Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6172
Peer-review started: July 23, 2020
First decision: August 7, 2020
Revised: August 19, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: December 6, 2020
Processing time: 134 Days and 1.4 Hours
Ectopic thyroid is a rare developmental disorder, typically found in lingual areas, and most distantly in the abdomen. Thyroid ectopia in multiple regions is extremely rare. To date, there are no reports of ectopic goiter in four regions of the abdominal cavity in a single patient.
We present a case of thyroid ectopia in four areas of the abdomen, comprising normal orthotopic thyroid tissue. A 36-year-old woman, who underwent ovarian teratoma resection 10 years previously due to symptomatic ovarian teratoma, was referred to our hospital for treatment of an incidental hepatic mass. Magnetic resonance imaging and computed tomography (CT) of the abdomen showed a heterogeneously enhanced lobulated lesion in the sixth and seventh hepatic segment adjacent to the diaphragm. The mass was surgically excised, and histologic examination determined an ectopic nodular goiter. At the one-year follow-up, the abdominal CT scan, whole-body radionuclide I131 examination, and abdominal wall biopsy showed similar lesions in the left renal fascia and anterior abdominal wall.
Multiple para-ectopic thyroid is often misdiagnosed, owing to its extremely rare incidence and non-specific clinical manifestations and imaging features. A combination of multiple examinations is necessary for diagnostic accuracy.
Core Tip: Ectopic thyroid glands in the abdomen are extremely rare, and the occurrence of ectopic thyroid tissues in multiple regions simultaneously is even rarer. However, it is best to diagnose ectopic thyroid, its function and location, before surgery. Additionally, abdominal metastasis due to thyroid cancer and ectopic thyroid cancer must be differentiated from benign lesions.
- Citation: Qin LH, He FY, Liao JY. Multiple ectopic goiter in the retroperitoneum, abdominal wall, liver, and diaphragm: A case report and review of literature. World J Clin Cases 2020; 8(23): 6172-6180
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6172.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6172
Ectopic thyroid is a rare developmental disease with an incidence of only one in 300000[1]. The rate of incidence is higher in females (75%-80%)[2]. Thyroid ectopic tissue is most often located in the neck and head, accounting for 90% of all ectopic
A 36-year-old woman, who had undergone ovarian teratoma resection 10 years previously due to symptomatic ovarian teratoma, was referred to our hospital for treatment of an incidental hepatic mass.
She presented with occasional dull pain below the xiphoid.
She had undergone ovarian teratoma resection 10 years previously.
No special personal and family history.
Physical examination showed no abnormalities.
The liver function test and all tumor markers were negative.
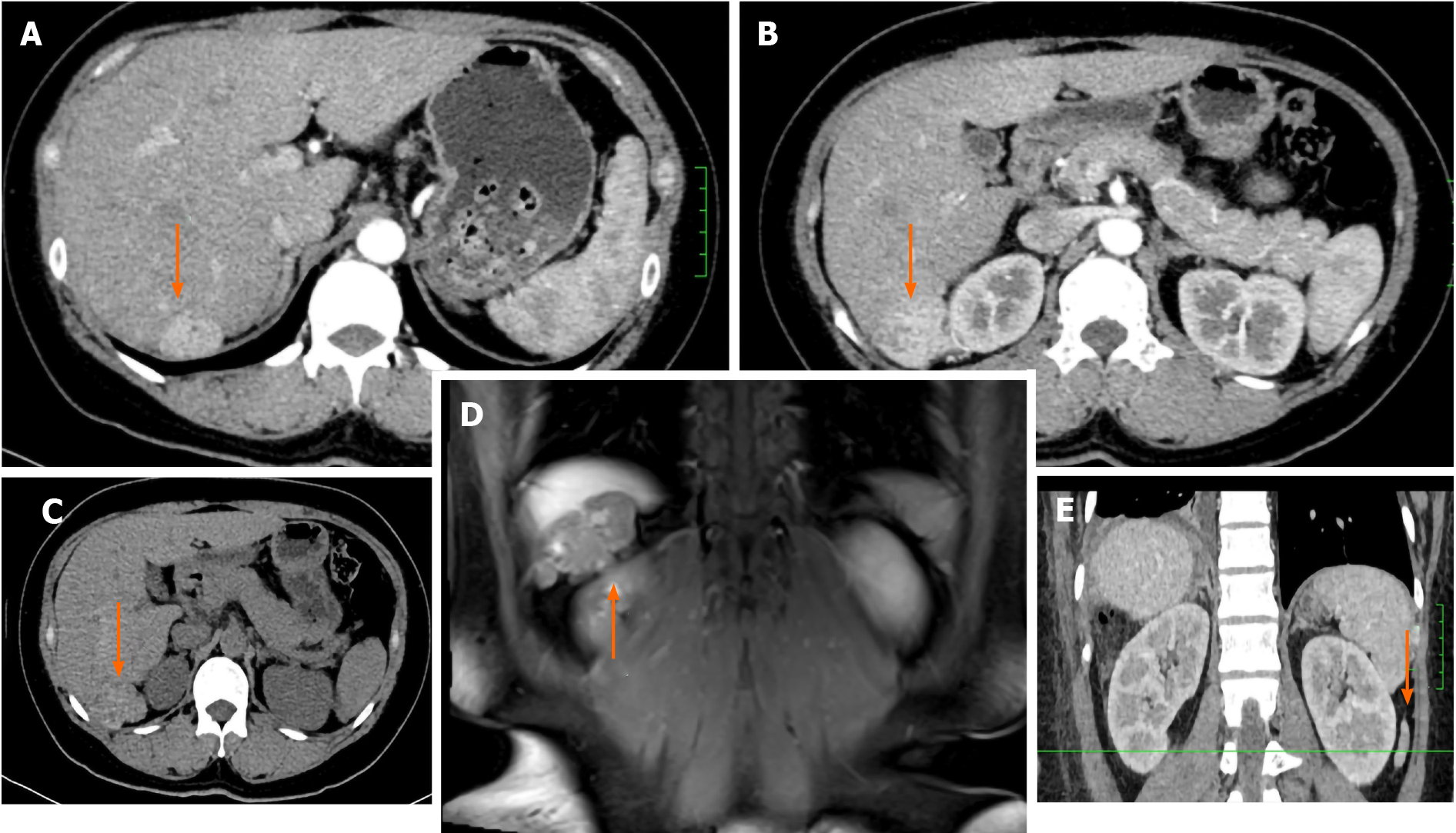
Abdominal computed tomography (CT) showed a 1.2 cm × 2.9 cm × 2.8 cm (transverse × anteroposterior × craniocaudal) lobulated lesion in the diaphragm (Figure 1A), and a 4.2 cm × 3.9 cm × 3.9 cm solid lesion in the sixth hepatic segment (Figure 1B), with a 60-70 Hounsfield unit (HU) value (Figure 1C).
On post-contrast CT, the lesion revealed a heterogeneous enhancement pattern (Figure 1A and B). The lesions showed equal signal intensity on T2-weighted imaging and slightly low signals on T1-weighted imaging (Figure 1D). The magnetic resonance imaging (MRI) enhancement pattern was similar to the CT pattern, and diffusion-weighted imaging showed a slightly higher signal (b value = 800). The lesions showed no restricted diffusion, and no contrast agent uptake on the hepatobiliary specific phase, displaying low signal.
Based on these examinations, we clinically diagnosed a benign adenoma with hemorrhage.
Surgery was performed, which revealed a 6.5 cm × 5.5 cm × 4.5 cm mass in the right posterior lobe of the liver, and a 2.5 cm × 2.0 cm × 1.5 cm mass in the right diaphragm adjacent to the sixth hepatic segment, both with an incomplete capsule. The gross specimens were grayish white and gelatinous.
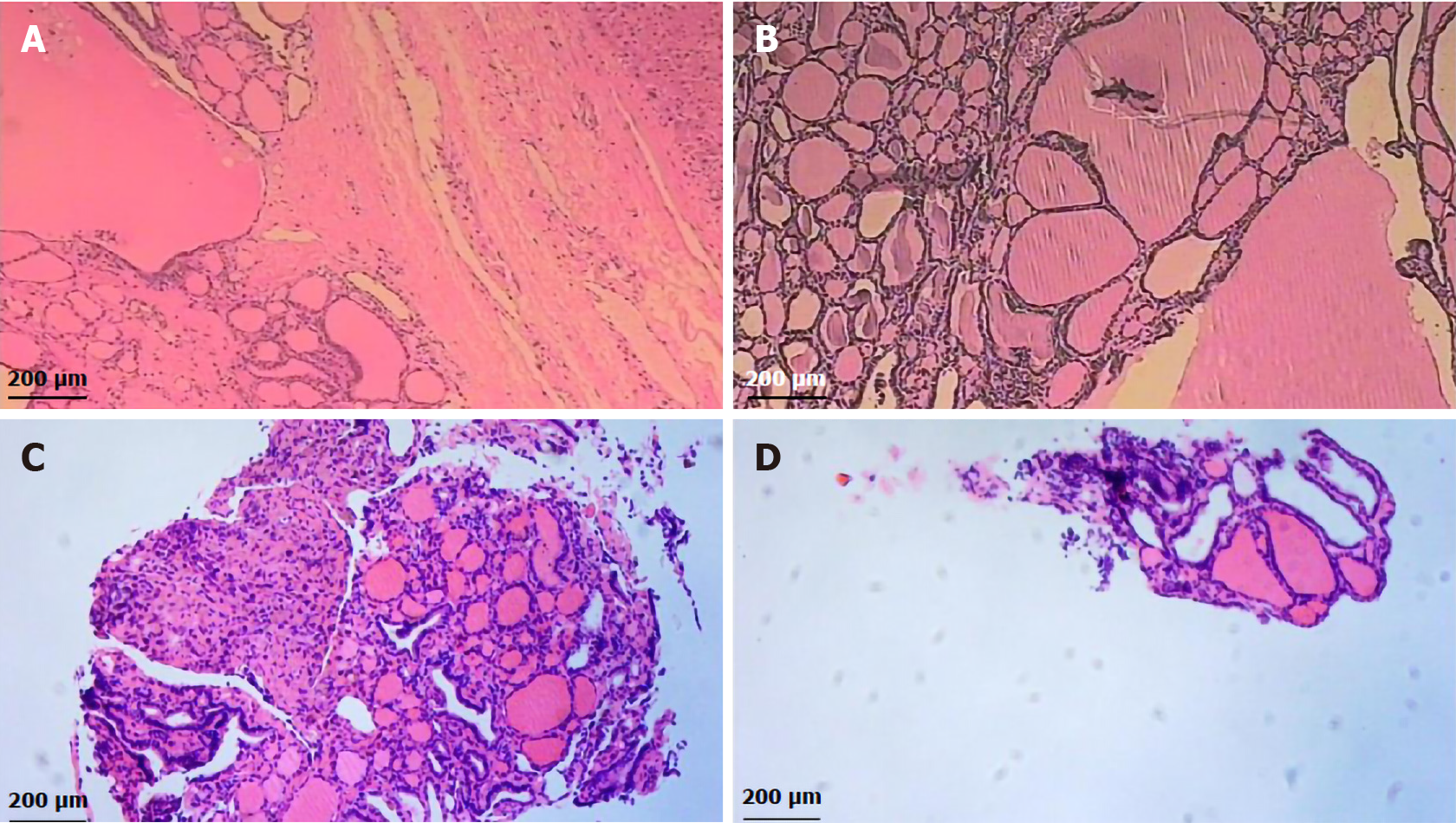
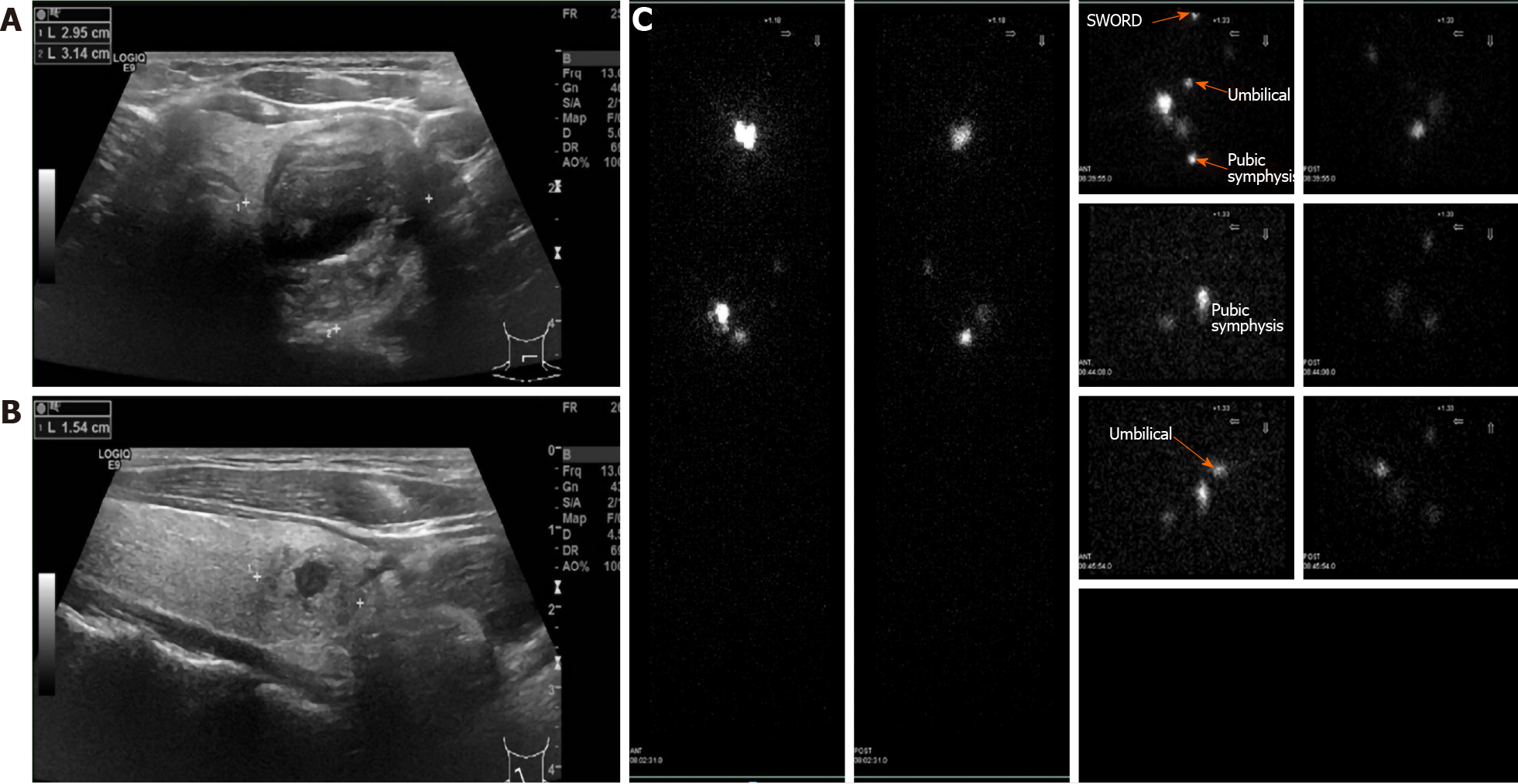
Histological examination revealed ectopic goiters in the right diaphragm and in the right lobe of the liver (Figure 2A and B). Immunohistochemistry staining revealed the strong presence of thyroid transcription factor-1 (TTF-1), thyroglobulin, thyroperoxidase (TPO), CK19, and CK7; while galectin-3 and CD56 were negative. The postoperative thyroid function test was normal. Thyroid and cervical lymph nodular ultrasonography indicated nodular goiter (Figure 3A), confirmed by simultaneous ultrasound-guided puncture, with no malignant cells, and without thyroid cancer metastasis.
At the one-year follow-up, abdominal CT showed a 2.4 cm × 0.9 cm ovoid slightly hyperintense lesion (84 HU) adjacent to the left renal fascia (Figure 1E). To confirm further thyroid ectopia in the left retroperitoneum, we recommended that the patient undergo 99mTc sodium pertechnetate scintigraphy. To our surprise, this showed a patchy abnormal concentration equivalent to the area of the left kidney, as well as two patchy abnormal concentrations in the right lower abdominal wall (Figure 3B). Considering the possibility of ectopic thyroid in the right lower abdominal wall of the left kidney, an ultrasound-guided puncture provided proof (Figure 2C and D).
The mechanism of abdominal ectopic thyroid formation remains controversial, but several theories have been proposed. The most common theory to explain the presence of ectopic thyroid tissue is excessive descent of thyroid precursor cells outside the usual path of thyroid anlage[6], or abnormal migration of precursor cells[7]. However, it is difficult to prove this due to the rarity of abdominal ectopic thyroid, and the distance of the path of embryonic development.
Secondly, there is a theory that the precursor cells of the foregut endoderm differentiate into thyroid ectopia[8,9] because most abdominal organs, as well as the thyroid, originate in the endoderm. However, it is difficult to explicate why the adrenal gland is located in the retroperitoneum, since it originates from mesoderm, while the cortex and medulla derive from the epiblast[10].
A third theory is that germ cell neoplasms can differentiate into mature teratoma-type thyroid tissue[11]. Tamaki et al[12] confirmed that, after the first division of meiosis, a single germ cell could generate into ectopic thyroid tissue and other tissue components (e.g., skin appendages and bone). However, peritoneal strumosis that originated from ovarian teratoma may develop into malignant papillary thyroid cancer[5,13,14]. In addition, there can be complications due to thyroid tissue implantation during surgery[15,16]. This theory may clarify why goiters in the present case were located in the anterior abdominal wall.
Ectopic thyroid gland tissue may be classified as vagus thyroid or parathyroid; the former has no normal orthotopic thyroid gland tissue, while the latter coexists with normal orthotopic thyroid gland tissue. We reviewed the current literature in the electronic databases Medline and Embase, and found 15 cases of multiple-site ectopic thyroid (Table 1)[3,4,17-24]. Most cases with three sites were located in the neck, while those in four or more regions were apt to locate in post-operative regions or previous ovarian teratoma.
| Ref. | Age, yr | Gender | Location1 | Endocrine | Ectopic location | Diagnosis |
| Agrawal et al[3], 2019 | 11 | Female | Not normal | Normal | Infrahyoid region, the base of the tongue and the other in the prehyoid location | TFT, US, Tc-99m TcO4 scan, SPECT/CT, FNA |
| Barai et al, 2004 | 6 | Male | Not normal | Hyperthyroidism | Region of the foramen cecum, suprahyoid and in the region of the cricoid cartilage | TFT, 131I WBS, pathology |
| Belgur et al[22], 2016 | 25 | Male | Not normal | NA | Tongue (posteriorly), the sublingual, the prehyoid and the right submandibular regions | US, CT, MRI, FNA |
| Dobrescu et al[14], 2014 | 48 | Female | Normal | Hyperthyroidism | Pulmonary areas, right pelvis, axial skeleton, pelvic bones, skull | US, CT, 131I WBS, TFT, pathology |
| Hua et al[24], 2019 | 56 | Female | NA | SH | Tongue base, neck region over the submental and hyoid bone level | 131I WBS, FNA, CT |
| Jain et al[23], 2010 | 20 | Female | Normal | SH | Base of the tongue, the suprahyoid and the subhyoid | TFT, 131I WBS, CT |
| Kim et al[16], 2015 | 35 | Female | Normal | Hyperthyroidism | Right chest wall and axilla, the left chest wall | 131I WBS, SPECT/CT |
| Konde et al[17], 2012 | 16 | Female | Not normal | Normal | Lingual foramen cecum level, sublingual (between the geniohyoid and mylohyoid muscles), below the hyoid bone level | CT, US, TFT, Tc-99m TcO4 scan |
| Kuramoto et al[19], 2013 | 10 | Female | NA | NA | Near the base of the tongue, prehyoid and pretracheal region | NA |
| Nilegaonkar et al[21], 2011 | 16 | Female | NA | Hypothyroidism | Base of tongue, the level of the hyoid and suprahyoid location | US, CT, Tc-99m TcO4 scan, FNAC, TFT |
| Passah et al[4], 2018 | 5 | Female | Not normal | SH | Base of the tongue, prehyoid region, anterior to the thyroid cartilage towards the right side | TFT, Tc-99m TcO4 scan, SPECT/CT |
| Rahalkar et al[20], 2014 | 42 | Female | Not normal | Normal | Surface of posterior tongue, anterosuperior, close to the body of the hyoid bone and in the subhyoid region | CT, Tc-99m TcO4 scan |
| Spencer-Segal et al, 2015 | 37 | Female | Normal | Normal | Right sternocleidomastoid, periclavicular, pectoralis and axillary regions | TFT, I-123 SPECT-CT, CT, pathology |
| Thomas et al[5], 2013 | 14 | Female | Normal | Normal | Omentum, left adnexa, peritoneum, spleen, abdominal wall, bladder and rectum | TFT, CT, pathology |
| Weng et al, 2000 | 86 | Female | Normal | Hyperthyroidism | Lung, visceral pleura, pelvic cavity and the skeleton | TFT, chest X-ray, US, pathology |
According to the review literature, ectopic thyroid is mostly asymptomatic[2]. However, non-specific symptoms may also occur depending on the anatomical location, such as pain, difficulty breathing, diarrhea, bleeding, and other complications. In the present case, the patient experienced an occasional dull pain below the xiphoid, because the ectopic thyroid was located at the sixth and seventh hepatic segment adjacent to the diaphragm. Liang et al[25] reported a 60-year-old woman with recurrent pain in her right upper abdomen due to a gallbladder mass, which proved after surgical resection to be ectopic thyroid tissue. In another case, a 60-year-old woman underwent routine appendectomy due to sudden right lower abdominal pain; the histological examination revealed abnormal ectopic thyroid tissue in the fat around the appendix[11]. In the present case, thyroid tissue was found in the orthotopic position of the ectopic thyroid, and the thyroid function test was normal.
In our patient, the various imaging examinations were inconclusive and could not provide a confident diagnosis; only postoperative pathologic examination confirmed ectopic thyroid. Due to the rarity of ectopic thyroid tissue in the abdominal cavity and the limited experience with diagnostic imaging in these cases, the location and function of ectopic thyroid are usually determined postoperatively or after biopsy[8].
However, it is best to diagnose ectopic thyroid, its function and location, before surgery. Abdominal metastasis due to thyroid cancer and ectopic thyroid cancer must be differentiated from benign lesions. Distant metastases of papillary carcinoma of the thyroid have been found in the pancreas[26], liver[27], kidney[28], adrenal gland[29], ovaries[30], and other sites. Ectopic thyroid may also be cancerous. The canceration rate of lingual thyroid is about 1%[31].
For differential diagnosis, there are a variety of examination methods: thyroid function test, and non-invasive imaging such as ultrasound, CT, MRI, whole-body thyroid radionuclide scan, and single-photon emission computed tomography (SPECT)/CT. Invasive examinations include puncture biopsy guided by ultrasound or CT, but these are not preferred.
Imaging methods can detect the extent and location of ectopic thyroid, and ultrasound is the cheapest and most easily available[2]. Ultrasound can distinguish benign lesions from malignant thyroid nodules[32]. However, ultrasound cannot distinguish ectopic thyroid gland from orthotopic thyroid gland, which is easy to misdiagnose.
When abdominal CT imaging depicts abdominal masses with higher density than that of surrounding soft tissue, with a clear boundary, then ectopic thyroid tissue should be considered[33]. On CT imaging, ectopic thyroid tissue, like normal thyroid tissue, contains a certain amount of iodine, and its attenuation relative to the adjacent skeletal muscle increases (70 HU ± 10 HU). After contrast agent is injected, most tissues show heterogeneous enhancement[8,22,34]. Moreover, ectopic goiter is generally found with calcification[35]. In the present case, non-contrast CT imaging displayed hepatic lesion hyperintensity (60-70 HU) that was higher than that of the surrounding normal liver tissue; contrast CT imaging showed heterogeneous enhancement.
On MRI, the ectopic thyroid has equal intensity or slight hyperintensity in T1-weighted and T2-weighted images (T1WI and T2WI), and the enhancement pattern is the same as CT imaging[22,36]. To evaluate the function and anatomy of the suspected ectopic thyroid tissue, especially thyroid tissue that is distant from the thyroid tongue tube, radionuclide and SPECT/CT imaging can show the uptake of radionuclide (99 TcmO4 or 131I) by the ectopic thyroid and positivity[3,37,38]. Therefore, for suspected multiple abdominal ectopic thyroid, multiple imaging methods are required.
Radiologically, ectopic thyroid in our case, associated with multiple sites and lesions in the abdomen, was difficult to differentiate from hematological diseases such as lymphomas or leukemia. Additionally, multiple enlarged lymph nodes in the abdomen were typical manifestations of lymphomas or leukemia, which were limited to multiple round or oval soft tissue in certain areas at the preliminary stage. With regard to disease progression, it manifested in the retroperitoneal space, mesentery, superficial lymph node enlargement, and even involved the liver and spleen[39], as well as pelvic organs, such as the uterus[40]. Lymphomas or leukemia are usually seen as homogeneous low-density lesions on CT imaging, with mild to moderate enhancement. However, ectopic thyroid showed high density on CT imaging. In addition, the density of lymph nodes with necrosis may be heterogeneous. In lymphomas, MRI features show low signal intensity of relative fat and slightly high signal intensity of muscle on T1WI. On T2WI, the signal intensity of relative fat is equal or slightly lower, and that of muscle is high signal intensity. DWI showed characteristic homogeneous high signal intensity[41]. However, ectopic thyroid had equal intensity or slight hyperintensity in T1WI and T2WI.
In conclusion, multiple para-ectopic thyroid is often misdiagnosed, owing to its extremely rare incidence and non-specific clinical manifestations and imaging features. A combination of multiple examinations is necessary for diagnostic accuracy. When thyroid tissue is found in an abnormal location, ectopic thyroid should be considered, especially if there is a previous history of ovarian teratoma. First, an ultrasound examination should determine whether there is normal thyroid tissue. This is followed in turn with a thyroid function test, CT or MRI (especially 99mTc sodium pertechnetate scintigraphy), and SPECT/CT. Finally, a biopsy and even pathological examination after surgical resection can provide confirmation. For the patient with a previous thyroidectomy, a follow-up that includes 99mTc sodium pertechnetate scintigraphy, or SPECT/CT examination, is essential to check for implantation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mazzei MA S-Editor: Gao CC L-Editor: Webster JR P-Editor: Ma YJ
| 1. | Ibrahim NA, Fadeyibi IO. Ectopic thyroid: etiology, pathology and management. Hormones (Athens). 2011;10:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Santangelo G, Pellino G, De Falco N, Colella G, D'Amato S, Maglione MG, De Luca R, Canonico S, De Falco M. Prevalence, diagnosis and management of ectopic thyroid glands. Int J Surg. 2016;28 Suppl 1:S1-S6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Agrawal K, Patro PSS, Pradhan P. Triple Ectopic Thyroid Detected on SPECT/CT: A Rare Case Report. Clin Nucl Med. 2019;44:e453-e455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Passah A, Arora S, Damle NA, Sharma R. Triple Ectopic Thyroid on Pertechnetate Scintigraphy. Indian J Endocrinol Metab. 2018;22:712-713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Thomas J, Bargman R, Rosenthal DS, Nikiforov YE, Gebre W, Liu P, Martinez-Schlurmann N, Hupart KH. Malignant struma ovarii: Controversies, challenges and the promise of molecular diagnosis. Endocr Rev. 2013;34. |
| 6. | Cassol CA, Noria D, Asa SL. Ectopic thyroid tissue within the gall bladder: case report and brief review of the literature. Endocr Pathol. 2010;21:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Guerra G, Cinelli M, Mesolella M, Tafuri D, Rocca A, Amato B, Rengo S, Testa D. Morphological, diagnostic and surgical features of ectopic thyroid gland: a review of literature. Int J Surg. 2014;12 Suppl 1:S3-S11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Ma A, Liu H. Ectopic thyroid of the pancreas: A case report and literature review. Medicine (Baltimore). 2017;96:e8707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Campora M, Trambaiolo Antonelli C, Mastracci L, Pigozzi S, Grillo F. A Never Ending Journey: Ectopic Thyroid. Int J Surg Pathol. 2017;25:241-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Rawitzer J, Kapakoglou A, Walz MK, Schmid KW, Reis H. [Ectopic thyroid tissue in the adrenal gland : A case report and review of the literature]. Pathologe. 2020;41:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Campora M, Trambaiolo Antonelli C, Valle L, Fiocca R, Mastracci L, Grillo F. Abdominal Ectopic Thyroid Tissue: The Man From Istanbul. Int J Surg Pathol. 2019;27:553-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Tamaki S, Miyakura Y, Someya S, Ishikawa H, Kakizawa N, Hasegawa F, Tanaka H, Kikugawa R, Tsujinaka S, Tanaka A, Lefor AK, Rikiyama T. Laparoscopic resection of retroperitoneal ectopic thyroid tissue. Asian J Endosc Surg. 2017;10:331-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Uzum AK, Iyibozkurt C, Canbaz B, Ciftci SD, Aksakal N, Kapran Y, Aral F, Ozbey NC. Management and follow-up results of an incidental thyroid carcinoma in a young woman with ovarian teratoma. Gynecol Endocrinol. 2013;29:724-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Dobrescu R, Coles D, Goldstein A, Ioachim D, Magurean M, Ceausu I, Badiu C. Diagnostic and evolutive peculiarities in a case series of malignant struma ovarii. Eur Thyroid J. 2014;3:139. |
| 15. | Espiard S, Petyt G, Lion G, Béron A, Do Cao C, Wémeau JL, Vantyghem MC, Pattou F, Caiazzo R. Ectopic Subcutaneous Implantation of Thyroid Tissue After Gasless Transaxillary Robotic Thyroidectomy for Papillary Thyroid Cancer. Thyroid. 2015;25:1381-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Kim MR, Jo S, Shim HK. Port-Site Implantation Diagnosed by Iodine-131 Post-Ablation Single-Photon Emission Tomography-Computed Tomography After Robotic Thyroidectomy: A Case Report. Am J Case Rep. 2019;20:1695-1698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Konde SR, Singh H Retd, Pawar A, Sasane A. Triple ectopic thyroid. Med J Armed Forces India. 2012;68:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Maru P, Rao R. Case report of multiple ectopic thyroid. Global J Res Anal. 2017;. |
| 19. | Kuramoto R, Oikawa K, Fujita K, Oridate N, Fukuda S. Triple Ectopic Thyroid: A Case Report and Review of Literature. J Thyroid Disord Ther. 2013;2:216. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Rahalkar M, Rahalkar A, Solav S. A rare case of triple thyroid ectopia. Indian J Endocrinol Metab. 2014;18:238-240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Nilegaonkar S, Naik C, Sonar S, Hirawe D. Triple ectopic thyroid: A rare entity. Indian J Nucl Med. 2011;26:194-195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Belgur SC, Shah YM, Moorthy BR, Pavithra S. Multiple ectopia of the thyroid gland: A rare case report. West Afr J Radiol. 2016;23:142-145. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Jain A, Pathak S. Rare developmental abnormalities of thyroid gland, especially multiple ectopia: A review and our experience. Indian J Nucl Med. 2010;25:143-146. [PubMed] |
| 24. | Hua MW, Lin WC, Wang CC. Triple Ectopic Thyroid Excision by Robotic Surgery via Trans-Oral and Post-Auricular Approach Report of a Case. Ann Clin Case Rep. 2019;4. |
| 25. | Liang K, Liu JF, Wang YH, Tang GC, Teng LH, Li F. Ectopic thyroid presenting as a gallbladder mass. Ann R Coll Surg Engl. 2010;92:W4-W6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Murakami Y, Shimura T, Okada R, Kofunato Y, Ishigame T, Yashima R, Nakano K, Suzuki S, Takenoshita S. Pancreatic metastasis of papillary thyroid carcinoma preoperatively diagnosed by endoscopic ultrasound-guided fine-needle aspiration biopsy: a case report with review of literatures. Clin J Gastroenterol. 2018;11:521-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Zhou J, Luo Y, Ma BY, Ling WW, Zhu XL. Contrast-enhanced ultrasound diagnosis of hepatic metastasis of concurrent medullary-papillary thyroid carcinoma: A case report. Medicine (Baltimore). 2017;96:e9065. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Liou MJ, Lin JD, Chung MH, Liau CT, Hsueh C. Renal metastasis from papillary thyroid microcarcinoma. Acta Otolaryngol. 2005;125:438-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Farina E, Monari F, Tallini G, Repaci A, Mazzarotto R, Giunchi F, Panzacchi R, Cammelli S, Padula GD, Deodato F, Pasquali R, Fanti S, Fiorentino M, Morganti AG. Unusual Thyroid Carcinoma Metastases: a Case Series and Literature Review. Endocr Pathol. 2016;27:55-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 30. | Logani S, Baloch ZW, Snyder PJ, Weinstein R, LiVolsi VA. Cystic ovarian metastasis from papillary thyroid carcinoma: a case report. Thyroid. 2001;11:1073-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Huang NS, Wei WJ, Qu N, Wang YL, Wang Y, Ji QH. Lingual ectopic papillary thyroid carcinoma: Two case reports and review of the literature. Oral Oncol. 2019;88:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Ohnishi H, Sato H, Noda H, Inomata H, Sasaki N. Color Doppler ultrasonography: diagnosis of ectopic thyroid gland in patients with congenital hypothyroidism caused by thyroid dysgenesis. J Clin Endocrinol Metab. 2003;88:5145-5149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Zander DA, Smoker WR. Imaging of ectopic thyroid tissue and thyroglossal duct cysts. Radiographics. 2014;34:37-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 34. | Altay C, Erdoğan N, Karasu S, Uluç E, Sarsılmaz A, Mete B, Oyar O. CT and MRI findings of developmental abnormalities and ectopia varieties of the thyroid gland. Diagn Interv Radiol. 2012;18:335-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Sato D, Hayashi S, Sakata S, Kawachi R, Shimamura M, Sakurai H. Intrapericardial Ectopic Goiter: A Very Unusual Presentation. Ann Thorac Cardiovasc Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Chen M, Hu J, Cai X. Ectopic Thyroid Gland Tissue in the Liver. Clin Gastroenterol Hepatol. 2019;Online ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Ahuja K, Bhandari T, Banait-Deshmane S, Crowe DR, Sonavane SK. Incidentally detected ectopic thyroid in juxta cardiac location-Imaging and pathology. Radiol Case Rep. 2018;13:909-913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Hummel J, Wachsmann J, Carrick K, Oz OK, Mathews D, Peng F. Ectopic Thyroid Tissue in the Mediastinum Characterized by Histology and Functional Imaging with I-123 SPECT/CT. Case Rep Radiol. 2017;2017:9084207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Cencini E, Fabbri A, Guerrini S, Mazzei MA, Rossi V, Bocchia M. Long-term remission in a case of plasmablastic lymphoma treated with COMP (cyclophosphamide, liposomal doxorubicin, vincristine, prednisone) and bortezomib. Eur J Haematol. 2016;96:650-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Mazzei MA, Bettini G, Pozzessere C, Guerrini S, Defina M, Ambrosio MR, Aprile L, Bocchia M, Volterrani L. A solitary uterine relapse in T-cell Acute Lymphoblastic Leukaemia: CT features and pathologic correlation. J Biol Regul Homeost Agents. 2016;30:871-875. [PubMed] |
| 41. | McCarten KM, Nadel HR, Shulkin BL, Cho SY. Imaging for diagnosis, staging and response assessment of Hodgkin lymphoma and non-Hodgkin lymphoma. Pediatr Radiol. 2019;49:1545-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |