Published online Apr 6, 2020. doi: 10.12998/wjcc.v8.i7.1271
Peer-review started: December 9, 2019
First decision: January 7, 2020
Revised: January 13, 2020
Accepted: March 9, 2020
Article in press: March 9, 2020
Published online: April 6, 2020
Processing time: 118 Days and 17.6 Hours
Spinal intraosseous schwannomas (SIS) are rare, and as yet have not been fully described in the literature. The first case of SIS was reported in 1971, and 24 cases of SIS have been reported so far. However, including the present case, there are only seven cases without spinal canal and neuroforamina involvement.
A 56-year-old man presented with a history of neck pain for 2 years. An obvious osteolytic destruction of the seventh cervical (C7) vertebra was observed on imaging examination. Magnetic resonance imaging of the cervical spine showed space-occupying lesions in the C7 vertebra, and destruction of the anterior cortex of the vertebra. The lesions had an exophytic component that extended from the C7 vertebra into the soft tissue on the front side. The foramen transversarium on both sides were intact. The patient underwent surgical biopsy and focal excision of the C7 lesion. The diagnosis of “schwannoma” was verified by postoperative pathological examinations. In a review of the literature, this is the seventh case of SIS without spinal canal and neuroforamina involvement, and the third reported case of type VIII SIS. We discussed our case with respect to reported classification characteristics of SIS.
SIS is a very rare tumor. We report a rare case that may be important for further classification of osteo-schwannoma. The establishment of a complete disease classification is of high importance for the treatment and prognosis of this disease. Thus, more basic studies and retrospective analysis of related cases are necessary.
Core tip: Intraosseous schwannomas are extremely rare, accounting for < 0.2% of primary bone tumors. Spinal intraosseous schwannomas (SIS) are even rarer. We present a rare case of SIS of the seventh cervical (C7) vertebra in a 56-year-old man presenting with a history of neck pain for 2 years. An obvious osteolytic destruction of the C7 vertebra was observed on imaging examination. The patient underwent surgical biopsy and focal excision of the C7 lesion. The diagnosis of “schwannoma” was verified by postoperative pathological examinations. In a review of the literature, this is the seventh case of SIS without spinal canal and neuroforamina involvement, and the third case of type VIII SIS. It is important for further classification of osteo-schwannoma.
- Citation: Xu ZQ, Zhang P, Zhong ZH, Zhou W, Yu HT. Spinal intraosseous schwannoma without spinal canal and neuroforamina involvement: A case report. World J Clin Cases 2020; 8(7): 1271-1277
- URL: https://www.wjgnet.com/2307-8960/full/v8/i7/1271.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i7.1271
Intraosseous schwannomas are extremely rare, accounting for < 0.2% of primary bone tumors. The most common intraosseous lesions include the mandible and sacrum, while spinal lesions are less common. Spinal intraosseous schwannomas (SIS) are even rarer. Only 24 cases of SIS have been reported, of which 18 cases had lesions extending into the spinal canal or neuroforamina. We here present the seventh case of SIS without spinal canal and neuroforamina involvement, and the third case of type VIII SIS, with a review of the literature and discussion of this rare tumor.
A 56-year-old man presented with chronic and persistent neck pain for three months.
He had no previous trauma and medical problems.
There was local pain elicited by percussion of cervical spine. The range of cervical spinal motion was decreased, especially with regard to the flexion. Neurological examination revealed no abnormalities.
Routine blood examination and the C reactive protein concentration were normal.
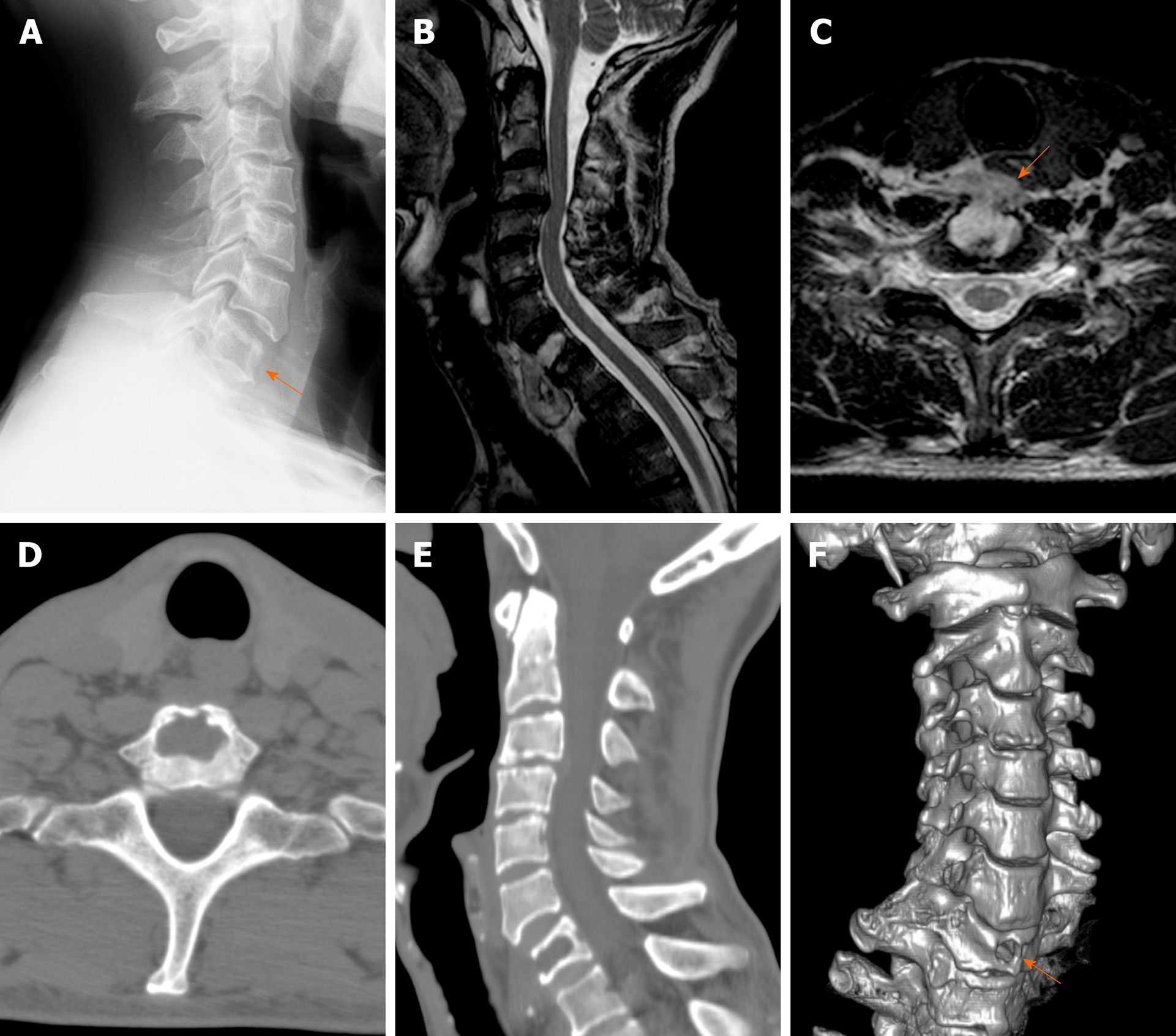
Conventional radiograph of the cervical spine showed loss of height of the seventh cervical (C7) vertebral body (Figure 1A). Magnetic resonance imaging (MRI) of the cervical spine showed space-occupying lesions in the C7 vertebra, and destruction of the anterior cortex of the vertebra. The lesions had an exophytic component that extended from the C7 vertebra into the soft tissue on the front side. The foramen transversarium on both sides were intact. The lesion area was well-circumscribed, showing a low signal on T1-weighted MRI and a high signal on T2-weighted MRI (Figure 1B and 1C). There was no extension of the lesion into the spinal canal, and no involvement of the spinal cord nerve. Computed tomography (CT) showed a C7 vertebral body lesion with lytic features indicative of a malignant etiology, and a bony defect of the C7 body, although the bony cortex of the vertebra was well preserved (Figure 1D-F).
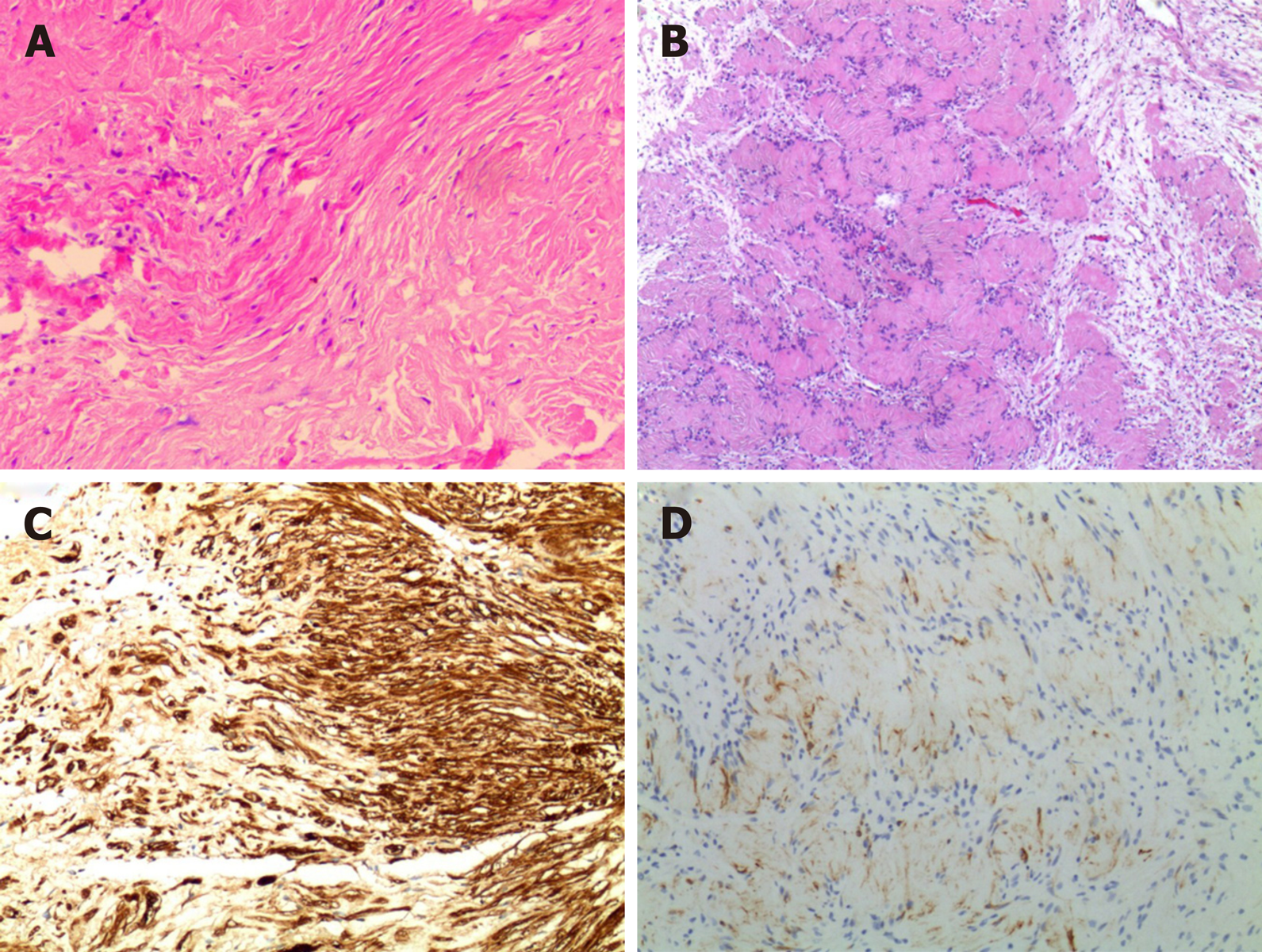
Histological examination of the lesion showed Antoni A and B areas with hypercellular, palisaded cells alternating with hypocellular stroma (Figure 2A). There were also regions with nuclear palisading suggestive of Verocay body formation (Figure 2B). Immunohistochemical staining with S100 protein and glial fibrillary acidic protein were diffusely positive (Figure 2C and 2D). The features were of a schwannoma (World Health Organization grade I). No nerve root remnants were identified in the specimen.
The final diagnosis of the presented case is spontaneous cerebral abscess due to spinal intraosseous schwannoma.
Based on the findings of typical vertebral lesions, suspected malignancy, with no evidence of a primary malignant process, surgical treatment was considered. The patient was operated upon via an anterior approach. A well-capsulated mass (3 cm × 2 cm) was found, which seemed to extrude from the anterior of the C7 vertebral body. The exophytic component was excised and the tumor was totally removed from the vertebral body using curettes, followed by C7 fusion using an iliac bone autograft.
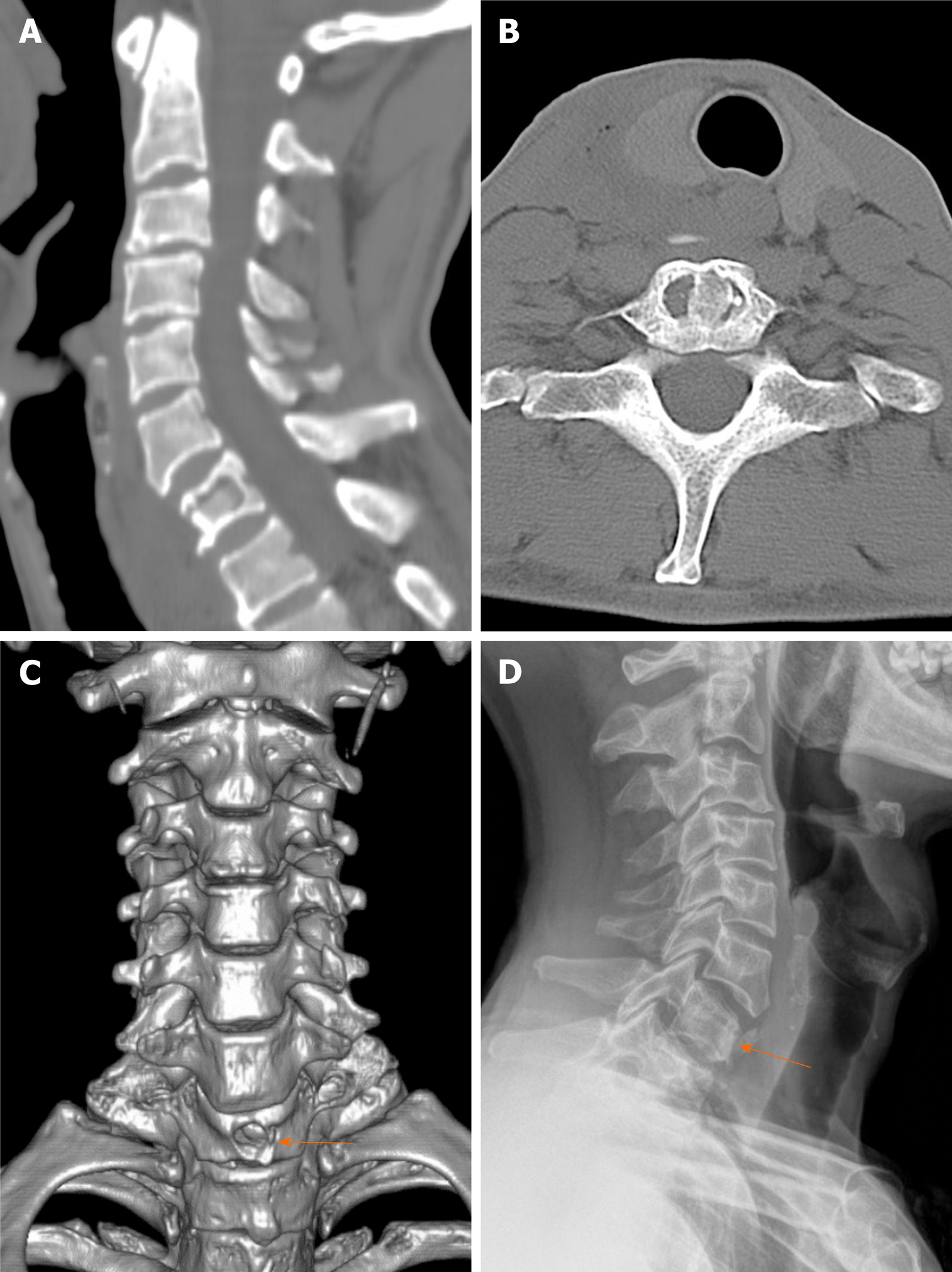
One week after surgery, postoperative computed tomography and X-ray did not reveal any evidence of tumor recurrence (Figure 3A-3D). The patient recovered well in the postoperative period. The neck pain was disappeared and at 1-year follow-up, the patient was doing well without any deficits.
Intraosseous schwannomas are rare benign tumors, accounting for < 0.2% of primary bone tumors. The most common intraosseous lesions include the mandible and sacrum, while spinal lesions are less common. The first case of SIS of a lumbar vertebral body was reported by Dickson et al[1] in 1971, where the lesion was located at the level of L3, but with extension to the spinal canal resulting in compression of the thecal sac. Only 24 cases of SIS (Table 1) have been reported, of which 18 cases had lesions extending into the spinal canal or neuroforamina. These tumors originally arose from the abutting nerve root, extending into the spinal canal and invading the vertebrae, suggesting that the SIS lesions likely involved intraosseous invasion of the extraosseous nerve sheath tumor originating from the spinal nerve root. This hypothesis is supported by most reports on SIS. However, the classification of SIS has not been fully described in the literature.
| No. | Ref. | Gender/age | Symptoms | Level | Classification | Stabilization | Final follow-up |
| 1 | Dickson et al[1], 1971 | F/51 | Radicular pain | L3 | VII | Iliac crest bone graft | No recurrence |
| 2 | Polkey et al[7], 1975 | F/34 | Pain and weakness | C6-C7 | VII | Iliac crest bone graft | No recurrence |
| 3 | Naidu et al[8], 1988 | M/50 | Weakness | C3-C4 | VII | - | No recurrence |
| 4 | Nooraie et al[9], 1997 | M/46 | Asymptomatic | T12 | VII | Fusion + fixation | No recurrence |
| 5 | Chang et al[10], 1998 | M/58 | Pain and numbness | L4-L5 | VII | Fusion + fixation | No recurrence |
| 6 | Schreuder et al[6], 2001 | F/38 | Dysphagia | C6 | VIII | Fusion + fixation | No recurrence |
| 7 | Ramasamy et al[11], 2001 | M/37 | Local pain, weakness | T12 | VII | Fusion + fixation | No recurrence |
| 8 | Gupta et al[12], 2005 | F/30 | Local pain, weakness | L2 | VII | Fusion + fixation | No recurrence |
| 9 | Nannapaneni et al[13], 2005 | M/42 | Asymptomatic | C5 | VIII | Fusion + fixation | No recurrence |
| 10 | Singrakhia et al[14], 2005 | M/43 | Numbness, weakness | C3-C4 | VII | Fusion + fixation | Recurrence |
| 11 | Singrakhia et al[14], 2006 | M/45 | Radicular pain, weakness | C3 | VII | Fusion + fixation | Recurrence |
| 12 | Choudry et al[15], 2007 | M/18 | Local pain, weakness | T12 | VII | Fusion + fixation | No recurrence |
| 13 | Cetinkal et al[16], 2009 | F/55 | Local pain, numbness | T12 | VII | - | No recurrence |
| 14 | Park et al[4], 2009 | F/46 | Local pain | L4 | VII | Fusion + fixation | No recurrence |
| 15 | Kojima et al[17], 2010 | M/60 | Weakness, numbness | T9 | VII | Fixation | No recurrence |
| 16 | Mizutani et al[18], 2010 | F/44 | Paresthesis | C4 | VI | - | No recurrence |
| 17 | Peng et al[19], 2011 | M/44 | Weakness | C3 | VII | Fusion + fixation | Recurrence |
| 18 | Youn et al[20], 2012 | M/65 | Local, numbness | L2 | VII | Fusion + fixation | No recurrence |
| 19 | Mohanty et al[5], 2013 | M/10 | Local pain, dysphagia | C4 | VIII | Fusion + fixation | No recurrence |
| 20 | Song et al[21], 2014 | M/44 | Numbness | L5 | VII | Fusion + fixation | No recurrence |
| 21 | Zhang et al[22], 2015 | M/71 | Radicular pain, weakness | L4 | VII | Fusion + fixation | No recurrence |
| 22 | Zhang et al[22], 2015 | F/54 | Radicular pain, weakness | T9 | VII | Fusion + fixation | No recurrence |
| 23 | Jia et al[23], 2018 | F/64 | Radicular pain, weakness | T7-T8 | VI | Fusion + fixation | No recurrence |
| 24 | Zaidman et al[24], 2019 | F/56 | Asymptomatic | T1 | VI | Fusion + fixation | No recurrence |
| 25 | Present study | M/56 | Local pain | C7 | VIII | Iliac crest bone graft | No recurrence |
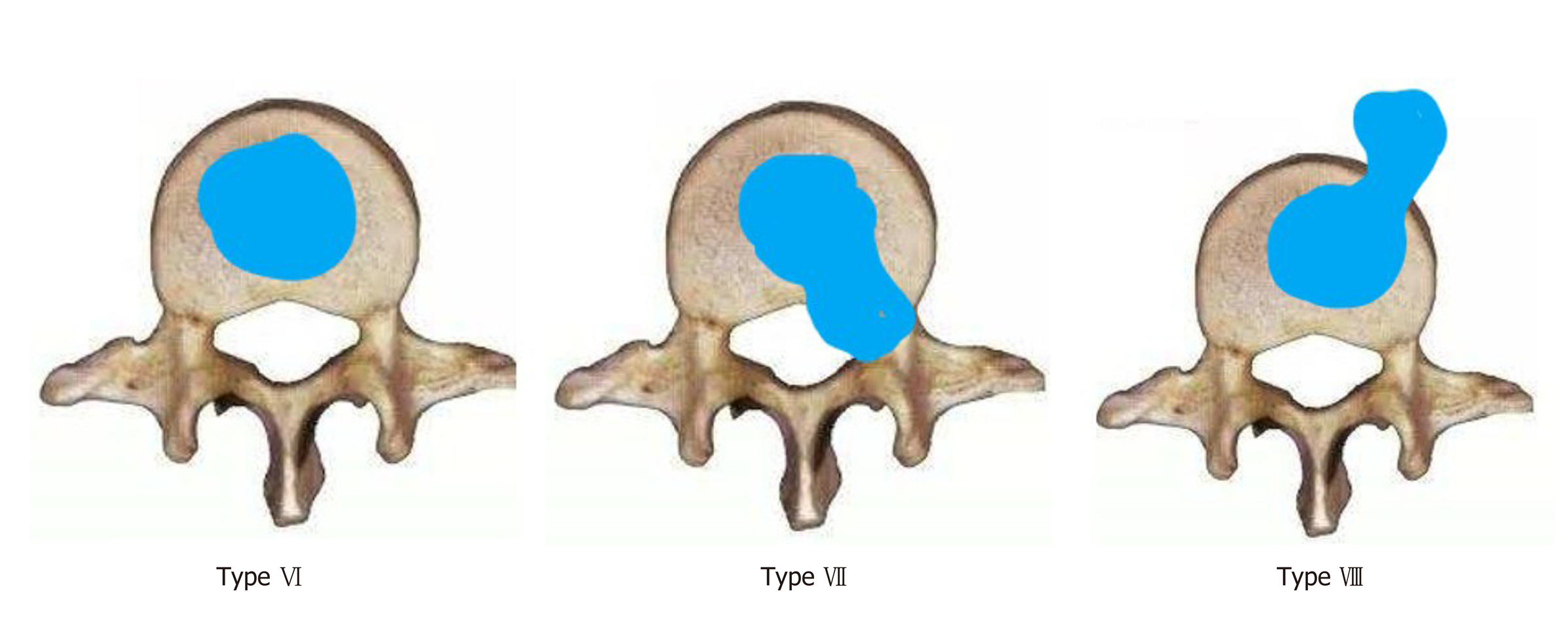
Wang et al[2] described the largest series of cases of SIS to date, with a retrospective analysis of the clinical features, surgical strategies, and outcomes of 20 cases of SIS. In that study, all of the lesions extended from layers A to D of the Weinstein-Boriani-Biagini classification, and all lesions exhibited extraosseous components extending into the spinal canal. In 2001, Sridhar et al[3] classified benign nerve sheath tumors, in which V-type tumors caused vertebral erosion. Park et al[4] modified this classification by adding type VI and type VII lesions; type VI is a complete intraspinal tumor, while type VII is an intraspinal tumor with vertebral erosion and expansion into the nerve foramen. However, the present case does not fit into any of these subtypes.
Mohanty et al[5] proposed a new subtype (type VIII) involving intraosseous tumors with an exophytic component, but without any intraspinal or neural foraminal extension. The present case is the third case of this VIII type SIS (Figure 4). The first case was published by Schreuder et al[6] in 2001, who described a lesion that extruded from the C6 vertebral body, and passed in front of the C7 vertebral body, although no specific category was described. We believe that the establishment of a VIII type is very important for SIS, and that the VIII and V types are associated with very different symptoms, surgical methods, and prognosis. Type VIII, which has an exophytic component, may present with symptoms related to compression of the surrounding structures such as dysphagia or pain, while no radicular pain or myelopathic features are present. Because the tumor does not involve the spinal canal or neuroforamina, it is not necessary to separate the tumor from the nerve root, making the operation safer. Postoperative nerve root numbness was reported in some patients.
A small number of patients with type VII relapsed during follow-up time, while no patient with type VIII relapsed. This may relate to the small number of patients with VIII, as well as the inability to fully dissect the nerve and tumor during type VII surgery. Most authors believe that vertebral resection and external fixation are appropriate surgical options, and the other two reported type VIII cases[5,6] utilized vertebral resection and external fixation. In the present case, the lesion was circumscribed within the cortical bone, the pedicle and facet joints were intact, and the stability of the cervical spine was not significantly decreased. Thus, after the lesion was completely scrapped, we used iliac bone grafting at the anterior edge of the vertebral body, without spinal external fixation. According to the follow-up and re-examination at 1 year after surgery, the prognosis of the patient was favorable, and no recurrence was observed (Figure 3D).
SIS is a very rare tumor. We report a rare case that may be important for further classification of osteo-schwannoma. The establishment of a complete disease classification is of great importance for the treatment and prognosis of this disease. Thus, more basic studies and retrospective analysis of related cases are necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Anand A, Emara KM, Elgafy H, Kung WM S-Editor: Dou Y L-Editor: MedE - Ma JY E-Editor: Zhang YL
| 1. | Dickson JH, Waltz TA, Fechner RE. Intraosseous neurilemoma of the third lumbar vertebra. J Bone Joint Surg Am. 1971;53:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Wang YQ, Hu JX, Yang SM, Jiang L, Liu XG, Yuan HS, Wei F, Liu ZJ. Intraosseous schwannoma of the mobile spine: a report of twenty cases. Eur Spine J. 2018;27:3092-3104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Sridhar K, Ramamurthi R, Vasudevan MC, Ramamurthi B. Giant invasive spinal schwannomas: definition and surgical management. J Neurosurg. 2001;94:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 61] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Park SC, Chung SK, Choe G, Kim HJ. Spinal intraosseous schwannoma: a case report and review. J Korean Neurosurg Soc. 2009;46:403-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Mohanty CB, Rao KV, Sampath S. Pediatric cervical intraosseous schwannoma. Pediatr Neurosurg. 2012;48:364-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Schreuder HW, Veth RP, Pruszczynski M, Lemmens JA, van Laarhoven EW. Intraosseous schwannoma (neurilemmoma) of the cervical spine. Sarcoma. 2001;5:101-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Polkey CE. Intraosseous neurilemmoma of the cervical spine causing paraparesis and treated by resection and grafting. J Neurol Neurosurg Psychiatry. 1975;38:776-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Naidu MR, Dinakar I, Rao KS, Ratnakar KS. Intraosseous schwannoma of the cervical spine associated with skeletal fluorosis. Clin Neurol Neurosurg. 1988;90:257-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Nooraie H, Taghipour M, Arasteh MM, Daneshbod K, Erfanie MA. Intraosseous schwannoma of T12 with burst fracture of L1. Arch Orthop Trauma Surg. 1997;116:440-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Chang CJ, Huang JS, Wang YC, Huang SH. Intraosseous schwannoma of the fourth lumbar vertebra: case report. Neurosurgery. 1998;43:1219-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Ramasamy P, Shackleford I, Al Jafari M. Schwannoma of t12 vertebra: case report and review of literature. Sarcoma. 2000;4:185-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Gupta SP, Agarwal A. Intraosseous neurilemmoma of L2 vertebra--a case report. Indian J Pathol Microbiol. 2005;48:367-369. [PubMed] |
| 13. | Nannapaneni R, Sinar EJ. Intraosseous schwannoma of the cervical spine. Br J Neurosurg. 2005;19:244-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Singrakhia MD, Parmar H, Maheshwari M, Fehlings M. Cervical schwannoma presenting as an expansile vertebral body lesion: report of two cases with a technical note on the surgical management. Surg Neurol. 2006;66:192-6; discussion 196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Choudry Q, Younis F, Smith RB. Intraosseous schwannoma of D12 thoracic vertebra: diagnosis and surgical management with 5-year follow-up. Eur Spine J. 2007;16 Suppl 3:283-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Cetinkal A, Atabey C, Kaya S, Colak A, Topuz AK. Intraosseous schwannoma of thoracic 12 vertebra without spinal canal involvement. Eur Spine J. 2009;18 Suppl 2:236-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Kojima M, Seichi A, Yamamuro K, Inoue H, Kimura A, Hoshino Y. Intraosseous schwannoma originating from the posterior column of the thoracic spine. Eur Spine J. 2011;20 Suppl 2:S153-S156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Mizutani A, Yokota N, Kawaji H, Yamaguchi-Okada M, Miyagawa T, Namba H. Intraosseous schwannoma of the cervical vertebral body: A case report and review of the literature. Br J Neurosurg. 2010;24:604-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Peng X, Chen L, Du H, Lai Y, Li F, Zou X. Malignant transformation of benign intraosseous schwannoma in the cervical spine: a case report with an immunohistochemical study. Int Surg. 2011;96:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Youn B, Lee SH, Kim ES, Eoh W. Intraosseous schwannoma with ancient change on the lumbar spine. Br J Neurosurg. 2012;26:561-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Song D, Chen Z, Song D, Li Z. Lumbar intraosseous schwannoma: case report and review of the literature. Turk Neurosurg. 2014;24:982-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Zhang F, Lu F, Jiang J, Wang H. Two Case Reports and an Updated Review of Spinal Intraosseous Schwannoma. J Korean Neurosurg Soc. 2015;57:478-483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Jia S, Zheng W, Ruan J, Chen T, Huang Y, Guan J. Mobile thoracic schwannoma combined with intraosseous schwannomas: A case report. Medicine (Baltimore). 2019;98:e14153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Zaidman N, Merve A, Russo V. Intraosseous Thoracic Schwannoma: Case Report and Review of the Literature. World Neurosurg. 2019;130:313-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |