Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6444
Peer-review started: August 4, 2020
First decision: August 21, 2020
Revised: September 25, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: December 26, 2020
Processing time: 135 Days and 1.9 Hours
Pulmonary cryptococcosis (PC) is an invasive fungal disease caused mainly by Cryptococcus (C.) neoformans or C. gattii. It may be present in immunocompetent or immunocompromised patients. The radiographic features of PC vary, and the most common computed tomography manifestation is the presence of solitary or multiple pulmonary nodules or masses distributed in the outer zone of the lung field. The appearance of nodular or mass-like PC on computed tomography scans resembles that of primary or metastatic lung cancers, and differential diagnosis is sometimes difficult. The coexistence of PC and malignant tumors is rarely observed.
This paper reports three cases of PC combined with lung adenocarcinoma diagnosed by video-assisted thoracic surgery lung biopsy, which were successfully managed by early diagnosis and treatment.
The present case report might serve as a reminder not to neglect PC coexisting with adenocarcinoma. Early diagnosis and treatment lead to a better prognosis.
Core Tip: The appearance of nodular or mass-like pulmonary cryptococcosis on computed tomography scans resembles that of primary or metastatic lung cancers, and differential diagnosis is sometimes difficult. To the best of our knowledge, the coexistence of pulmonary cryptococcosis and malignant tumors is rarely reported. However, the possibility of the coexistence of pulmonary cryptococcosis and adenocarcinoma indicates that the pathological results of one lesion cannot represent the characteristics of all lesions. In such cases, close follow-up and biopsy of multiple lesions may be required.
- Citation: Zheng GX, Tang HJ, Huang ZP, Pan HL, Wei HY, Bai J. Clinical characteristics of pulmonary cryptococcosis coexisting with lung adenocarcinoma: Three case reports. World J Clin Cases 2020; 8(24): 6444-6449
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6444.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6444
Pulmonary cryptococcosis (PC) is a fungal infection that results from the inhalation of spores from Cryptococcus neoformans[1]. The infection usually occurs in immuno-compromised patients, especially in those with T-lymphocytopenia[2]. The multiple nodular shadows that manifest, particularly in the peripheral lung, can sometimes be confused with malignant tumors and metastatic cancer based on nonspecific symptoms and radiological findings. Many case reports have focused on the misdiagnosis of PC as a malignant tumor[3]. This study aimed to describe three cases of multiple nodules with imaging findings, which were eventually diagnosed by thoracoscopy as PC coexisting with lung adenocarcinoma. After treatment, they all had a better prognosis. The coexistence of PC and malignant tumor was presented only in a few reports[4-9], and it is often easily misdiagnosed. Delayed treatment of malignant tumor results in a higher pathologic stage and poorer prognosis.
Case 1: A 69-year-old man presented with cough accompanied by chest discomfort for 2 mo, with no significant sputum and no fever, chest pain, wheezing, or weight loss.
Cases 2 and 3: A 54-year-old man (case 2) and a 46-year-old woman (case 3) had no chief complaints.
Case 1 presented to our hospital in August 2017 for cough accompanied by chest discomfort for 2 mo. He denied other discomfort. Cases 2 and 3 had no clinical symptoms. They were admitted to our hospital for abnormal findings on annual screening chest radiography.
Case 1 had a history of smoking. Case 3 had a history of systemic lupus erythematosus and chronic viral hepatitis B, and was administered oral telbivudine, hydroxy-chloroquine, and methylprednisolone sodium succinate regularly. These three patients denied having a history of exposure to pigeon droppings or pets.
All the three cases had not traveled recently and their family history was unremarkable.
There were no physical findings to note.
Case 1: Laboratory data, including the results of routine blood tests, C-reactive protein levels, and erythrocyte sedimentation rates, were all normal. Blood fungal examinations (Candida antigen, Aspergillus DNA, Cryptococcus neoformans antigen, and beta-D-glucan) were all negative. An enzyme-linked immunosorbent assay test for human immunodeficiency virus (HIV) was negative. Total lymphocyte, CD4, and CD8 counts and serum complement and immunoglobulin levels were normal. Triple sputum smears for the acid-fast bacilli test and fungus were negative. Tumor markers in blood, including carcinoembryonic antigen (CEA), cancer antigen 125 (CA125), CA199, neuron-specific enolase, squamous cell carcinoma, and cytokeratin 19, were all normal.
Case 2: Laboratory data, including routine blood tests and blood tumor markers (CEA and CA125), were all normal.
Case 3: Laboratory data were normal for routine blood tests, the tumor marker CEA was normal, and the CA125 level increased by 50.91 U/mL (normal value 0-35 U/mL).
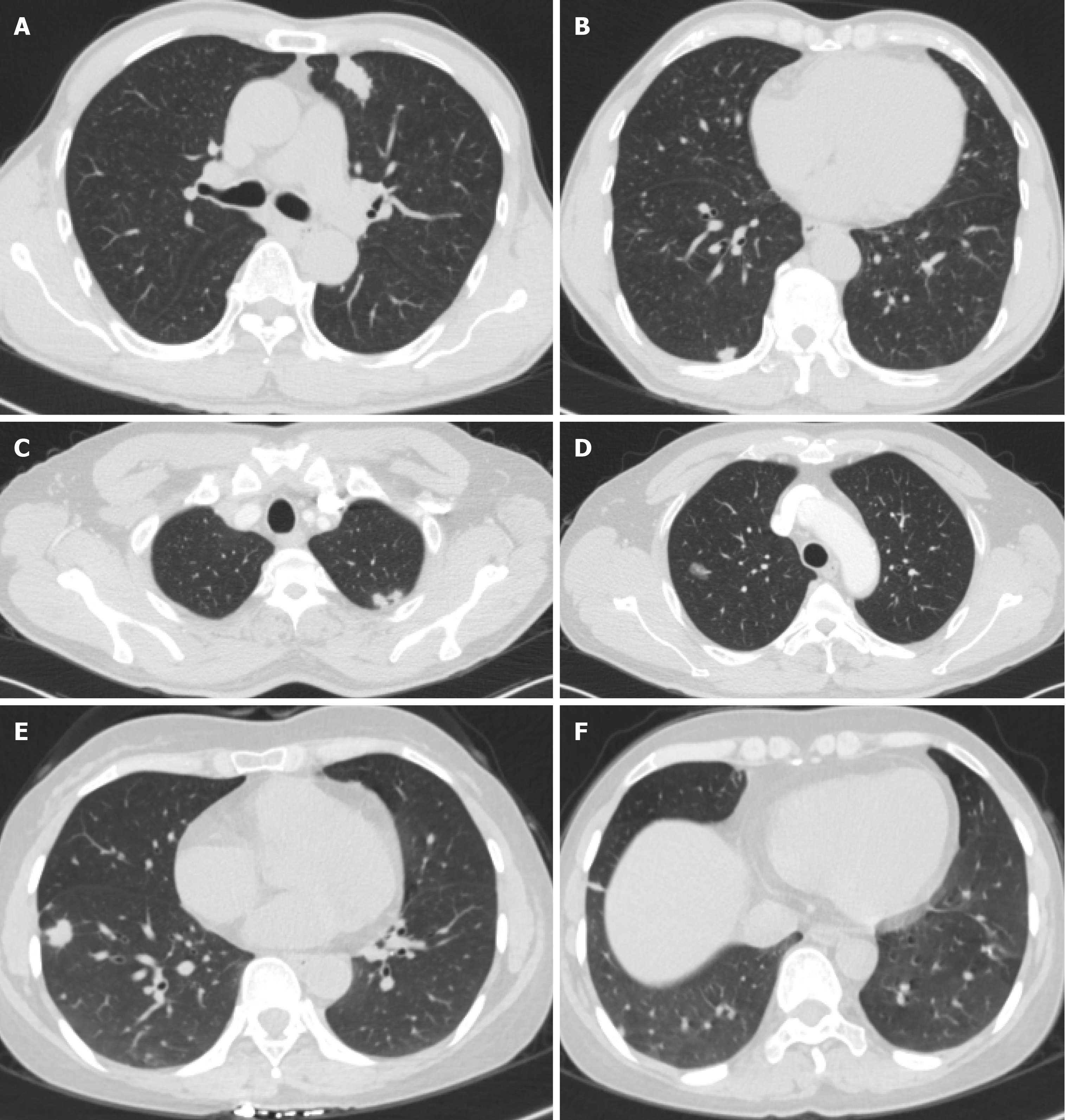
Case 1: Computed tomography (CT) of his chest showed multiple nodules in both lungs (Figure 1A and B).
Case 2: Chest CT revealed a ground-glass nodule in the posterior segment of the right upper lobe apex (Figure 1C and D) and multiple nodules in the left upper lobe with a maximum diameter of 7 mm. Neither hilar nor mediastinal lymphadenopathy was noted. The lesions did not change after 1 year of follow-up.
Case 3: A CT scan of her chest showed two nodules in the right lower lobe, one in the dorsal segment and the other in the outer basal segment (Figure 1E and F).
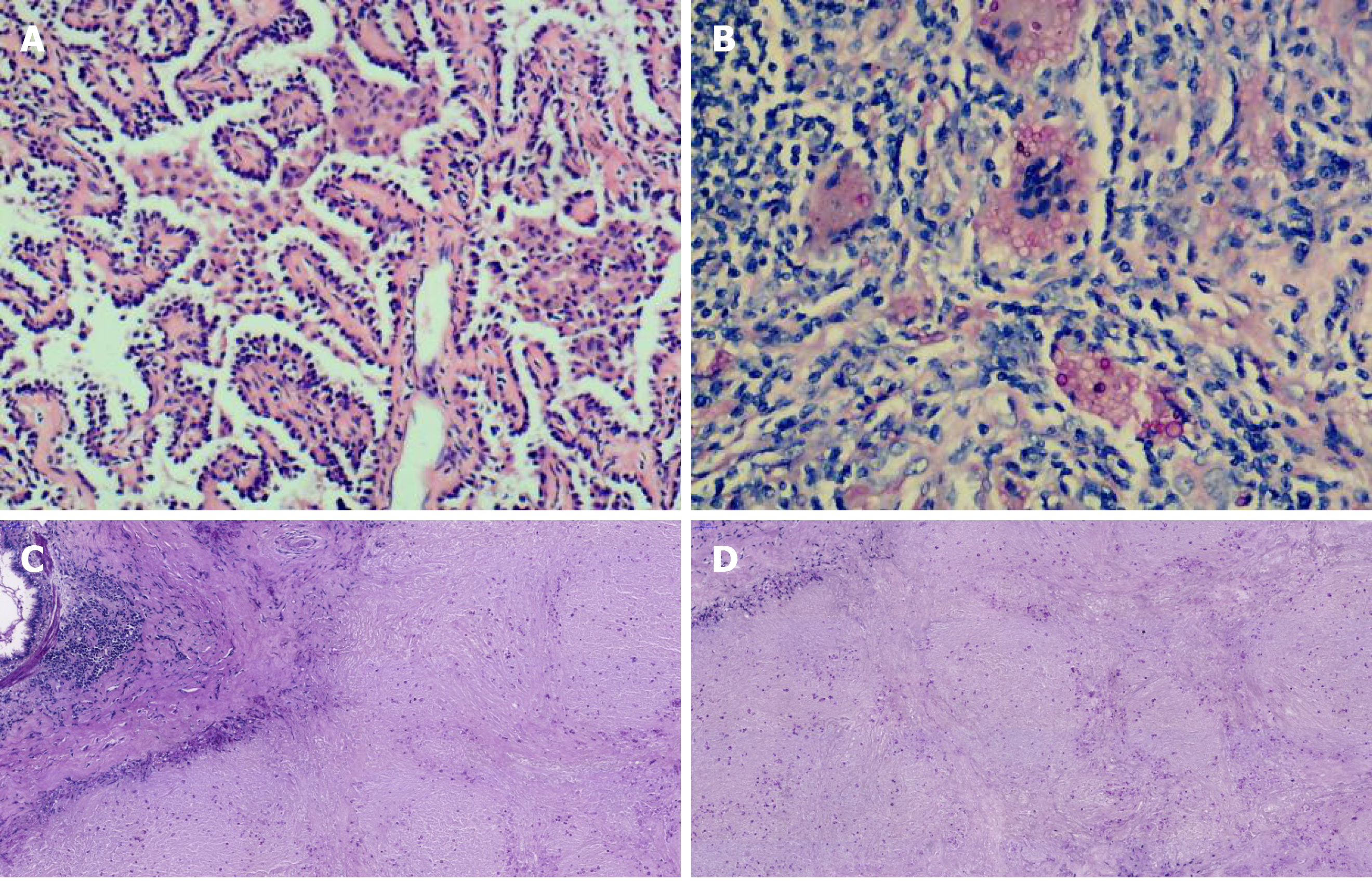
Preoperative diagnosis was lung cancer with intrapulmonary metastasis. Finally, the patient underwent surgery. Partial resection of the left upper lobe was performed using video-assisted thoracoscopy. The histologic examination after resection revealed primary lung adenocarcinoma (Figure 2A). Additionally, partial resection of the right lower lobe using video-assisted thoracoscopy showed PC (Figure 2B), with positive periodic acid-Schiff (PAS) (Figure 2C) staining and PAS diastase (D-PAS) (Figure 2D) staining.
Cryptococcosis was diagnosed by histologic examination of the left upper lobe. Histologic finding of the right upper lobectomy reveled alveolar cell carcinoma.
Alveolar cell carcinoma in the dorsal segment of the lower lobe of her right lung and cryptococcosis in the outer basal segment of the lower lobe of her right lung were diagnosed by lung biopsy under video-assisted thoracoscopy.
Partial resection of the left upper lobe and the right lower lobe was performed using video-assisted thoracoscopy. The patient received fluconazole (200 mg daily) for 6 mo after the surgery.
Cryptococcosis was diagnosed by wedge resection under video-assisted thoracoscopy of the left upper lobe. But 1-mo fluconazole (200 mg/d) as an antifungal therapy did not reduce the size of masses. We performed a right upper lobectomy. The patient received 6 mo of treatment with fluconazole (200 mg daily) postoperatively.
The patient took fluconazole (200 mg daily) as an antifungal therapy for 6 mo.
There was no evidence of recurrence at 2 years postoperatively and after fluconazole treatment in these three cases.
PC coexisting with pulmonary carcinoma is rare, with only one case each reported in Japan, China, South Korea, and other countries in East Asia[4-9]. The aforementioned three cases had multiple lung nodules, and the patients were ultimately diagnosed with PC coexisting with adenocarcinoma by lung tissue biopsy. The cases highlighted the possibility of duality in the diagnosis of multiple pulmonary nodules based on the CT examination. They point to the possibility of the coexistence of PC and adenocarcinoma and indicate that the pathological results of one lesion cannot represent the characteristics of all lesions. In such cases, close follow-up and biopsy of multiple lesions may be required.
The clinical symptoms of the aforementioned cases were nonspecific, including mainly cough and sputum; cases might also be asymptomatic. The results of routine blood tests and tumor marker CEA for these cases were normal. Serum cryptococcal antigen detection tests by latex agglutination were performed in one case, with negative results. The PC nodules in these cases were located in the field of the lung, adjacent to or involving the pleura; single or multiple nodules with a diameter of less than 1 cm were predominant. The CT findings of lung cancer consisted of a solitary nodule shadow accompanied by a variety of CT tumor-like signs, such as lobulation signs, burr signs, pleura depression signs, and focal ground-glass opacity. In one case (case 3), lung cancer and cryptococcus nodules were located in the same lung lobe. In the remaining two cases, the lung cryptococcosis nodules and lung cancer nodules were not on the same side of the lung lobe. Nodular or mass-type PC is easily misdiagnosed as lung cancer or metastatic cancer. Notably, the differences in imaging findings between the two diseases may help in identification: PC nodules predominantly occur adjacently to the pleura, have different shapes and sizes, and are limited to a single lung lobe; pulmonary metastatic tumors that usually present with variable in sizes and shapes with smooth edges frequently occur in the lower lungs. In most reported cases, the pathological type of lung cancer was pulmonary adenocarcinoma, which was similar to that in patients in this study. Cryptococcus may prefer residing in the peripheral lung, and therefore it is difficult to obtain a definitive diagnosis for multiple pulmonary nodules in the peripheral lung on chest CT. Attention should be paid to the characteristics of the nodule, and thoracoscopic surgery should be performed in time so that patients can be diagnosed and treated as early as possible. A definite diagnosis for the patients in this study took less time. The nodules with different etiology have characteristic imaging manifestations, and pathology is the key to diagnosis.
Cryptococcal infections affect a variety of hosts, including those who have severely compromised immune systems and those who have “normal” immune systems. However, they are occasionally found in immunocompetent hosts and are more likely to occur in immunosuppressed patients, such as those undergoing organ transplant or long-term glucocorticoid therapy and those with hematological malignancies, diabetes, and liver cirrhosis, among others. In China, PC is the third most common pulmonary fungal infection; most patients with PC in China have no underlying disease[10]. The patients in the present study denied any history of contact with birds or polluted environment and had not traveled recently. When and where these patients became infected with spores was not known. Harada et al[4] suggested that the coexistence of the two lesions was coincidental. However, Robinson et al[7] proposed that lung cancer caused immunosuppression and secondary cryptococcal infection. The relationship between lung cancer and PC should be further explored.
The present study provided many interesting insights into the differential diagnosis of multiple pulmonary nodules. Resection of the lesion should be performed under medically permissive conditions to obtain a definitive diagnosis for pulmonary nodules suspected as malignancy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yu M S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Chang WC, Tzao C, Hsu HH, Lee SC, Huang KL, Tung HJ, Chen CY. Pulmonary cryptococcosis: comparison of clinical and radiographic characteristics in immunocompetent and immunocompromised patients. Chest. 2006;129:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 151] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 2. | Campuzano A, Wormley FL. Innate Immunity against Cryptococcus, from Recognition to Elimination. J Fungi (Basel). 2018;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 3. | Wang D, Wu C, Gao J, Zhao S, Ma X, Wei B, Feng L, Wang Y, Xue X. Comparative study of primary pulmonary cryptococcosis with multiple nodules or masses by CT and pathology. Exp Ther Med. 2018;16:4437-4444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Harada T, Hakuma N, Kamimura A, Ito K, Okamoto K. Pulmonary cryptococcosis within a pulmonary carcinoma-review of reported cases. Intern Med. 2006;45:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Kawasaki H, Ishikawa K, Kuniyoshi M, Ohta M, Kawabata T, Hirayasu T. Lung adenocarcinoma with coexisting pulmonary cryptococcoma. Jpn J Thorac Cardiovasc Surg. 2004;52:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Huang J, Lan C, Li H, Chen S, Lin Q, Weng H. Concomitant lung adenocarcinoma and pulmonary cryptococcosis confirmed by pathologic examinations. Medicine (Baltimore). 2019;98:e18316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Robinson TD, Barnes DJ, Watson GF. Coexistent cryptococcosis and carcinoma within a solitary pulmonary nodule. Aust N Z J Med. 1999;29:561-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Li L, Zhuang L, Zhou J, Shao C. Pulmonary cryptococcosis coexisting with adenocarcinoma: a case report and review of the literature. J Med Case Rep. 2018;12:327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Ahn IS, Kim HG, Ryu JS, Kim L, Kwak SM, Lee HL, Yoon YH, Cho JH. A case of pulmonary cryptococcosis with non-small cell lung cancer in idiopathic CD4+ T-lymphocytopenia. Yonsei Med J. 2005;46:173-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Lan CQ, Weng H, Li HY, Chen L, Lin QH, Liu JF, Huang JB. [Retrospective analysis of 117 cases of pulmonary cryptococcosis]. Zhonghua Jie He He Hu Xi Za Zhi. 2016;39:862-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |