Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6190
Peer-review started: August 7, 2020
First decision: August 21, 2020
Revised: August 26, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: December 6, 2020
Processing time: 118 Days and 16.9 Hours
Poliomyelitis is an acute infection caused by an enterovirus, which primarily infects the human gastrointestinal tract. In general, patients with polio have no association with the occurrence of cancer. The present case study presents a rare case of poliomyelitis combined with primary breast cancer.
A 61-year-old woman who was diagnosed with poliomyelitis at 5 years old and confirmed invasive breast cancer by core needle biopsy (CNB) after hospitalization. The patient received a modified radical mastectomy and four cycles of chemotherapy with the TC (docetaxel and cyclophosphamide) regimen. The patient was also prescribed endocrine therapy without radiotherapy after chemotherapy. The patient had no evidence of lymphedema in the right upper extremities and no evidence of either regression or distant metastasis at the 1-year follow-up.
The pectoral muscles of patients with polio are easily damaged in traumatic procedures, such as CNB, local anesthesia for tumor excision, and general anesthesia for surgery. A CNB, modified radical mastectomy, and four cycles of TC chemotherapy were successfully completed for the present case and the adverse reactions were found to be tolerable. This case may indicate the relationship between breast cancer and polio, and the examination and treatment methods used could be used as a guide for similar cases in the future.
Core Tip: This is the first case report on poliomyelitis combined with primary breast cancer. Due to the poliomyelitis, the pectoral muscles of patients with polio are easily damaged in traumatic procedures, such as core needle biopsy (CNB), local anesthesia for tumor excision, and general anesthesia for surgery. A CNB, modified radical mastectomy, and four cycles of TC chemotherapy were successfully completed for the present case and the adverse reactions were found to be tolerable. This case may indicate the relationship between breast cancer and polio, and the examination and treatment methods used could be used as a guide for similar cases in the future.
- Citation: Wang XM, Cong YZ, Qiao GD, Zhang S, Wang LJ. Primary breast cancer patient with poliomyelitis: A case report. World J Clin Cases 2020; 8(23): 6190-6196
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6190.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6190
Poliomyelitis is an acute infectious disease caused by a neurotropic poliovirus. It primarily invades the motor nerve cells of the central nervous system, most commonly the motor neurons in the anterior horn of the spinal cord[1]. The majority of the patients affected are 1-6 years old. The main symptoms of poliomyelitis are fever, general malaise, myalgia, and varying degrees of flaccid paralysis with irregular distribution. The clinical manifestations of poliomyelitis vary, but include mild non-specific lesions, aseptic meningitis (non-paralytic poliomyelitis), and flaccid weakness of various muscle groups (paralytic poliomyelitis). In patients with poliomyelitis, due to the damage of the motor neurons in the anterior horn of the spinal cord, the muscles associated with the neurons lose their control over nerve regulation and atrophy occurs. Concurrently, atrophy also occurs in the subcutaneous fat, tendons, and bone, making the whole limb thinner. Nevertheless, China has made significant achievements in eradicating polio following the generation of the oral live attenuated polio vaccine[2]. In general, patients with polio are not associated with the occurrence of cancers and poliomyelitis-associated malignancies are rarely reported. Breast cancer is the most common type of cancer for women worldwide[3]. However, the rate of early detection of breast cancer is increasing due to the widespread use of breast magnetic resonance imaging (MRI)[4]. The present paper reports a cases of primary breast cancer in a patient with previous poliomyelitis.
A post-menopausal woman, aged 61 years, visited The Affiliated Yantai Yuhuangding Hospital of Qingdao University after finding a painless lump in the right breast 1 wk previously.
The patient felt a painless lump in the right breast while taking a bath accidentally.
The patient suffered from a poliovirus infection over 50 years ago, which was diagnosed as poliomyelitis. She gave birth at the age of 25 but did not breastfeed, and she experienced irregular menstrual cycles and had no family history of cancer. The patient is right-handed and can write and walk around without crutches or a wheelchair.
She was diagnosed with invasive breast cancer by core needle biopsy (CNB) after hospitalization. A physical examination of the patient revealed a 1.0 cm × 1.0 cm, 1 cm from the nipple, non-tender mass in the upper outer quadrant of the right breast. No mass was palpable in the left breast and no tumescent lymph node was palpable in the bilateral axilla and supraclavicular fossae. A general physical examination revealed that her vision was clear, and both eyeballs moved freely without diplopia or nystagmus in any direction. Her left limb muscle strength, muscular tension, and tendon reflex were normal, whilst the right limb muscle strength was reduced, and she experienced muscle hypotonia and tendon areflexia. Her abdomen was slightly protruded and the size of her liver and spleen was normal, while both lower limbs were not swollen.
Laboratory examinations were normal.
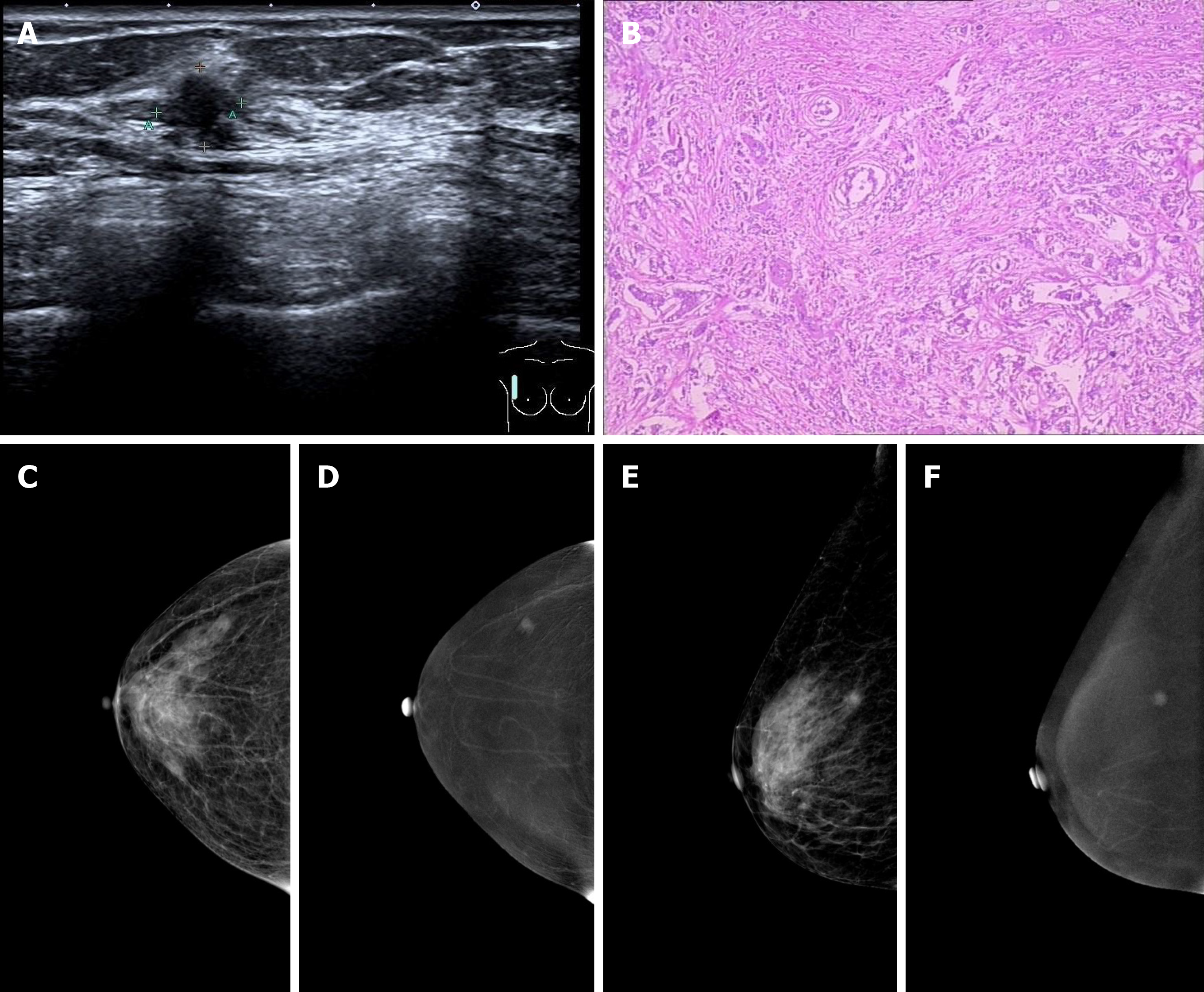
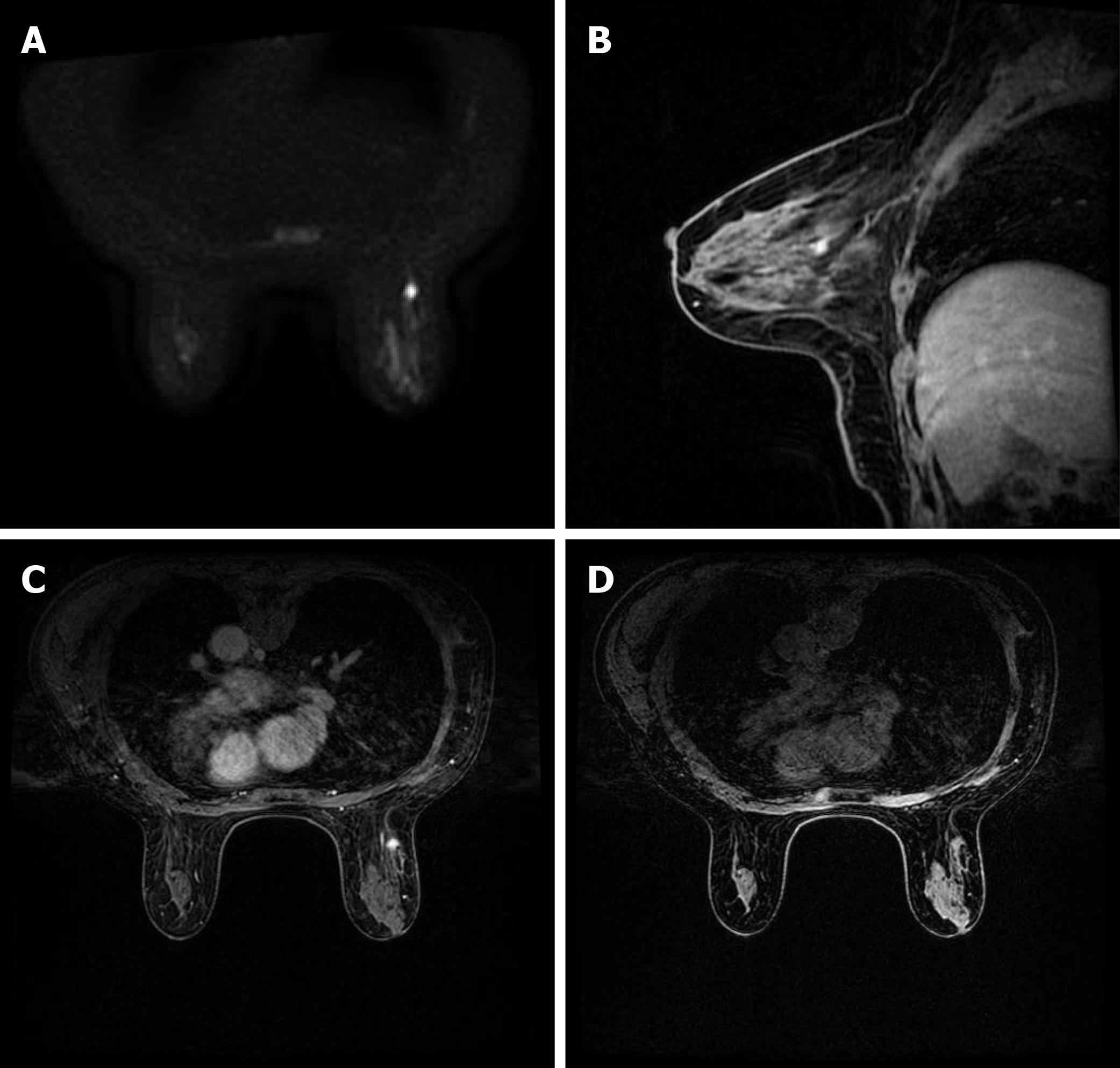
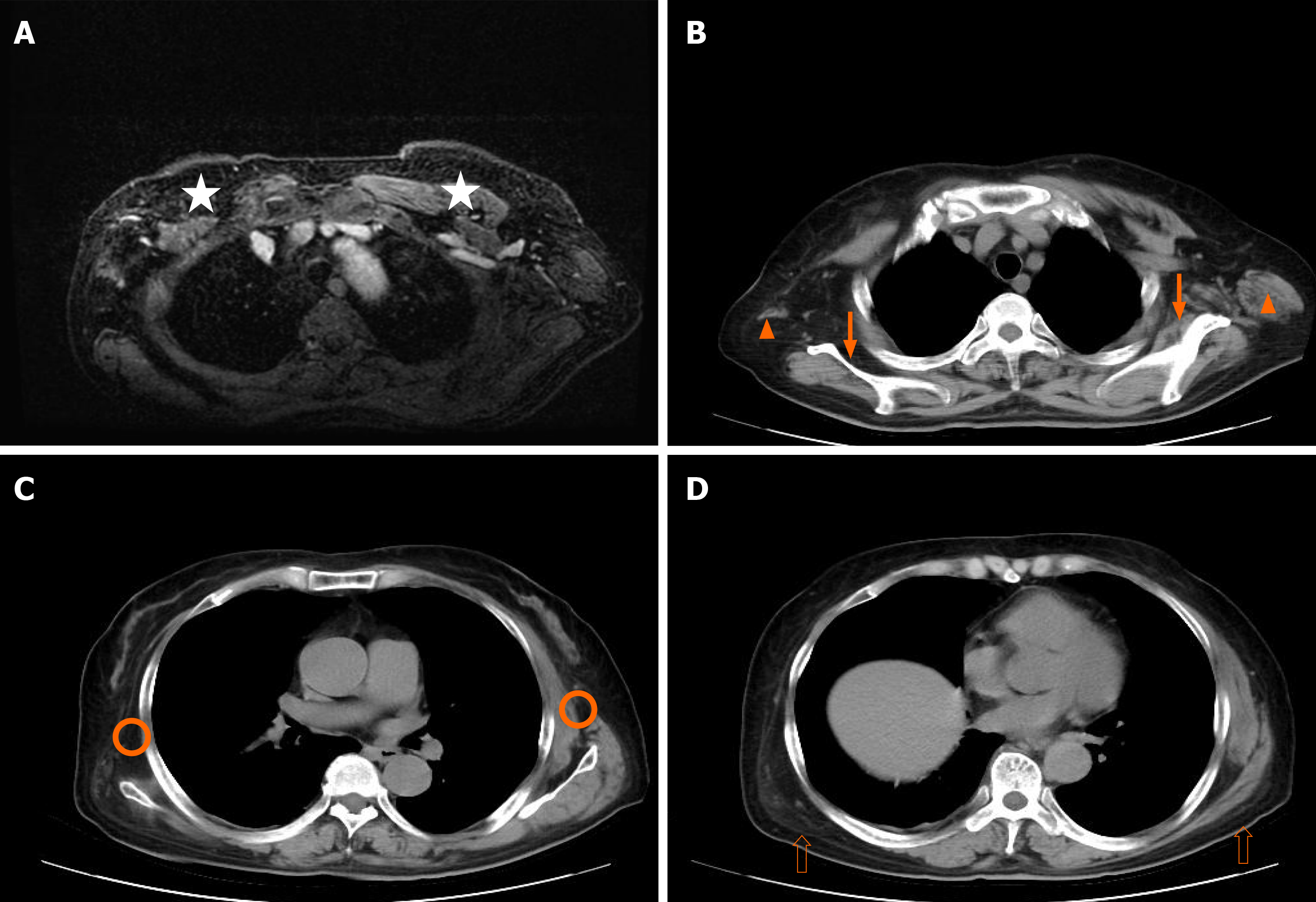
Breast ultrasound revealed a hypoechoic nodule approximately 0.8 cm × 0.8 cm in size in the upper outer quadrant of the right breast, with an irregular shape, obscure boundary, heterogenous internal echo, and punctate blood flow signals, which was classified as breast imaging reporting and data system (BI-RADS) 4b (Figure 1). However, no tumescent lymph node was detected in the right axillary or supraclavicular region. Preoperative contrast enhanced spectral mammography identified an irregular and hard-density mass of 1.0 cm × 1.0 cm in size in the upper outer quadrant of the right breast, which had an obscure boundary with no abnormal calcification, and was significantly enhanced and classified as BI-RADS 4b (Figure 1). A breast MRI scan revealed an ill-defined mass with uniform equal signal intensity. Axial diffusion weighted imaging (b = 800) identified the mass with high signal intensity. Axial and sagittal post-contrast fat-saturated T1-weighted MRI showed a 0.8 × 0.9 cm enhancing irregular mass at the 9-10 o'clock position, approximately 6 cm from the nipple (Figure 2). Finally, a chest computed tomography scan was used to identify the atrophy occurring in the right pectoral muscles (pectoralis major, pectoralis minor, subclavius, and serratus anterior), teres major, subscapularis muscle, and latissimus dorsi muscle (Figure 3).
Multidisciplinary team (MDT) recommended that she need adjuvant chemotherapy combined with endocrine therapy after surgery but have no need for radiotherapy.
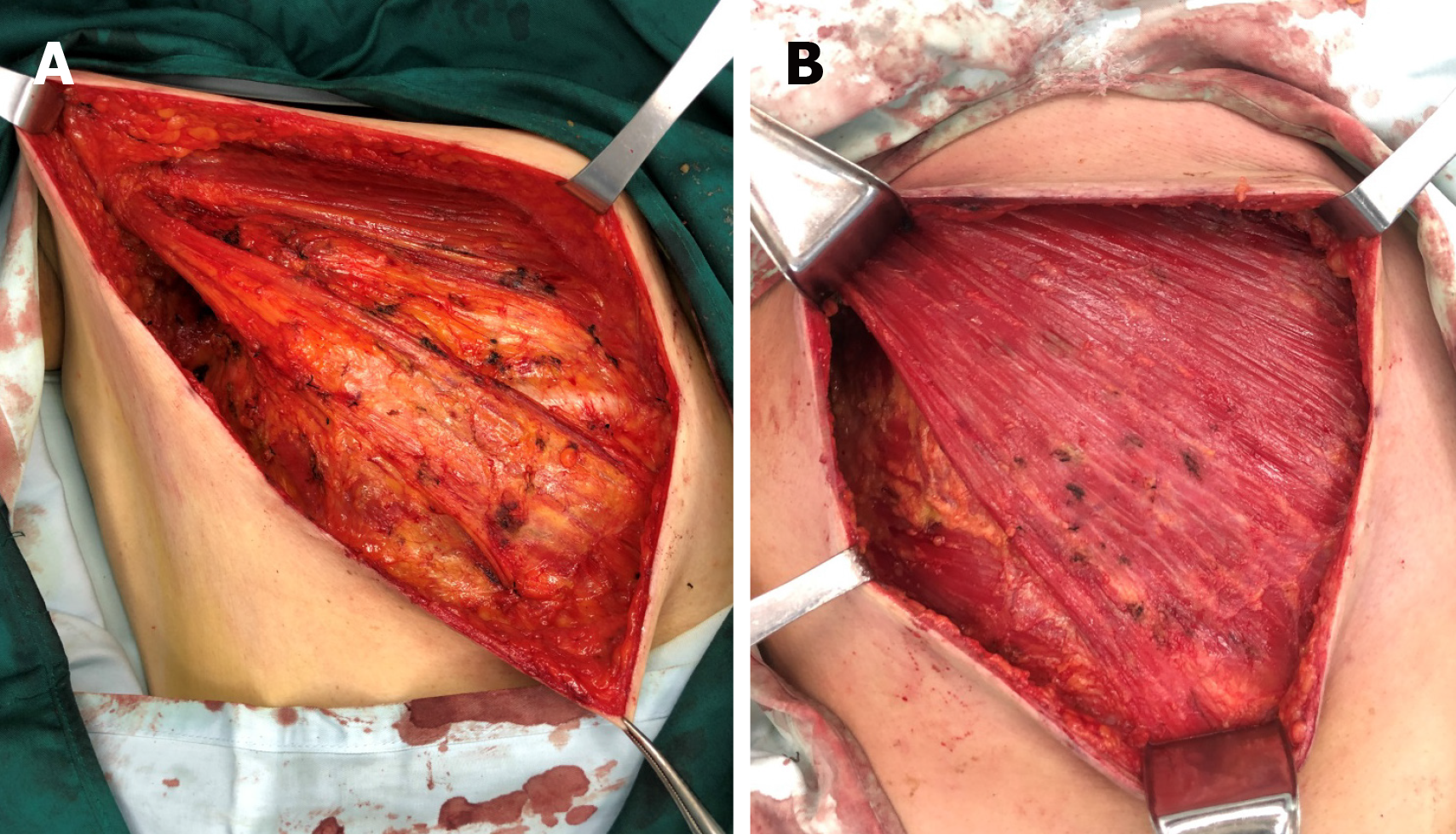
The final diagnosis was confirmed to be primary breast cancer combined with poliomyelitis.
As the patient had no desire to conserve the breast tissue, a mastectomy and sentinel lymph node biopsy for the right breast were performed under general anesthesia. An axillary lymph node dissection was performed because the sentinel lymph node biopsy was also positive. The pectoralis major, pectoralis minor, serratus anterior, and external intercostal muscles were discovered to be atrophying to varying degrees during the operation (Figure 4). Due to the pectoralis major muscle of the patient being atrophied, with no clear boundary being observed between the fat and fascia in the posterior space of the breast, there was a higher probability of injury occurring during the operation compared with normal patients (Figure 4).
The postoperative pathology revealed a grade II right breast invasive ductal carcinoma, in which the size of the lump was 0.9 cm × 0.9 cm. Immunohistochemical staining indicated that the carcinoma was positive for estrogen receptor (90% strongly positive) and progesterone receptor (10% weakly positive) and negative for human epidermal growth factor receptor 2. In addition, positive Ki-67 staining was observed in 40% of the tumor cells. No cancer cells were observed in the nipple and deep resection plane, and axillary lymph node dissection revealed cancer metastasis in only one sentinel lymph node. The patient was ultimately diagnosed with breast cancer in the right breast of luminal B subtype, pT1N1M0, stage IIa. A TC (75 mg/m2 i.v. docetaxel, and 600 mg/m2 i.v. cyclophosphamide on day 1) regimen was administered every 3 wk for 4 cycles following the operation, and she received the formal advice from the MDT that there was no need for radiotherapy following surgery. The patient was prescribed endocrine therapy consisting of 2.5 mg letrozole and 600 mg vitamin D3 once a day for 1 year (The endocrine therapy was planned for 5 years).
The patient exhibited no evidence of lymphedema in the right upper extremities and no signs of recurrence or distant metastasis at the 1-year follow-up. However, the functional abilities of the right upper extremities of the patient were significantly affected following the operation due to post-polio syndrome.
Polio (short for poliomyelitis) is an infectious disease caused by the poliovirus. Children under the age of five are the most infected age group compared with any other age group. According to the World Health Organization, 1/200 of people with polio experience permanent paralysis. However, as a result of the global polio eradication initiative of 1988, numerous countries and regions have now been certified polio-free. The polio vaccine was developed in 1953 and made available in 1957, which caused the cases of polio to significantly drop worldwide[5].
Polio can affect the nervous system and lead to partial or complete paralysis, which is caused by the poliovirus inhabiting the throat and intestines of infected individuals[1]. It can be spread directly by person-to-person contact, by contact with infected nasal or oral mucus or sputum, or through contact with infected feces. The incidence of the disease has been significantly reduced since the development of the polio vaccine. There are three basic types of polio infection: Subclinical infection, non-paralytic infection, and paralytic infection[6]. In total, approximately 95% of infections are classified as subclinical infections, which may be asymptomatic. Clinical poliomyelitis affects the central nervous system (brain and spinal cord), and is divided into non-paralytic and paralytic types, which may occur following the recovery from a subclinical infection. Currently, the aim of poliomyelitis treatment is to control the symptoms while the infection runs its course. The prognosis depends on the subtype of the disease (subclinical, non-paralytic, or paralytic) and the site of infection; for example, if the spinal cord and brain are not involved, > 90% of individuals completely recover[1,7-9].
However, approximately 1% of polio cases can develop into the paralytic type. Paralytic polio leads to the paralysis of the spinal cord (spinal polio), brainstem (bulbar polio), or both (bulbospinal polio). The initial symptoms are similar to those of non-paralytic polio; however, after a week or so, more severe symptoms begin to appear. These symptoms include the loss of reflexes, severe spasms, muscle pain, limb relaxation, temporary or permanent paralysis, and the deformation of the limbs. In addition, polio may recur following recovery, which can even happen 15 to 40 years later. The common symptoms of post-polio syndrome (PPS) include muscle and joint weakness, severe muscle pain, muscle atrophy, dyspnea, and dysphagia[9,10]; it is estimated that 25%-50% of polio survivors will experience PPS. Currently, there is no cure for polio, only treatment options aimed at alleviating the symptoms are available[10]. Heat and physical therapy are used to stimulate the muscles and antispasmodic drugs are provided to relax the muscles. While this can improve mobility, it cannot reverse permanent polio paralysis[7,10,11]. Thus, the most effective way to treat polio is through preventative measures such as vaccinations.
To date, there has been no direct association identified between cancer and poliomyelitis. Previous studies have reported that the incidence rate of tumors of the central nervous system in patients with poliomyelitis may increase, and the incidence of breast cancer and skin cancer was higher in female patients with poliomyelitis compared with the general population[12]. Another previous study suggested that poliovirus infection in colon cells may induce resistance to the development of colon cancer to some extent, which subsequently reduces the mortality of colon cancer[13]. However, further investigations are required to determine the relationship between poliomyelitis and cancer.
Although breast cancer is the most common type of malignancy diagnosed in women, to date, no previous studies have reported any cases of breast cancer due to poliomyelitis complications. In addition, there are no reports investigating the chemotherapy risk assessment in patients with polio. The pectoralis major and minor muscles during poliomyelitis usually atrophy to differing degrees, which causes the thinning of the chest. Therefore, traumatic procedures, such as CNB, local anesthesia for tumor excision, and general anesthesia for surgery should be performed with caution to avoid damaging the chest organs. Breast MRI can predict the features of tumor, pectoral muscle and axillary lymph node status, and the risk of recurrence after breast conserving surgery[14,15].
In conclusion, the present paper reports a case of breast cancer following poliovirus infection, and to the best of our knowledge, this is the first report demonstrating this occurrence. In addition, we did not find precedent of chemotherapy in almost all instances of reported poliomyelitis. The patient received a chemotherapy regimen of TC (75 mg/m2 i.v. docetaxel and 600 mg/m2 i.v. cyclophosphamide on 1st day) every 3 wk for 4 cycles following the operation and did not receive radiotherapy following the chemotherapy. The patient was also prescribed endocrine therapy consisting of 2.5 mg letrozole and 600 mg vitamin D3 once a day. After 1 year of follow-up, local recurrence and distant metastasis were not present, and the patient will continue to be monitored in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abd El-Razek A, Hanna S S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Kidd D, Williams AJ, Howard RS. Poliomyelitis. Postgrad Med J. 1996;72:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Hampton LM, Farrell M, Ramirez-Gonzalez A, Menning L, Shendale S, Lewis I, Rubin J, Garon J, Harris J, Hyde T, Wassilak S, Patel M, Nandy R, Chang-Blanc D; Immunization Systems Management Group of the Global Polio Eradication Initiative. Cessation of Trivalent Oral Poliovirus Vaccine and Introduction of Inactivated Poliovirus Vaccine - Worldwide, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:934-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 151] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 3. | Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, Ruddy K, Tsang J, Cardoso F. Breast cancer. Nat Rev Dis Primers. 2019;5:66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 999] [Cited by in RCA: 1797] [Article Influence: 299.5] [Reference Citation Analysis (0)] |
| 4. | Wenkel E, Geppert C, Schulz-Wendtland R, Uder M, Kiefer B, Bautz W, Janka R. Diffusion weighted imaging in breast MRI: comparison of two different pulse sequences. Acad Radiol. 2007;14:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Bandyopadhyay AS, Garon J, Seib K, Orenstein WA. Polio vaccination: past, present and future. Future Microbiol. 2015;10:791-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 196] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 6. | Kay L, Nielsen NM, Wanscher B, Jennum P. Neurological Symptoms in Danes with a History of Poliomyelitis: Lifelong Follow-Up of Late Symptoms, their Association with Initial Symptoms of Polio, and Presence of Postpolio Syndrome. Eur Neurol. 2018;80:295-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Agre JC, Rodríquez AA, Tafel JA. Late effects of polio: critical review of the literature on neuromuscular function. Arch Phys Med Rehabil. 1991;72:923-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Dénes Z, Varga M. [Poliomyelitis and the post-polio syndrome]. Orv Hetil. 2001;142:1493-1496. [PubMed] |
| 9. | Lo JK, Robinson LR. Post-polio syndrome and the late effects of poliomyelitis: Part 2. treatment, management, and prognosis. Muscle Nerve. 2018;58:760-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Farbu E, Gilhus NE, Barnes MP, Borg K, de Visser M, Driessen A, Howard R, Nollet F, Opara J, Stalberg E. EFNS guideline on diagnosis and management of post-polio syndrome. Report of an EFNS task force. Eur J Neurol. 2006;13:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Farbu E. Update on current and emerging treatment options for post-polio syndrome. Ther Clin Risk Manag. 2010;6:307-313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Nielsen NM, Wohlfahrt J, Aaby P, Hjalgrim H, Pedersen CB, Askgaard DS, Melbye M. Cancer risk in a cohort of polio patients. Int J Cancer. 2001;92:605-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lehrer S, Rheinstein PH. Inverse Relationship Between Polio Incidence in the US and Colorectal Cancer. In Vivo. 2018;32:1485-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Razek AA, Lattif MA, Denewer A, Farouk O, Nada N. Assessment of axillary lymph nodes in patients with breast cancer with diffusion-weighted MR imaging in combination with routine and dynamic contrast MR imaging. Breast Cancer. 2016;23:525-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Abdel Razek AAK, Zaky M, Bayoumi D, Taman S, Abdelwahab K, Alghandour R. Diffusion tensor imaging parameters in differentiation recurrent breast cancer from post-operative changes in patients with breast-conserving surgery. Eur J Radiol. 2019;111:76-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |