Published online Apr 26, 2020. doi: 10.12998/wjcc.v8.i8.1532
Peer-review started: January 19, 2020
First decision: February 26, 2020
Revised: March 9, 2020
Accepted: April 10, 2020
Article in press: April 10, 2020
Published online: April 26, 2020
Processing time: 95 Days and 21.7 Hours
Abdominal wall endometriosis can occur secondary to gynecological and obstetric pelvic laparotomy; however, this is a rare clinical event. There are few cases of endometriosis involving the incision site of a laparoscopic surgery, especially for those of the endometrial nodule at the umbilical trocar port site where the camera is placed.
We describe the case of a 37-year-old woman who presented with a 2-year history of a tough swelling below the umbilicus, which presented periodical pain during menstruation. The patient had undergone laparoscopic ovarian cystectomy 4 years prior, and we theorized that the umbilical nodule was a complication of that laparoscopic surgery. Histological analysis confirmed the diagnosis of abdominal umbilical scar endometriosis secondary to previous laparoscopic surgery. Surgical removal of the nodule followed by three cycles of leuprorelin was curative.
Abdominal mass and pain in women of childbearing age with a previous history of pelvic surgery should support consideration of endometriosis at the surgical site.
Core tip: Incisional endometriosis after laparoscopy is very rare, and if occurring, it is often seen in the cannula incision of that collected specimen. In our patient, incisional endometriosis occurred in the umbilical cannula incision, which was not the cannula incision from which the specimen was taken out of. We also review the published literature and summarize the characteristics, differential diagnosis, and treatment of umbilical endometriosis.
- Citation: Ao X, Xiong W, Tan SQ. Laparoscopic umbilical trocar port site endometriosis: A case report. World J Clin Cases 2020; 8(8): 1532-1537
- URL: https://www.wjgnet.com/2307-8960/full/v8/i8/1532.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i8.1532
Endometriosis occurs mostly in pelvic organs and is rarely detected in extrapelvic locations, such as the abdominal wall, central nervous system, lungs, kidneys, ureters, limbs, gallbladder, nasal cavity, brain, and distant skin[1,2]. Abdominal wall endometriosis (AWE) is the most common site of extrapelvic endometriosis. AWE can be spontaneous, but it can also occur after gynecological and obstetric pelvic surgery, with approximately 57% of cases developing secondary to cesarean section[3]. In addition, AWE can also be detected in the abdominal wall incision after ovarian cyst removal, appendectomy, and tubal ligation, being clinically defined as scar endometriosis or incision endometriosis.
Herein, we report a case of AWE detected in the umbilicus, which served as the trocar port site where the laparoscope body and camera were placed during previous laparoscopic surgery.
A 37-year-old woman found a slow-growing nodule under the skin of the surgical scar on the umbilicus which caused periodic pain and presented to the Dermatology Department of West China Hospital, Sichuan University (Chengdu, China) on March 29, 2019 for treatment. Histological analysis of a fine needle aspiration biopsy of the nodule suggested endometriosis.
Umbilical nodules appeared at the incision site of the original laparoscopic cannula at the lower edge of the umbilicus about 4 years prior, which had gradually increased from 0.5 cm to approximately 1.5 cm in diameter and were accompanied by pain during menstruation.
The patient had undergone laparoscopic ovarian cyst removal and bilateral salpingoplasty at the Department of Reproductive Endocrinology of our hospital 6 years prior. After cyst removal, pathological examination had led to the diagnosis of endometrial cyst.
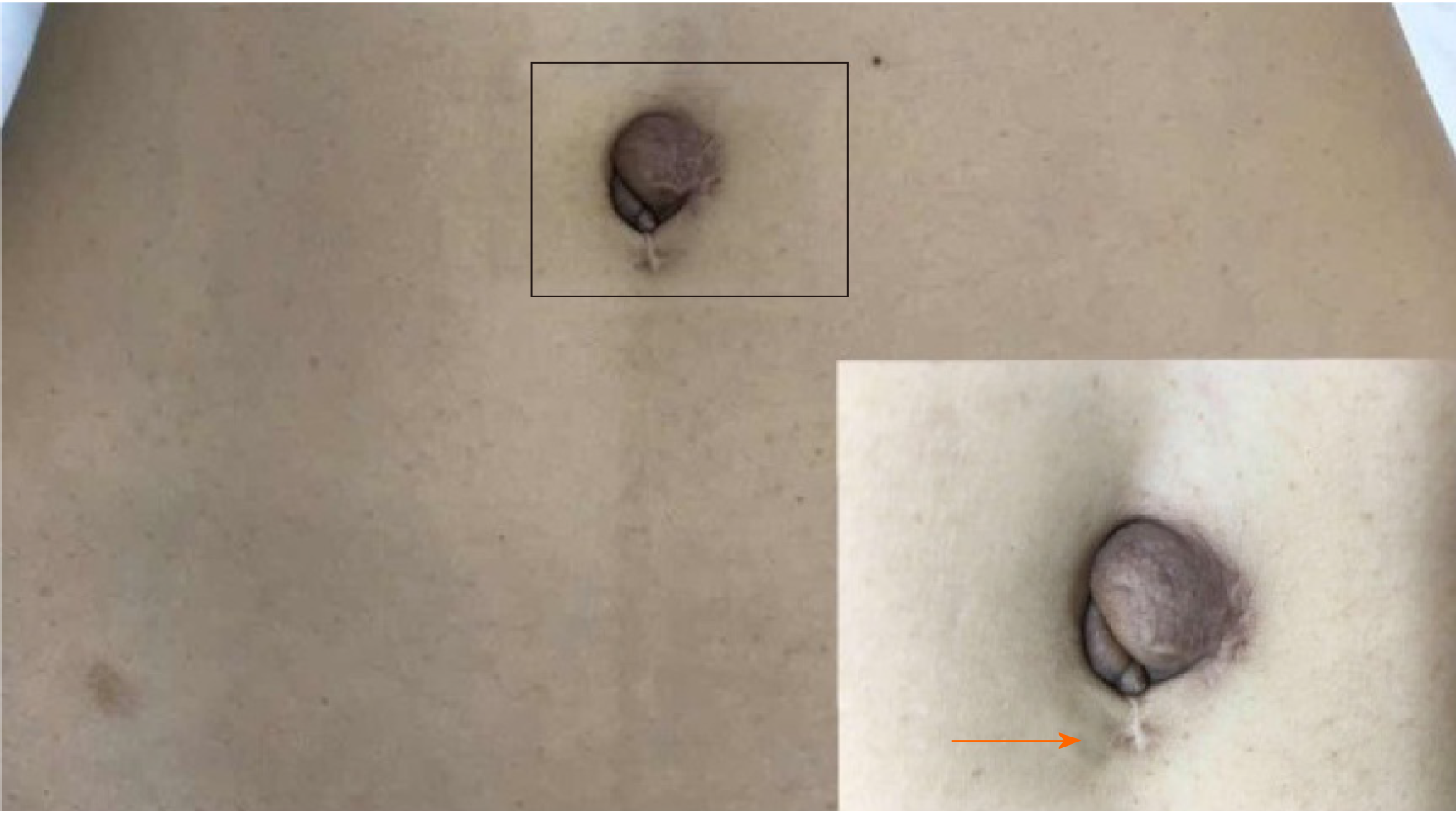
The patient’s vital signs were normal. Abdominal examination revealed no tenderness or rebound tenderness. At the incision of the original laparoscopic cannula at the lower edge of the umbilicus, three brown hard nodules of different sizes were detected, with the maximum diameter of about 1.5 cm. No redness or ulceration was found on the surface of the nodules (Figure 1). The boundary between the nodules and surrounding tissues was clear.
Fine needle biopsy of the umbilical nodule confirmed the diagnosis of umbilical endometriosis. Positive expression of the immunohistochemical markers’ estrogen receptor, progesterone receptor, and p63 was found in the infiltrated glands of the dermis; in addition, progesterone receptor and cluster of differentiation 10 were expressed in the periglandular interstitial space. Ki67 was about 10% positive in the gland and interstitium. Serum level of tumor marker carbohydrate antigen 19-9 was 39.1 U/mL and that of carbohydrate antigen 12-5 was 19.7 U/mL.
No superficial ultrasound examination of the abdominal wall was performed because the nodules could be seen clearly by the naked eye. Transvaginal Doppler showed that the endometrial echo was uneven, with a slightly strong echo (endometrial polyp could not be excluded). A cyst about 1.5 to 2.9 cm in diameter was present on both ovaries (chocolate cyst of the ovary is likely).
Abdominal umbilical scar endometriosis secondary to previous laparoscopic surgery.
The nodule was surgically removed, and leuprorelin was administered for three cycles.
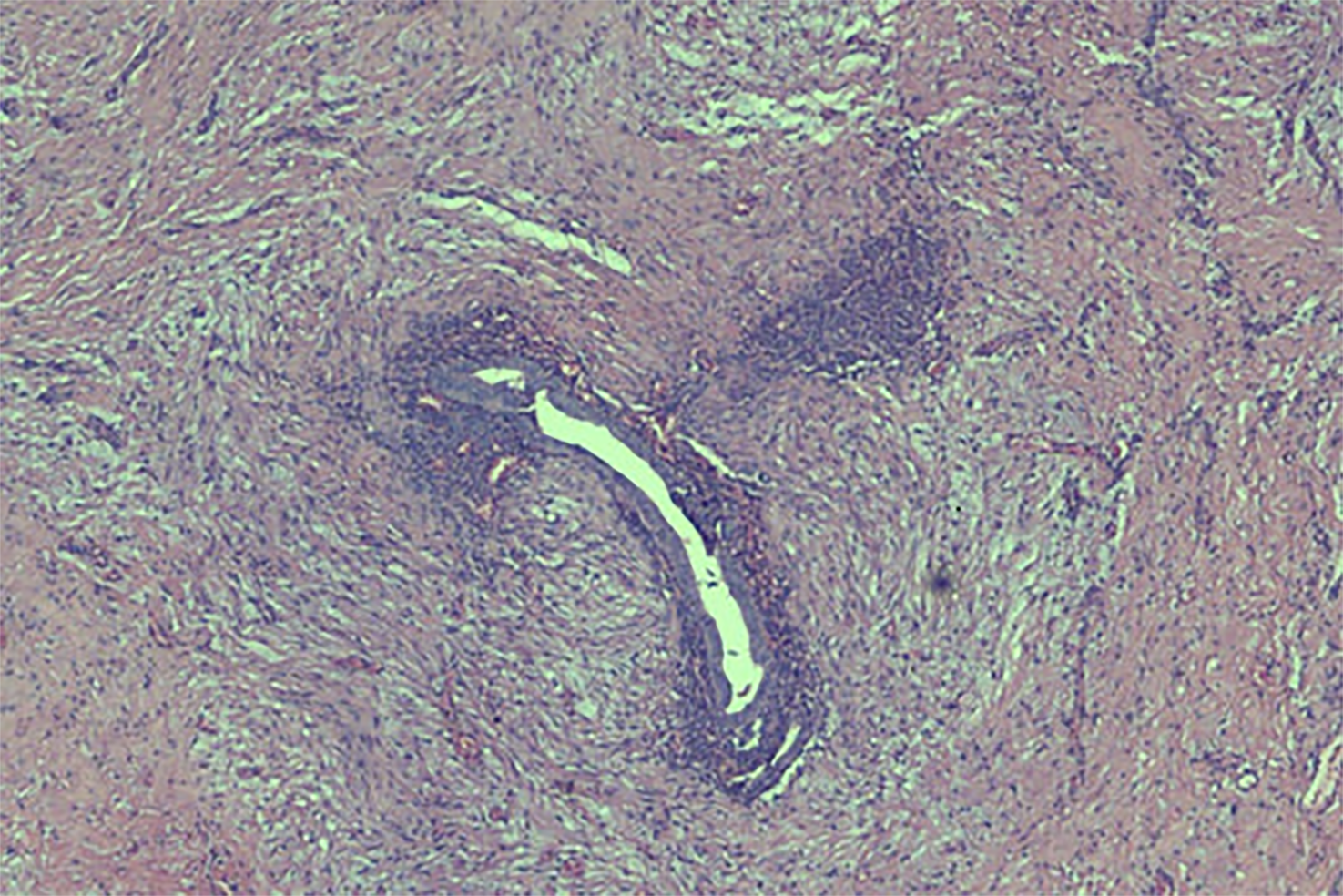
Postoperative anatomy showed the cut surface of the mass to be gray-white, gray-yellow, and solid. Both intraoperative and postoperative histological analyses confirmed umbilical endometriosis (Figure 2), and the wound recovered well after operation, without any recurrence to date.
This is a case report of an AWE that appeared in the abdominal wall incision after minimally invasive laparoscopic surgery. With the extensive development of laparoscopic surgery, there have been few reports of endometriosis at the cannula incision. Laparoscopic incision endometriosis was first reported by Denton et al[4] in 1990, as umbilical endometriosis after laparoscopic sterilization in a 37-year-old woman. According to Akbarzadeh-Jahromi et al[5], there have been 17 cases reported in the English literature. However, according to our literature review, the total number of cases reported in either English or Chinese is 71 to date, including 32 cases in English and 39 cases in Chinese. Overall, prospective studies are required to increase the quality of the existing literature. Most scholars agree that the etiology of scar endometriosis is endometrial cell planting during surgical treatment[1,5]. Endometriosis of the abdominal wall most commonly involves tissues around incisions following surgery, such as from cesarean section, abdominal wall incision after hysterectomy, and laparoscopic cannula incision for specimen collection. When taking out the tissue containing endometrial cells, the abdominal incision is most likely to contact endometrial cells. In our case, incision endometriosis occurred in the umbilical cannula incision. This incision is only used to place the laparoscopic camera, so the chance of contact with endometrial cells is small. We suspect that gloves or instruments contaminated with endometrial cells were responsible for the endometrial cells or debris present at the abdominal incision closed (by suture).
Abdominal wall mass (82%-96%) and pain (41%-87%) are the most common symptoms of AWE[6,7]. Only 57% of patients report periodic symptoms[7], and 3.08% (2/65) are asymptomatic[8]. Therefore, the periodicity of lump pain related to menstruation is not a necessary condition to diagnose AWE. In a study by Horton et al[7] that reviewed 29 articles, the average age of patients was 31.4 years (95% confidence interval: 29.1-33.8 years) and the average time of symptom onset was 3.6 years (95% confidence interval: 2.5-4.8 years)[7]. Anand et al[9] described the appearance of ectopic umbilical scar nodules being usually above the incision, with brown skin changes on the surface of the nodules, consistent with the appearance in our case (Figure 1).
AWE should be differentiated from incisional hernia, granulation tissue, hematoma, abscess, sediment, desmoid fibromatosis, lipoma, infection, soft tissue sarcoma, and metastatic malignant tumors[7,10]. Gupta et al[11] described cases of sporadic desmoid fibromatosis in the umbilical cord 8 mo after laparoscopic cholecystectomy. Desmoid fibromatosis is a rare benign soft tissue tumor originating from muscle-aponeurosis, without malignant potential; however, it can be locally invasive and is similar to AWE. It has been reported that many cases are misdiagnosed as hernia[5,12], and one case was misdiagnosed as umbilical granuloma[13].
Most AWEs have typical clinical symptoms, including palpable masses and pain without compression, combined with abdominal surgery history, which indicates a preliminary diagnosis of AWE. Nevertheless, there is no gold standard for preoperative diagnosis. Nodules on ultrasound (a modality characterized by low cost, safety, and noninvasiveness) are usually pear-shaped, with a solid hypoechoic or cystic appearance. Ultrasound, magnetic resonance imaging, or computed tomography can assist in determining the extent of lesions. Ultrasound-guided fine needle puncture can confirm the diagnosis and exclude the diagnosis of malignancies before operation. Surgical resection not only treats patients but can also confirm the diagnosis.
It is widely accepted that surgical excision is the most appropriate approach, and surgical excision of normal tissue 5-10 mm away from the edge of the lesion is required to prevent recurrence, according to the literature[3,5]. In the case of extensive lesions, computed tomography or magnetic resonance imaging can assess the location and size of AWE more accurately than ultrasound; moreover, they can prevail for the determination of whether to accumulate fascia and rectus abdominis muscles and if preoperative surgical evaluation is needed for reticular repair of the abdominal wall[3]. Large lesion area and rectus muscle involvement often indicate a higher recurrence rate. Apart from surgical excision, therapeutic percutaneous cryoablation can reduce the volume of lesions, as shown by preliminary studies but not yet confirmed by high-quality literature. Due to the histological characteristics of scars, it is difficult to achieve therapeutic effects around the lesion by oral medication alone. Oral contraceptives and progesterone can attenuate symptoms only slightly but cannot eliminate the lesion[3]. However, in a study conducted by Alborzi et al[14], who performed laparoscopic exploration after resection of abdominal wall mass in 30 AWE patients, it was found that 28 (93.3%) patients had pelvic endometriosis. Our case report is likely to support this conclusion. Therefore, after surgical resection of AWE, we believe that the postoperative treatment should be supplemented with medication.
A Japanese group, Tsuruga et al[15], previously reported the case of a 49-year-old woman with mixed endometrioid and clear cell carcinoma caused by endometriosis in the laparoscopic cannula during laparoscopic oophorocystectomy. Nevertheless, malignant transformation of peritoneal endometriosis is extremely rare. Clear cell carcinoma of abdominal incision is the most common histological type, followed by endometrioid carcinoma[16]. Other types include mixed adenocarcinoma, serous carcinoma, clear cell carcinoma, and carcinosarcoma. There is no authoritative consensus or guideline on the treatment of AWE malignancies. Despite the lack of direct evidence to support the benefit of chemotherapy at present, adjuvant chemotherapy or radiotherapy is typically administered after extensive surgical operation. The malignant transformation of AWE emphasizes the importance of surgical excision and pathological biopsy.
In consideration of the etiology of AWE iatrogenic implantation, prevention is the fundamental precaution to eliminate AWE. Clinically, the dissemination of endometrial cells should be avoided as much as possible in the first pelvic surgery for patients with ovarian function. In addition, preventive measures can be taken, such as using specimen bags to collect specimens. Saline irrigation should be carefully used when closing abdominal wall incisions, and potentially contaminated cannula incisions should also be flushed out. In addition, instruments contacting the specimens should be rinsed, hands and stitches should be flushed, or the stitches should be replaced. Laparoscopic surgery should not be performed during the menstrual period, and the postoperative complications should be reduced as much as possible for patients.
In summary, incisional endometriosis after laparoscopic surgery is rare, and the biological characteristics of the endometriosis are the appearance, growth, infiltration, and formation of nodules and masses in tissues outside the endometrium. Hence, abdominal mass and pain in women of childbearing age with a previous history of pelvic surgery should support consideration of AWE.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Family Planning Special Committee of the Sichuan Medical Association (Member), Reproductive Endocrinology Group of the Sichuan Medical Association (Member), Gynecological Endoscopy Group of the Sichuan Medical Association (Member).
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Daniilidis A, Richardson WS, Ulker K S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Uysal A, Mun S, Taner CE. Endometrioma in abdominal scars: case reports of four cases and review of the literature. Arch Gynecol Obstet. 2012;286:805-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Emre A, Akbulut S, Yilmaz M, Bozdag Z. Laparoscopic trocar port site endometriosis: a case report and brief literature review. Int Surg. 2012;97:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Rindos NB, Mansuria S. Diagnosis and Management of Abdominal Wall Endometriosis: A Systematic Review and Clinical Recommendations. Obstet Gynecol Surv. 2017;72:116-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Denton GW, Schofield JB, Gallagher P. Uncommon complications of laparoscopic sterilisation. Ann R Coll Surg Engl. 1990;72:210-211. [PubMed] |
| 5. | Akbarzadeh-Jahromi M, Motavas M, Fazelzadeh A. Recurrent abdominal wall endometriosis at the trocar site of laparoscopy: A rare case. Int J Reprod Biomed (Yazd). 2018;16:653-656. [PubMed] |
| 6. | Vellido-Cotelo R, Muñoz-González JL, Oliver-Pérez MR, de la Hera-Lázaro C, Almansa-González C, Pérez-Sagaseta C, Jiménez-López JS. Endometriosis node in gynaecologic scars: a study of 17 patients and the diagnostic considerations in clinical experience in tertiary care center. BMC Womens Health. 2015;15:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Horton JD, Dezee KJ, Ahnfeldt EP, Wagner M. Abdominal wall endometriosis: a surgeon's perspective and review of 445 cases. Am J Surg. 2008;196:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 224] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 8. | Ecker AM, Donnellan NM, Shepherd JP, Lee TT. Abdominal wall endometriosis: 12 years of experience at a large academic institution. Am J Obstet Gynecol. 2014;211:363.e1-363.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Anand M, Deshmukh SD. Massive abdominal wall endometriosis masquerading as desmoid tumour. J Cutan Aesthet Surg. 2011;4:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Siddiqui ZA, Husain F, Siddiqui Z, Siddiqui M. Port site endometrioma: a rare cause of abdominal wall pain following laparoscopic surgery. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Gupta R, Andley M, Talwar N, Kumar A. Sporadic Desmoid-Type Fibromatosis Occurring at Laparoscopic Trocar Site: An Unusual Entity. Indian J Surg. 2018;80:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Tatli F, Gozeneli O, Uyanikoglu H, Uzunkoy A, Yalcın HC, Ozgonul A, Bardakci O, Incebiyik A, Guldur ME. The clinical characteristics and surgical approach of scar endometriosis: A case series of 14 women. Bosn J Basic Med Sci. 2018;18:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Efremidou EI, Kouklakis G, Mitrakas A, Liratzopoulos N, Polychronidis ACh. Primary umbilical endometrioma: a rare case of spontaneous abdominal wall endometriosis. Int J Gen Med. 2012;5:999-1002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Alborzi S, Hamedi B, Abbasi S, Parsanejad ME. Association Rate between Incisional and Pelvic Endometriosis. J Endometriosis. 2011;3:183-187. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Tsuruga T, Hirata T, Akiyama I, Matsumoto Y, Oda K, Fujii T, Osuga Y. Mixed endometrioid and clear cell carcinoma arising from laparoscopic trocar site endometriosis. J Obstet Gynaecol Res. 2019;45:1613-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Taburiaux L, Pluchino N, Petignat P, Wenger JM. Endometriosis-Associated Abdominal Wall Cancer: A Poor Prognosis? Int J Gynecol Cancer. 2015;25:1633-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |