Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6353
Peer-review started: July 3, 2020
First decision: September 24, 2020
Revised: September 27, 2020
Accepted: October 27, 2020
Article in press: October 27, 2020
Published online: December 26, 2020
Processing time: 169 Days and 10.2 Hours
Tuberculosis (TB) mostly attacks the lungs, and extrapulmonary TB involving the central nervous system is uncommon; among these cases, spinal intramedullary TB is even more rare. The clinical manifestations of spinal intramedullary TB are similar to those of intramedullary spinal cord tumors. Therefore, it is necessary to make a careful differential diagnosis of spinal intramedullary lesions to achieve the appropriate treatment and favorable prognosis. We report a rare case of a young male patient with paraplegia due to spinal intramedullary TB, which is uncommon and regrettable.
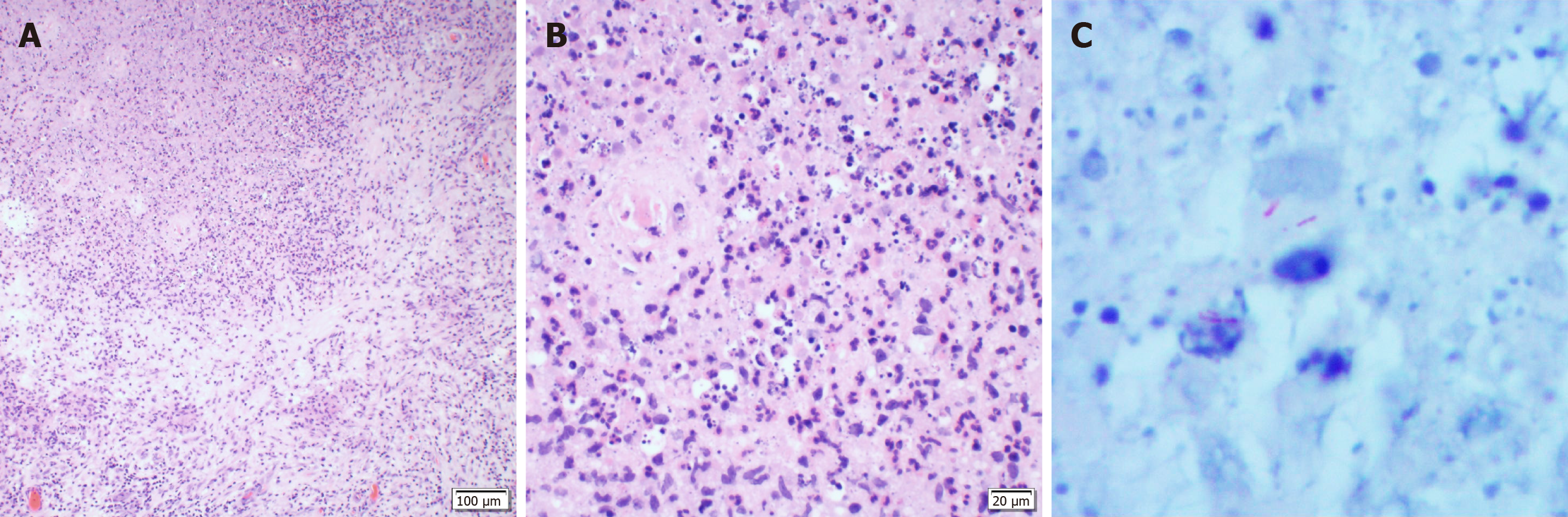
A 23-year-old male presented with fever accompanied by nausea and vomiting lasting for 2 mo and was then diagnosed with tubercular meningitis. After anti-TB treatment, his symptoms were significantly improved. However, 2 mo after the diagnosis of tubercular meningitis, the patient felt numbness below the costal arch level, which lasted for 1 wk, and he paid no attention to this symptom. What followed was paraplegia and urine/fecal incontinence. Magnetic resonance imaging of the thoracic spine showed a ring-enhanced intramedullary cord lesion at T8-T9. Lesion exploration showed enlargement of the spinal cord at T8-T9, and the lesion could be observed by incision. The lesion was adhered to the peripheral tissue and was grayish-white and tough with a poor blood supply and a diameter of approximately 0.8 cm. The lesion was resected completely. The results of pathological examination by both hematoxylin-eosin staining and acid-fast bacilli staining confirmed TB, accompanied by acute and chronic suppurative inflammation and granulation tissue formation. The patient was instructed to continue anti-TB treatment after the operation, but he did not follow the medical advice. Follow-up continued for ten years, the patient had persistent paraplegia, the numbness disappeared and urine/fecal sensation recovered.
Although TB is a kind of benign disease, some cases progress rapidly. Moreover, spinal intramedullary TB may seriously endanger quality of life and still needs timely diagnosis and proper treatment.
Core Tip: Tuberculosis mostly attacks the lungs, and extrapulmonary tuberculosis involving the central nervous system is rare. However, we should still pay attention to these cases in order to timely diagnose and properly treat. We report a case of a young male patient diagnosed with tuberculous meningitis. His disease progressed and involved the spinal cord, leading to paraplegia and urine/fecal incontinence. Unfortunately, after surgical resection of the spinal intramedullary lesion, the paraplegia failed to recover, and only urine/fecal sensation recovered. As a result, the patient remained in a wheelchair for ten years after the operation.
- Citation: Qu LM, Wu D, Guo L, Yu JL. Paraplegia from spinal intramedullary tuberculosis: A case report. World J Clin Cases 2020; 8(24): 6353-6357
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6353.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6353
According to global data, India has the highest incidence of tuberculosis (TB), which is mainly pulmonary TB[1]. While the incidence of cases of pulmonary TB has shown a downward trend in China, these are not uncommon[2,3]. TB of the central nervous system accounts for approximately 1% of all cases of TB, and 50% of these cases involve the spine[4]. Intramedullary involvement is rare in extrapulmonary TB, and less than 50 cases of this disease have been reported in the literature. The clinical manifestations of spinal intramedullary TB are similar to those of intramedullary spinal cord tumors with diverse manifestations[5]. Although spinal intramedullary TB is a kind of benign disease, timely diagnosis and proper treatment are still needed to achieve a better prognosis. We retrospectively collected the only case of spinal intramedullary TB confirmed by pathological examination at the First Hospital of Jilin University from 2010 to 2020, reported as follows.
The patient was a 23-year-old male who presented with fever accompanied by nausea and vomiting lasting for 2 mo. He had paraplegia and urine/fecal incontinence lasting for 7 d.
Two months ago, the patient was diagnosed with tubercular meningitis, and his symptoms improved obviously after anti-TB treatment. Seven days ago, he felt numbness below the costal arch level followed by paraplegia and urine/fecal incontinence.
The patient had no significant past medical history or surgical history and did not take any medications.
His family members denied a history of TB.
The temperature was 37.4 °C, the heart rate was 80 beats per minute, the respiratory rate was 16 breaths per minute and the blood pressure was 126/97 mmHg. The patient had clear consciousness and clear and fluent speech. His sensations of pain, warmth and deep stimuli were absent below the costal arch level. The muscular tension and tendon reflexes of the lower limbs were absent with grade 0 muscle strength. The bilateral Babinski sign was negative.
The laboratory examination findings were all within normal limits, including the complete blood count, routine urine test results and liver function test results. The results of hepatic serology were also negative. The fasting blood glucose level increased to 6.43 mmol/L (3.9-6.1 mmol/L). Neither lung digital radiography nor thoracic vertebrae digital radiography showed involvement on radiography.
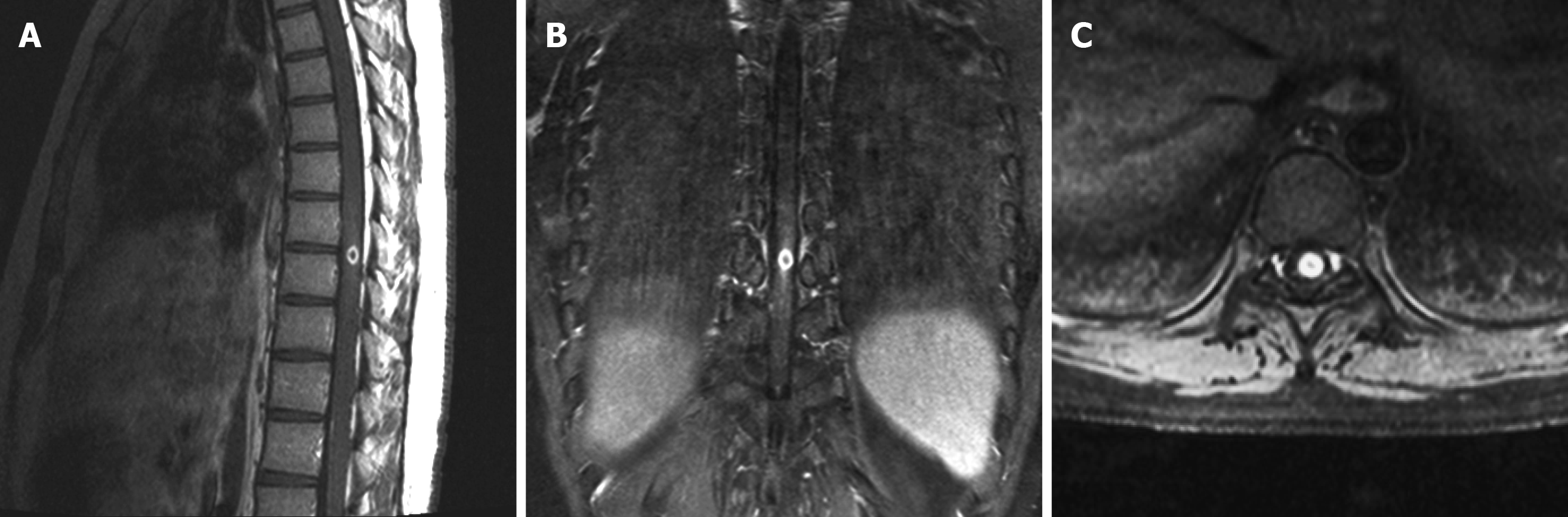
Magnetic resonance imaging (MRI) of the thoracic spine showed a ring-enhanced intramedullary cord lesion at T8-T9 (Figure 1).
There is a possibility of tumor but need to exclude nontumor disease.
Spinal intramedullary TB with acute and chronic suppurative inflammation and granulation tissue formation.
Surgical resection was performed.
After the operation, the patient stopped anti-TB treatment. Follow-up continued for ten years. The patient had persistent paraplegia, the numbness disappeared and urine/fecal sensation recovered without new TB lesions.
TB can involve the central nervous system, accounting for approximately 10% of all cases, and it can occur due to latent infection reactivation, transmission from organ donors or new nosocomial infections. Most cases of central nervous system TB are intracranial TB, while spinal intramedullary TB is even rarer with a ratio between the two at approximately 42:1[6]. The pathways by which Mycobacterium tuberculosis reach the spinal cord include hematogenous dissemination and cerebrospinal fluid. While the probability of spinal intramedullary TB in the thoracic, cervical and lumbar segments decreases successively, intramedullary TB can also occur near the end of the spinal cord and in the medullary cone[7]. The spinal intramedullary TB focus in this case was located in the intramedullary cord at T8-T9.
In some cases of spinal intramedullary TB, there are clinical manifestations of pulmonary or systemic TB, and recent history of tubercular meningitis is not uncommon. In this patient, the disease involved the spinal cord after the onset of tubercular meningitis for 2 mo. There have been a few case reports describing intramedullary suppurative and subdural abscesses[8]. The postoperative pathological examination in this case revealed many neutrophils in the lesion as well as granulation tissue formation, indicating the trend of suppurative inflammation and abscess formation.
Patients with spinal intramedullary TB often present with signs of spinal cord compression, such as progressive lower limb weakness, paresthesia, quadriplegia, paraplegia and bladder and bowel dysfunction. However, as reported in the literature, almost all of these symptoms resolved in patients who underwent surgical resection of the lesion. The urine/defecation function recovered to normal, and the muscle strength of the lower limbers recovered to grade 4. Unfortunately, the paraplegia in our reported 23-year-old male patient failed to recover after surgical resection of the spinal intramedullary lesion. His urine/fecal sensation recovered, but he could still not excrete on his own. Furthermore, he remained in a wheelchair for 10 years after the operation. Cases of such poor postoperative conditions have rarely been reported. This case us unusual because the pathological examination showed acute suppurative inflammation in the lesion, which had already formed granulation tissue. Whether the above pathological changes induced the failure to recover from the paraplegia needs to be further discussed.
The diagnosis of spinal intramedullary TB requires the combination of clinical, imaging and pathological examinations. Special attention should be paid to this disease in patients with medical history of pulmonary TB or systemic TB, especially those with immunodeficiency or a history of organ transplantation. In terms of imaging, MRI is valuable for diagnosis, while pathological examination is the most accurate diagnostic method. The criteria for the diagnosis of TB under microscopy are caseous necrosis, epithelioid nests and Langhans giant cells (Figure 2). But in different cases or stages, there will be different manifestations, and the proportion of these three changes will vary greatly. Some cases mainly show caseous necrosis, while other cases show proliferative lesions dominated by epithelioid cell masses. TB is often accompanied by acute and chronic inflammation as well, such as the acute infection and granulation tissue formation reported in this paper.
The treatment of spinal intramedullary TB mainly consists of anti-TB drugs. In addition, it has been reported that steroids in combination with anti-TB drugs have achieved positive clinical results[9]. Abnormal reactions to anti-TB drugs, such as the enlargement of existing tuberculomas or emergence of new tuberculomas as the treatment begins, have been reported in a small number of cases of spinal intramedullary TB. This is believed to be the result of increased inflammation caused by the anti-TB drugs relieving cell-mediated immunosuppression[10]. The course of disease in our case may be in accordance with this theory. Surgical indications include paralysis due to spinal compression or increasing spinal intramedullary lesions despite anti-TB drug treatment or pathological findings in patients with an unclear diagnosis indicating the need for lesion excision.
Spinal intramedullary TB is extremely rare among cases of the central nervous system TB, and in these cases, the clinical manifestations are similar to subacute myelopathy. The diagnosis of spinal intramedullary TB is based on clinical features, MRI findings and pathological and microbiological examination. Most patients have a good prognosis after surgical resection of the lesion. However, patients whose pathological examinations show acute suppurative inflammation in the lesion, which has already formed granulation tissue, may have poor prognosis, such as the case we reported.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: García-Elorriaga G S-Editor: Chen XF L-Editor: Filipodia P-Editor: Li JH
| 1. | Rabha P, Pandey A. Prospective study of reactive tubercular arthritis in patients with pulmonary and extrapulmonary TB. J Assoc Physicians India. 2020;68:72. [PubMed] |
| 2. | Wang YY, Xie BD. Progress on Diagnosis of Tuberculous Meningitis. Methods Mol Biol. 2018;1754:375-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Xu B, Zhang Y, Yu J. Brainstem tuberculous abscesses successfully treated by microsurgical excision: A case report and review of the literature. Oncol Lett. 2017;13:2708-2712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Schaller MA, Wicke F, Foerch C, Weidauer S. Central Nervous System Tuberculosis : Etiology, Clinical Manifestations and Neuroradiological Features. Clin Neuroradiol. 2019;29:3-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 115] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 5. | Varghese P, Abdul Jalal MJ, Kandathil JC, Mathew IL. Spinal Intramedullary Tuberculosis. Surg J. 3:e53-e57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Ghali MGZ, Srinivasan VM, Kim MJ, Malik A. Spinal Intramedullary Tuberculosis with Concurrent Supra- and Infratentorial Intracranial Disease in a 9-Month-Old Boy: Case Report and Comprehensive Review of the Literature. World Neurosurg. 2017;106:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Liu J, Zhang H, He B, Wang B, Niu X, Hao D. Intramedullary Tuberculoma Combined with Abscess: Case Report and Literature Review. World Neurosurg 2016; 89: 726.e1-726. e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Bhandari A, Bhandari H, Shukla R, Giri P. Phlyctenular conjunctivitis: a rare association with spinal intramedullary tuberculoma. BMJ Case Rep. 2014;2014. [PubMed] [DOI] [Full Text] |
| 9. | Kroesen VM, Rodríguez-Martínez P, García E, Rosales Y, Díaz J, Martín-Céspedes M, Tapia G, Sarrias MR, Cardona PJ, Vilaplana C. A Beneficial Effect of Low-Dose Aspirin in a Murine Model of Active Tuberculosis. Front Immunol. 2018;9:798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Das KK, Jaiswal S, Shukla M, Srivastava AK, Behari S, Kumar R. Concurrent cerebellar and cervical intramedullary tuberculoma: Paradoxical response on antitubercular chemotherapy and need for surgery. J Pediatr Neurosci. 2014;9:162-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |