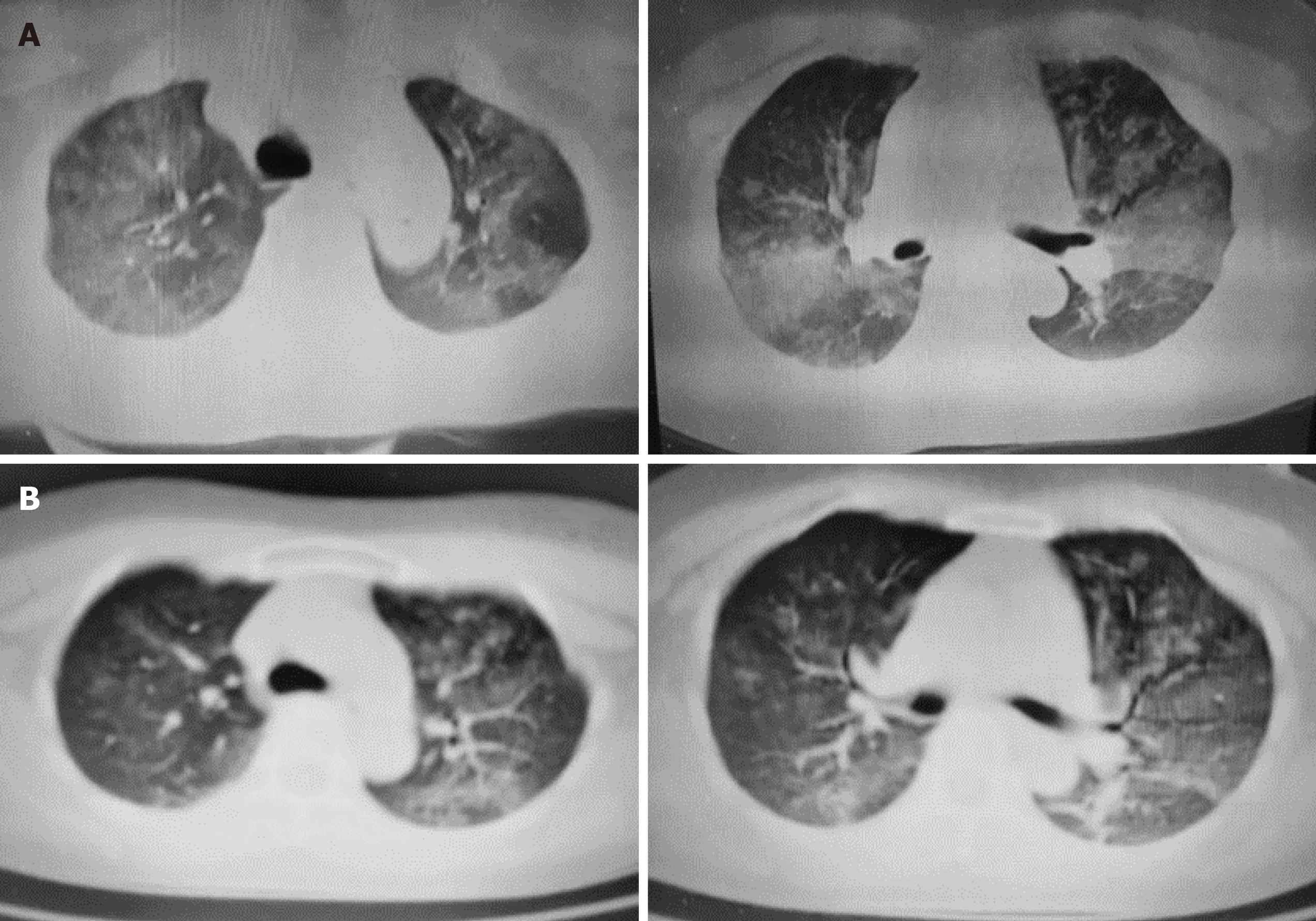
On February 7, 2020, X-ray examination confirmed compressed fracture of the 12th thoracic vertebra and fracture of the spinous process of the 11th thoracic vertebra and the calcaneus of both sides. Chest CT performed on February 7, 2020 revealed patchy GGOs scattered in both lungs (Figure 1A) and discontinuity of the cortex in the 12th thoracic vertebrae and pubic bone on both sides, and CT of the head and abdomen showed no obvious signs of trauma. Although COVID-19 was highly suspected, no nucleic acid test was performed, as the white blood cell count and lymphocyte count showed an alleviated condition.
The patient was diagnosed with a pulmonary contusion with thoracic spinal fracture (T12), calcaneal fracture, and pelvic fracture.
After hospitalization, the patient was treated as a case of general trauma. Isolation, prevention, and control measures for infection were not taken. On day 4 after injury, the patient’s condition worsened and she was transferred to the intensive care unit. After improvement with conservative treatment with antibiotics and expectorants, she was transferred to the respiratory department and discharged on day 9 after injury. Fractures were only treated conservatively.
She was discharged on day 9 after injury. A chest CT scan performed on February 15, 2020 showed that the lung contusion was alleviated, but it had not completely dissipated (Figure 1B).
COVID-19 is characterized by obvious human-to-human transmission, probable clustering onset, and infective asymptomatic carriers, and can result in severe and even fatal respiratory diseases such as acute respiratory distress syndrome[1,4,5,10,13]. Early identification and proper management of patients with COVID-19 are important.
The route of COVID-19 infection is mainly through the respiratory tract, namely, the nasopharyngeal cavity → trachea → bronchus → bronchioles → terminal bronchioles → respiratory bronchioles → alveoli. Throughout the process, the virus evades surveillance of the defense system including the tonsils and mucous membranes of various parts of the respiratory tract, goes straight to the lung lobules, and rapidly replicates to cause lung consolidation. Therefore, its pathophysiological changes usually start from the center of the lobule, which usually appears initially as small, frosted, glass-like shadows, or may diffuse to the surroundings, mainly under the pleura. In severe cases, the leaflets are fused into a large film, and even diffusely distributed.
Several studies have demonstrated that chest CT characteristics can facilitate identifying newly infected cases of COVID-19[9,14-17]. CT features of COVID-19 are diverse, including pure or mixed GGOs with a patchy to confluent or nodular shape, consolidations, and crazy-paving appearance, and they can be located in the central or peripheral areas of the posterior lungs, with peripheral lesions dominating their distribution. The hallmarks of COVID-19 infection on imaging are bilateral and peripheral GGO and consolidative pulmonary opacity, but almost 56% of early patients with COVID-19 had normal CT[14]. The features change throughout the disease course. As the disease progresses, GGOs may exist in the subpleural area of one or both lungs. Changes in CT may proceed rapidly with increased density of GGOs, and then progress into consolidations with perilobular thickening. Multifocal peripheral patchy areas of nodular consolidations and nodular GGO lesions can also be seen in subpleural areas in the lower lobes[17,18]. Chest CT plays a vital role in early detection, observation, and evaluation of COVID-19. Increasing numbers, extent, and density of GGOs on CT indicate disease progression[16].
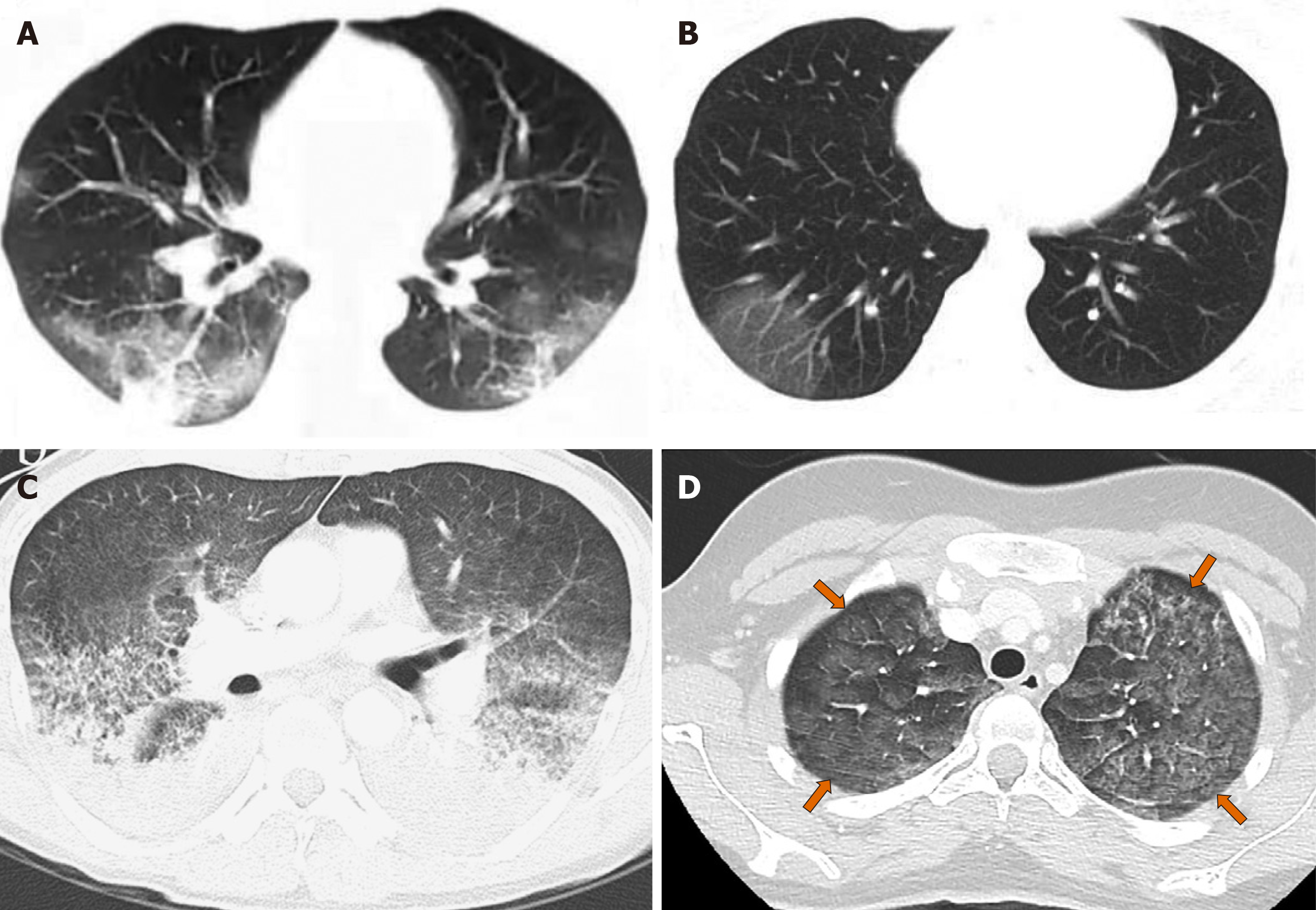
Pulmonary contusion is defined as alveolar consolidation or GGO[12], which is similar to CT images of COVID-19 pneumonia (Figure 2). It may develop in accidental injuries such as traffic accidents, falls, bumps, and crushes, and is characterized by parenchymal hemorrhage, interstitial edema, and alveolar collapse, which potentially lead to compromised respiratory function[19]. The pathological changes of pulmonary contusion are mainly damage to lung parenchymal cells, alveolar and capillary bleeding, pulmonary interstitial edema, atelectasis, and pulmonary consolidation. Pulmonary contusion generally begins with mild interstitial edema after injury; interstitial hemorrhage occurs after 1-2 h, and becomes apparent after 4 h, subsequently with exudation of monocytes and neutrophils. Protein, red blood cells, and many inflammatory cells appear in the alveoli, and the normal alveolar structure begins to disappear. Normally, pulmonary contusion starts to be absorbed within 7-10 d, and could return to normal without leaving any traces. Therefore, according to the amount of alveolar hemorrhage, chest CT of pulmonary contusions can appear as patchy or disseminated GGO because of a large volume of alveolar blood and/or consolidation as a result of a large volume of blood in the alveoli; the edges are blurred, and the dorsal subpleural distribution is dominant.
On imaging, lung contusion is different from COVID-19 in that the former has a significantly higher proportion of consolidation than the latter, and the former is often combined with bilateral pleural effusion and subpleural atelectasis.
In addition, over time, according to the characteristics of the above two diseases, follow-up chest CT has different trends. COVID-19 may show the following imaging changes. First, some cases can be improved. The extent or number of lesions reduces; the density of GGO increases and transforms into consolidation; and the edges of the consolidations become flat or contracted. The increase in the extent and density of some lesions may be caused by secondary alveolar pulmonary edema, increased exudation, increased mucus, combined bacterial infection, and the beginning of mechanization. Second, some cases show successive imaging changes, that is, some lesions improve and are absorbed, and new lesions appear. This may be caused by the delayed inflammatory response in some lung regions. Finally, some cases become exacerbated, showing an increase in the extent and number of lesions. There is a “white lung” change that pervades the entire lung, and the prognosis is poor.
However, the prognosis for lung contusion is different. Due to the pathophysiology of lung contusion, within 4-6 h after injury, the lungs may have no or only a few sheet shadows, which gradually increase over time, reaching a peak within 24-48 h, and those with exacerbations may have atelectasis. Our patient started to improve at 72 h after injury; the contusion was gradually absorbed after 7–10 d until it completely returned to normal.
For trauma patients with pulmonary contusion, epidemiological history and CT scan of the lungs are important in the current epidemic of COVID-19, so as to avoid misdiagnosis or missed diagnosis that may be combined with COVID-19 infection and avoid causing severe clustering infection.
As to the management of trauma patients with pulmonary contusion, epidemiological investigation is compulsory. In the case of COVID-19 infection, protective measures must be taken before the patient is ruled out as having COVID-19, as any suspected case of COVID-19 may become a “super spreader” with serious consequences. We believe that in the current epidemic of COVID-19, in the presence of strict mass prevention and control measures, special attention should be paid to trauma patients with pulmonary contusion. First, a detailed investigation of the patient’s epidemiological history is required. All trauma patients should be routinely asked about their epidemiological history; if there has been any travel to areas with high incidence of COVID-19; whether there is a history of contact with confirmed or suspected COVID-19 pneumonia patients; and history of contact with personnel in high-incidence areas. For medical history, a detailed investigation should be carried out on whether the patient has a history of fever, cough, shortness of breath, and contact with wild animals within 2 wk before injury. At the same time, all patients with trauma should undergo routine chest CT. If COVID-19 is suspected, nucleic acid testing should be routinely performed at least twice if possible. Even if the test is negative, if the imaging and medical history are highly suspect, the test should be repeated multiple times and relevant experts should be consulted.
Due to its transmissibility and severity, sustained global transmission of COVID-19 is possible. During the epidemic of COVID-19, the differential diagnosis of lung contusion and COVID-19 must be emphasized in trauma patients. Both conditions require effective prompt actions, especially COVID-19. Strict and standardized processing procedures are suggested for COVID-19.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bueno V, Drozdov E S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Phelan AL, Katz R, Gostin LO. The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. JAMA. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 744] [Article Influence: 148.8] [Reference Citation Analysis (6)] |
| 2. | World Health Organization. Novel coronavirus (2019-nCoV) situation report-39. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200228-sitrep-39-covid-19.pdf?sfvrsn=aa1b80a7_2. |
| 3. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9317] [Article Influence: 1863.4] [Reference Citation Analysis (0)] |
| 4. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11505] [Article Influence: 2301.0] [Reference Citation Analysis (0)] |
| 5. | Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, Zhang YL, Yan JB. Potential Presymptomatic Transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 327] [Cited by in RCA: 321] [Article Influence: 64.2] [Reference Citation Analysis (0)] |
| 6. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12973] [Article Influence: 2594.6] [Reference Citation Analysis (1)] |
| 7. | Swerdlow DL, Finelli L. Preparation for Possible Sustained Transmission of 2019 Novel Coronavirus: Lessons From Previous Epidemics. JAMA. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 8. | Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;200490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1106] [Cited by in RCA: 952] [Article Influence: 190.4] [Reference Citation Analysis (1)] |
| 9. | Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295:202-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1827] [Cited by in RCA: 1696] [Article Influence: 339.2] [Reference Citation Analysis (0)] |
| 10. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30112] [Article Influence: 6022.4] [Reference Citation Analysis (3)] |
| 11. | Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, Fabian TC. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51:223-228; discussion 229-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 189] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Cho SH, Kim EY, Choi SJ, Kim YK, Sung YM, Choi HY, Cho J, Yang HJ. Multidetector CT and radiographic findings of lung injuries secondary to cardiopulmonary resuscitation. Injury. 2013;44:1204-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model. 2020;5:248-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 334] [Cited by in RCA: 386] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 14. | Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020;200463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1728] [Cited by in RCA: 1597] [Article Influence: 319.4] [Reference Citation Analysis (1)] |
| 15. | Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020;200343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1213] [Cited by in RCA: 1211] [Article Influence: 242.2] [Reference Citation Analysis (1)] |
| 16. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes On Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology. 2020;200370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1617] [Cited by in RCA: 1761] [Article Influence: 352.2] [Reference Citation Analysis (0)] |
| 17. | Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, Park CM, Kim YH. Chest Radiographic and CT Findings of the 2019 Novel Coronavirus Disease (COVID-19): Analysis of Nine Patients Treated in Korea. Korean J Radiol. 2020;21:494-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 431] [Cited by in RCA: 374] [Article Influence: 74.8] [Reference Citation Analysis (0)] |
| 18. | Wei J, Xu H, Xiong J, Shen Q, Fan B, Ye C, Dong W, Hu F. 2019 Novel Coronavirus (COVID-19) Pneumonia: Serial Computer Tomography Findings. Korean J Radiol. 2020;21:501-504. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 19. | Cohn SM. Pulmonary contusion: review of the clinical entity. J Trauma. 1997;42:973-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 185] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Belabbas D, Auger M, Lederlin M, Bonenfant J, Gandon Y, Aubé C, Paisant A. Whole-Body CT after Motor Vehicle Crash: No Benefit after High-Energy Impact and with Normal Physical Examination. Radiology. 2019;292:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |