Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6322
Peer-review started: August 31, 2020
First decision: September 13, 2020
Revised: September 26, 2020
Accepted: October 13, 2020
Article in press: October 13, 2020
Published online: December 26, 2020
Processing time: 110 Days and 1.4 Hours
Uterine rupture is a serious obstetric emergency, a severe event, and a serious threat to maternal and fetal life. It is a rare and not well characterized by the fact that multiple operations of uterine cavities contribute to uterine rupture during pregnancy. Atypical uterine rupture is easily misdiagnosed as other obstetric or surgical diseases. In current guidelines, abdominocentesis is a contraindication for late pregnancy. Therefore, the cases presented in this report provide new ideas for clinical diagnosis and treatment of uterine rupture.
Case 1, a 34-year-old woman (gravida 5, para 2), 32 wk and 4 d of gestation, presented with acute upper abdominal pain for 8 h with nausea and vomiting. Computed tomography (CT) revealed pelvic and abdominal effusion. We extracted 3 mL unclotted blood from her abdominal cavity. An emergency caesarean section was performed. A uterine rupture was found, and the fimbrial portion of the left fallopian tube was completely adhered to the rupture. The prognosis of both the mother and the infant was good. Case 2, a 39-year-old woman (gravida 10, para 1) at 34 wk and 3 d of gestation complained of persistent lower abdominal pain for half a day. Her vital signs were normal. CT revealed a high probability of pelvic and abdominal hemoperitoneum. We extracted 4 mL dark red blood without coagulation. An emergency laparotomy was performed. Uterine rupture was identified during the operation. Postoperative course in both the mother and infant was uneventful.
For pregnant women in the second or the third trimester with persistent abdominal pain, abdominal effusion, fetal distress and even fetal death, the possibility of uterine rupture should be highly suspected. CT can identify acute abdominal surgical or gynecological and obstetric diseases. Abdominocentesis is helpful for diagnosing and clarifying the nature of effusion, but its clinical value need to be confirmed by further clinical studies.
Core Tip: With the full implementation of two-child policy in China, the prevalence of uterine rupture has shown an increasing trend. Atypical uterine rupture is easily misdiagnosed as other obstetric or surgical diseases. For atypical uterine rupture, abdominocentesis can be used to make a diagnosis. We present two atypical cases of uterine rupture, and explore risk factors, clinical manifestations, early diagnosis, prevention and treatment of uterine rupture.
- Citation: Deng MF, Zhang XD, Zhang QF, Liu J. Uterine rupture in patients with a history of multiple curettages: Two case reports. World J Clin Cases 2020; 8(24): 6322-6329
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6322.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6322
Uterine rupture is the tearing of the corpus or the lower segment of uteri during pregnancy or delivery. Untimely diagnosis and treatment may directly endanger maternal and fetal life. Uterine rupture during pregnancy is a rare complication and is usually associated with trial of labor after previous cesarean delivery[1]. Any previous history of uterus operation, such as myomectomy or other surgical interventions are also important risk factors. Other risk factors include operation of multiple uterine cavities, abnormal pregnancy-labor history, hypoplasia of the uterus and so on. Uterine rupture caused by multiple operations of uterine cavities during pregnancy is rarer and more atypical than spontaneous uterine rupture.
Here, we present two atypical cases of uterine rupture. One is at 32 wk of gestation in a 34-year-old woman with a history of two prior cesarean sections and two curettages, and the other is at 34 wk of gestation in a 39-year-old woman with a history of laparoscopic salpingectomy (LPSC) and six curettages. In association with related literature review, we discuss risk factors, clinical manifestations, therapy and prevention of uterine rupture.
Case 1: A 34-year-old woman (gravida 5, para 2) at 32 wk and 4 d of gestation was admitted to the emergency department of our hospital on December 8, 2019 because of acute upper abdominal pain for 8 h with nausea and vomiting.
Case 2: A 39-year-old woman (gravida 10, para 1) at 34 wk and 3 d of gestation complained of persistent lower abdominal pain for half a day before admission to the obstetrics department of our hospital on December 19, 2019.
Case 1: There were no complaints of fever, vaginal bleeding, or any other symptoms.
Case 2: There were no other symptoms.
Case 1: She had a history of two caesarean sections and curettages and denied a history of trauma.
Case 2: Her surgical history included conservative operation and LPSC for two tubal pregnancies and six curettages.
Case 1: The Personal and family history was unremarkable.
Case 2: The Personal and family history was unremarkable.
Case 1: On admission to the hospital, the patient appeared pale and felt faint. She was in a forced sitting position. Upon physical examination, her temperature was 36 °C, her respiratory rate was 20 breaths per minute, her blood pressure was 86/54 mmHg, and her pulse rate was 85 bpm. An abdominal examination revealed obvious tenderness and rebound tenderness in the upper abdomen, and we did not detect uterine contractions. The fetal heart rate was 135 bpm.
Case 2: Her vital signs were normal. The abdomen was firm, and there was sharp tenderness and rebound pain in the lower abdomen, especially in the right lower quadrant. A vaginal examination revealed that the cervix was closed, and the fetal membrane was intact. There was no vaginal bleeding or fluid.
Case 1: Blood tests revealed the following: White blood cells (WBC), 19.71 × 109/L; neutrophils, 92.4%; red blood cells, 3.05 × 1012/L; hemoglobin (Hb), 102.00 g/L; platelets, 248 × 109/L. C-reaction protein (CRP) was normal. Tests for serum amylase and lipase concentrations, coagulation and liver function yielded normal results.
Case 2: Blood tests showed elevated white blood cell count, neutrophilic granulocyte percentage, platelet count, and Hb level at 13.58 × 109/L, 92.4%, 192 × 109/L, and 114 g/dL, respectively. CRP was 3.68 mg/L and procalcitonin was < 0.05 ng/mL. Fetal non-stress test showed a reactive type. Examinations of blood electrolytes, coagulation profile, renal function, thyroid function, and blood glucose were unremarkable.
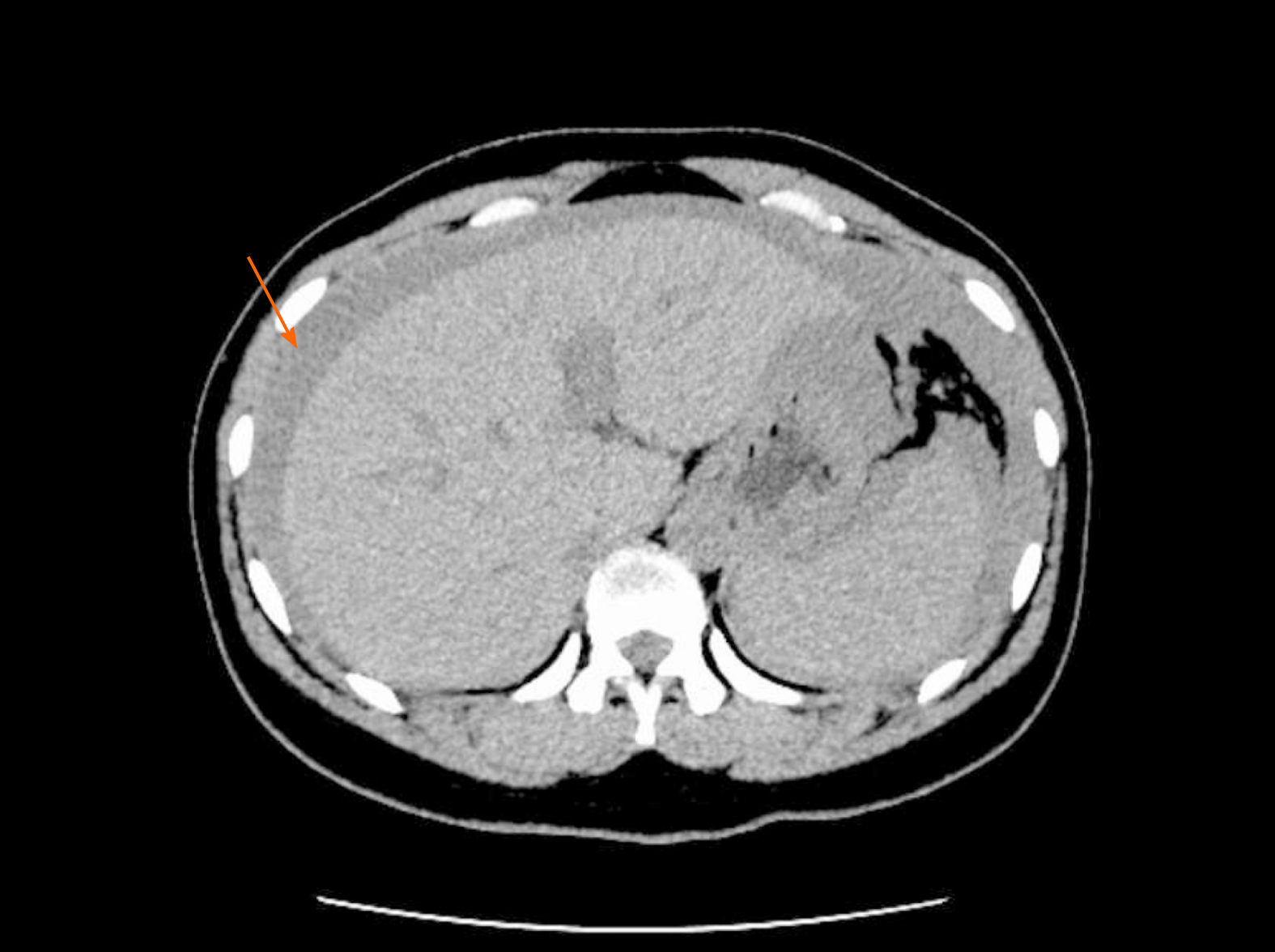
Case 1: Obstetric ultrasonography showed a live fetus in a cephalic presentation. The placental and amniotic fluid volumes were normal. Abdominal ultrasonography showed abdominal effusion, and computed tomography (CT) revealed pelvic and abdominal effusion (Figure 1). Chest CT examination showed exudative lesions in both lungs.
Case 2: Fetal ultrasonography suggested a single live fetus, equivalent to approximately 34 wk of pregnancy. There were no placental abnormalities. An ultrasound of the abdomen showed abdominal effusion. Pelvic and abdominal CT revealed a high probability of pelvic and abdominal hemoperitoneum (Figure 2).
Based on the patient’s medical history, physical examination and auxiliary examination, we performed abdominocentesis on the patient, and extracted 3 mL unclotted blood from her abdomen. We then decided to perform emergency cesarean section under general anesthesia. During surgery, we found hemoperitoneum (approximately 900 mL) in the abdominal cavity. A complete rupture of the uterus could be seen at the fundus of the left posterior wall of the uterus. The rupture was approximately 1.5 cm long, with active bleeding, and the fimbrial portion of the left fallopian tube had completely adhered to the rupture (Figure 3). The previous caesarean scar was found intact. The right oviduct and both ovaries were normal. A diagnosis of complete uterine rupture was confirmed.
We performed abdominocentesis on the patient, and extracted 4 mL dark red blood without coagulation. Cesarean section was performed immediately under general anesthesia. During the operation, hemoperitoneum (approximately 800 mL) was collected. A local bulge (4 cm × 4 cm) was observed in the anterior wall of the right corner of the uterus, which was only composed of the serous layer and some of the weak muscle layers of the uterus (Figure 4). There was a small rupture of approximately 0.5 cm on the surface with active bleeding (Figure 5). The right oviduct was defective, and the left oviduct and both ovaries were normal. At the same time, we found three fibroids, one (3 cm × 3 cm) was in the anterior wall of the uterus and two (4 cm × 4 cm and 1 cm × 1 cm) in the posterior wall of the uterus. Uterine rupture was confirmed.
Uterine repair and left salpingectomy were performed. A premature infant was delivered, the 1-min and 5-min Apgar score was 3, the 15-min Apgar score was 8, and the baby was transferred to the neonatal intensive care unit. The patient was transfused with 1.5 U packed red blood cells on the first postoperative day, and the abdominal drainage tube was removed on the second postoperative day.
We then repaired the uterus with absorbable sutures and performed a myomectomy. A male infant was delivered (1 min and 5 min Apgar scores were 8 and 10, respectively; weight 2150 g). The patient was transfused with 2 U packed red blood cells on the second postoperative day, and the abdominal drainage tube was removed on the seventh postoperative day.
The pathological results showed chronic tubal inflammation, with tissue adhesion of the decidua. The mother was discharged after 9 d. The infant was discharged on day 23 of life. Follow-up assessments of the mother and the infant on the 42nd postpartum day showed normal results, and an ultrasound examination of the uterus was normal.
The woman was discharged on her ninth postoperative day. The baby was transferred to the newborn intensive care unit and discharged from the hospital after 11 d. The results of pathological examination showed that decidual tissue could be seen in the ruptured uterine tissue, and uterine leiomyoma with red degeneration was observed. Postoperative course at 2-mo follow-up was uneventful in both the mother and infant.
With the implementation of the two-child policy in China, the prevalence of uterine rupture is increasing. The two cases in the present report were eventually diagnosed with complete uterine rupture. Complete uterine rupture of the uterus refers to the rupture of all the layers of the uterus, connecting the uterine cavity with the abdominal cavity[2]. It is a rare obstetric complication with a prevalence between 2.4 and 3.0 per 10000 deliveries[3,4]. In 2018, a multicenter study conducted by Vandenberghe et al[5] showed that the prevalence of uterine rupture was 0.033%.
Healthy and strong connective tissue, and healthy uterus have minimal uterine rupture risk during pregnancy[6]. The risk factors for uterine rupture include trial of labor after previous caesarean delivery, uterine operation history (such as multiple caesareans, myomectomy[6] and laparoscopic salpingectomy), multiple curettages, cephalopelvic disproportion, advanced maternal age, macrosomia, a shorter interval between deliveries, overdue pregnancy, placental factors and so on[1,7-8]. However, for patients with an unscarred uterus, the risk factors may be associated with the weakness of the myometrium due to trauma, congenital anomaly, or multiple gestations and the use of uterotonic drugs[9]. In our two cases of complete uterine rupture, the reason may be related to damage to the myometrium caused by multiple curettages. In the first case, the possibility of uterine perforation during one of the curettages, followed by the fallopian tube blocking the rupture and affecting the healing of the uterine rupture, can not be ruled out.
The early diagnosis of uterine rupture is difficult. Typical clinical manifestations include abdominal pain, abnormalities of the fetal heart and vaginal bleeding. These symptoms are nonspecific and easily misdiagnosed as other obstetric or surgical diseases. Additionally, the signs of uterine rupture may differ depending on the site of rupture as well as the time since onset[10]. Most ruptures occur in the lower uterine segment[11]. In these cases[12,13], the fundus is the most common site of rupture. In our cases, the rupture occurred in the fundus uteri or cornua uteri, which is an atypical site. For patients with a history of caesarean section, a previous caesarean scar is intact, which could easily mislead the clinician's judgement.
For the early diagnosis of uterine rupture, we should determine whether the patient presents with any risk factors and whether the patient complains of persistent abdominal pain, with emphasis on physical examination of the mother, and hemodynamic and fetal heart rate monitoring. At the same time, pelvic and abdominal ultrasonography should be performed to determine whether there are uterine rupture and abdominal effusion. If necessary, abdominocentesis under the guidance of B-ultrasound can be performed to determine whether the effusion is blood. Treatment is then carried out based on the above factors.
Our patient had a past history of uterine surgery (the first was a caesarean section; the second was LPSC for an ectopic pregnancy) and curettage for abortion. They had persistent abdominal pain and showed few classic symptoms of localized peritonitis on presentation. The fetal heart rate (FHR) was normal. Laboratory reports showed an increased WBC and neutrophilic granulocyte percentage. Abdominal ultrasonography showed abdominal effusion. The accuracy of ultrasound can often be affected by low resolution, gas in the enteric cavity, body position, and anatomical distortion of the abdomen and pelvis caused by the gravidity, but ultrasound, as a fast and noninvasive examination, still plays an important role in the early diagnosis of uterine rupture[7,14,15]. CT has a wide scanning range that can observe the conditions of the other abdominal and pelvic organs, and provide evidence for identifying acute abdominal surgical or gynecological and obstetric diseases such as acute pancreatitis and ovarian torsion. Bhoil et al[16] have suggested that CT is more useful than ultrasound in the diagnosis of uterine rupture. To clarify the diagnosis, an emergency CT examination was performed in our cases and revealed a high probability of pelvic and abdominal hemperitoneum. To provide a direct basis for an exploratory laparotomy, abdominocentesis should be considered if the patient’s condition permits.
In current guidelines, abdominocentesis is a contraindication for late pregnancy. However, for atypical uterine rupture, abdominocentesis can be used to make a diagnosis. Before the operation, we need to evaluate the patient's condition first and then perform the operation if the patient's condition permits. Then, we need to communicate with the patient about the risks of abdominocentesis, and the operation can only be carried out after the patient agrees and signs consent forms. For pregnant women, we should only puncture under the guidance of B-ultrasound to avoid important organs injury and to get the exact location with an abundant amount of fluid. There are few cases of abdominocentesis in the literature that can be used to assist in the diagnosis of uterine rupture, and its clinical value remains to be confirmed by more clinical studies.
The key to the treatment of uterine rupture is to shorten the diagnosis time as much as possible. The surgical mode of the parturient depends on the type of uterine rupture, the position of the rupture, the length of the rupture, the rupture time, the infection degree of the rupture, bleeding, the physical tolerance of the parturient and the willingness of the woman to give birth again. A uterus-saving procedure is performed only in patients whose uterus is viable and only when it is deemed to not threaten the life of the patient[17]. In addition, a rare method was used to immediately repair the uterine defect, leading to a prolonged pregnancy[18,19]. In the present two cases, the uterine rupture was neat and small, and the bleeding was controllable. The patients and their families requested to preserve the uterus. Then, we repaired the uterus with 1-0 interrupted sero-muscular sutures after removing the fetus and successfully retained the uterus.
In our clinical work, prevention is the primary means to prevent uterine rupture. To prevent uterine rupture during pregnancy, the physicians must first accurately assess the indications for caesarean section and reduce the rate of first caesarean section as much as possible. In addition, to establish a complete health care manual for pregnant women, regular antenatal examination and obstetric outpatient management of high-risk pregnant women, is recommended. If necessary, ultrasonography or MRI can be performed to assess the thickness and continuity of scars in suspicious areas[7].
In recent years, the incidence of uterine rupture has gradually increased, higher in developing countries than in developed countries[4-5], which may be related to the increase in the number of scarred uteruses[3]. In addition to the rupture of the scar of the original incision, the possibility of rupture of other parts of the uterus should be considered. Abdominocentesis is helpful for diagnosis and clarifying the nature of effusion. Early diagnosis and timely treatment help to achieve good outcomes in pregnant women and neonates. When women present with a risk of uterine rupture, we should strengthen the management and supervision during pregnancy, strive to achieve early diagnosis and treatment and improve the prognosis of mother and child.
We would like to thank these two patients for allowing us to share their cases and using their picture and we are also grateful to all of our team members who were involved in the management of the cases.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hortu I S-Editor: Gao CC L-Editor: MedE-Ma JY P-Editor: Zhang YL
| 1. | Halassy SD, Eastwood J, Prezzato J. Uterine rupture in a gravid, unscarred uterus: A case report. Case Rep Womens Health. 2019;24:e00154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Ofir K, Sheiner E, Levy A, Katz M, Mazor M. Uterine rupture: risk factors and pregnancy outcome. Am J Obstet Gynecol. 2003;189:1042-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 121] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Al-Zirqi I, Stray-Pedersen B, Forsén L, Daltveit AK, Vangen S. Uterine rupture: trends over 40 years. BJOG. 2016;123:780-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Vilchez G, Nazeer S, Kumar K, Warren M, Dai J, Sokol RJ. Contemporary epidemiology and novel predictors of uterine rupture: a nationwide population-based study. Arch Gynecol Obstet. 2017;296:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Vandenberghe G, Bloemenkamp K, Berlage S, Colmorn L, Deneux-Tharaux C, Gissler M, Knight M, Langhoff-Roos J, Lindqvist PG, Oberaigner W, Van Roosmalen J, Zwart J, Roelens K; INOSS (the International Network of Obstetric Survey Systems). The International Network of Obstetric Survey Systems study of uterine rupture: a descriptive multi-country population-based study. BJOG. 2019;126:370-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Hortu İ, Akdemir A, Şendağ F, Öztekin MK. Uterine rupture in pregnancy after robotic myomectomy. Turk J Obstet Gynecol. 2015;12:188-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Zhao B, Wang Y, Zhang Y. Uterine rupture in patients with a history of laparoscopy or hysteroscopy procedures: Three case reports. Medicine (Baltimore). 2019;98:e15491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Guiliano M, Closset E, Therby D, LeGoueff F, Deruelle P, Subtil D. Signs, symptoms and complications of complete and partial uterine ruptures during pregnancy and delivery. Eur J Obstet Gynecol Reprod Biol. 2014;179:130-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 9. | You SH, Chang YL, Yen CF. Rupture of the scarred and unscarred gravid uterus: Outcomes and risk factors analysis. Taiwan J Obstet Gynecol. 2018;57:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Sun Y, Huang J, Kong HF. Spontaneous rupture of unscarred uterus in the third trimester after in vitro fertilization-embryo transfer because of bilateral salpingectomy: A case report. Medicine (Baltimore). 2019;98:e18182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Islam A, Shah AA, Jadoon H, Fawad A, Javed M, Abbasi AN. A Two-Year Analysis Of Uterine Rupture In Pregnancy. J Ayub Med Coll Abbottabad. 2018;30(Suppl 1):S639-S641. [PubMed] |
| 12. | Mannini L, Sorbi F, Ghizzoni V, Masini G, Fambrini M, Noci I. Spontaneous Unscarred Uterine Rupture at 15 Weeks of Pregnancy: A Case Report. Ochsner J. 2016;16:545-547. [PubMed] |
| 13. | Sun HD, Su WH, Chang WH, Wen L, Huang BS, Wang PH. Rupture of a pregnant unscarred uterus in an early secondary trimester: a case report and brief review. J Obstet Gynaecol Res. 2012;38:442-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Aherne E, Beauchamp K, Maher N, Walsh T, Boyd W, Eogan M, Lawler L. "Showercap" Sign: Spontaneous Uterine Rupture in a Primiparous Woman. Ulster Med J. 2017;86:111-113. [PubMed] |
| 15. | Pontis A, Prasciolu C, Litta P, Angioni S. Uterine rupture in pregnancy: two case reports and review of literature. Clin Exp Obstet Gynecol. 2016;43:304-309. [PubMed] |
| 16. | Bhoil R, Surya M, Mistry KA. CT diagnosis of spontaneous uterine rupture at term, sonographic appearance of which was confused with placenta praevia. Ann Saudi Med. 2016;36:440-441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Ali MB, Ali MB. Late Presentation of Uterine Rupture: A Case Report. Cureus. 2019;11:e5950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Hawkins L, Robertson D, Frecker H, Berger H, Satkunaratnam A. Spontaneous uterine rupture and surgical repair at 21 weeks gestation with progression to live birth: a case report. BMC Pregnancy Childbirth. 2018;18:132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Leduc L, Monet B, Sansregret A, Gauthier R, Bourque J, Rypens F. Immediate closure of uterine wall following spontaneous rupture at 23 wk' gestation, allowing prolongation of pregnancy. Ultrasound Obstet Gynecol. 2016;48:534-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |