Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.658
Peer-review started: January 2, 2020
First decision: January 19, 2020
Revised: January 20, 2020
Accepted: February 15, 2020
Article in press: February 15, 2020
Published online: February 26, 2020
Processing time: 55 Days and 8.4 Hours
Gastric signet ring cell carcinoma (GSRCC) is one of the most malignant tumors. It has the features of high invasiveness, rapid progression, and resistance to chemotherapy. However, systematic analyses of mRNAs have not yet been performed for GSRCC.
To identify key mRNAs and signaling pathways in GSRCC.
A transcriptome analysis of two GSRCC and two non-GSRCC samples was performed in this study. Differentially expressed mRNAs and pathways were identified based on the KEGG and PANTHER pathway annotations. The interactive relationships among the differential genes were mapped with the STRING database. Quantitative real-time polymerase chain reaction was used to validate the key gene expression in GSRCC.
About 1162 differential genes (using a 2-fold cutoff, P < 0.05) were identified in GSRCC compared with non-GSRCC. The enriched KEGG and PANTHER pathways for the differential genes included immune response pathways, metabolic pathways, and metastasis-associated pathways. Ten genes (MAGEA2, MAGEA2B, MAGEA3, MAGEA4, MAGEA6, MUC13, GUCA2A, FFAR4, REG1A, and REG1B) were identified as hub genes in the protein-protein interaction network. The expression levels of five genes (MAGEA2, MAGEA3, MAGEA4, MAGEA6, and REG1B) showed potential clinical value.
We have identified the potential key genes and pathways in GSRCC, and these hub genes and pathways could be diagnostic markers and therapeutic targets for GSRCC.
Core tip: Gastric signet ring cell carcinoma (GSRCC) is one of the most malignant tumors. It has the features of high invasiveness, rapid progression, and resistance to chemotherapy. However, systematic analyses of mRNAs have not yet been performed for GSRCC. We have identified the potential key genes and pathways of GSRCC, and these hub genes and pathways could be diagnostic markers and therapeutic targets for GSRCC.
- Citation: Zhao ZT, Li Y, Yuan HY, Ma FH, Song YM, Tian YT. Identification of key genes and pathways in gastric signet ring cell carcinoma based on transcriptome analysis. World J Clin Cases 2020; 8(4): 658-669
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/658.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.658
Gastric cancer (GC) is the 5th most common carcinoma in the world, with a morbidity of over 1000000 new patients in 2018, and is the 3rd principal cause of death by cancer worldwide[1]. Recently, different pathohistological standard methods have been established for GC. The massive majority of GCs are adenocarcinomas, which can be further divided into intestinal and diffuse types by Lauren classification[2,3]. An alternative classification, proposed by the World Health Organization, divides gastric cancer into tubular, mucinous, papillary, and poorly cohesive carcinomas[4]. Diffuse type is generated by poorly cohesive cells without gland formation and is frequently referred to as gastric signet ring cell carcinoma (GSRCC). GSRCC is a histologic diagnosis based on microscopic characteristics as the presence of signet ring cells in over 50% of the cancer cells by the World Health Organization[5]. These classification methods have little clinical value. An important priority of proper classifiers should be studied to guide therapeutics. Considering the epidemiology of GSRCC, it happens more frequently in females than non-GSRCC, and occurs among patients aged between 55 to 61 years, 7 years ahead of those with non-GSRCC[6,7]. Since the beginning of treatment to eradicate Helicobacter pylori, the incidence of gastric adenocarcinoma has decreased. Conversely, the incidence of GSRCC is rising. The GSRCC is found in 8% to 30% of GCs[8].
The prognosis of GSRCC in entire mentioned reports has been described as un-inferior than the other gastric cancer subtypes in the early stage[9,10]. Contrariwise, the prognosis of GSRCC in advanced stages is quite poor, and most studies showed a significantly worse 5-year survival rate in patients with GSRCC than in those with non-GSRCC. Furthermore, Lemoine et al[11] showed that patients with advanced GSRCC appeared to benefit less from chemotherapy. Pathological response rate to chemotherapy was significantly lower in GSRCC patients (5.3% vs 28.1%, P = 0.0004). Another German analysis confirmed that a worse histopathological response (16.3% vs 28.9%, P < 0.001) in patients was affected by preoperative chemotherapy. An ongoing PRODIGE19 trial (NCT01717924) tends to randomize patients with resectable GCs with signet ring cells receiving perioperative chemotherapy with ECF vs an upfront surgery followed by adjuvant chemotherapy with the same regimen[12]. However, the results are still uncertain. The effects of chemotherapy on GSRCC are still in controversy. According to its potential drug resistance, current studies have mainly focused on the pathogenesis study of GSRCC with regard to some disease-related genes.
To find out the molecular mechanisms for tumorigenesis and heterogeneity of GSRCC at the molecular level, large studies have been taken to characterize the comprehensive genomic features through transcriptome sequencing, and multiple driver alterations have been recognized. The exploration of the molecular mechanism of GSRCC is important to improve the recognition of GSRCC and find the effective therapeutics to raise the survival rate of patients. To our best knowledge, systematic and comprehensive analyses of mRNAs have not yet been conducted for GSRCC. In this study, transcriptome sequencing and comprehensive analysis were performed to identify key mRNAs and signaling pathways in GSRCC, with an aim to provide new insights into the treatment and feature of GSRCC.
A total of 60 patients who underwent surgery for GSRCC at National Cancer Center, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China were selected for inclusion in the study. All clinicopathological data including age, sex, histological type, and lymph node metastasis were obtained from the database. Four of samples were sent to conduct transcriptome sequencing, and 56 of samples were taken for validation.
The transcriptome sequencing was used for mRNA expression profiling (CapitalBio).
The functional enrichment of the differential genes was assessed based on the KEGG and PANTHER pathway annotations.
To evaluate the interactive relationships among the differential genes, we mapped the differential genes to the STRING database (http://string-db.org).
Total RNA was extracted from frozen fresh tissues with the RNAExpress Total RNA Kit (New Cell & Molecular Biotech Co., Ltd). cDNA was synthesized with the First-Strand cDNA Synthesis Kit (Applied Biological Materials). Quantitative real-time polymerase chain reaction (qPCR) was performed with EvaGreen 2X qPCR MasterMix (Applied Biological Materials). And the primers used are listed in Table 1. The mRNA sequence of MAGEA2/3/6 is too similar to design primers for separately verifying and validating these three genes, so we designed three pairs of primers for MAGEA2/3/6 to validate the expression of these genes together.
| Gene | Primer sequence (5’-3’) |
| MAGEA2/3/6; primer 1 | F: CAGAGGAGTCAGCACTGCAA |
| R: TAGTCGAGAAGCTGGAGGCT | |
| MAGEA2/3/6; primer 2 | F: CAGAGGAGTCAGCACTGCAA |
| R: TAGTCGAGAAGCTGGAGGCT | |
| MAGEA4 | F: CTGCTGTCTCCTCCTCCTCT |
| R: GGAACAAGGACTCTGCGTCA | |
| MAGEA2/3/6; primer 3 | F:CAGAGGAGTCAGCACTGCAA |
| R:GACTCTGGGGAGGATCTGGT | |
| REG1A | F: TGACCCCAAAAAGAACCGCC |
| R: AGAACTTGTCTTCACAAGGCAC | |
| REG1B | F: GATCCCCGAGCAGTGCTAAT |
| R: CTTCTCACAAGATTCATCCTTCCA | |
| GAPDH | F: TGTTGCCATCAATGACCCCTT |
| R: CTCCACGACGTACTCAGCG |
The data are presented as the mean ± SE. The differences were assessed by the two-tailed Student's t-test for group comparisons using the GraphPad Prism 5 software package. Differences were considered significant when P values were less than 0.05.
In this study, four primary GC patients underwent transcriptome sequencing, consisting of two patients with GSRC and two with adenocarcinoma. All of them are male with a median age of 49 years old and poorly differentiated carcinomas. The positive lymph node rate was separately 26/70 and 5/26 in the GSRC group, and 0/45 and 27/34 in the adenocarcinoma group. The two GSRC samples pathologically consisted of over 90% of signet ring cells in the tumor.
Further, 56 samples were chosen for validation. The analysis of the 60 samples showed that there were not significant differences between the GSRCC group and adenocarcinoma group in baseline characteristics such as age, gender, TNM stages, lymphovascular invasion, or nerve invasion, although there were significant differences in Lauren type (P < 0.001) and histology differentiation (P = 0.038, Table 2).
| Characteristic | Overall (n = 60) | GSRCC (n = 30) | Adenocarcinoma (n = 30) | P value |
| Age (yr) | 0.052 | |||
| ≤ 65 | 41 (68.3) | 24 (80.0) | 17 (56.7) | |
| > 65 | 19 (31.7) | 6 (20.0) | 13 (43.3) | |
| Gender | 0.584 | |||
| Male | 40 (66.7) | 21 (70.0) | 19 (63.3) | |
| Female | 20 (33.3) | 9 (30.0) | 11 (36.7) | |
| Tumor size (cm) | 0.584 | |||
| ≤ 5 | 40 (66.7) | 21 (70.0) | 19 (63.3) | |
| > 5 | 20 (33.3) | 9 (30.0) | 11 (36.7) | |
| Lauren type | 0 | |||
| Intestinal | 12 (20.0) | 0 (0) | 12 (40.0) | |
| Diffuse | 35 (58.3) | 26 (86.7) | 9 (30.0) | |
| Mixed | 12 (20.0) | 4 (13.3) | 8 (26.7) | |
| Unknown | 1 (1.67) | 0 (0) | 1 (3.3) | |
| Histology differentiation | 0.038 | |||
| Poorly/un-differentiated | 56 (93.3) | 30 (100.0) | 26 (86.7) | |
| Well/moderately differentiated | 4 (6.7) | 0 (0) | 4 (13.3) | |
| Unknown | ||||
| T stage | 0.725 | |||
| T1 | 5 (8.3) | 3 (10.0) | 2 (6.7) | |
| T2 | 9 (15.0) | 3 (10.0) | 6 (20.0) | |
| T3 | 12 (20.0) | 6 (20.0) | 6 (20.0) | |
| T4 | 34 (56.7) | 18 (60.0) | 16 (53.3) | |
| N stage | 0.639 | |||
| N0 | 16 (26.7) | 8 (26.7) | 8 (26.7) | |
| N1 | 6 (10.0) | 3 (10.0) | 3 (10.0) | |
| N2 | 20 (33.3) | 8 (26.7) | 12 (40.0) | |
| N3 | 18 (30.0) | 11 (36.7) | 7 (23.3) | |
| M stage | 0.15 | |||
| Metastasis | 2 (3.3) | 2 (6.7) | 0 (0) | |
| No metastasis | 58 (96.7) | 28 (93.3) | 30 (100.0) | |
| Positive lymph nodes | 0.39 | |||
| ≤ 8 | 43 (71.7) | 20 (66.7) | 23 (76.7) | |
| > 8 | 17 (28.3) | 10 (33.3) | 7 (23.3) | |
| Lymphovascular invasion | 0.355 | |||
| Yes | 31 (51.7) | 15 (50.0) | 16 (53.3) | |
| No | 27 (45.0) | 13 (43.3) | 14 (46.7) | |
| Unknown | 2 (3.3) | 2 (6.7) | 0 (0) | |
| Nerve invasion | 0.213 | |||
| Yes | 42 (70.0) | 22 (73.3) | 20 (66.7) | |
| No | 16 (26.7) | 6 (20) | 10 (33.3) | |
| Unknown | 2 (3.3) | 2 (6.7) | 0 (0) | |
| Neoadjuvant chemotherapy | 0.688 | |||
| Yes | 7 (88.3) | 4 (13.3) | 3 (10.0) | |
| No | 53 (11.7) | 26 (86.7) | 27 (90.0) |
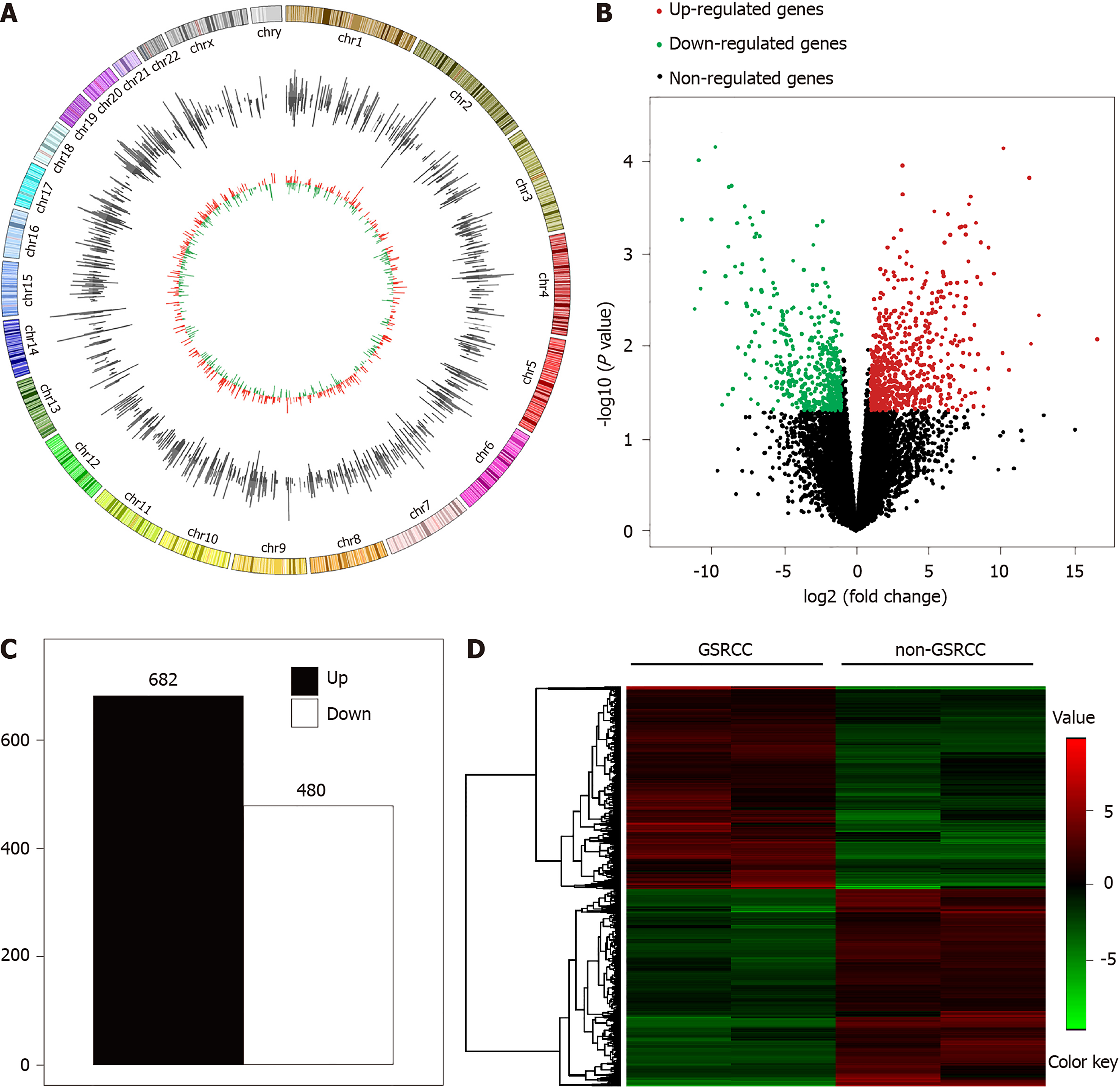
Transcriptome sequencing was used to profile the mRNA expression in four patients with GC (two with GSRCC and two with non-GSRCC) who underwent surgical treatment (Figure 1). There were 1162 differential genes (using a 2-fold cutoff, P < 0.05), which included 682 upregulated and 480 downregulated genes in GSRCC compared with non-GSRCC. The top 10 up-regulated genes were MAGEA2, MAGEA6, MAGEA3, MAGEA2B, ISY1-RAB43, MAGEA9, MAGEA9B, MAGEA12, KRT16P6, and NEUROD2. The top 10 down-regulated genes were REG1B, REG1A, SPINK4, GIF, ATOH1, IGHV4-4, GUCA2A, DMBT1, SOSTDC1, and ATP4B. The fold changes and P values of these differential genes are listed in Table 3.
| Genes | Fold change | P value |
| Top 10 up-regulated genes | ||
| MAGEA2 | 9182.176 | 0.000031 |
| MAGEA6 | 4410.054 | 0.000429 |
| MAGEA3 | 2508.358 | 0.0000307 |
| MAGEA2B | 1971.738 | 0.0000976 |
| ISY1-RAB43 | 1921.249 | 0.0000394 |
| MAGEA9 | 1787.459 | 0.002399 |
| MAGEA9B | 1469.006 | 0.001587 |
| MAGEA12 | 1064.08 | 0.000427 |
| KRT16P6 | 633.9792 | 0.043469 |
| NEUROD2 | 574.5342 | 0.000245 |
| Top 10 down-regulated genes | ||
| REG1B | 0.00000891 | 0.008502 |
| REG1A | 0.000149 | 0.004671 |
| SPINK4 | 0.000217 | 0.009491 |
| GIF | 0.000237 | 0.000152 |
| ATOH1 | 0.000632 | 0.018238 |
| IGHV4-4 | 0.000822 | 0.0000723 |
| GUCA2A | 0.000853 | 0.011982 |
| DMBT1 | 0.001304 | 0.001651 |
| SOSTDC1 | 0.001678 | 0.000862 |
| ATP4B | 0.001709 | 0.017566 |
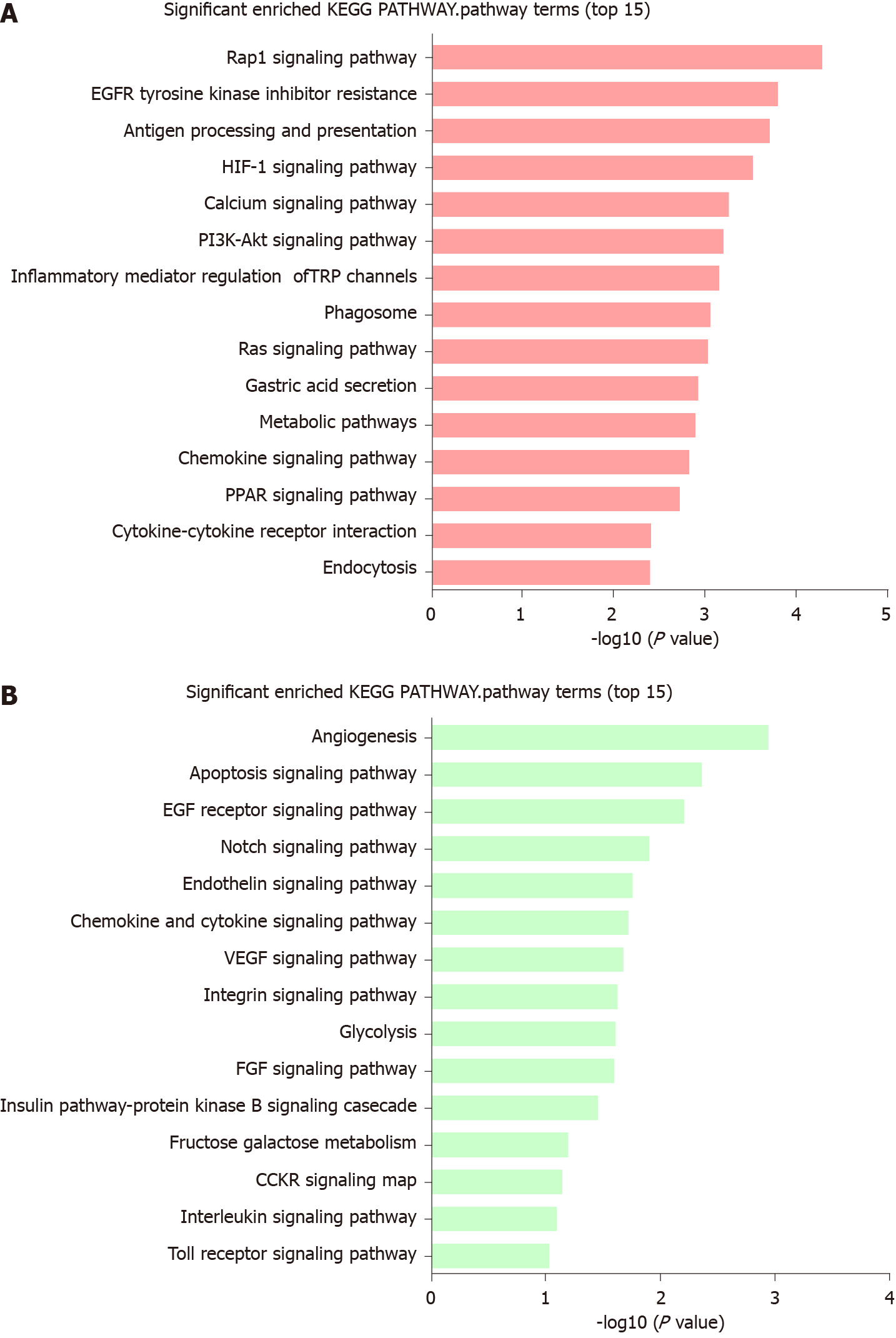
KEGG pathway enrichment analyses were performed on the differential genes. The enriched KEGG pathways (Figure 2A) for the differential genes included Rap1 signaling pathway, epidermal growth factor receptor tyrosine kinase inhibitor resistance, antigen processing and presentation, HIF-1 signaling pathway, calcium signaling pathway, PI3K-Akt signaling pathway, inflammatory mediator regulation of TRP channels, phagosome, Ras signaling pathway, gastric acid secretion, metabolic pathways, chemokine signaling pathway, peroxisome proliferator-activated receptors signaling pathway, cytokine-cytokine receptor interaction, and endocytosis. For the differential genes, the enriched PANTHER pathways (Figure 2B) included angiogenesis, apoptosis signaling pathway, epidermal growth factor receptor signaling pathway, Notch signaling pathway, endothelin signaling pathway, inflammation mediated by chemokine and cytokine signaling pathway, vascular endothelial growth factor signaling pathway, glycolysis, fibroblast growth factor signaling pathway, integrin signaling pathway, insulin/insulin like growth factor pathway-protein kinase B signaling cascade, fructose galactose metabolism, CCKR signaling map, interleukin signaling pathway, and Toll receptor signaling pathway. Both KEGG and PANTHER pathways mainly focused on immune response pathways, metabolic pathways, and metastasis-associated pathways.
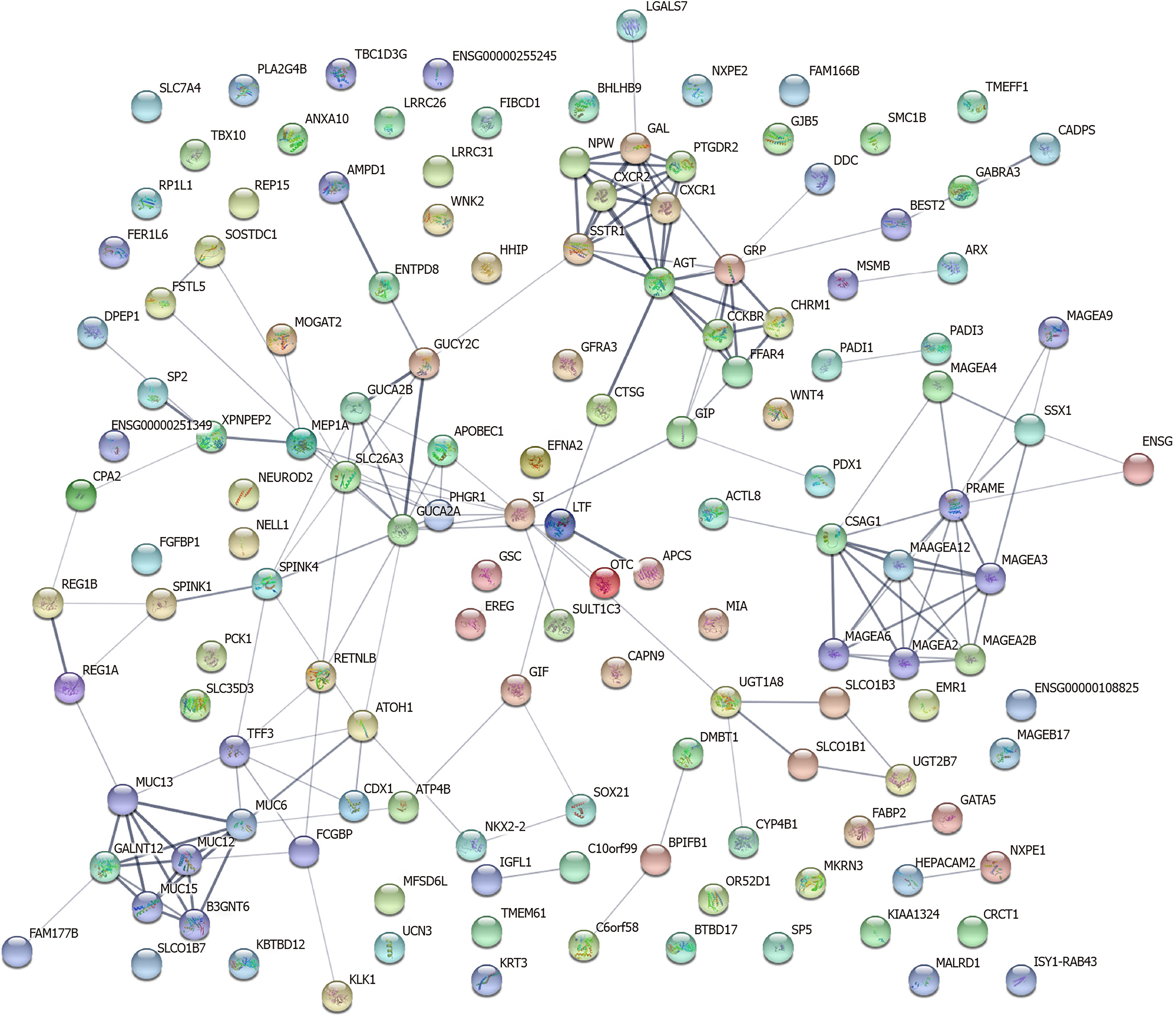
As shown in Figure 3, a regulatory network of differential genes (a 20-fold cutoff, P < 0.05) was constructed. There were 141 nodes and 171 edges among these 310 genes. The top 10 hub genes were MAGEA2, MAGEA2B, MAGEA3, MAGEA4, MAGEA6, MUC13, GUCA2A, FFAR4, REG1A, and REG1B.
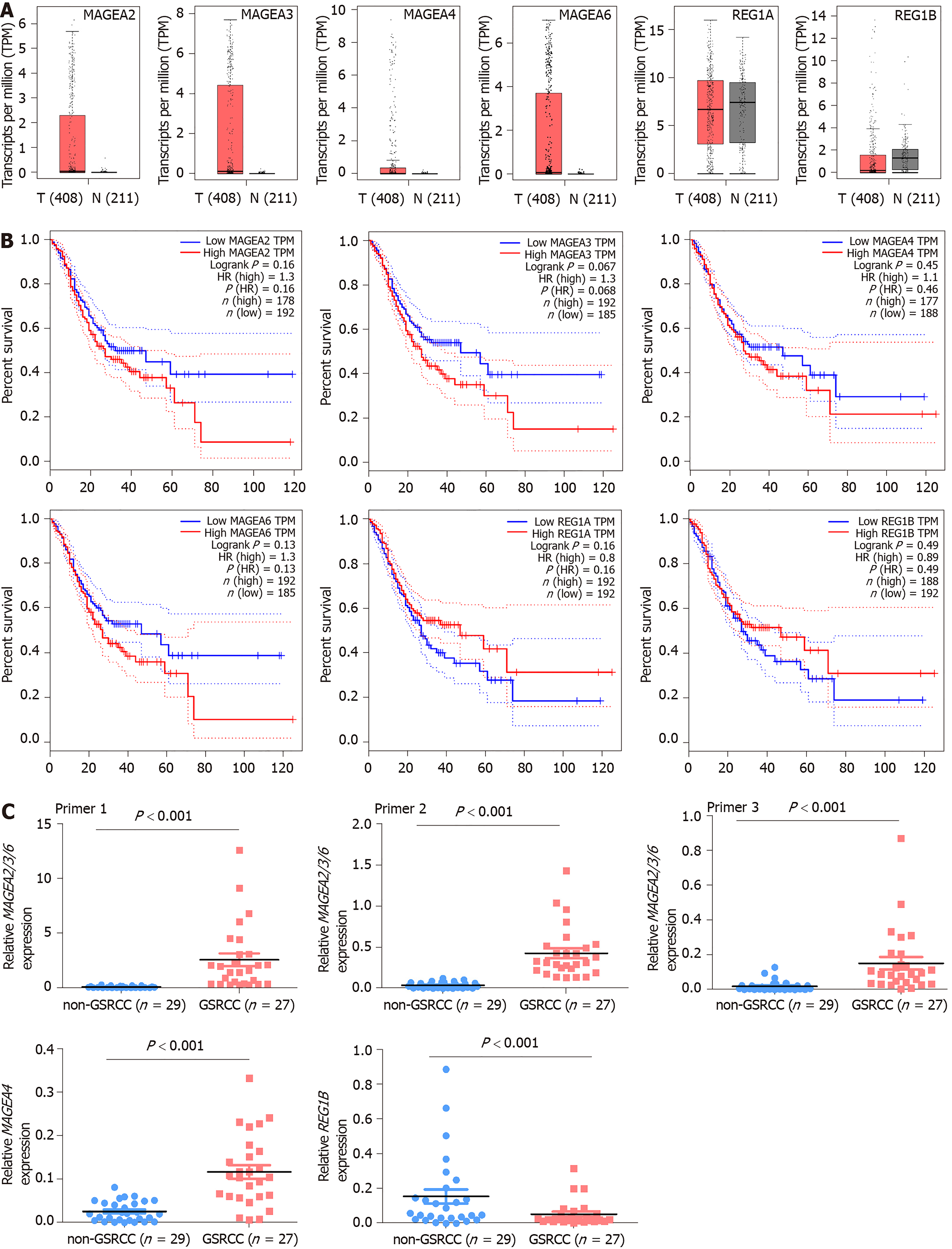
According to the difference of gene expression and pathway and the protein-protein interaction result, we chose MAGEA2, MAGEA3, MAGEA4, MAGEA6, REG1A, and REG1B for validation. The data of TCGA and GTEx (GEPIA, http://gepia.cancer-pku.cn/index.html) revealed that the expression of MAGEA2, MAGEA3, MAGEA4, and MAGEA6 was upregulated, but the expression of REG1B was downregulated, in GC compared to the normal gastric tissue, and there was no difference in REG1A between GC and normal gastric tissues (Figure 4A). The correlation analysis of gene expression and clinical data revealed a negative correlation between MAGEA2, MAGEA3, MAGEA4, and MAGEA6, but a positive correlation between REG1A and REG1B, and poor survival in patients with GC (GEPIA, http://gepia.cancer-pku.cn/index.html, Figure 4B).
To investigate the clinical value of these five genes in GC, qPCR was used to measure their expression in 27 GSRCC and 29 non-GSRCC samples. The qPCR results revealed that the expression of MAGEA2/3/6 and MAGEA4 was significantly higher, but the expression of REG1B was much lower, in patients with GSRCC than in patients with non-GSRCC (Figure 4C).
Advanced GSRCC is commonly considered to be more invasive, has a greater probability of lymph node metastasis than other gastric cancer types, has a worse prognosis[13,14], and is less sensitive to chemotherapy than non-SRCC[15-17]. Chemotherapy remains the major treatment for advanced GC. Several studies report that chemoresistance exists in GSRCC with a poor prognosis[8]. It is still unclear whether GSRCC patients can benefit from a detailed therapy.
As we know, vascular endothelial growth factor and HER-2 have been agreed as targets for molecular pathways in GC. However, SRCC cannot benefit from targeted therapy for a low expression level of HER-2[18]. Some studies have mentioned that elevated expression of PKM2 and E-cadherin, and declined expression of TMEM207 in GSRCC are associated with its biological behavior of invasion and metastasis[19].
Systematic analyses of mRNAs in GSRCC were rare. Chen et al[19] reported that hsa-miR-665 and hsa-miR-95 were found in GSRCC compared to intestinal GC, and concluded that these two mRNAs were downregulated in GSRCC but upregulated in intestinal GC, and the relatively differential expression of the miRNAs negatively regulating their target genes could be intently associated with high invasion, metastasis, and chemoresistance of GSRCC[19]. Yao et al[20] have described the genome features of GSRCC and they found the importance of highly frequent CLDN18-ARHGAP26/6 fusions in chemotherapy response in GSRCC. Kakiuchi et al[21] reported that RHOA mutations happen specifically in diffused GCs, the majority of which were pathologically characterized by the presence of poorly differentiated components, with no available molecularly targeted drugs for this poor-prognosis subtype of GC. However, that study was not specific for GSRCC. Due to a very limited number of studies in this area, this present study aimed to identify specifically expressed genes and identify biological features in GSRCC.
By pathway analyses, we confirmed frequent alterations across various pathways in GSRCC, including immunological response pathways, metabolic pathways, and metastasis-associated pathways. Further protein-protein interaction network analyses identified the hub genes in GSRCC. Of the hub genes, MAGE-A family and REG1B are immune-related genes. REG1B has been reported to be able to upregulate the expression of interleukin (IL)-6 mRNA and protein.
MAGE-A family are the best characterized cancer-testis antigens (CTA) family members, which are expressed mainly, but not exclusively, in germ cells. MAGE-A family are infrequently expressed in the normal human placenta, but they are widely expressed in numerous human cancers. Alvi et al[22] concluded that the MSI+/CIMP+/BRAF V600E+/CD3+/PDL1+ hypermethylated genotype is an ideal candidate for immune checkpoint inhibitor therapy. In addition, one-fourth of SRCC cases can potentially be targeted by KIT inhibitors. As similar as we found, MAGE-A proteins are highly immunogenic and are considered as potential targets for immuno-therapy.
In conclusion, we have identified the potential key genes and pathways in GSRCC. These hub genes and pathways could be diagnostic markers and therapeutic targets for GSRCC. MAGE-A family as a CTA family member may be the potential targets for GSRCC. More research should be conducted for exploration of the mechanisms involved.
Gastric signet ring cell carcinoma (GSRCC) has the features of high invasiveness, rapid progression, and resistance to chemotherapy. However, systematic analyses of mRNAs have not yet been performed.
The exploration of the molecular mechanism of GSRCC is important to improve the recognition of GSRCC and find the effective therapeutics to raise the survival rate of patients.
Transcriptome sequencing and comprehensive analysis were performed to identify key mRNAs and signaling pathways in GSRCC.
A transcriptome analysis of two GSRCC and two non-GSRCC samples was performed. Differentially expressed mRNAs and pathways were identified. The interactive relationships among the differential genes were mapped with the STRING database.
The enriched KEGG and PANTHER pathways for the differential genes included immune response pathways, metabolic pathways, and metastasis-associated pathways. MAGEA2, MAGEA2B, MAGEA3, MAGEA4, MAGEA6, MUC13, GUCA2A, FFAR4, REG1A, and REG1B were identified as hub genes in the protein-protein interaction network. The expression levels of MAGEA2, MAGEA3, MAGEA4, MAGEA6, and REG1B showed potential clinical value.
The potential key genes and pathways of GSRCC have been identified. These hub genes and pathways could be diagnostic markers and therapeutic targets for GSRCC.
MAGE-A family as a CTA family member may be the potential targets for GSRCC. More research should be conducted for exploration of the mechanisms involved.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim SE, Lee ST, Park SJ S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55808] [Article Influence: 7972.6] [Reference Citation Analysis (132)] |
| 2. | Taghavi S, Jayarajan SN, Davey A, Willis AI. Prognostic significance of signet ring gastric cancer. J Clin Oncol. 2012;30:3493-3498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 197] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 3. | Shu Y, Zhang W, Hou Q, Zhao L, Zhang S, Zhou J, Song X, Zhang Y, Jiang D, Chen X, Wang P, Xia X, Liao F, Yin D, Chen X, Zhou X, Zhang D, Yin S, Yang K, Liu J, Fu L, Zhang L, Wang Y, Zhang J, An Y, Cheng H, Zheng B, Sun H, Zhao Y, Wang Y, Xie D, Ouyang L, Wang P, Zhang W, Qiu M, Fu X, Dai L, He G, Yang H, Cheng W, Yang L, Liu B, Li W, Dong B, Zhou Z, Wei Y, Peng Y, Xu H, Hu J. Prognostic significance of frequent CLDN18-ARHGAP26/6 fusion in gastric signet-ring cell cancer. Nat Commun. 2018;9:2447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 4. | Hu B, El Hajj N, Sittler S, Lammert N, Barnes R, Meloni-Ehrig A. Gastric cancer: Classification, histology and application of molecular pathology. J Gastrointest Oncol. 2012;3:251-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 256] [Reference Citation Analysis (0)] |
| 5. | Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2554] [Cited by in RCA: 2428] [Article Influence: 485.6] [Reference Citation Analysis (3)] |
| 6. | Kim HW, Kim JH, Lim BJ, Kim H, Kim H, Park JJ, Youn YH, Park H, Noh SH, Kim JW, Choi SH. Sex Disparity in Gastric Cancer: Female Sex is a Poor Prognostic Factor for Advanced Gastric Cancer. Ann Surg Oncol. 2016;23:4344-4351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 7. | Ren J, Niu G, Wang X, Song T, Hu Z, Ke C. Effect of Age on Prognosis of Gastric Signet-Ring Cell Carcinoma: A SEER Database Analysis. Med Sci Monit. 2018;24:8524-8532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Pernot S, Voron T, Perkins G, Lagorce-Pages C, Berger A, Taieb J. Signet-ring cell carcinoma of the stomach: Impact on prognosis and specific therapeutic challenge. World J Gastroenterol. 2015;21:11428-11438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 178] [Cited by in RCA: 229] [Article Influence: 22.9] [Reference Citation Analysis (3)] |
| 9. | Kao YC, Fang WL, Wang RF, Li AF, Yang MH, Wu CW, Shyr YM, Huang KH. Clinicopathological differences in signet ring cell adenocarcinoma between early and advanced gastric cancer. Gastric Cancer. 2019;22:255-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 10. | Hyung WJ, Noh SH, Lee JH, Huh JJ, Lah KH, Choi SH, Min JS. Early gastric carcinoma with signet ring cell histology. Cancer. 2002;94:78-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 139] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Lemoine N, Adenis A, Bouche O, Duhamel A, Heurgue A, Leteurtre E, Amela E, Salleron J, Hebbar M. Signet Ring Cells and Efficacy of First-line Chemotherapy in Advanced Gastric or Oesogastric Junction Adenocarcinoma. Anticancer Res. 2016;36:5543-5549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Piessen G, Messager M, Le Malicot K, Robb WB, Di Fiore F, Guilbert M, Moreau M, Christophe V, Adenis A, Mariette C. Phase II/III multicentre randomised controlled trial evaluating a strategy of primary surgery and adjuvant chemotherapy versus peri-operative chemotherapy for resectable gastric signet ring cell adenocarcinomas - PRODIGE 19 - FFCD1103 - ADCI002. BMC Cancer. 2013;13:281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Lee D, Ham IH, Son SY, Han SU, Kim YB, Hur H. Intratumor stromal proportion predicts aggressive phenotype of gastric signet ring cell carcinomas. Gastric Cancer. 2017;20:591-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Liu K, Wan J, Bei Y, Chen X, Lu M. Prognostic Impact of Different Histological Types on Gastric Adenocarcinoma: a Surveillance, Epidemiology, and End Results Database Analysis. Pathol Oncol Res. 2017;23:881-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Messager M, Lefevre JH, Pichot-Delahaye V, Souadka A, Piessen G, Mariette C, FREGAT working group - FRENCH. The impact of perioperative chemotherapy on survival in patients with gastric signet ring cell adenocarcinoma: a multicenter comparative study. Ann Surg. 2011;254:684-93; discussion 693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 174] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 16. | Voron T, Messager M, Duhamel A, Lefevre J, Mabrut JY, Goere D, Meunier B, Brigand C, Hamy A, Glehen O, Mariette C, Paye F. Is signet-ring cell carcinoma a specific entity among gastric cancers? Gastric Cancer. 2016;19:1027-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Charalampakis N, Nogueras González GM, Elimova E, Wadhwa R, Shiozaki H, Shimodaira Y, Blum MA, Rogers JE, Harada K, Matamoros A, Sagebiel T, Das P, Minsky BD, Lee JH, Weston B, Bhutani MS, Estrella JS, Badgwell BD, Ajani JA. The Proportion of Signet Ring Cell Component in Patients with Localized Gastric Adenocarcinoma Correlates with the Degree of Response to Pre-Operative Chemoradiation. Oncology. 2016;90:239-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Jin S, Xu B, Yu L, Fu Y, Wu H, Fan X, Wei J, Liu B. The PD-1, PD-L1 expression and CD3+ T cell infiltration in relation to outcome in advanced gastric signet-ring cell carcinoma, representing a potential biomarker for immunotherapy. Oncotarget. 2017;8:38850-38862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Chen J, Sun D, Chu H, Gong Z, Zhang C, Gong B, Li Y, Li N, Jiang L. Screening of differential microRNA expression in gastric signet ring cell carcinoma and gastric adenocarcinoma and target gene prediction. Oncol Rep. 2015;33:2963-2971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Yao F, Kausalya JP, Sia YY, Teo AS, Lee WH, Ong AG, Zhang Z, Tan JH, Li G, Bertrand D, Liu X, Poh HM, Guan P, Zhu F, Pathiraja TN, Ariyaratne PN, Rao J, Woo XY, Cai S, Mulawadi FH, Poh WT, Veeravalli L, Chan CS, Lim SS, Leong ST, Neo SC, Choi PS, Chew EG, Nagarajan N, Jacques PÉ, So JB, Ruan X, Yeoh KG, Tan P, Sung WK, Hunziker W, Ruan Y, Hillmer AM. Recurrent Fusion Genes in Gastric Cancer: CLDN18-ARHGAP26 Induces Loss of Epithelial Integrity. Cell Rep. 2015;12:272-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 114] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 21. | Kakiuchi M, Nishizawa T, Ueda H, Gotoh K, Tanaka A, Hayashi A, Yamamoto S, Tatsuno K, Katoh H, Watanabe Y, Ichimura T, Ushiku T, Funahashi S, Tateishi K, Wada I, Shimizu N, Nomura S, Koike K, Seto Y, Fukayama M, Aburatani H, Ishikawa S. Recurrent gain-of-function mutations of RHOA in diffuse-type gastric carcinoma. Nat Genet. 2014;46:583-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 420] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 22. | Alvi MA, Loughrey MB, Dunne P, McQuaid S, Turkington R, Fuchs MA, McGready C, Bingham V, Pang B, Moore W, Maxwell P, Lawler M, James JA, Murray GI, Wilson RH, Salto-Tellez M. Molecular profiling of signet ring cell colorectal cancer provides a strong rationale for genomic targeted and immune checkpoint inhibitor therapies. Br J Cancer. 2017;117:203-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |