Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6432
Peer-review started: July 28, 2020
First decision: September 24, 2020
Revised: October 7, 2020
Accepted: November 14, 2020
Article in press: November 14, 2020
Published online: December 26, 2020
Processing time: 140 Days and 16.6 Hours
Wet cupping (WC) is a traditional therapy of skin suction-assisted bloodletting that is widely used in modern alternative medicine in Asia and the Middle East. Herein, we report the case of a male who presented with ST-elevation myocardial infarction (STEMI) and life-threatening anemia and underwent excessive WC.
A 55-year-old male presented with chest pain (30 min) and dyspnea (3 wk). His initial electrocardiogram suggested STEMI in the anterior wall. Furthermore, his laboratory results showed severe anemia with a hemoglobin level of 4.1 g/dL. Of note, the patient underwent regular WC therapy for chronic back pain, which he had recently intensified. His WC practice resulted in life-threatening anemia and eventually STEMI. Percutaneous coronary intervention in the left anterior descending artery was performed to treat the STEMI. His dyspnea dramatically improved after the transfusion, and his hemoglobin level returned to 14.8 g/dL within 2 mo after discharge. He has been uneventful for the last seven years of follow-up.
The current case demonstrates that excessive WC without adequate medical monitoring can result in severe anemia, which can further develop into STEMI.
Core Tip: Wet cupping (WC) is a traditional therapy for promoting bloodletting by applying subatmospheric pressure to a glass cup attached to a skin-pricked, bleeding lesion. Herein, we report a man who self-performed excessive WC and presented with ST-elevation myocardial infarction and life-threatening anemia.
- Citation: Jang AY, Suh SY. Extreme venous letting and cupping resulting in life-threatening anemia and acute myocardial infarction: A case report. World J Clin Cases 2020; 8(24): 6432-6436
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6432.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6432
Wet cupping (WC) is one of the most widely used traditional therapies for musculoskeletal pain or headache that is performed in the Middle East, Asia, and Europe[1]. WC promotes bloodletting by applying subatmospheric pressure to a glass cup attached to a skin-pricked, bleeding lesion[1]. Herein, we report a man who self-performed excessive WC and presented with ST-elevation myocardial infarction (STEMI) and life-threatening anemia.
A 55-year-old male presented to the emergency department with chest pain and dyspnea.
The patient had a history of smoking (30 pack years). He had been experiencing dyspnea for 3 wk prior and his chest pain started 30 min before arrival, with a numeric rating scale score of seven.
The patient had a history of hypertension.
The patient was pale and had anemic conjunctiva. His initial blood pressure was 90/60 mmHg with a heart rate of 114 beats per minute.
An electrocardiogram showed ST segment elevation in leads V1 to V3 and reciprocal changes in leads II, III, and aVF, suggestive of STEMI.
The patient was moved to the catheter lab for emergent percutaneous coronary intervention (PCI) before the laboratory results were available because of the strict door-to-balloon time regulations in Korea.
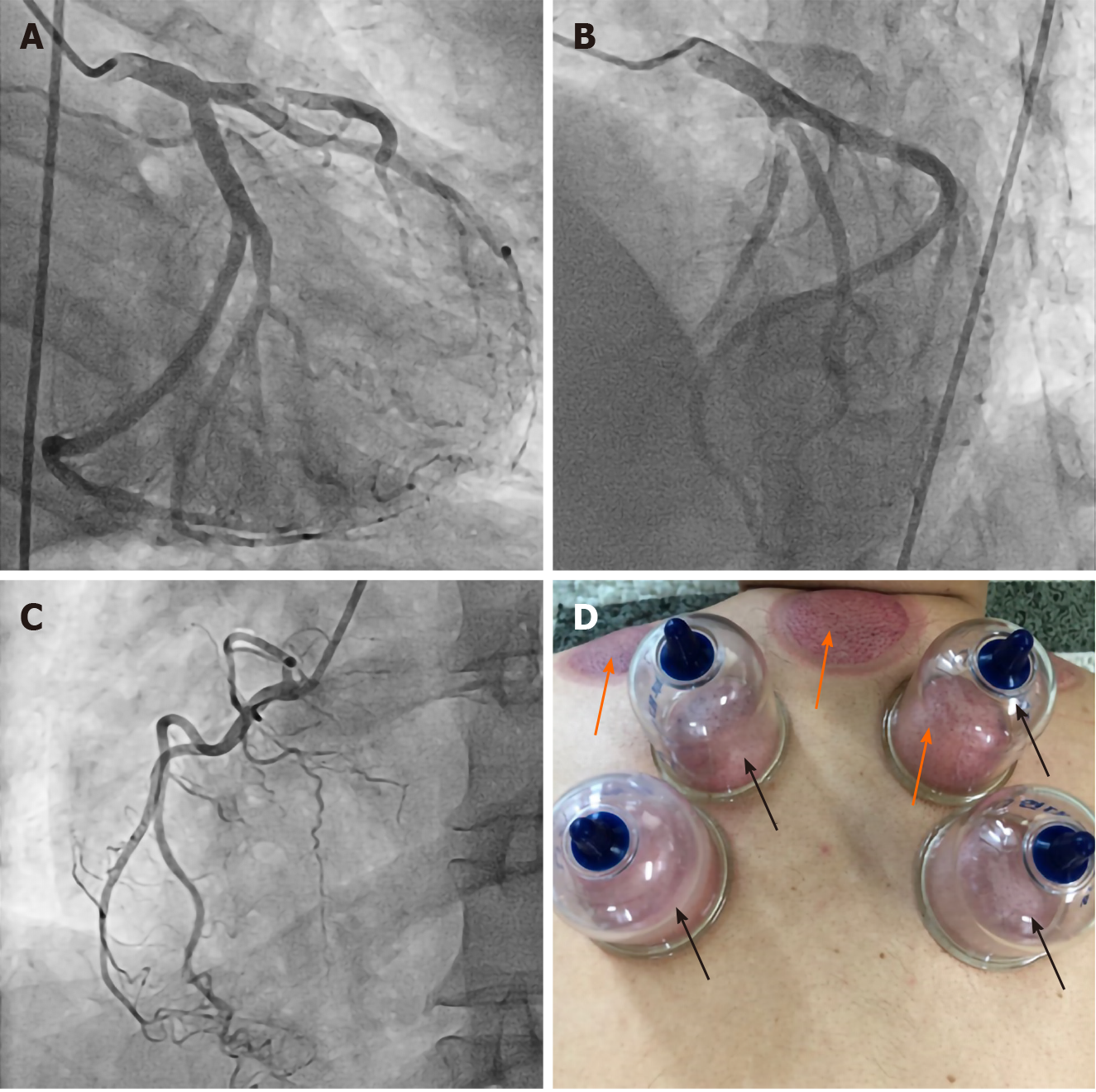
Coronary angiography revealed 99% stenosis of the proximal left anterior descending (LAD) artery caused by a ruptured plaque, with distal thrombolysis in myocardial infarction flow 3 (Figure 1A-C). A drug-eluting stent (Cilotax™ 3.5 mm × 15 mm) was inserted into the LAD lesion without complications. Consistently low blood pressure was noted during and after PCI.
After PCI, the patient’s chest pain was improved, although his dyspnea remained. The lab results were reported after PCI, and cardiac markers were increased as expected. Strikingly, however, the hemoglobin (Hb) level was 4.1 g/dL. Rectal digital tests and nasogastric tube aspiration examinations were negative, ruling out gastrointestinal tract bleeding. Furthermore, his low-density lipoprotein cholesterol level was only 66 mg/dL. Upon careful history taking, we learned that the patient regularly self-performed WC therapy. He had recently intensified his WC routine by implementing it more frequently, which may have led to an excessive loss of blood. We further checked his iron and ferritin levels and total iron binding capacity (TIBC), which showed a typical pattern of iron deficiency anemia (iron, 16 μmoL/L; ferritin, 2.3 μg/L; TIBC, 374 μmoL/L). The initial echocardiography showed akinetic regional wall motion abnormalities in the LAD territory, although the contractile motion of other territories was hyperdynamic.
We consulted with Dr. Hong, who determined that the patient should be immediately transfused and given iron supplements for iron deficiency anemia.
The final diagnosis of the presented case was anemia due to excessive WC. The patient also developed STEMI, which was possibly induced by vigorous heart contractions compensating for the poor blood supply caused by life-threatening anemia.
A transfusion was immediately initiated, while concurrent iron supplementation was performed after consultation with hematology. Four packed red blood cells were transfused. After transfusion, the patient’s dyspnea was dramatically ameliorated and his hypotension recovered to normal blood pressure (120/80 mmHg). His Hb was 7.9 g/dL when he was discharged 2 d post-PCI. We also educated the patient regarding the consequences of unmonitored WC. Iron supplementation was maintained for the next 2 mo. Dual-antiplatelet therapy, angiotensin-converting enzyme inhibitors, beta-blockers, and statins were also given.
Two months after PCI, during his outpatient department visit, the patient’s Hb level had increased to 14.8 g/dL and his symptoms were completely alleviated. He no longer performs WC to this day and has been uneventful for the last seven years. A timeline of the patient’s disease course is shown in Table 1.
| Event | Timeline |
| Chest pain and ER presentation | Day 1 |
| PCI to proximal LAD | Day 1 |
| Initial Hb level checked (4.1 g/dL) | Day 1 |
| Transfusion and iron supplementation | Day 1 |
| Discharge (Hb: 7.9 g/dL) | Day 3 |
| Outpatient department visit (Hb: 14.8 g/dL) | Day 63 |
WC therapy is the application of subatmospheric pressure to a skin-attached glass or plastic cup after pricking precise acupuncture points or painful areas (Figure 1D)[1]. The intensity of bruises and the amount of suctioned blood are dependent on the strength of the negative pressure applied. Such practices were traditionally performed in Asia, the Middle East, and Europe with great popularity because they were thought to remove harmful blood or toxins that were causative of diseases[1]. Even today, WC is widely performed in Asia and the Middle East in the field of alternative medicine for chronic musculoskeletal pain. Although several small, modern studies have investigated the therapeutic efficacy of WC, the benefits remain relatively unknown[2].
The patient in our study practiced regular WC for his chronic upper back pain. He also stated that as his shortness of breath developed, he had more frequently performed WC during the 3 wk prior to admission because he thought that it would improve his symptoms. Considering that his dyspnea may have developed with decreased cardiac output due to blood loss, his intensified bloodletting may have aggravated his heart failure to a further extent. Furthermore, vigorous heart contractility to compensate for the loss of preload may also have facilitated the imbalance between the patient’s myocardial supply and consumption.
Anemia is a well-established risk factor for future adverse events in patients with acute coronary syndrome, stroke, and heart failure[2,3]. Although whether anemia leads to the formation of atherosclerosis is relatively undiscovered, an intravascular ultrasound study revealed that anemia was independently associated with thin-cap fibroatheroma, which is thought to be impending plaque rupture[4]. The mechanism of this finding has not been elucidated; however, it has been demonstrated that hypovolemia-induced hypernatremia leads to chronic inflammation and the development of atherosclerosis[5]. Considering that the patient had relatively low levels of low-density lipoprotein and triglycerides, it is conceivable that other mechanisms, anemia in this case, may have played a major role in the development of atherosclerosis and the rupture of plaque. The dehydrated state of the patient may have promoted systemic inflammation, further leading to the formation of a vulnerable plaque and the subsequent rupture that caused the STEMI[5].
The current case demonstrates that excessive WC without adequate medical monitoring can result in severe anemia, which can further develop into life-threatening myocardial infarction.
We thank Professor Junshik Hong, who works at Seoul National University Hospital, for offering great advice for managing this patient.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saad K S-Editor: Fan JR L-Editor: A P-Editor: Ma YJ
| 1. | Li JQ, Guo W, Sun ZG, Huang QS, Lee EY, Wang Y, Yao XD. Cupping therapy for treating knee osteoarthritis: The evidence from systematic review and meta-analysis. Complement Ther Clin Pract. 2017;28:152-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 2. | AlBedah A, Khalil M, Elolemy A, Hussein AA, AlQaed M, Al Mudaiheem A, Abutalib RA, Bazaid FM, Bafail AS, Essa A, Bakrain MY. The Use of Wet Cupping for Persistent Nonspecific Low Back Pain: Randomized Controlled Clinical Trial. J Altern Complement Med. 2015;21:504-508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Mamas MA, Kwok CS, Kontopantelis E, Fryer AA, Buchan I, Bachmann MO, Zaman MJ, Myint PK. Relationship Between Anemia and Mortality Outcomes in a National Acute Coronary Syndrome Cohort: Insights From the UK Myocardial Ischemia National Audit Project Registry. J Am Heart Assoc. 2016;5:e003348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Hong YJ, Jeong MH, Choi YH, Song JA, Kim DH, Lee KH, Yamanaka F, Lee MG, Park KH, Sim DS, Yoon NS, Yoon HJ, Kim KH, Park HW, Kim JH, Ahn Y, Cho JG, Park JC, Kang JC. Relation between anemia and vulnerable coronary plaque components in patients with acute coronary syndrome: virtual histology-intravascular ultrasound analysis. J Korean Med Sci. 2012;27:370-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Dmitrieva NI, Burg MB. Elevated sodium and dehydration stimulate inflammatory signaling in endothelial cells and promote atherosclerosis. PLoS One. 2015;10:e0128870. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |