Published online Mar 26, 2020. doi: 10.12998/wjcc.v8.i6.1142
Peer-review started: November 25, 2019
First decision: February 20, 2020
Revised: February 24, 2020
Accepted: March 5, 2020
Article in press: March 5, 2020
Published online: March 26, 2020
Processing time: 121 Days and 10.7 Hours
A swallowing disorder may occur following a brainstem stroke, especially one that occurs in the swallowing centers. Lateral medullary syndrome (referred to as LMS), a rare condition in which a vascular event occurs in the territory of the posterior inferior cerebellar artery or the vertebral artery, has been reported to lead to more severe and longer lasting dysphagia.
We report two patients with dysphagia due to LMS and propose a novel technique named hyoid-complex elevation and stimulation technique (known as HEST). The two patients had no other functional incapacity back into life, but nasogastric feeding was the only possible way for nutrition because of severe aspirations. Swallowing function was evaluated by functional oral intake scale, modified water swallow test, surface electromyographic signal associated with video fluorography swallowing study to assess the situation of aspiration, pharyngeal residue, pharyngeal peristalsis, upper esophageal opening and the ability of deglutition. Both patients were treated with the HEST method for dysphagia and recovered quickly.
HEST is effective for shortening the in-hospital time and improving the quality of life for patients with dysphagia who suffer from LMS and likely other strokes.
Core tip: For dysphagia treatment of lateral medullary syndrome, hyoid-complex elevation and stimulation technique is a novel technique that combines balloon dilation with electromyography-triggered electrical stimulation to restore swallowing function. It is easy to operate, safe for patients, and effective for shortening the in-hospital time. This case report suggests a new treatment for dysphagia patients, especially for those who cannot achieve the expected effect with traditional therapy.
- Citation: Jiang YE, Lyu QQ, Lin F, You XT, Jiang ZL. Hyoid-complex elevation and stimulation technique restores swallowing function in patients with lateral medullary syndrome: Two case reports. World J Clin Cases 2020; 8(6): 1142-1149
- URL: https://www.wjgnet.com/2307-8960/full/v8/i6/1142.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i6.1142
A swallowing disorder (dysphagia) may occur following a brainstem stroke, especially one that occurs in the swallowing centers in the posterior and lateral regions of the medulla oblongata. Lateral medullary syndrome (LMS), also known as Wallenberg syndrome, is a rare condition in which a vascular event occurs in the territory of the posterior inferior cerebellar artery or the vertebral artery[1] and reportedly leads to severe and long-lasting dysphagia[2] due to the absence of the swallowing reflex, extension of swallowing latency, dysfunction of the upper esophageal sphincter (UES) opening, and pharyngeal constriction. Nasogastric feeding has been the only possible method for obtaining nutrition because of severe aspiration. For patients with LMS, swallowing training is an indispensable treatment, and recovery of swallowing occurs with the restoration of pharyngeal function[3].
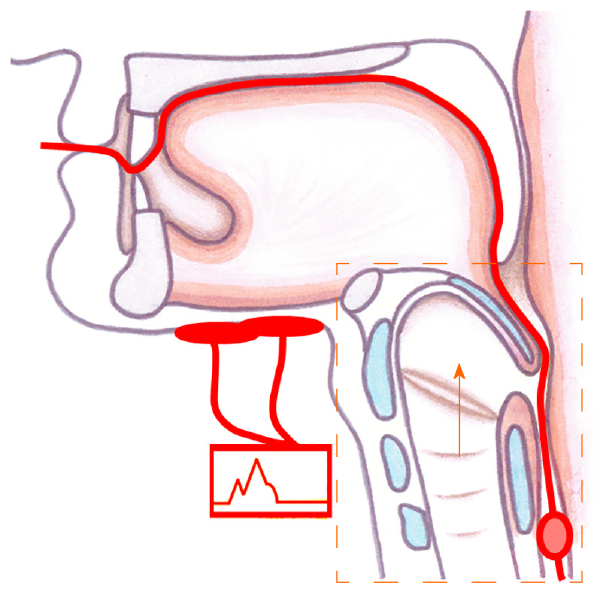
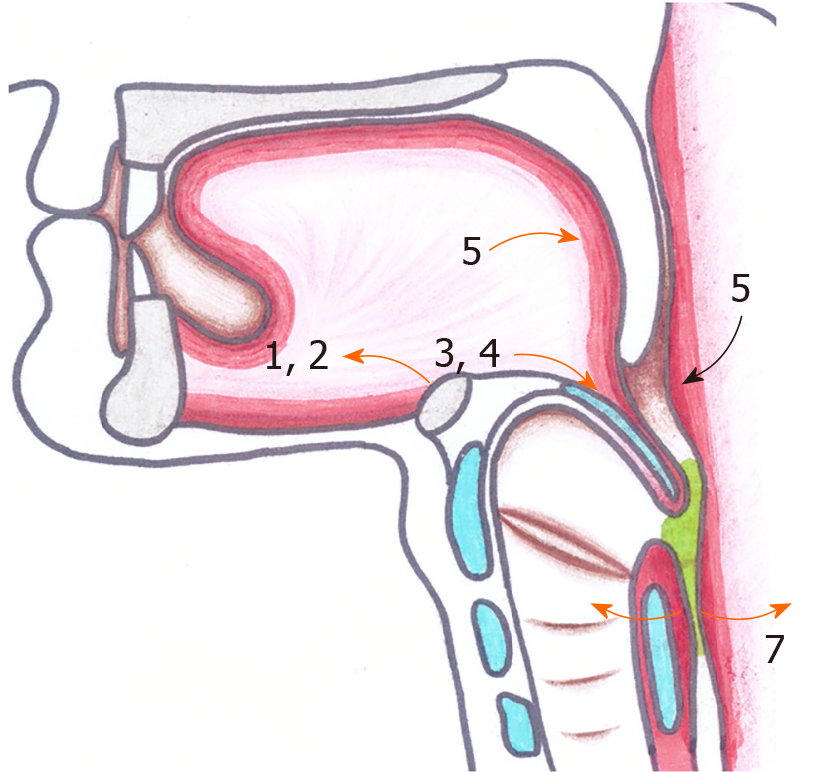
Here, we report two cases of patients with LMS who had restored swallowing function in a short period of time by using a hyoid-complex (the hyoid bone with pedunculus or epiglottidean complex tissues) elevation and stimulation technique (HEST). The operation procedure of this technique was as follows (Figure 1). First, a balloon catheter was inserted through the mouth to the edge of the UES, and the balloon was inflated by water when it was located at the lower edge of the cricoid cartilage and the UES. Then the balloon was lifted up at the same time as the hyoid-complex. Finally, patients were asked to swallow hard while the suprahyoid muscles were facilitated by electrical stimulation with a stimulus intensity dependent on the measured surface myoelectricity results. When an effective swallow was completed, the inflated balloon was very easy to remove. Aside from dysphagia due to lateral medullary infarction, neither patient with LMS had other functional incapacities in daily life.
Case 1: A 58-year-old male with LMS was admitted to the hospital with a chief complaint of “aphagosis for 20 d accompanying salivation and emaciation”.
Case 2: A 72-year-old male with LMS was admitted to the hospital with a chief complaint of “dysphagia for 24 d”.
Case 1: The patient had lost approximately 3 kg over the past 20 d and exhibited nutritional deficiency caused by dysphagia.
Case 2: The patient had lost approximately 5 kg over the past 24 d and exhibited nutritional deficiency caused by dysphagia.
Case 1: The patient was diagnosed with diabetes at the age of 48. His family members were all healthy.
Case 2: The patient had suffered from hypertension for over 10 years and from diabetes for over 5 years. His family members were all healthy.
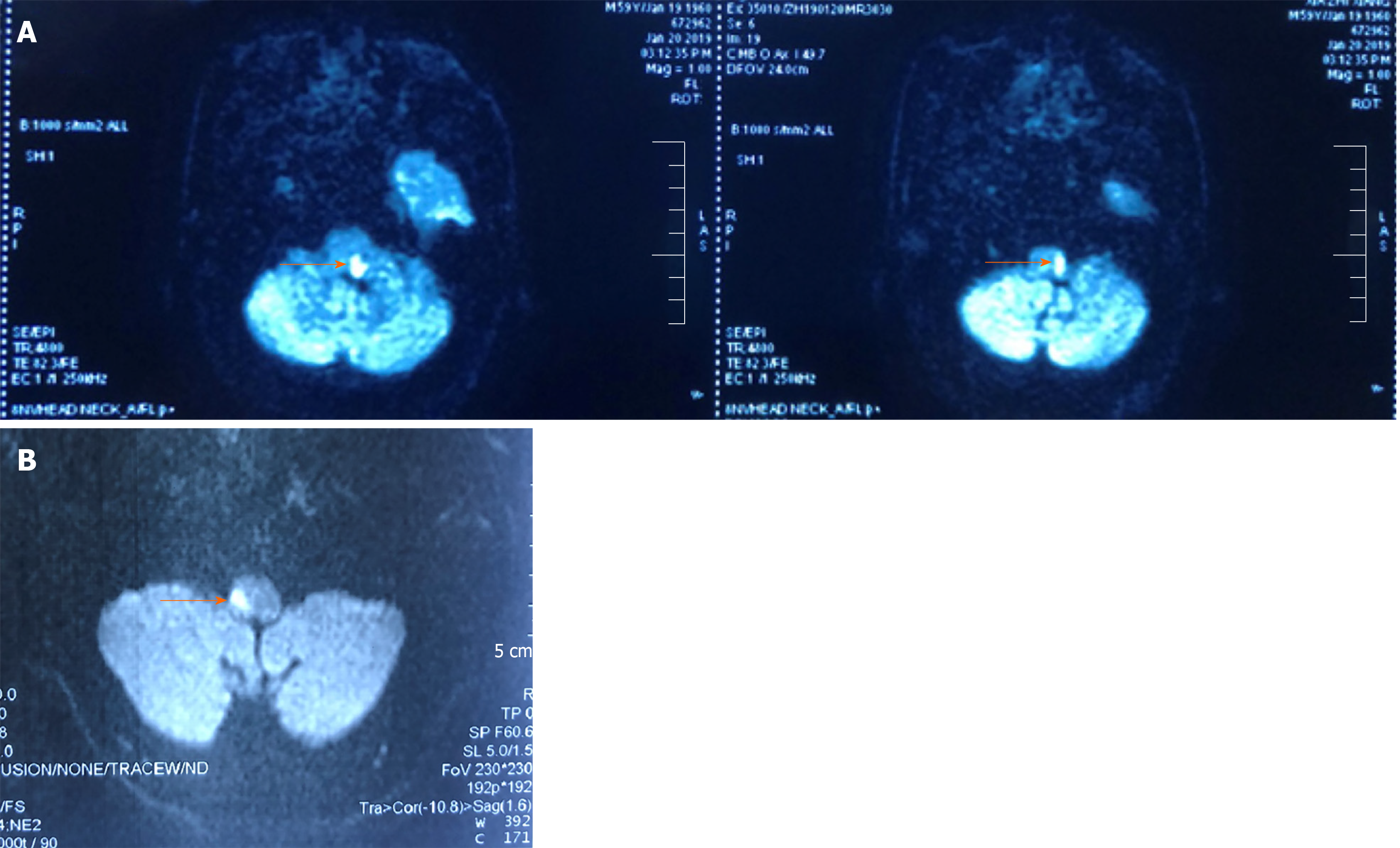
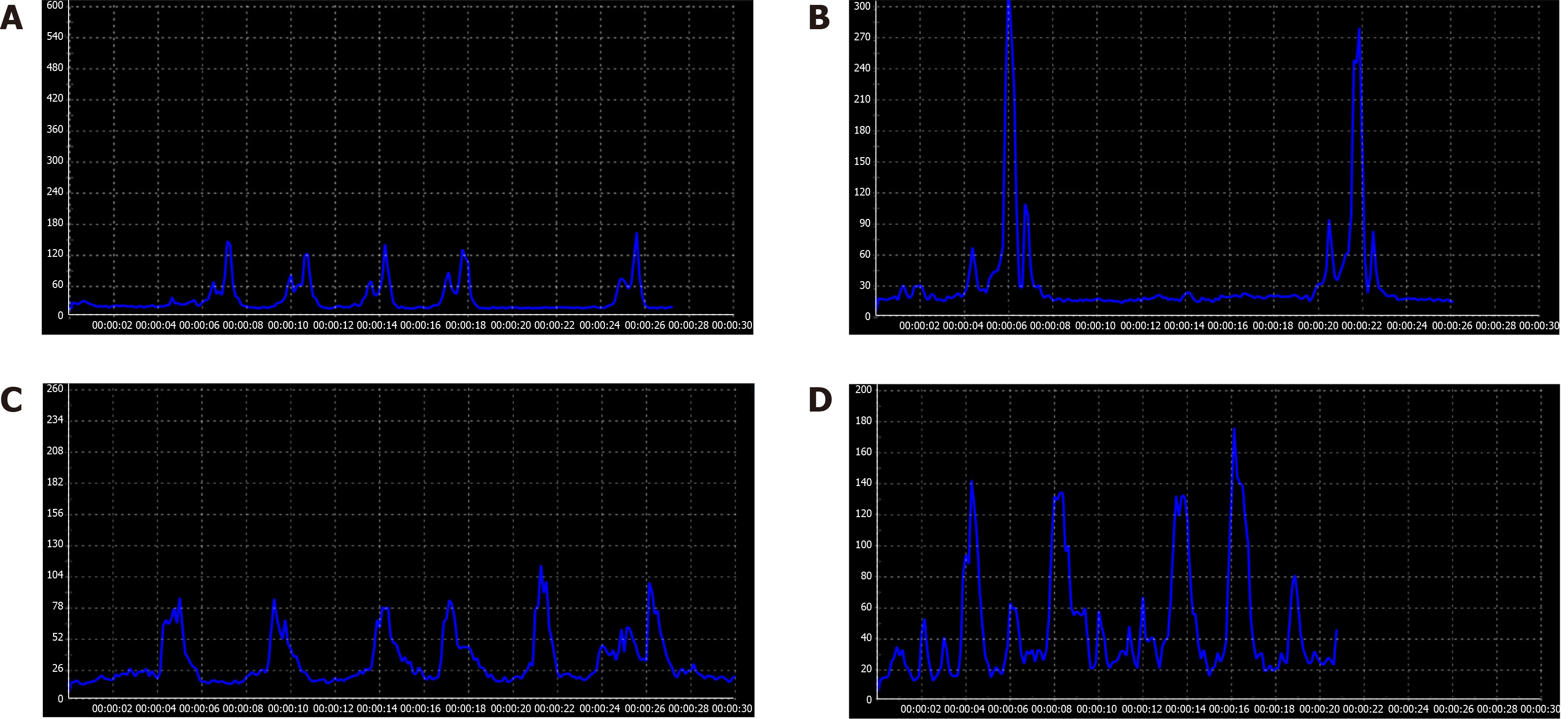
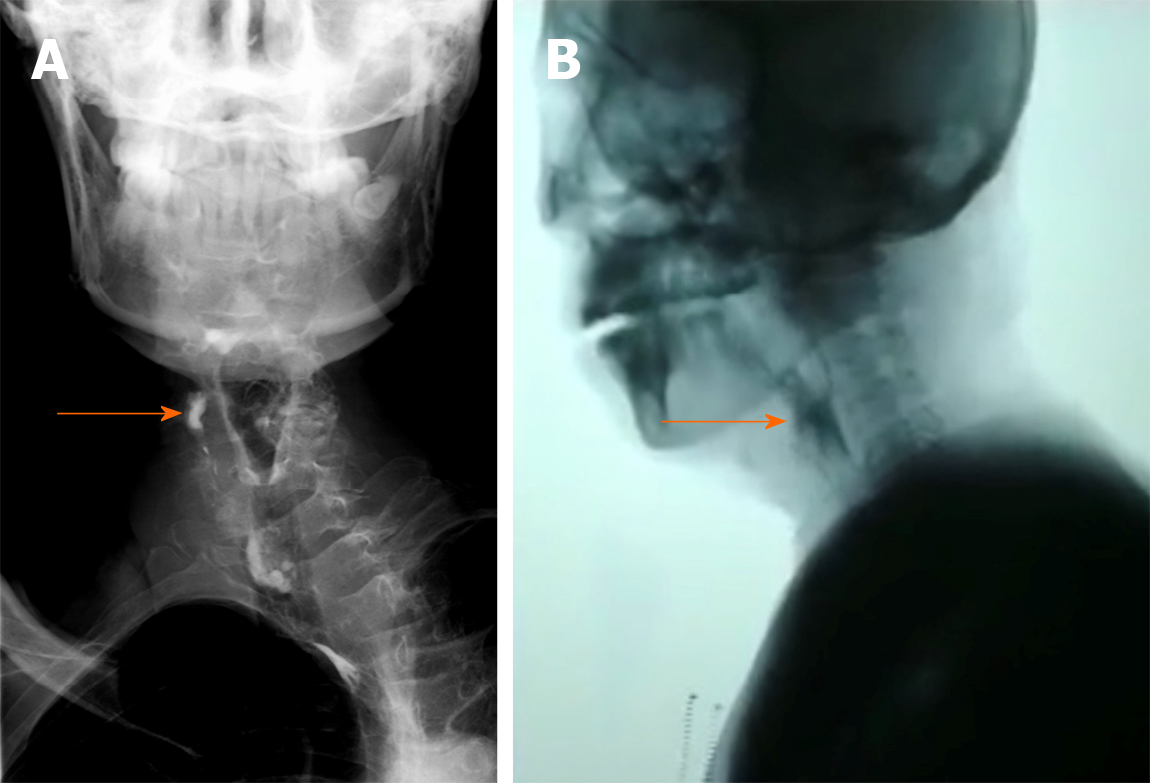
Case 1: An absent gag reflex, dystaxia in the left arm and leg, and decreased pain and temperature sensations in the right side of body were noted. Magnetic resonance imaging showed a left lateral medullary infarction (Figure 2A). The final diagnosis of the presented case was LMS. In the very beginning, the patient was unable to initiate a swallowing motion due to the absence of a swallowing reflex. The result of functional oral intake scale (FOIS) was performed at 20 d after the onset of stroke was level 1 (nothing by mouth), and the result of the modified water swallow test (MWST) was grade 1 (dysphagia with bucking, a wet voice and palatal paresis). On the 4th d after hospitalization, the surface electromyography (sEMG) signals of the suprahyoid muscles were recorded when the patient was asked to try to swallow, in which an imperfect swallowing motion and delayed pharyngeal transit time could also be observed (Figure 3A). A video fluorography swallowing study (VFSS) was examined on the 5th d after hospitalization, which showed leakage or aspiration, pharyngeal residue, incomplete epiglottic closure and UES dysfunction (Figure 4A). In addition, the fiberoptic endoscopic evaluation of swallowing examination (FEES) demonstrated epiglottis insufficiencies (Figure 5).
Case 2: An absent gag reflex and decreased sensation on the left side of the body were found by physical examination. Magnetic resonance imaging showed a right lateral medullary infarction (Figure 2B). The final diagnosis of the presented case was LMS. The initial FOIS result was level 1 (nothing by mouth). A VFSS was examined on the 19th d after the onset of the stroke, which showed leakage or aspiration, pharyngeal residue, decreased laryngeal elevation and impaired opening of the UES (Figure 4B). The result of the MWST performed on the 24th d after the onset of the stroke was grade 4 (no bucking, no residue and 1 swallowing movement could be initiated). Imperfect swallowing waves were observed by sEMG, especially when swallowing occurred on the left side (Figure 3B).
The final diagnosis of the presented two cases was LMS.
During the patient’s first week in the hospital, he received conventional treatment, including a behavioral approach and electrical stimulation. Swallowing function was not significantly improved. HEST was adopted in the second week and performed twice a day, 5 d per wk.
HEST was performed twice a day as well.
After 2 wk of treatment, the patient was able to resume oral feeding, and the nasogastric tube was removed. The second examination showed that the FOIS result was improved to level 7 (total oral diet with no restrictions) and the MWST result improved to grade 5 (no bucking, no residue and at least 2 or more swallowing motions could be initiated), and the sEMG signals resembled normal swallowing. At each initial swallowing movement, the target value could be easily achieved, but the latency became longer in the second and subsequent movements (Figure 3C). After discharge, the patient was advised to continue endurance training for a long time. The long-term outcome was investigated 12 mo later over the telephone because the present address of the patient was quite far away from the hospital. The only possible evaluation was FOIS, which maintained level 7 and the nutrition way maintained oral feeding. The time required for each meal was limited in 30 min.
On the third day after treatment, the patient was able to resume oral feeding, and the nasogastric tube was removed. The second examination showed that the FOIS result was level 7 (total oral diet with no restrictions), and the MWST result was grade 5 (no bucking, no residue and at least 2 or more swallowing movements could be initiated). Normal swallowing waves were observed by sEMG (Figure 3D). The follow-up was investigated 9 mo later over the telephone because the patient felt free to eat all kinds of foods and believed there was no need to be hospitalized. The FOIS of the patient-maintained level 7 as well. The nutrition way remained the same with each meal finished within 30 min.
The clinical treatment schedule of the two patients is shown in Table 1.
| Case 1 | Case 2 | |
| Chief complaint | Aphagosis for 20 d accompanying salivation and emaciation | Dysphagia for 24 d |
| MRI examination | Left lateral medullary infarction | Right lateral medullary infarction |
| Admission evaluation | Fois: Level 1 | Fois: Level 1 |
| MWST: Grade 1 | MWST: Grade 4 | |
| Semg: Imperfect swallowing motion and delayed pharyngeal transit time | sEMG: Imperfect swallowing waves especially when swallowing at the left side | |
| VFSS: Leakage or aspiration, pharyngeal residue, incomplete epiglottic closure and UES dysfunction | VFSS: Leakage or aspiration, pharyngeal residue, decreased laryngeal elevation and impaired opening of UES | |
| FEES: Epiglottis insufficiency | ||
| Start times of HEST | The 2nd wk (After 2 wk, the patient was able to resume oral feeding) | The 1st d (After 3 d, the patient was able to resume normal oral feeding) |
| Discharge evaluation | FOIS: Level 7 | FOIS: Level 7 |
| MWST: Grade 5 | MWST: Grade 5 | |
| sEMG: Normal | sEMG: Normal | |
| Follow-up | FOIS: Level 7 | FOIS: Level 7 |
| Oral feeding (Each meal could be finished within 30 min) | Oral feeding (Each meal could be finished within 30 min) |
Traditional therapy for dysphagia involves exercises to strengthen the oropharyngeal musculatures, lifting and compensatory maneuvers to facilitate laryngeal elevation and closure, techniques to stimulate and strengthen the swallowing reflex and diet modifications[4]. HEST therapy combines balloon techniques with electromyography-triggered electrical stimulation (ETS) patterns to reshape the physiological order of swallowing. The former technique was used to loosen the UES and elevate the hyoid-complex, meanwhile the latter technique was used for myoelectric biofeedback training. First, a No. 14 balloon catheter was gently inserted through the pharyngeal into the esophagus. If the patient did not cough and phonation was normal, 3 ml of water was injected into the balloon, and then the catheter was pulled upward until resistance was encountered, indicating the balloon was positioned at the lowest edge of the UES[5]. The plump balloon distracted the UES and lifted up when the sustaining resistance generated. Second, 2 electrodes of ETS were placed on mylohyoid muscles in the submental region above the hyoid bone[6]. ETS patterns were observed with the Guardian Aspire2[7], which incorporates neuromuscular electrical stimulation and surface electromyography biofeedback technology for measurement and treatment. The threshold value of the electrical stimulation was set in advance depending on the intensity to evoke the macroscopic contraction of mylohyoid muscles, which could be revealed by the movement of prominentia laryngea. In other words, ETS patterns were delivered to help accomplish the complete swallowing at the moment of every beginning. Hence, when the inflated balloon encountered resistance, the patients were instructed to swallow with effort, and ETS stimulation was simultaneously administered. A complete swallowing exercise was completed when the balloon could be pulled out with ease, which means the UES was loosen up and the hyoid-complex was elevated. This treatment was terminated when the patients reported restoration of full oral intake.
Swallowing is a patterned sequence of motor activity coordinated by bilateral swallowing centers in the rostral dorsolateral medulla[8]. The swallowing sequence involved with pharyngeal function followed seven steps[9]: (1) Laryngeal elevation; (2) Anterior hyoid motion; (3) Epiglottis movement; (4) Laryngeal closure; (5) Pharyngeal stripping wave; (6) Pharyngeal contraction; and (7) Pharyngoesophageal segment opening (Figure 6). Lateral medullary infarction impairs the sequence of swallowing events[10]. The patients cannot initiate contraction of the suprahyoid muscles for complete swallowing, and thus, the movements of the pharynx and the root of the tongue are affected. Without enough pressure from the tongue base, the epiglottis loses the ability to sufficiently close. However, HEST helps elevate the hyoid-complex and opens the UES at the right time, which are the beginning and ending of the normal swallowing movements, respectively. To be specific, ETS stimulation and balloon lifting work together to upraise the hyoid bone with pedunculus and epiglottidean complex tissues, while the active swallowing along with the balloon dilation help loosen the UES.
Compared with isolated muscle strength exercises such as the Mendelson maneuver, Masako maneuver, and electrical stimulation, HEST can improve the strength of suprahyoid muscles and lift the hyoid bone as well. In addition, HEST solves the tricky problem of UES opening, which results in leaking or aspiration from residue. On the other hand, balloon dilatation is an effective approach for UES opening and pharyngeal contraction[11]. However, patients with LMS require UES relaxation only during swallowing movements instead of plastic deformation[12,13]. The use of balloon dilatation alone does not improve laryngeal elevation, epiglottic closure, or pharyngeal contraction, which are necessary for swallowing efficiency and safety. In contrast, HEST can help reestablish a normal swallowing mechanism that follow the appropriate steps and complete the integrated movement.
We report two patients with dysphagia, who were treated with HEST technique and had restored swallowing function within a short time. Because this technique is effective, easy to operate, and safe, the possibility of a wider application of HEST is suggested to restore swallowing function in patients with oropharyngeal dysphagia. Further studies with a larger population are needed to clearly verify the underlying mechanisms.
The authors would like to thank the rehabilitation team at Sir Run Run Hospital for their collaboration and our patients. The patients were informed about, and consented to, publication of the case details.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Paredes-Vieyra JP, Yen HH S-Editor: Dou Y L-Editor: Filipodia E-Editor: Li X
| 1. | El Mekkaoui A, Irhoudane H, Ibrahimi A, El Yousfi M. Dysphagia caused by a lateral medullary infarction syndrome (Wallenberg's syndrome). Pan Afr Med J. 2012;12:92. [PubMed] |
| 2. | Eker A, Kaymakamzade B, Akpinar S. Treatment of Wallenberg's Syndrome related dysphagia with pyridostigmine. Acta Neurol Belg. 2017;117:329-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Vigderman AM, Chavin JM, Kososky C, Tahmoush AJ. Aphagia due to pharyngeal constrictor paresis from acute lateral medullary infarction. J Neurol Sci. 1998;155:208-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Frost J, Robinson HF, Hibberd J. A comparison of neuromuscular electrical stimulation and traditional therapy, versus traditional therapy in patients with longstanding dysphagia. Curr Opin Otolaryngol Head Neck Surg. 2018;26:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Wei X, Yu F, Dai M, Xie C, Wan G, Wang Y, Dou Z. Change in Excitability of Cortical Projection After Modified Catheter Balloon Dilatation Therapy in Brainstem Stroke Patients with Dysphagia: A Prospective Controlled Study. Dysphagia. 2017;32:645-656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Zhang M, Tao T, Zhang ZB, Zhu X, Fan WG, Pu LJ, Chu L, Yue SW. Effectiveness of Neuromuscular Electrical Stimulation on Patients With Dysphagia With Medullary Infarction. Arch Phys Med Rehabil. 2016;97:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | ASHA. National Outcomes Measurement System (NOMS): Adult Speech-Language Pathology Userâs Guide. 2003. Available from: http://docshare01.docshare.tips/files/7828/78286027.pdf. |
| 8. | Aydogdu I, Ertekin C, Tarlaci S, Turman B, Kiylioglu N, Secil Y. Dysphagia in lateral medullary infarction (Wallenberg's syndrome): an acute disconnection syndrome in premotor neurons related to swallowing activity? Stroke. 2001;32:2081-2087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 86] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS measurement tool for swallow impairment--MBSImp: establishing a standard. Dysphagia. 2008;23:392-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 460] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 10. | Nakao M, Oshima F, Maeno Y, Izumi S. Disruption of the Obligatory Swallowing Sequence in Patients with Wallenberg Syndrome. Dysphagia. 2019;34:673-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Lan Y, Xu G, Dou Z, Wan G, Yu F, Lin T. Biomechanical changes in the pharynx and upper esophageal sphincter after modified balloon dilatation in brainstem stroke patients with dysphagia. Neurogastroenterol Motil. 2013;25:e821-e829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Mendell DA, Logemann JA. Temporal sequence of swallow events during the oropharyngeal swallow. J Speech Lang Hear Res. 2007;50:1256-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Herzberg EG, Lazarus CL, Steele CM, Molfenter SM. Swallow Event Sequencing: Comparing Healthy Older and Younger Adults. Dysphagia. 2018;33:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |