Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6473
Peer-review started: September 8, 2020
First decision: September 24, 2020
Revised: October 6, 2020
Accepted: November 2, 2020
Article in press: November 2, 2020
Published online: December 26, 2020
Processing time: 102 Days and 2.5 Hours
Acute arterial embolism of the extremities is a surgical emergency. Atrial fibrillation is the major etiology of acute arterial embolism of the extremities. Emergency femoral artery thrombectomy can successfully treat this issue. However, polycythemia vera (PV) may sometimes explain this medical emergency. Recurrent thrombosis in the lower extremities after thrombectomy can be found in patients with PV, and reoperation is needed for this condition.
A 68-year-old man in China suffered from sudden pain in the left lower extremity for 14 h. The examination in the emergency department showed a diagnosis of acute arterial embolism of the extremities combined with PV. The patient’s complaint disappeared after repeat emergency thrombectomy.
Patients with acute arterial embolism of the extremities should be treated carefully, especially those who have recurrent thrombosis after emergency thrombectomy. Clinicians should be aware of PV, a rare cause of acute arterial embolism of the extremities. The combination of thrombectomy, phlebotomy, and antiplatelet and anticoagulant drugs may be a suitable therapeutic regimen for these patients.
Core Tip: Acute arterial embolism of extremities is a surgical emergency. Atrial fibrillation is the major etiology, and emergency femoral artery thrombectomy is the treatment. However, polycythemia vera (PV) may sometimes explain this medical emergency. Reoperation is needed for recurrent thrombosis after thrombectomy in patients with PV. Here, a patient suffered from sudden pain of left lower extremity for 14 h. Emergency diagnosis was acute arterial embolism of extremities combined with PV. Patient’s complaint disappeared after repeated thrombectomy. Patients with PV having recurrent thrombosis after emergency thrombectomy should be treated carefully. Combination of thrombectomy, phlebotomy, and antiplatelet and anticoagulant drugs may be a suitable therapeutic regimen.
- Citation: Jiang BP, Cheng GB, Hu Q, Wu JW, Li XY, Liao S, Wu SY, Lu W. Recurrent thrombosis in the lower extremities after thrombectomy in a patient with polycythemia vera: A case report. World J Clin Cases 2020; 8(24): 6473-6479
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6473.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6473
Acute arterial embolism of the extremities is an emergent condition in the department of vascular surgery. Atrial fibrillation is the major etiology of acute arterial embolism of the extremities. Emergency femoral artery thrombectomy is the first-choice treatment. However, polycythemia vera (PV), a kind of myeloproliferative disease, may sometimes explain this medical emergency[1]. Recurrent thrombosis in the lower extremities after thrombectomy can be found in patients with PV. In this situation, reoperation is required. Here, we report an elderly man with PV who recovered from recurrent thrombosis in the lower extremities after thrombectomy. Related cases are seldomly described in the literature.
A 68-year-old man in China suffered from sudden pain in the left lower extremity for 14 h.
This patient presented a history of thrombectomy of the left femoral artery 17 years ago. Since then, his treatment has comprised an irregular course of cilostazol and beraprost sodium. He had no history of other vascular diseases, such as aortic aneurysm.
In addition, he had a history of hypertension for 7 years. During this period, he had taken irbesartan 150 mg and amlodipine besylate tablets 5 mg once a day. His blood pressure control status was unknown. He had no history of diabetes mellitus or coronary heart disease. This patient acknowledged smoking and drinking for 40 years but no drug allergies or blood transfusions.
His family members had no records of vascular diseases.
The vital signs at emergency admission showed a normal temperature, heart rate, and breathing rate, but he had a blood pressure of 173/93 mmHg. The patient looked acutely ill. The numerical rating scale (NRS) score was one. Physical examination revealed accessible bilateral femoral artery pulsation and unavailable pulsation of the dorsal artery of the left foot and left posterior tibial artery. The skin temperature of the left lower extremity was cold.
Relevant laboratory tests showed a hemoglobin level of 187 g/L, an erythrocyte count of 5.63 × 1012/L, a platelet count of 223 × 109/L, and a hematocrit value of 0.560.
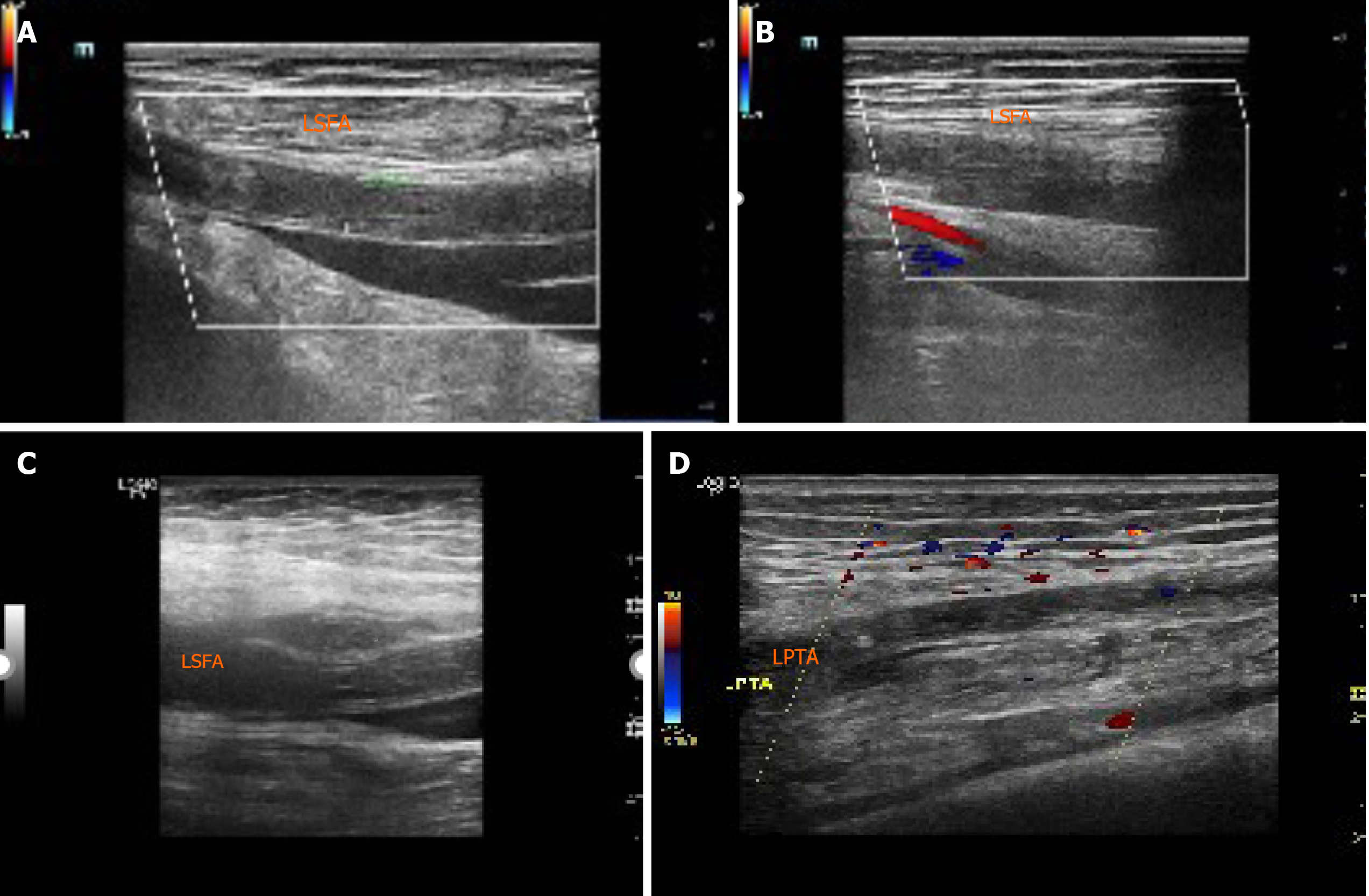
Emergency double lower extremity vascular ultrasound revealed acute occlusion of the left superficial femoral artery and left posterior tibial artery (Figure 1A and B).
In this case, according to the patient’s complaint, physical examination, laboratory tests, and ultrasonography results, the diagnosis of acute arterial embolism of the lower extremities was obviously clear. For the differential diagnosis, acute arterial thrombosis of the lower extremities should be taken into account. A study pointed out that a history of previous arterial embolism and a normal peripheral pulse on the contralateral extremity can often be found in people with acute arterial embolism of the extremities, while those with acute arterial thrombosis of the lower extremities often have a history of intermittent claudication[2].
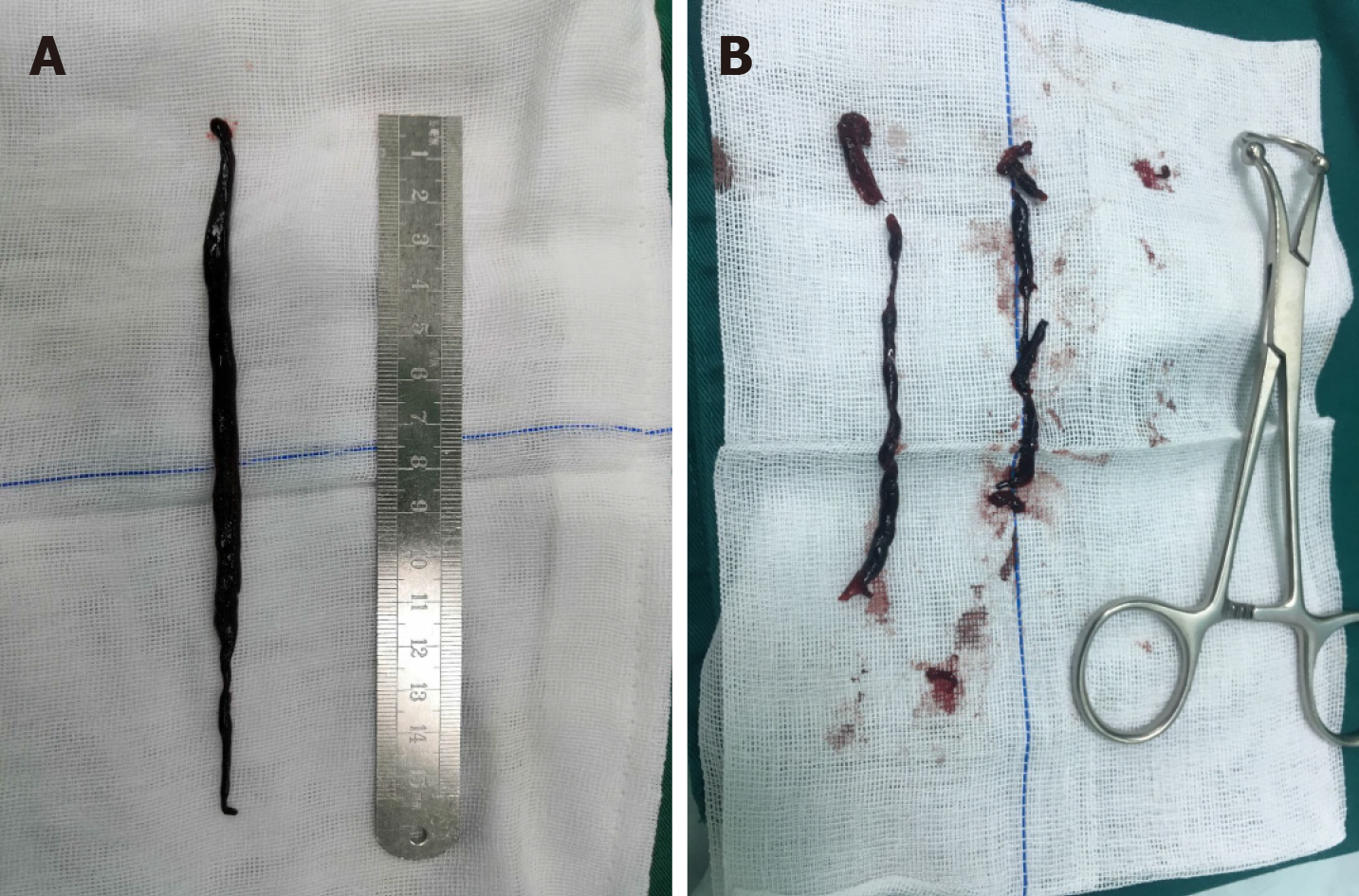
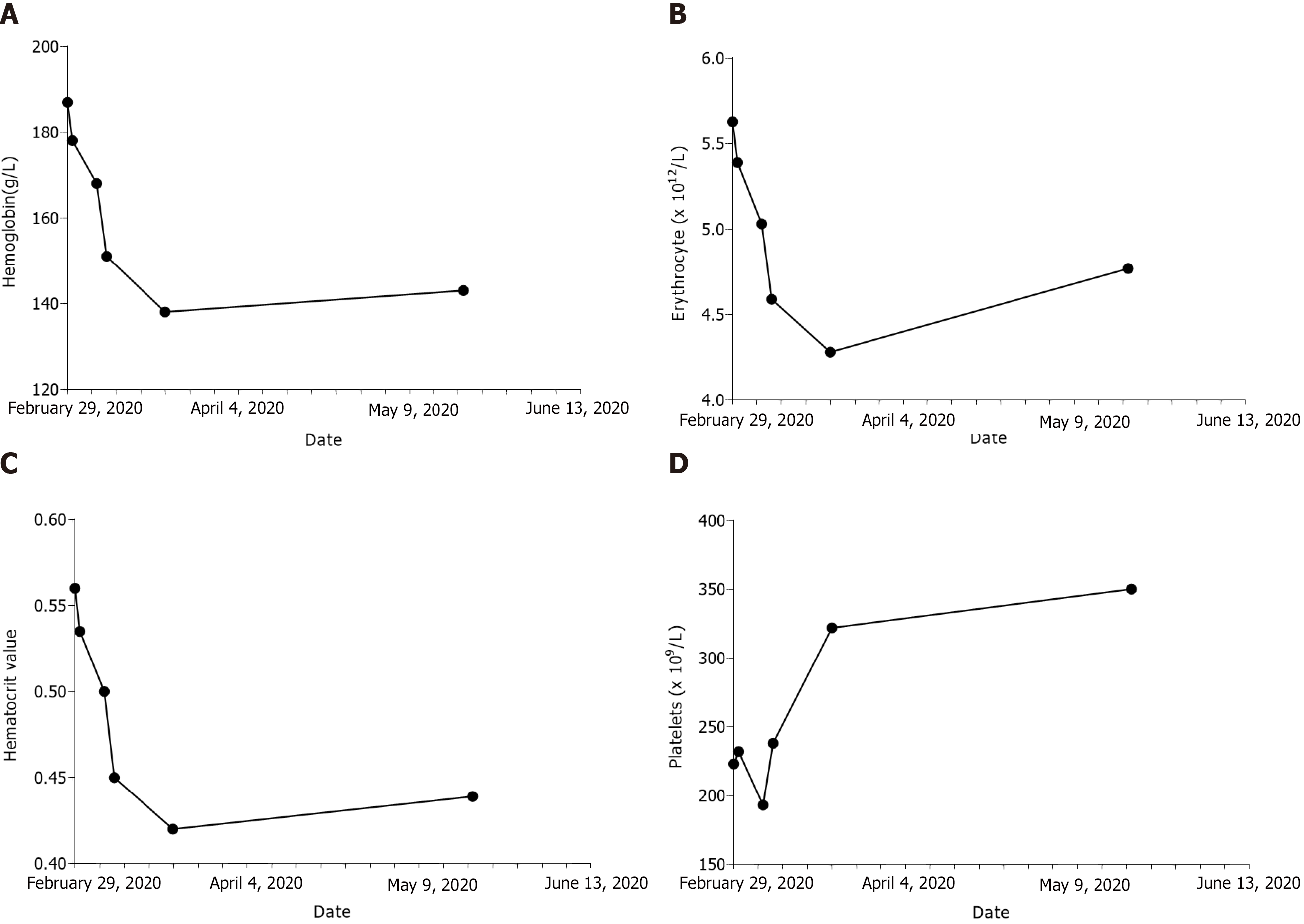
Taking limb survival into consideration, an emergency operation was performed on February 29, 2020. We used local anesthesia around the left inguinal area. A 15-cm-long thrombus was removed by 3F and 4F catheters for thrombectomy (Figure 2A). On the first day after the operation, a routine blood test revealed a high hemoglobin of 178 g/L, an erythrocyte count of 5.39 × 1012/L, a platelet count of 232 × 109/L, and a hematocrit value of 0.535. Therefore, we invited the Department of Hematology for consultation. They suggested phlebotomy therapy, bone marrow puncture, and detection of related genes by bone marrow extraction and hematopoiesis. The results were positive for a JAK2 V617F mutation. On March 6, 2020, this patient complained of pain in the left lower extremity with a NRS value of 3. An emergency double lower extremity vascular ultrasound was performed, showing occlusion of the left superficial femoral artery and posterior tibial artery (Figure 1C and D). Therefore, an urgent operation was carried out for the same purpose on March 6, 2020. A 10 cm long thrombus was completely removed (Figure 2B). On the first day after reoperation, routine blood tests revealed that hemoglobin was 168 g/L, erythrocyte was 5.03 × 1012/L, platelets were 193 × 109/L, and hematocrit was 0.500. On March 8, 2020, to avoid further emboli in the lower extremities, phlebotomy therapy was carried out. A total of 300 mL blood was released from his body. A routine blood test taken immediately was as follows: Hemoglobin 151 g/L, erythrocyte 4.59 × 1012/L, platelets 238 × 109/L, and hematocrit 0.450.
When he was discharged on March 20, 2020, his hemoglobin was 138 g/L, erythrocyte was 4.28 × 1012/L, platelet was 322 × 109/L, and hematocrit was 0.420, and both legs were warm. Two months later, he returned to our hospital for re-examination and presented a hemoglobin level of 143 g/L, an erythrocyte level of 4.77 × 1012/L, and a platelet level of 350 × 109/L with a hematocrit of 0.439 (Table 1). He temporarily refused, however, further examination of ultrasound and computed tomography angiography of lower extremity arteries. Until now, he took a regular course of 100 mg of aspirin and 10 mg of rivaroxaban every day, and no hemorrhage events happened during this course.
| Date | Item | Laboratory test indicators | Clinical intervention | |||
| Hemoglobin, g/L | Erythrocyte, × 1012/L | Hematocrit value | Platelets, × 109/L | |||
| February 29, 2020 | Admission | 187 | 5.63 | 0.560 | 223 | First emergency operation |
| March 1, 2020 | Recheck of blood | 178 | 5.39 | 0.535 | 232 | Hematology consultation |
| March 6, 2020 | Hospitalization | 168 | 5.03 | 0.500 | 193 | Second emergency operation |
| March 8, 2020 | Hospitalization | 151 | 4.59 | 0.450 | 238 | Phlebotomy therapy |
| March 20, 2020 | Discharged | 138 | 4.28 | 0.420 | 322 | Start of follow-up |
| May 20, 2020 | Follow-up | 143 | 4.77 | 0.439 | 350 | Aspirin, 100 mg qd + rivashaban, 10 mg qd |
Generally, acute arterial embolism of the lower extremity is a common vascular surgical condition. Atrial fibrillation is often believed to give rise to this complication[3]. Once diagnosed, surgery should be performed as soon as possible if the patient’s condition allows. When surgeons encounter these patients, emergency surgery must be carried out immediately within 6-8 h to rescue limbs on the verge of necrosis. A study revealed that patients may still benefit from surgery if the ischemia time of the extremities is no longer than 24 h[4]. However, recurrent arterial embolism caused by PV, a myeloproliferative disease, is rarely reported.
PV is a typical kind of hematological system disease. Epidemiology shows that the morbidity of PV ranges from 1 to 40 persons per million people. The age at diagnosis is often older than 60 years[5]. Arterial embolism can be an initial symptom of PV[6]. These emboli can appear anywhere in the body, such as the brain, eyes, mesenteric vessels, and extremities. The most common site in the extremities is the common femoral artery[7]. Inpatient examination often reveals increased blood viscosity and a relevant mutant gene named JAK2 V617F. From our point of view, this situation was very likely caused by the thickened blood, which is in accordance with Virchow’s triad. The National Comprehensive Cancer Network guidelines recommend phlebotomy as treatment for PV[8]. One study pointed out that the target hematocrit is less than 0.450 for phlebotomy in patients with PV[9]. Our treatment achieved this goal very well (Figure 3).
This case is special in several aspects. First, acute arterial embolism of the extremities caused by PV is uncommon. Second, recurrent thrombosis in the lower extremities after thrombectomy in a patient with PV is seldom and rare. Notably, our center’s repeated thrombectomy procedure proved to be successful. Finally, in future clinical work, patients diagnosed with recurrent acute arterial embolism of the lower extremity should be vigilant against PV. If possible, routine consultations of the hematology department are necessary. Once diagnosed, the regular use of antiplatelet drugs, such as aspirin, is also important in patients with PV[10].
The limitations in this case were as follows: We did not invited the Department of Hematology for consultation before operation, and phlebotomy therapy was ignored during operation. We must avoid the same mistakes in our future clinical work.
Patients with acute arterial embolism of the extremities should be treated carefully, especially those who have recurrent thrombosis after emergency thrombectomy. Clinicians should be aware of PV, a rare cause of acute arterial embolism of the extremities. The combination of thrombectomy, phlebotomy, and antiplatelet and anticoagulant drugs may be a suitable therapeutic regimen for these patients.
We thank the colleagues, the platform, and the nursing team in our center.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Suppiah A S-Editor: Chen XF L-Editor: Filipodia P-Editor: Wang LL
| 1. | Ahmed AK, Youssef A, Skeik N. Medical Management of Extensive Arterial Thromboembolism in a Patient with Essential Thrombocythemia and Warfarin Failure. Ann Vasc Surg 2017; 42: 306.e5-306. e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Mutirangura P, Ruangsetakit C, Wongwanit C, Sermsathanasawadi N, Chinsakchai K. Clinical differentiation between acute arterial embolism and acute arterial thrombosis of the lower extremities. J Med Assoc Thai. 2009;92:891-897. [PubMed] |
| 3. | Ueberrueck T, Marusch F, Schmidt H, Gastinger I. Risk factors and management of arterial emboli of the upper and lower extremities. J Cardiovasc Surg. 48:181-186. [PubMed] |
| 4. | Mutirangura P, Ruangsetakit C, Wongwanit C, Sermsathanasawadi N, Chinsakchai K. Acute arterial embolism of the lower extremities: impact of 24-hour duration on the outcome of management. J Med Assoc Thai. 2008;91:1360-1367. [PubMed] |
| 5. | Parnes A, Ravi A. Polycythemia and Thrombocytosis. Prim Care. 2016;43:589-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Griesshammer M, Kiladjian JJ, Besses C. Thromboembolic events in polycythemia vera. Ann Hematol. 2019;98:1071-1082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 7. | Vrtík L, Zernovický F, Kubis J, Simo JD, Matis P. [Arterial embolisms in the extremities]. Rozhl Chir. 2001;80:465-469. [PubMed] |
| 8. | Mesa RA, Jamieson C, Bhatia R, Deininger MW, Fletcher CD, Gerds AT, Gojo I, Gotlib J, Gundabolu K, Hobbs G, McMahon B, Mohan SR, Oh S, Padron E, Papadantonakis N, Pancari P, Podoltsev N, Rampal R, Ranheim E, Reddy V, Rein LAM, Scott B, Snyder DS, Stein BL, Talpaz M, Verstovsek S, Wadleigh M, Wang ES, Bergman MA, Gregory KM, Sundar H. NCCN Guidelines Insights: Myeloproliferative Neoplasms, Version 2.2018. J Natl Compr Canc Netw. 2017;15:1193-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 9. | Barbui T, Passamonti F, Accorsi P, Pane F, Vannucchi AM, Velati C, Gale RP, Tura S, Barosi G. Evidence- and consensus-based recommendations for phlebotomy in polycythemia vera. Leukemia. 2018;32:2077-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Squizzato A, Romualdi E, Passamonti F, Middeldorp S. Antiplatelet drugs for polycythaemia vera and essential thrombocythaemia. Cochrane Database Syst Rev. 2013;(4):CD006503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |