Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6456
Peer-review started: September 4, 2020
First decision: September 30, 2020
Revised: October 11, 2020
Accepted: October 26, 2020
Article in press: October 26, 2020
Published online: December 26, 2020
Processing time: 106 Days and 2.3 Hours
Mucosa-associated lymphoid tissue (MALT) lymphoma is a subtype of non-Hodgkin lymphoma that is mainly involved in the gastrointestinal tract. The synchronous occurrence of colonic MALT lymphoma and adenocarcinoma in the same patient is extremely rare. We here report a case of synchronous colonic MALT lymphoma found on surveillance colonoscopy five months after surgery and chemotherapy for sigmoid adenocarcinoma.
A 67-year-old man was admitted because of hematochezia for two months. Colonoscopy suggested a colonic tumor before hospitalization. Abdominal computed tomography (CT) revealed local thickening of the sigmoid colon. The patient underwent a left hemicolectomy with local lymph node dissection. The histopathology revealed moderately differentiated adenocarcinoma and partially mucinous adenocarcinoma. The pTNM stage was T3N1Mx. The patient received chemotherapy with six cycles of mFOLFOX6 after surgery. Colonoscopy was performed five months later and revealed single, flat, polypoid lesions of the colon 33 cm away from the anus. Subsequently, the patient underwent endoscopic mucosal resection for further diagnosis. The pathological diagnosis was MALT lymphoma. Positron emission tomography /CT suggested metastasis. The patient refused further treatment and died ten months later.
Colonic MALT lymphoma may occur after surgery and chemotherapy for adenocarcinoma as a synchronous malignancy. Regular surveillance colonoscopy and careful monitoring after surgery are critical.
Core Tip: The synchronous occurrence of colonic mucosa-associated lymphoid tissue (MALT) lymphoma and adenocarcinoma in the same patient is extremely rare. Few cases have been reported in the literature to date. Colonic MALT lymphoma is often asymptomatic and found on surveillance colonoscopy. When it presents synchronously with colonic adenocarcinoma, MALT lymphoma is easily missed. Regular surveillance colonoscopy and careful monitoring after surgery are critical. We report a case of synchronous colonic MALT lymphoma found on surveillance colonoscopy five months after surgery and chemotherapy for sigmoid adenocarcinoma.
- Citation: Li JJ, Chen BC, Dong J, Chen Y, Chen YW. Synchronous colonic mucosa-associated lymphoid tissue lymphoma found after surgery for adenocarcinoma: A case report and review of literature. World J Clin Cases 2020; 8(24): 6456-6464
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6456.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6456
Mucosa-associated lymphoid tissue (MALT) lymphoma, also known as extranodal marginal zone lymphoma, is a subtype of non-Hodgkin lymphoma (NHL)[1,2]. MALT lymphoma is the third most frequent histologic subtype, accounting for approximately 7% - 8% of all NHLs[3]. MALT lymphoma may arise anywhere outside the lymph nodes, predominantly involving the gastrointestinal (GI) tract and other areas, such as the ocular adnexa, salivary glands, thyroid, skin, lungs, and breast. MALT lymphoma occurring in the GI tract is found mainly in the stomach, accounting for more than half of all cases, followed by MALT lymphomas in the small intestine, cecum, and colorectum[4]. The synchronous occurrence of colonic MALT lymphoma and adenocarcinoma in the same patient is extremely rare[5-7]. Only one case of synchronous colonic MALT lymphoma diagnosed after hemicolectomy due to adenocarcinoma within six months has been reported in the literature to date[8]. We here report a case of synchronous colonic MALT lymphoma found on surveillance colonoscopy five months after surgery and chemotherapy for sigmoid adenocarcinoma.
A previously healthy 67-year-old man presented with hematochezia for two months.
The patient had hematochezia for two months. His stool was dark red and bloody, occasionally pale pink in color, but the blood was not mixed with the stool; thinning of the stool was also observed. He occasionally had abdominal distension but no abdominal pain, nausea, vomiting, diarrhea, or fever. Colonoscopy at a local hospital suggested a sigmoid tumor.
The patient had no history of hypertension, heart disease, diabetes, smoking or drinking. He denied a history of surgery.
The patient denied a relevant family history.
The physical examination was unremarkable.
His hemoglobin level was 144 g/L. The blood biochemistry and coagulation function results were normal. Anti-human immunodeficiency virus (HIV) and anti-hepatitis C virus testing was negative. The carcinoembryonic antigen level was 6.7 μg/L, while the carbohydrate antigen 19-9 level was 39.0 U/mL. A fecal occult blood test was mildly positive.
Abdominal computed tomography (CT) revealed local thickening of the sigmoid colon.
The diagnosis was synchronous colonic MALT lymphoma following surgery and chemotherapy for sigmoid adenocarcinoma.
The patient underwent left hemicolectomy with local lymph node dissection. The histopathology revealed moderately differentiated adenocarcinoma and partially mucinous adenocarcinoma, and the macroscopic classification was the ulcerative type. The size of the mass was 3.3 cm × 3.0 cm × 1.0 cm, and the mass involved the serosal layer. Additionally, vascular and nerve involvement was observed. There was involvement of the pericolic lymph nodes (1/6) but no involvement of the mesenteric lymph nodes (0/6). Metastatic carcinomas were found in the abdominal cavity. The diameters of the three metastatic tumors were 0.2- 1.0 cm. Immunohistochemical staining showed that the tumor cells were positive for Ki67 (80% positive), CD34 (vascular), D2-40 (lymphatic), PMS2, MSH2, MSH6, MLH1, CDX2, E-cadherin, EGFR, CK20, and CK (pan) but negative for CK7 and p53. The final pTNM stage was T3N1Mx.
The patient received chemotherapy with six cycles of mFOLFOX6 (calcium folinate (0.6 g), fluorouracil (0.6 g), and oxaliplatin (130 mg) after surgery.
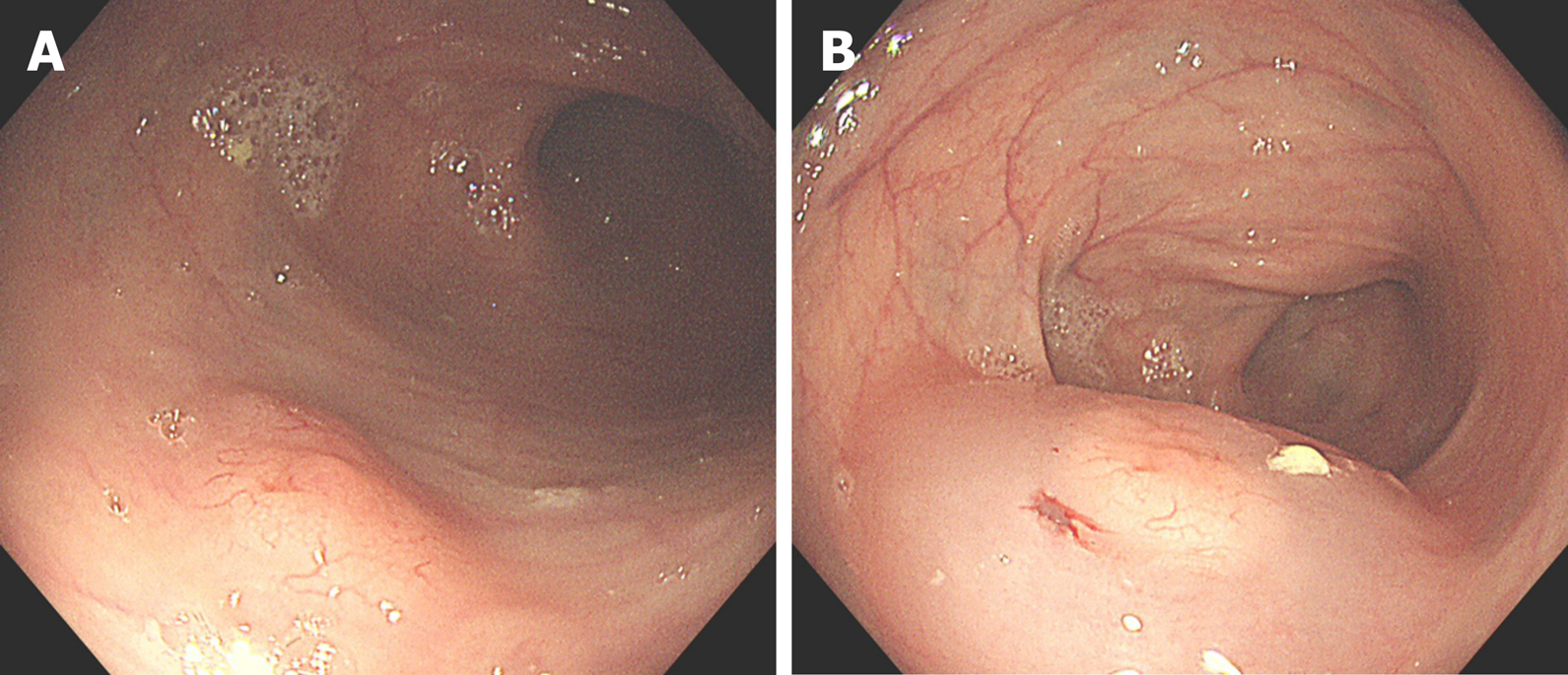
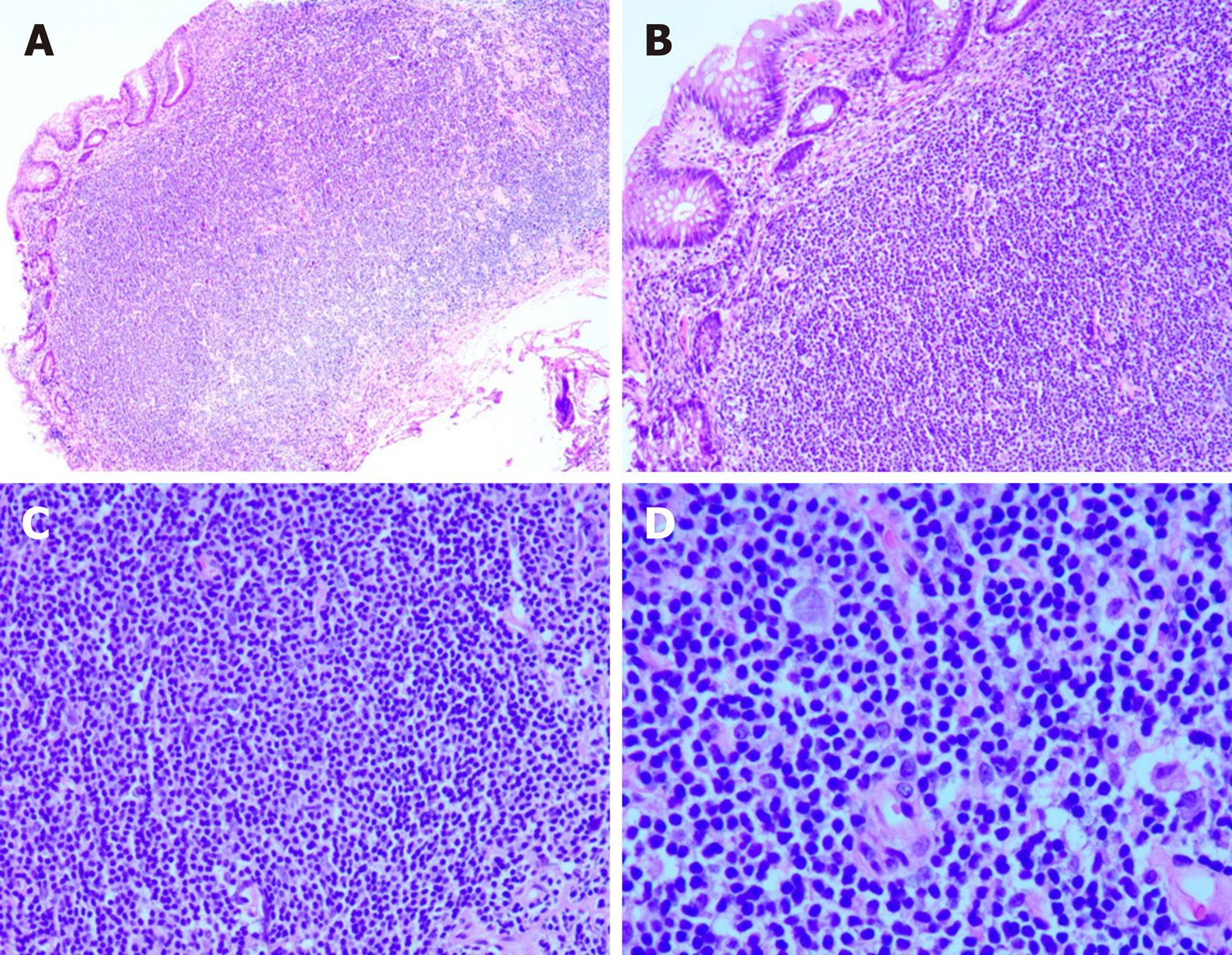
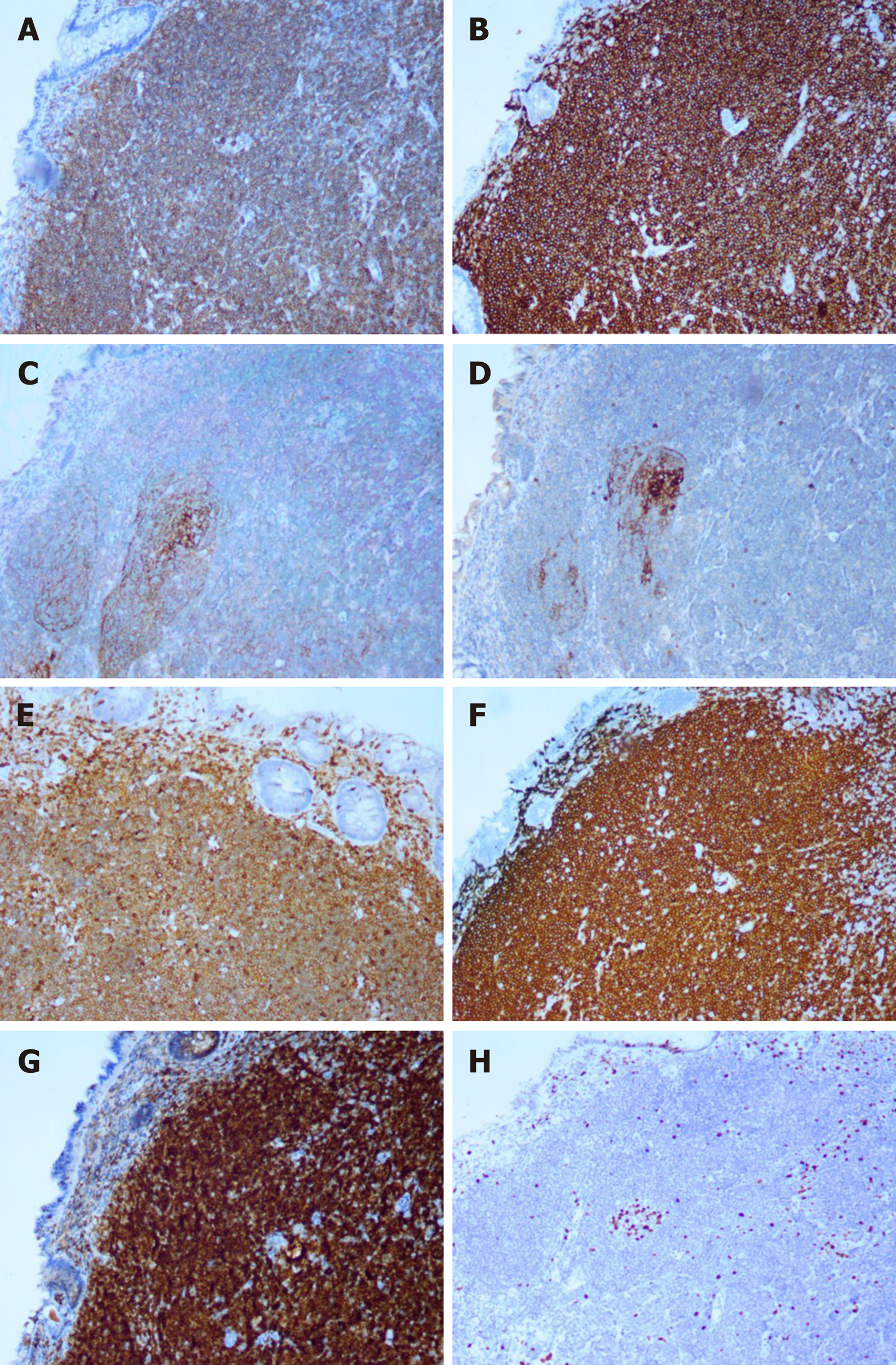
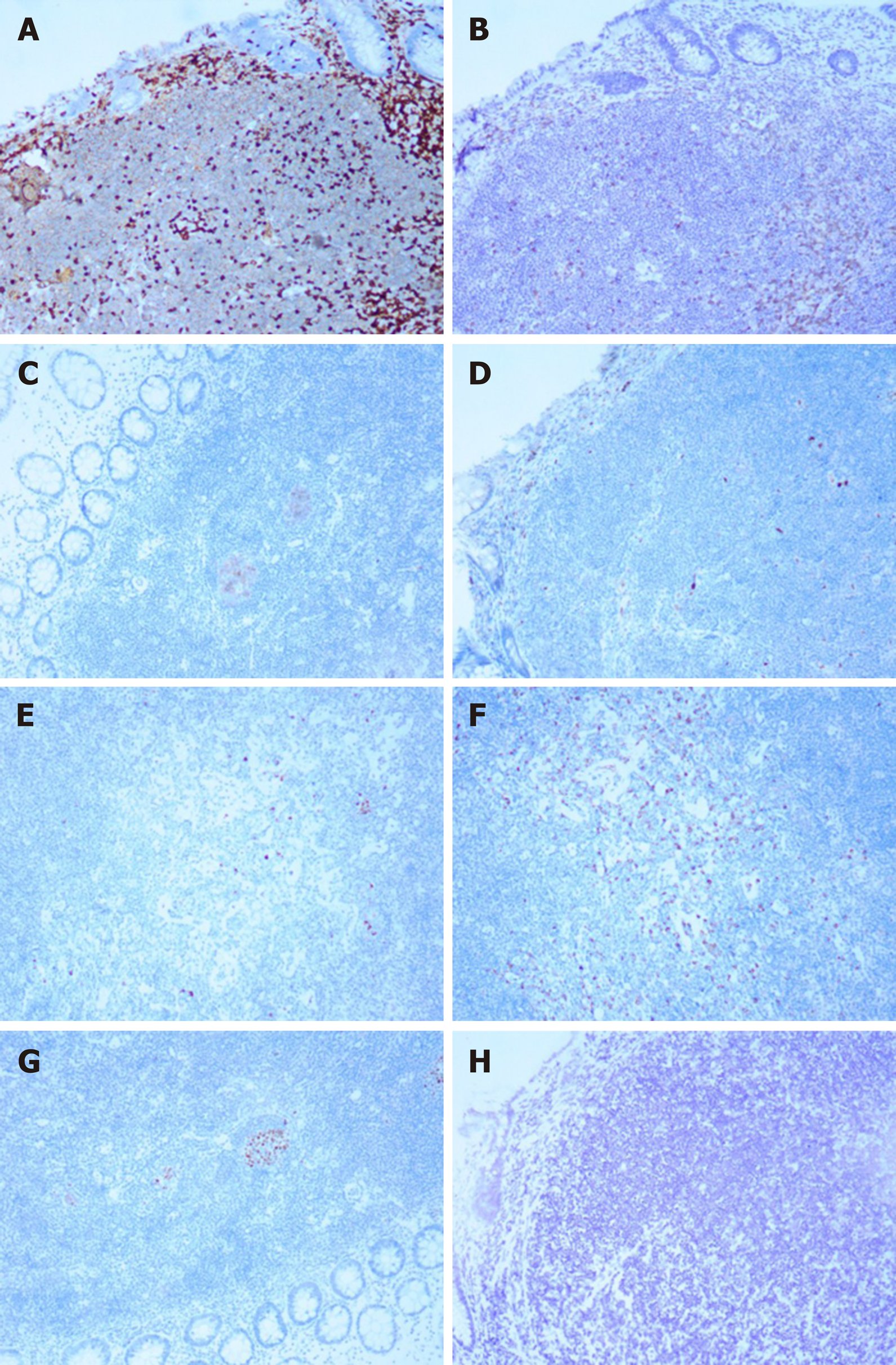
Colonoscopy was performed five months after surgery. Colonoscopy revealed a single, flat, 1.2 cm × 0.8 cm polypoid lesion of the colon 33 cm from the anus (Figure 1). The size was approximately 1.0 cm in diameter. Subsequently, the patient underwent endoscopic mucosal resection for further diagnosis. Microscopically, hematoxylin and eosin staining showed lymphoid hyperplasia (Figure 2). Immunohistochemical staining showed that the tumor cells were positive for CD19, CD20, CD21 and CD23 (dendritic cells), as well as CD43, CD79a, BCL-2, and Ki67 (10% positive) (Figure 3), but negative for CD3, CD5, CD10, Cyclin D1, Kappa, Lambda, BCL-6, and EBER (Figure 4). Molecular detection of EBER was also negative. The final pathological diagnosis was MALT lymphoma.
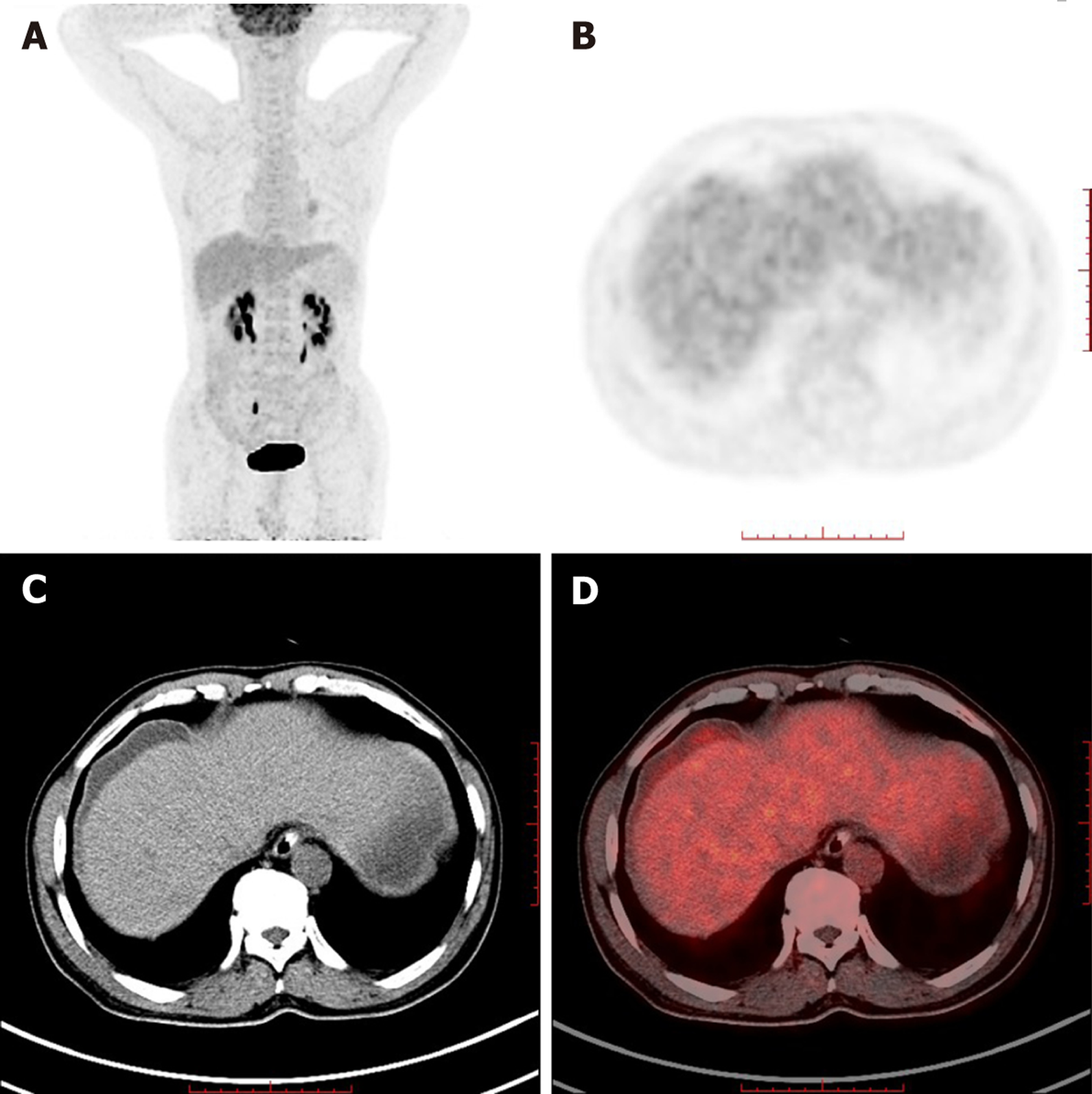
To confirm whether distant metastasis occurred, 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) was performed. PET/CT demonstrated subcapsular effusion in the liver with increased FDG metabolism; the upper right area of the peritoneum was slightly thickened and had slightly increased FDG metabolism (Figure 5). These results suggested metastasis.
The patient refused further treatment because of the suspicion of metastasis and died ten months later due to tumor metastasis.
To the best of our knowledge, our case is the one of the few ever reported concerning synchronous colonic MALT lymphoma found on surveillance colonoscopy after hemicolectomy for colonic adenocarcinoma.
Any second malignancy in a patient with an existing malignancy is classified as either synchronous or metachronous. According to the definition of Gluckman[9], synchronous malignancies include malignancies that are present either simultaneously or within six months of the original tumor diagnosis. Malignancies diagnosed beyond the six-month interval are referred to as metachronous. Our case met the definition of a synchronous malignancy.
MALT lymphoma, first described in 1983[10], was classified as an extranodal marginal zone B cell lymphoma by the World Health Organization in 2008[2]. MALT lymphoma may arise anywhere outside the lymph node and has cellular immunophenotypic features that are similar to those of lymphomas in other areas, predominantly affecting the GI tract as well as the ocular adnexa, salivary gland, thyroid, skin, lung, and breast[4,11]. The stomach is the most common site of MALT lymphoma in the GI tract, accounting for 60% - 75% of all cases, followed by MALT lymphomas of the small intestine, ileum, cecum, and colorectum[4]. Although the incidence of gastrointestinal lymphoma is increasing[12], primary colonic MALT lymphoma remains a rare disease, accounting for less than 5% of GI lymphomas[13] and less than 1% of all colorectal malignancies[14].
The causative factor of colonic MALT lymphoma remains unclear. An important causative factor is antigen-specific lymphoproliferation. Chronic antigenic stimulation by either microbial pathogens (e.g., Helicobacter pylori, Chlamydia psittaci, and Borrelia burgdorferi) or autoantigens (e.g., the antigens found in Hashimoto's thyroiditis and Sjögren's syndrome) indirectly determines the risk of involvement of specific mucosal sites in primary MALT lymphoma[15].
Colonic MALT lymphoma affects mainly adults in their fifth to seventh decades of life[4,16]. The mean age at presentation is 60 years[16]. The sex bias ranges from almost nonexistent to a 2:1 female predominance[16-18]. Approximately half of the patients are asymptomatic, with the disease discovered on surveillance colonoscopy[16,19]. Moreover, the cancer can present with diarrhea, constipation, mucoid stool, hematochezia, abdominal or epigastric pain, weight loss[19,20], GI bleeding[21], a palpable mass[19], intussusception[22], or acute intestinal obstruction[23].
MALT lymphoma of the colorectum may show variable presentations on endoscopy. Subepithelial tumors, polyposis, epithelial masses, and ileitis are the four distinct types of endoscopic appearances[16]. Single or multiple lesions may be flat, elevated, polypoid or semipedunculated, with the surface smooth, eroded, granular or nodular[17]. The size varies from millimeters to 4-5 centimeters[4,20,24]. Chromoendoscopy and narrow-band imaging may improve the detection and border delineation of colorectal MALT lymphoma[25].
Monocytoid B cells, centrocyte-like cells and small lymphocytes are the main cell types in MALT lymphoma, sometimes accompanied by cells with plasmacytoid differentiation, scattered immunoblasts and transformed centroblast-like cells[17]. The atypical cell population may exist in the mucosa or submucosa and even the muscularis propria of the colon[17]. Immunophenotypically, colonic MALT lymphomas coexpress B-cell markers, such as CD19, CD20 and CD79a, but are typically negative for CD5, CD10, CD23, and Cyclin D1[26]. Some also show CD5 reactivity[17], and the Ki67 proliferation rate is usually low[19]. Recurrent cytogenetic abnormalities in MALT lymphomas include mainly the t(1;14)(p22;q32), t(11;18)(q21;q21) and t(14;18)(q32;q21) translocations, which may affect the nuclear factor kappa light chain-enhancer of activated B cells (NF-κB) pathway, and trisomies of chromosomes 3 and 18[2,17,27].
To date, standardized treatments for colonic MALT lymphoma are lacking since the disease is relatively rare. The common therapies include surgical resection (partial colectomy), endoscopic resection, radiotherapy, chemotherapy, immune therapy (such as rituximab) and antibiotics in varying combinations[16,18,19,28,29]. The relationship between colonic MALT lymphoma and Helicobacter pylori (H. pylori) infection remains unclear[30]. However, the tumor may regress after H. pylori eradication[31]. Because of the indolence of colorectal MALT lymphoma, a "watch and wait" approach may be suggested in patients who are asymptomatic or who have minimally apparent disease on colonoscopy[29]. Colonic MALT lymphoma has a good prognosis with low recurrence[17]. The 5-year progression-free survival is 92%, while the overall survival is 94%. The disease-specific survival is 98% at five years[16].
The relationship between colonic MALT lymphoma and adenocarcinoma is unknown. Colonic MALT lymphoma was found to be a metachronous malignancy in a patient who had undergone hemicolectomy for a prior colon adenocarcinoma[32]. Very few cases have been reported on synchronous colonic MALT lymphoma and adenocarcinoma simultaneously present in the same patient[5-7]. Synchronous adenocarcinoma and MALT lymphomas may exist in the same tumor[5-7], which is also called a collision tumor. Some synchronous colonic adenocarcinomas are accompanied by MALT lymphoma in the lymph nodes and omentum[6]. Only one case has been reported in which a diagnosis of synchronous MALT lymphoma was made at the second surgery one month after the diagnosis of colonic adenocarcinoma, which was treated with right hemicolectomy[8]. In our case, the MALT lymphoma found on surveillance colonoscopy five months after surgery and chemotherapy for sigmoid adenocarcinoma occurred neither at the same time nor in the same segment of the colon. Immune-mediated diseases, such as Hashimoto's thyroiditis, Sjögren's syndrome, and inflammatory bowel disease, might be risk factors for colonic MALT lymphoma[15,33,34], as well as immunodeficiency factors, such as HIV, steroid use, and tuberculosis[5,35]. Therefore, colonic MALT lymphoma found after surgery and chemotherapy for adenocarcinoma may result from immunosuppression. However, additional research is needed to confirm this hypothesis.
There were limitations in this report. When colonic MALT lymphoma is diagnosed, synchronous malignancy should be excluded. Gastroscopy, bone marrow biopsy, and CT of the thorax and abdomen should be included for tumor staging[18]. In this case, the patient refused further examination and treatment because of the coexistence of advanced-stage colonic adenocarcinoma. Thus, he did not undergo gastroscopy or bone marrow biopsy.
We report an extremely rare case of synchronous colonic MALT lymphoma found on surveillance colonoscopy five months after surgery and chemotherapy for sigmoid adenocarcinoma. Colonic MALT lymphoma is often asymptomatic and found on surveillance colonoscopy. When presenting synchronously with colonic adenocarcinoma, MALT lymphoma is easily missed. Regular surveillance colonoscopy and careful monitoring after surgery are critical.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Srinivasamurthy B S-Editor: Gao CC L-Editor: MedE-Ma JY P-Editor: Zhang YL
| 1. | Psyrri A, Papageorgiou S, Economopoulos T. Primary extranodal lymphomas of stomach: clinical presentation, diagnostic pitfalls and management. Ann Oncol. 2008;19:1992-1999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Jaffe ES, Swerdlow SH CE, Campo E, Pileri S, Thiele J, Stein HT, Harris NL, Wardiman JW. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon, France: IARC Press, 2008. |
| 3. | A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood. 1997;89:3909-3918. [PubMed] |
| 4. | Abbas H, Niazi M, Makker J. Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma of the Colon: A Case Report and a Literature Review. Am J Case Rep. 2017;18:491-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Velu AR, Srinivasamurthy BC, Nagarajan K, Sinduja I. Colonic adenocarcinoma, mucosa associated lymphoid tissue lymphoma and tuberculosis in a segment of colon: A case report. World J Gastrointest Oncol. 2014;6:377-380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Argyropoulos T, Foukas P, Kefala M, Xylardistos P, Papageorgiou S, Machairas N, Boltetsou E, Machairas A, Panayiotides IG. Simultaneous occurrence of colonic adenocarcinoma and MALT lymphoma: A series of three cases. World J Gastrointest Oncol. 2012;4:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Devi P, Pattanayak L, Samantaray S. Synchronous adenocarcinoma and mucosa-associated lymphoid tissue lymphoma of the colon. Saudi J Gastroenterol. 2011;17:69-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Moriya Y, Koyama Y, Minato K, Shimoyama M, Hirota T, Itabashi M. [Coexisting malignant lymphoma and advanced adenocarcinoma of the colon--a case report]. Gan No Rinsho. 1985;31:894-899. [PubMed] |
| 9. | Gluckman JL, Crissman JD, Donegan JO. Multicentric squamous-cell carcinoma of the upper aerodigestive tract. Head Neck Surg. 1980;3:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 111] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 11. | Isaacson PG, Du MQ. MALT lymphoma: from morphology to molecules. Nat Rev Cancer. 2004;4:644-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 322] [Article Influence: 15.3] [Reference Citation Analysis (1)] |
| 12. | Howell JM, Auer-Grzesiak I, Zhang J, Andrews CN, Stewart D, Urbanski SJ. Increasing incidence rates, distribution and histological characteristics of primary gastrointestinal non-Hodgkin lymphoma in a North American population. Can J Gastroenterol. 2012;26:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, Grothaus-Pinke B, Reinartz G, Brockmann J, Temmesfeld A, Schmitz R, Rübe C, Probst A, Jaenke G, Bodenstein H, Junker A, Pott C, Schultze J, Heinecke A, Parwaresch R, Tiemann M; German Multicenter Study Group. Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001;19:3861-3873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 270] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 14. | Stanojevic GZ, Nestorovic MD, Brankovic BR, Stojanovic MP, Jovanovic MM, Radojkovic MD. Primary colorectal lymphoma: An overview. World J Gastrointest Oncol. 2011;3:14-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 15. | Suarez F, Lortholary O, Hermine O, Lecuit M. Infection-associated lymphomas derived from marginal zone B cells: a model of antigen-driven lymphoproliferation. Blood. 2006;107:3034-3044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 303] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 16. | Jeon MK, So H, Huh J, Hwang HS, Hwang SW, Park SH, Yang DH, Choi KD, Ye BD, Myung SJ, Yang SK, Byeon JS. Endoscopic features and clinical outcomes of colorectal mucosa-associated lymphoid tissue lymphoma. Gastrointest Endosc. 2018;87:529-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Hollie N, Asakrah S. MALT lymphoma of the colon: a clinicopathological review. J Clin Pathol. 2020;73:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Won JH, Kim SM, Kim JW, Park JH, Kim JY. Clinical features, treatment and outcomes of colorectal mucosa-associated lymphoid tissue (MALT) lymphoma: literature reviews published in English between 1993 and 2017. Cancer Manag Res. 2019;11:8577-8587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Kim MH, Jung JT, Kim EJ, Kim TW, Kim SY, Kwon JG, Kim EY, Sung WJ. A case of mucosa-associated lymphoid tissue lymphoma of the sigmoid colon presenting as a semipedunculated polyp. Clin Endosc. 2014;47:192-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Akasaka R, Chiba T, Dutta AK, Toya Y, Mizutani T, Shozushima T, Abe K, Kamei M, Kasugai S, Shibata S, Abiko Y, Yokoyama N, Oana S, Hirota S, Endo M, Uesugi N, Sugai T, Suzuki K. Colonic mucosa-associated lymphoid tissue lymphoma. Case Rep Gastroenterol. 2012;6:569-575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Kanneganti K, Balar B. Mucosa-associated lymphoid tissue lymphoma presenting as massive gastrointestinal bleeding: a case report. Case Rep Gastroenterol. 2008;2:296-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Adams KM, Roe NM. A Rare Case of MALT Lymphoma Underlying Ileocecal Intussusception. J Am Osteopath Assoc. 2016;116:e37-e40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Jain V, Misra S, Ahmad F, Rahul K, Singh A. MALT Lymphoma of Caecum Presenting as Acute Intestinal Obstruction: A Case Report. Indian J Surg. 2013;75:286-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Esteban JM, Gutiérrez del Olmo A, Baki W, Fernández S, Soria MT, Díaz Mediavilla J, Ramírez Armengol JA. Colonic mucosa-associated lymphoid tissue lymphoma presenting as multiple polyposis. Gastrointest Endosc. 2005;61:928-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Seo SW, Lee SH, Lee DJ, Kim KM, Kang JK, Kim DW, Lee JH. Colonic mucosa-associated lymphoid tissue lymphoma identified by chromoendoscopy. World J Gastroenterol. 2014;20:18487-18494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Toyomasu Y, Tsutsumi S, Yamaguchi S, Mochiki E, Asao T, Kuwano H. Laparoscopy-assisted ileocecal resection for mucosa-associated lymphoid tissue lymphoma of the appendix: case report. Hepatogastroenterology. 2009;56:1078-1081. [PubMed] |
| 27. | Troppan K, Wenzl K, Neumeister P, Deutsch A. Molecular Pathogenesis of MALT Lymphoma. Gastroenterol Res Pract. 2015;2015:102656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 28. | Kelley SR. Mucosa-associated lymphoid tissue (MALT) variant of primary rectal lymphoma: a review of the English literature. Int J Colorectal Dis. 2017;32:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Tannoury J, Amiot A, Lemonnier F, Dupuis J, Gagnière C, Belhadj K, Bras FL, Sobhani I, Haioun C, Copie-Bergman C, Lévy M. Colonic mucosa-associated lymphoid tissue lymphoma: a case series. Leuk Lymphoma. 2020;61:582-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Nakase H, Okazaki K, Ohana M, Ikeda K, Uchida K, Uose S, Itoh T, Iwano M, Watanabe N, Yazumi S, Kawanami C, Inoue F, Chiba T. The possible involvement of micro-organisms other than Helicobacter pylori in the development of rectal MALT lymphoma in H. pylori-negative patients. Endoscopy. 2002;34:343-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Matsumoto T, Iida M, Shimizu M. Regression of mucosa-associated lymphoid-tissue lymphoma of rectum after eradication of Helicobacter pylori. Lancet. 1997;350:115-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 86] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Shaheen S, Guddati AK. Secondary mucosa-associated lymphoid tissue (MALT) lymphoma of the colon. Med Oncol. 2013;30:502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Bennani A, Kharrasse G, Achraf M, Wafa K, Zahi I, Imane K, Mohamed B. Synchronous colonic adenoma and intestinal marginal zone B-cell lymphoma associated with Crohn's disease: a case report and literature review. BMC Cancer. 2019;19:966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Kawashima K, Katakura K, Takahashi Y, Asama H, Fujiwara T, Kumakawa H, Ohira H. Primary rectal mucosa-associated lymphoid tissue lymphoma in a patient with previously identified primary biliary cirrhosis and secondary Sjögren's syndrome. Clin J Gastroenterol. 2016;9:124-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Doolabh N, Anthony T, Simmang C, Bieligk S, Lee E, Huber P, Hughes R, Turnage R. Primary colonic lymphoma. J Surg Oncol. 2000;74:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |