Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6373
Peer-review started: July 30, 2020
First decision: September 24, 2020
Revised: September 30, 2020
Accepted: October 26, 2020
Article in press: October 26, 2020
Published online: December 26, 2020
Processing time: 142 Days and 11.4 Hours
Primary malignant melanoma of the lung (PMML) is a rare and highly malignant tumor with a poor prognosis. Here, we report a PMML case diagnosed by computed tomography (CT)-guided percutaneous biopsy, describe its pathological features and review relevant literature to improve our understanding of this tumor.
A 64-year-old Chinese female presented with productive cough for 7 mo. A chest CT scan showed a large and space-occupying lesion in Lingual lobe. Positron emission tomography-CT revealed multiple nodules located in the superior lobe apicoposterior segment of her left lung. Brain magnetic resonance imaging showed numerous enhancing nodules, suggesting brain metastasis. Abdominal CT scan did not show any abnormalities. By CT-guided percutaneous biopsy, four pieces of gray and taupe tissues (1 cm length and 0.1 mm in diameter) were obtained. After pathologic examination, the tumor was found to consist of epidermal and nested small round cells, fibrosis and thin-walled blood vessels. The finding was suggestive of malignant melanoma. To confirm the diagnosis, pathological morphology and immunophenotypic features of the biopsy specimens were observed. The patient denied any history of skin tumors. No abnormal lesions were detected in other sites of the body. Molecular testing was positive for wild-type EGFR and KIT gene mutations. Finally, the clinical and pathological findings suggested PMML.
PMML is very rare, and the percutaneous biopsy tissue is limited. Therefore, comprehensive consideration of histology, immunohistochemistry, imaging, and clinical information is important for the diagnosis of PMML.
Core Tip: Malignant melanoma is a refractory malignancy with a dismal prognosis. Primary malignant melanoma of lung is rare, accounting for only 0.01% of all primary lung tumors. This case highlights that comprehensive consideration of histology, immunohistochemistry, imaging, and clinical information is important for the diagnosis of primary malignant melanoma of the lung.
- Citation: Xi JM, Wen H, Yan XB, Huang J. Primary pulmonary malignant melanoma diagnosed with percutaneous biopsy tissue: A case report. World J Clin Cases 2020; 8(24): 6373-6379
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6373.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6373
Malignant melanoma (MM) is a malignant and highly aggressive tumor. It usually arises from embryonic neural crest melanocytes and occurs in the skin or mucosal surfaces. Primary MM of lung (PMML) is extremely rare, accounting for 0.01% of all primary lung tumors[1] (Table 1); thus, pathologists have limited experience with the diagnosis of this tumor. The clinical and pathological evaluation criteria recommended by the Armed Forces Institute of Pathology are: (1) A solitary pulmonary tumor; (2) A MM confirmed by immunohistochemistry and/or electron microscopy; (3) No past history of excision or fulguration of cutaneous, mucosal, or ocular lesion; (4) A central pulmonary lesion; and (5) No observable tumor elsewhere at the time of diagnosis[1]. Herein, we report a case of PMML diagnosed by computed tomography (CT)-guided percutaneous biopsy tissue and present its pathological morphology and immunophenotypic features with the aim to improve clinical understanding of PMML and avoid misdiagnosis.
| No. | Ref. | PMID | Age | Gender | Imaging test | Immunohistochemical staining, positive |
| 1 | Deng et al[12], 2020 | 32303211 | 57 | Male | PET-CT | HMB-45; Melan-A; S-100 |
| 2 | Hibiya et al[13], 2020 | 32028967 | 47 | Female | CT | S-100; HMB45 |
| 3 | Yunce et al[3], 2018 | 29686784 | 22 | male | CT; EBUS | HMB45; MSA; S-100; α-SMA |
| 4 | Yabuki et al[14], 2018 | 30360631 | 74 | male | CT; EBUS; Chest X-ray | HMB-45; Melan A; S100 |
| 5 | Shi et al[7], 2018 | 30062692 | 46 | male | CT; Fiberoptic bronchoscopy | HMB-45; Melan A; S100 |
| 6 | Peng et al[6], 2017 | 29145332 | 61 | Female | PET-CT; CT; Chest X-ray | HMB-45; Melan A; S100 |
| 7 | Mahowald et al[15], 2015 | 25841827 | 55 | Male | PET-CT; CT; Chest X-ray; MRI | HMB-45; Melan A; S100 |
| 8 | Liu et al[16], 2014 | 25126176 | 49 | Female | PET-CT; CT | HMB-45; Melan A; S-100 |
| 9 | Lazarou et al[17], 2014 | 26766979 | 82 | Male | Chest X-ray; CT; PET-CT | S-100 |
| 10 | Pan et al[18], 2010 | 20819656 | 81 | Male | PET-CT; MRI | HMB-45; S-100 |
| 11 | Maeda et al[19], 2009 | 20013105 | 68 | Male | CT; MRI; Fiberoptic bronchoscopy | HMB-45; S-100 |
| 12 | Reddy et al[20], 2007 | 17375790 | 74 | Male | CT | HMB-45; S-100 |
| 13 | Kundranda et al[21], 2006 | 16512984 | 60 | Male | PET-CT | S-100; NK1/C3 |
| 14 | Lie et al[22], 2005 | 15917706 | 44 | Female | CT; EBUS | HMB-45; S-100 |
| 15 | Dountsis et al[2], 2003 | 14750982 | 41 | Female | Chest X-ray | HMB-45; S-100 |
| 16 | Ozdemir et al[23], 2001 | 11574244 | 41 | Male | Chest X-ray; CT | HMB 45 |
A 64-year-old Chinese female was admitted to Hunan Academy of Traditional Chinese Medicine Affiliated Hospital due to productive cough for 7 mo, with blood in sputum, breathlessness and dizziness intermittently. She denied any history of skin cancer. No abnormal lesions were found in other parts of the body, including the skin, head, neck, scalp, anogenital region and eyes.
Gross examination and molecular testing: Four pieces of gray and taupe tissue (1 cm length and 0.1 mm in diameter) were obtained. KIT gene mutation was detected in the tumor tissue, while no specific EGFR mutations were found in the patient.
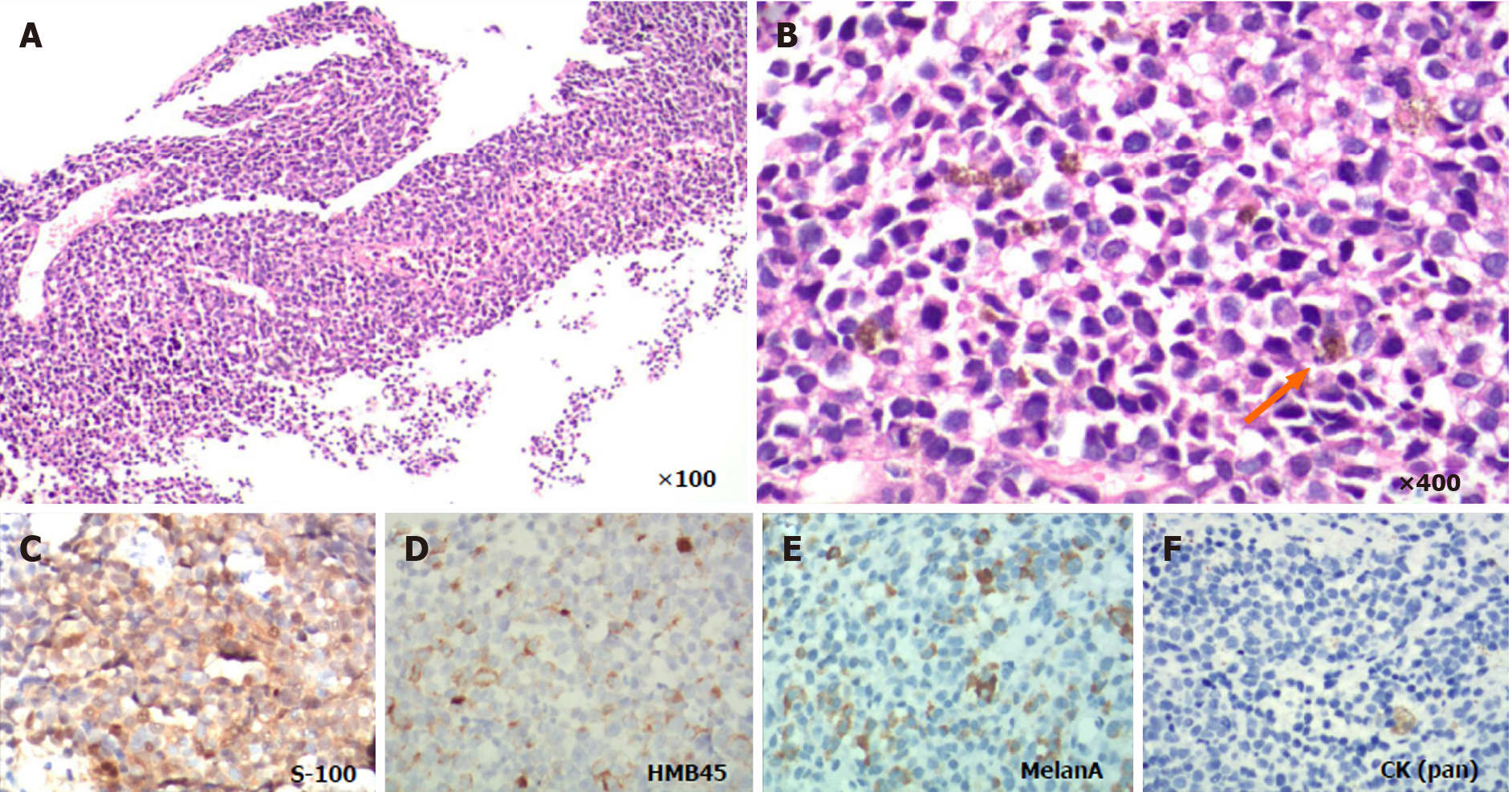
Microscopic examination: Histologically, the tumor was composed of small round cells and thin-walled blood vessels, with collagen fiber hyperplasia and few coagulative necrosis. The tumor cells were arranged in sheets, nests and a discohesive pattern and accompanied by vessels (Figures 1 and 2). The tumor cells were mostly medium-sized, rich in cytoplasm and light staining and had no clear boundary. Vacuolated nucleus and nucleoli and frequent mitoses were found in the tumor cells. However, a few of the tumor cells were darkly stained in the nucleus with eosinophilic staining in the cytoplasm. There were also individual cells with plasmacytoid appearance. In some areas, fine melanin granules exited in or out of the cells.
Immunohistochemical detection: Immunohistochemical (IHC) staining showed that the tumor cells were positive for MM markers human melanoma black 45 (HMB-45), Melan A, S-100 and vimentin, and negative for cytokeratin (pan), CD138, transcription termination factor 1, Napsin-A, Cytokeratin-7, P63, P40, synaptophysin, chromogranin-A, neuron-specific enolase, Desmin, CD99 and leukocyte common antigen (Figure 2). The positive rate of Ki67 was about 50%.
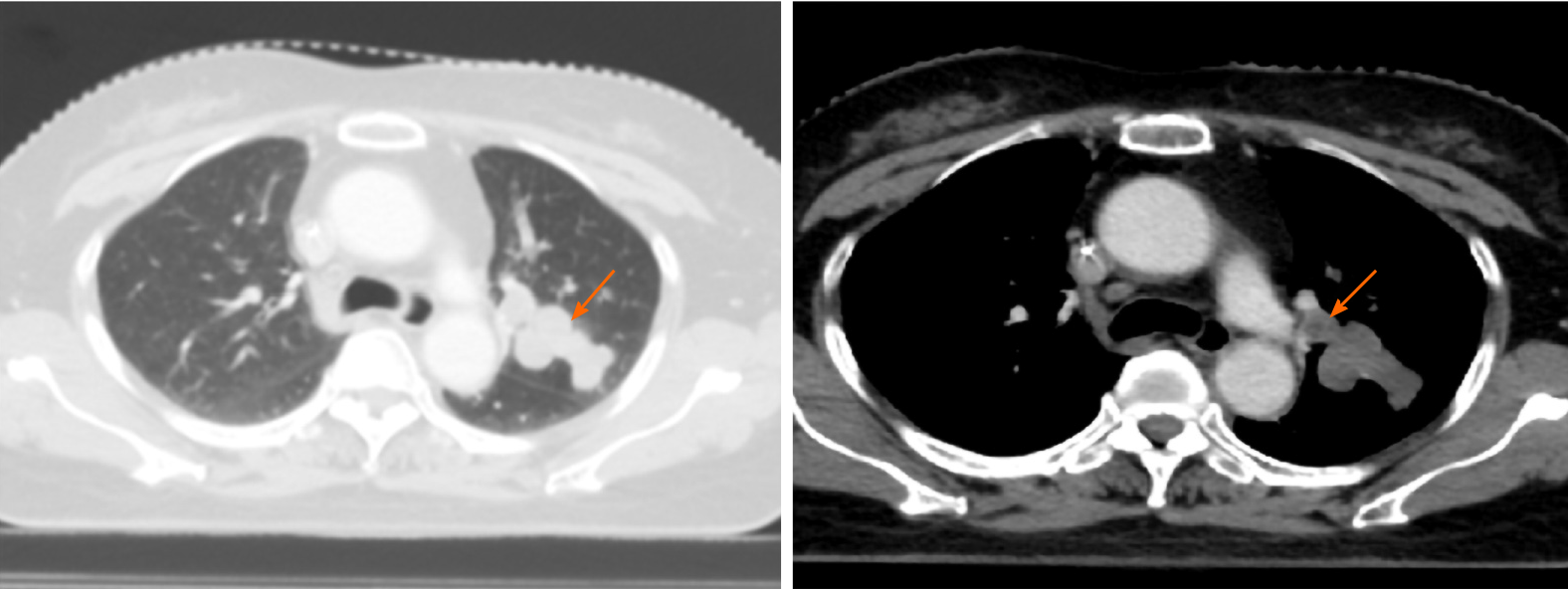
The patient underwent a CT scan of the lung, and the results showed a large, space-occupying lesion in the Lingual lobe. Positron emission tomography-CT (PET-CT) revealed multiple nodules located in superior lobe apicoposterior segment of her left lung. Nodules were partly integrated, well-demarcated and smooth. The largest nodule was 26 mm × 19 mm and irregular. The lesions were mostly accompanied with bronchus and lymph-vessel from peripheral to hilum of the lung. PET-CT also showed multiple left hilar lymph node metastases, and no metabolic abnormalities were detected in other parts of the body, including the head, neck, other parts of the chest, abdomen and pelvis. Brain magnetic resonance imaging showed numerous enhancing nodules, suggesting brain metastasis. The patient was clinically diagnosed with primary lung cancer. To obtain a specific pathological diagnosis, a CT-guided percutaneous biopsy of the lesions was performed, and then the small tissue samples were sent for pathological evaluation.
All of the aforementioned clinicopathological features were suggestive of PMML.
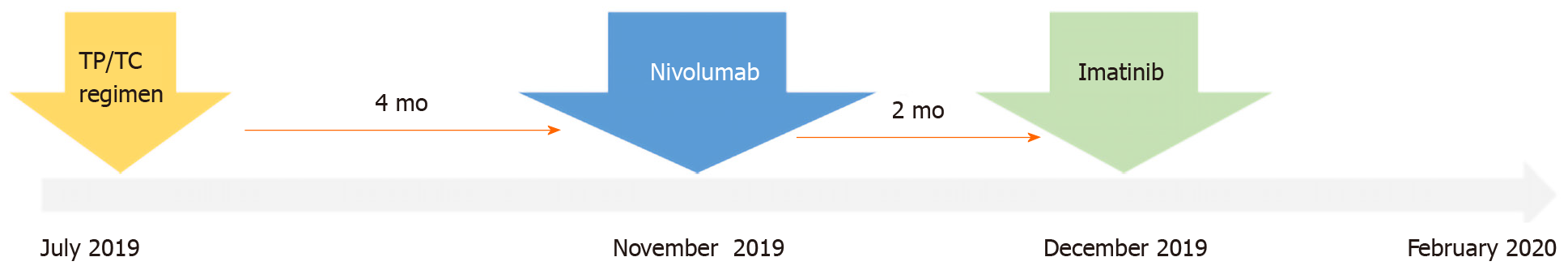
Beginning in July 2019, the patient was given two cycles of chemotherapy TP regimen (paclitaxel 270 mg/m2 intravenous (IV) on day 1 of a 21-d cycle) plus cisplatin (120 mg/m2 IV on days 1-3 of a 21-d cycle) and taxotere and cyclophosphamide regimen (240 mg/m2 IV on day 1 of a 21-d cycle) plus carboplatin (500 mg/m2 IV on days 1-3 of a 21-d cycle). Four months later, the tumor had rapidly progressed, and the patient was treated with nivolumab (3 mg/kg every 2 wk.). About 1 mo later, the clinical re-examination confirmed the disease progression, and then oral imatinib was prescribed at 400 mg once daily for 4-wk cycles.
In February 2020, the patient was discharged, and it was recommended to continue imatinib anti-tumor therapy (data collection period was from November 2019 to February 2020) (Figure 3). No additional follow-up information was obtained from the patient at the time of manuscript writing.
MM usually occurs in the tissues where the melanocytes are located, such as skin, eyes, meninges, oropharynx, and anal canal, accounting for 1%-3% of malignant tumors[2]. Skin melanoma is the most common type of primary melanoma. The PMML is extremely rare, accounting for only 0.01% of all primary lung tumor[1,3]. The incidence of PMML is similar in male and female, and the mean age at diagnosis is 59.1 years (range from 29-90 years)[4,5]. The pathogenesis of PMML remains controversial[6,7]. At present, three hypotheses have been mainly proposed to explain the occurrence of PMML: (1) During embryotic development, melanocytes in the body can migrate not only into the epidermis and dermis of the skin but also into internal organs, such as esophagus, throat, brain, and lung; (2) Melanocytes may be transformed from bronchial gland in submucosa; and (3) Potential stem cells located in the lower respiratory tract can differentiate into melanocytes. Hence, those melanocytes can further develop into PMML.
However, PMML has no specific clinical symptom and can easily be misdiagnosed as tuberculosis or lung carcinoma. In addition, some primary skin MM can be metastasized, and then their primary lesions disappear, so it is quite difficult to diagnose primary or metastatic MM of lung[8]. The patient in this report presented common clinical manifestations, including recurrent cough and occasional hemoptysis, which were not specific from other respiratory infectious disease and lung tumors. The other clinical characteristics include no previously resected pigmented skin lesion. Unlike lung carcinoma, CT scan of this patient showed that the tumor was multinodular and well-demarcated, most of which was accompanied with tracheobronchial lymph nodes. Magnetic resonance imaging of the brain showed brain metastasis. Whole-body PET-CT revealed no lesions in other parts of the body. That is, there were no other detectable tumors at the time of diagnosis. The pathological diagnosis showed that the tumor cells had darkly stained nuclei and eosinophilic cytoplasm. In some areas, fine melanin granules exited in or out of the cells. The tumor cells were arranged in sheets, nests and a discohesive pattern and were accompanied by vessels. IHC staining showed that tumor cells were positive for the MM markers HMB-45 and Melan-A, which were valuable for the diagnosis of MM[2,3,6,7].
Genetic assays were also performed to identify the driver mutations. The results showed that the KIT gene was mutated, and no EGFR gene mutation was found. Mutations in c-KIT mostly occur in acral, mucosal, and chronically sun-damaged melanomas. As an important factor for cell differentiation, proliferation, and survival, c-KIT has been used in clinical trials of advanced melanoma to inhibit its function[9-11]. Based on these findings, this case met the above diagnostic criteria and was diagnosed as PMML.
Although histologically it is difficult to distinguish PMML from lung squamous-cell carcinoma (SCC), it should be known that IHC staining of SCC is usually negative for HMB-45 and Melan-A. Primary melanoma often appears as a solitary nodule or mass, often involving the bronchial lumen.
A chest CT scan also can help find the abnormalities in the lungs. Usually, CT scan shows a mild or moderate enhancement of the PMML, which is different from the obvious enhancement of lung carcinoma. However, radiological detections cannot distinguish between primary and metastatic lesions. Therefore, it is necessary to ask medical history in detail (i.e. black spots and moles, skin ulcers and injuries) and to take physical examination of skin, mucosa, anal canal and vulva to check for pigmentation. Then, combined with the pathologic histology and immunophenotypic analysis of the tumor, PMML can be diagnosed.
Histopathological examination is still the gold standard for PMML diagnosis, but there are still many difficulties in the detection process. These include the difficulty to distinguish PMML from lung SCC. It should be known that IHC staining of SCC is usually negative for HMB-45 and Melan-A, and primary melanoma often appears as a solitary nodule or mass, often involving the bronchial lumen. Furthermore, when microscopic observation shows that the lesions are composed of small round cells and negative for carcinoma makers, the following points should be noted: Were the round cells morphologically diverse and diffusely distributed? Were tumor vessels pretty rich? Were tumor cells friendly to vessels? and were melanin granules inside or outside the tumor cell? If the answers are all yes, then MM may be taken into consideration. Consideration of MM should be verified by IHC staining of MM markers. Moreover, it is necessary to pay attention to the differential diagnosis of PMML and some diseases that are also composed of similar small round cells, such as lymphomas, extramedullary plasmacytoma, rhabdomyosarcoma and primitive neuroectodermal tumor.
PMML is an extremely rare, highly malignant neoplasm with a poor prognosis. Histopathological examination is a reliable gold standard for confirmation of a PMML diagnosis. Because of the morphological and immunophenotypic variations, the diagnosis of PMML remains difficult and should be distinguished from the diagnosis of other cancers. IHC staining is helpful for the differential diagnosis of PMML. Currently, with the in-depth study of the molecular biological characteristics and genetic variation of melanoma, targeted immunotherapy may further benefit clinical treatment and has broad prospects[12-23].
We thank the patient and her family for their support.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lim SC, Teragawa H S-Editor: Zhang L L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Wilson RW, Moran CA. Primary melanoma of the lung: a clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1997;21:1196-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Dountsis A, Zisis C, Karagianni E, Dahabreh J. Primary Malignant Melanoma of the Lung: A Case Report. World J Surg Oncol. 2003;1:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Yunce M, Selinger S, Krimsky W, Harley DP. Primary malignant melanoma of the lung: a case report of a rare tumor and review of the literature. J Community Hosp Intern Med Perspect. 2018;8:29-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Ost D, Joseph C, Sogoloff H, Menezes G. Primary pulmonary melanoma: case report and literature review. Mayo Clin Proc. 1999;74:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Kyriakopoulos C, Zarkavelis G, Andrianopoulou A, Papoudou-Bai A, Stefanou D, Boussios S, Pentheroudakis G. Primary Pulmonary Malignant Melanoma: Report of an Important Entity and Literature Review. Case Rep Oncol Med. 2017;2017:8654326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Peng J, Han F, Yang T, Sun J, Guan W, Guo X. Primary malignant melanoma of the lung: A case report and literature review. Medicine (Baltimore). 2017;96:e8772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Shi Y, Bing Z, Xu X, Cui Y. Primary pulmonary malignant melanoma: Case report and literature review. Thorac Cancer. 2018;9:1185-1189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Yamada S, Nawata A, Yoshioka M, Hiraki T, Higashi M, Hatanaka K, Tanimoto A. Complete regression of primary cutaneous malignant melanoma associated with distant lymph node metastasis: a teaching case mimicking blue nevus. BMC Res Notes. 2016;9:366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Chu PY, Pan SL, Liu CH, Lee J, Yeh LS, Liao AT. KIT gene exon 11 mutations in canine malignant melanoma. Vet J. 2013;196:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Tate G, Tajiri T, Suzuki T, Mitsuya T. Mutations of the KIT gene and loss of heterozygosity of the PTEN region in a primary malignant melanoma arising from a mature cystic teratoma of the ovary. Cancer Genet Cytogenet. 2009;190:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Pham DDM, Guhan S, Tsao H. KIT and Melanoma: Biological Insights and Clinical Implications. Yonsei Med J. 2020;61:562-571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 12. | Deng S, Sun X, Zhu Z, Lu J, Wen G, Chang X, Gao H, Hua Y, Wang L, Gao J. Primary malignant melanoma of the lung: a case report and literature review. BMC Pulm Med. 2020;20:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Hibiya T, Tanaka M, Matsumura M, Aoki A, Ikegami T, Okudela K, Kawano N, Ohashi K. An NRAS mutation in primary malignant melanoma of the lung: a case report. Diagn Pathol. 2020;15:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Yabuki H, Kuwana K, Minowa M. Resection of primary malignant lung melanoma: a case report. Asian Cardiovasc Thorac Ann. 2018;26:710-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Mahowald MK, Aswad BI, Okereke IC, Ng T. Long-term survival after pneumonectomy for primary pulmonary malignant melanoma. Ann Thorac Surg. 2015;99:1428-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Liu GH, Liu J, Dong H, Tang XJ. Primary malignant melanoma of the lung: a case report. Int J Clin Exp Med. 2014;7:1757-1759. [PubMed] |
| 17. | Lazarou I, Purek L, Duc C, Licker MJ, Spiliopoulos A, Tschopp JM. Primary malignant achromic melanoma of the lung. Thorac Cancer. 2014;5:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Pan XD, Zhang B, Guo LC, Gu DM, Mao YQ, Li J, Xie Y, Wang L. Primary malignant melanoma of the lung in the elderly: case report and literature review. Chin Med J (Engl). 2010;123:1815-1817. [PubMed] |
| 19. | Maeda R, Isowa N, Onuma H, Miura H, Tokuyasu H, Kawasaki Y. Primary malignant melanoma of the lung with rapid progression. Gen Thorac Cardiovasc Surg. 2009;57:671-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Reddy VS, Mykytenko J, Giltman LI, Mansour KA. Primary malignant melanoma of the lung: review of literature and report of a case. Am Surg. 2007;73:287-289. [PubMed] |
| 21. | Kundranda MN, Clark CT, Chaudhry AA, Chan V, Daw HA. Primary malignant melanoma of the lung: a case report and review of the literature. Clin Lung Cancer. 2006;7:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Lie CH, Chao TY, Chung YH, Lin MC. Primary pulmonary malignant melanoma presenting with haemoptysis. Melanoma Res. 2005;15:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Ozdemir N, Cangir AK, Kutlay H, Yavuzer ST. Primary malignant melanoma of the lung in oculocutaneous albino patient. Eur J Cardiothorac Surg. 2001;20:864-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |