Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6144
Peer-review started: June 28, 2020
First decision: September 23, 2020
Revised: October 3, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: December 6, 2020
Processing time: 159 Days and 3.3 Hours
Nodular fasciitis (NF) is a benign disease originating from fascial tissue and most commonly occurs in the extremities, followed by the trunk, head, and neck. NF of the head and neck occurs mainly in the face and neck, and it has not been reported in the occipital region.
A 30-year-old man was admitted because of a mass in the left occipital region. Imaging examination revealed a soft tissue nodule in the left occipital area. An enhanced magnetic resonance imaging scan showed characteristic inverted target and fascial tail signs. Histopathological analysis showed a large amount of spindle cell proliferation, and immunohistochemistry showed positive expression of SMA in the spindle cells in the lesion. Finally, nodular fasciitis was diagnosed.
NF of the head and neck is rare, but the possibility of NF should be considered when nodules or masses with rapid subcutaneous growth are found and tenderness in the head and neck is present. Imaging examination, in combination with clinical manifestations and histopathological examination, can improve the diagnostic accuracy for the disease. After diagnosis, local surgical resection is the first choice of treatment.
Core Tip: Nodular fasciitis is a benign disease originating from fascial tissue and often occurs in the extremities. We report a case of nodular fasciitis in the occipital region. Combined with clinical and pathological findings, we analyzed its imaging findings to improve the understanding of this disease.
- Citation: Wang T, Tang GC, Yang H, Fan JK. Occipital nodular fasciitis easily misdiagnosed as neoplastic lesions: A rare case report. World J Clin Cases 2020; 8(23): 6144-6149
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6144.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6144
Nodular fasciitis (NF), also known as infiltrative fasciitis, pseudogranulomatous fasciitis, or pseudosarcomatous fibromatosis, is a benign lesion originating from fascial tissue that is formed by fibrous tissue tumor-like hyperplasia[1], which most commonly occurs in the limbs, followed by trunk, head, and neck[2]. Head and neck NF usually occur in the subcutaneous tissue of the face and neck, and its clinical manifestations are usually single, fast-growing subcutaneous nodules. The course of disease is usually less than 3 mo. The nodule is generally less than 4 cm in diameter, with a medium texture and no pain or slight tenderness. Because of its lack of characteristic clinical manifestations and few related imaging reports, NF is easy to be misdiagnosed before surgery. The aim of our report is to present a case of nodular fasciitis in the occipita and analyze its clinical, pathological, and imaging features to improve the understanding of the disease.
A 30-year-old man was admitted to our hospital with a mass in his occipital region for 1 mo.
One month prior to admission, the patient had found a mass, the size of which was approximately 1 cm × 1 cm, in the left occipital region and he did not consider it to be serious. One month later, the patient found that the mass was enlarged, so he presented to the hospital.
The patient was in good health prior to the present illness.
The patient had no previous or family history of similar illnesses.
Physical examination showed a mass in the left occipital area of the patient, approximately 2 cm × 2 cm in size, that was rigid and had no associated tenderness.
The laboratory examinations (including routine blood and urine tests, coagulation function tests, liver and kidney function tests, and tumor markers) were normal.
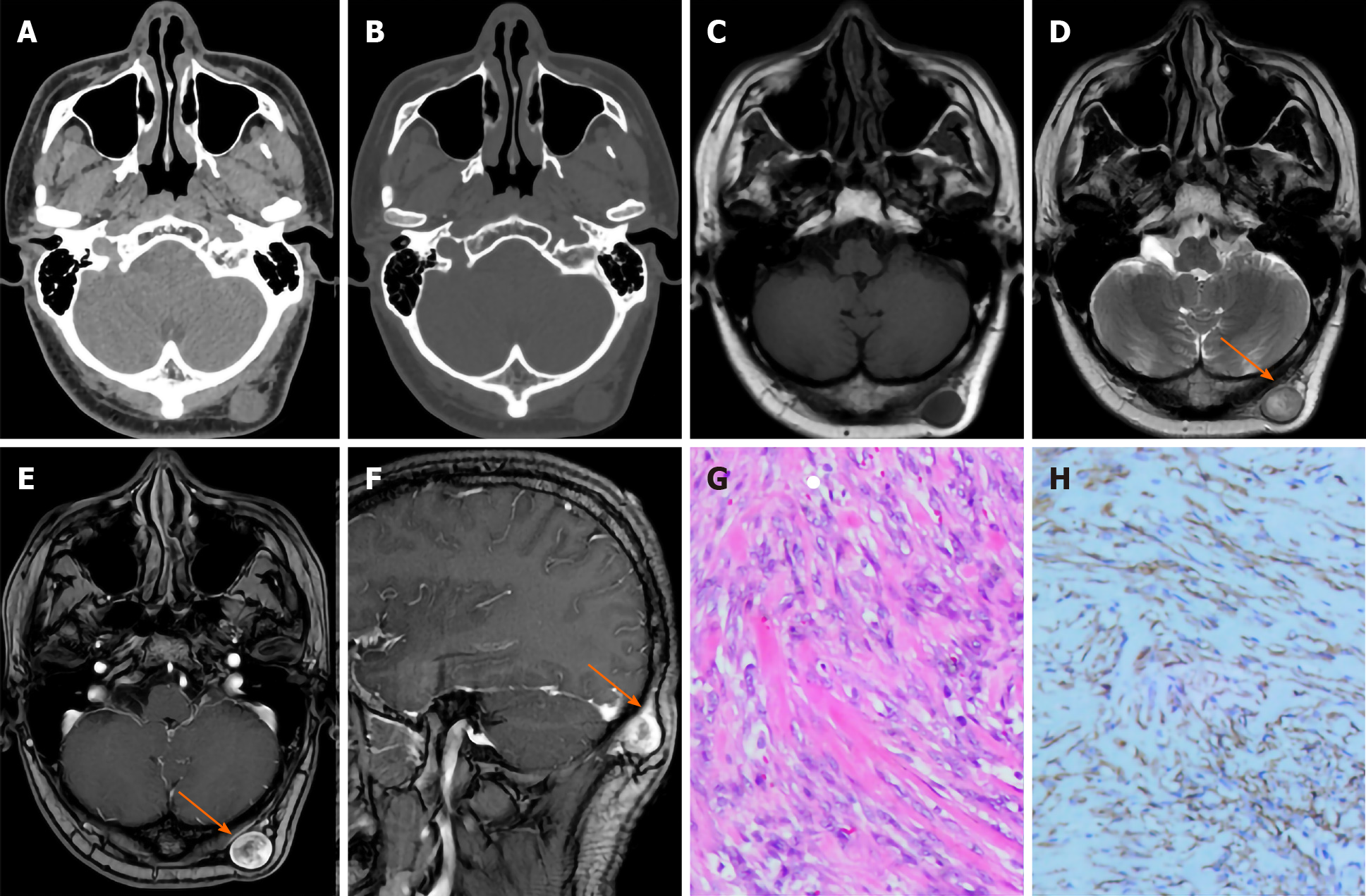
Computed tomography (CT) examination showed a left occipital nodule with a subcutaneous diameter of approximately 2 cm, a uniform density, and a CT value of approximately 25 Hu. The nodule boundary was clear, the edge was smooth (Figure 1A), and there was no destruction of the adjacent skull bone (Figure 1B). Magnetic resonance imaging (MRI) showed an oval subcutaneous nodule in the left occipita, and the lesion showed iso-signal intensity on T1-weighted imaging (T1WI). The nodule grew close to the superficial fascia of the left occipita to the subcutaneous fat layer, and the edge was clear and smooth (Figure 1C). T2-weighted imaging (T2WI) showed inhomogeneous high signal intensity in the lesion, and the central signal was higher than that of the periphery (Figure 1D). A contrast-enhanced scan of the lesion showed obvious inhomogeneous enhancement, and the peripheral enhancement was higher than that of the center, showing an inverted target sign (Figure 1E). The sagittal contrast-enhanced scan of the lesion showed obvious thickening and enhancement of the adjacent fascia, showing a fascial tail sign (Figure 1F).
Postoperative pathology showed that a large number of proliferated spindle cells were arranged erratically, and myxoid matrix, local angiogenesis, and a small amount of erythrocyte extravasation could be seen (Figure 1G). Immunohistochemistry showed positive expression of SMA in spindle cells in the lesion (Figure 1H).
Left occipital NF.
After the relevant examinations, the patient underwent left occipital mass resection. During the operation, the size of the mass was approximately 2 cm × 2 cm, and the base was approximately 1.5 cm × 1.5 cm. The boundary between the mass and the surrounding tissue was clear, and the base was closely connected with the occipital periosteum.
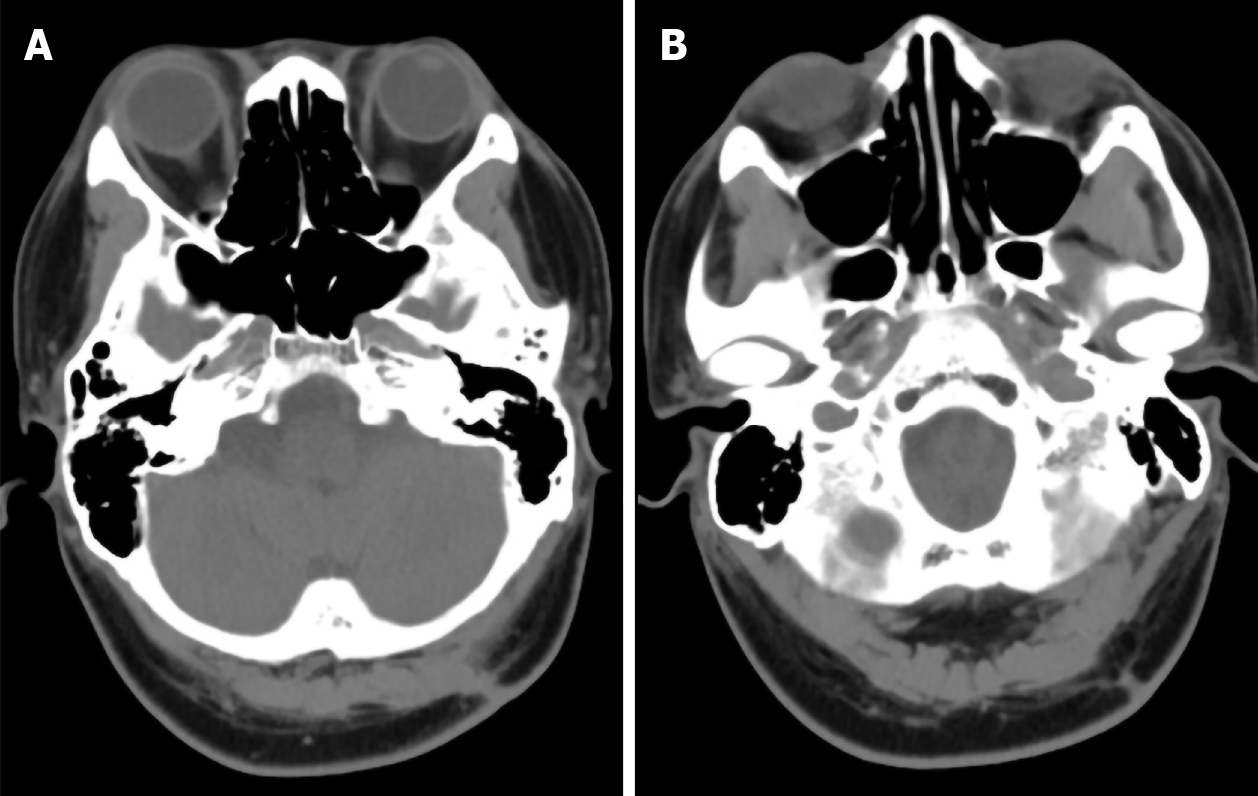
The patients recovered well after the operation, and CT scan showed no recurrence during follow-up for 2 years (Figure 2A and B).
NF is a kind of benign fibroblast proliferative lesion originating from fascial tissue that was first reported by Kornwaler et al[2] in 1955 and now belongs to the soft tissue benign lesion grouping in the 2017 edition of the WHO classification of head and neck tumors[3]. Some scholars[4] believe that NF is a transitional tumor between proliferation and tumor, when tumor cell proliferation is active and can also infiltrate and destroy adjacent tissue structures. NF of the head and neck is relatively rare in the clinic, but because it is more difficult to operate directly on the head and neck than on the limbs and torso, imaging examination before operation is more common. Most of the causes of NF are thought to be related to local trauma or inflammation[5], but this patient had no history of trauma. The disease can occur at any age, it is more common in patients between 20 and 40 years old, and there is no difference in race or sex prevalence. Local complete resection can be curative, and some cases can even disappear spon-taneously[6]. Deep NF may show infiltration and growth, and it is easily misdiagnosed clinically, even as soft tissue sarcoma.
The important clinical features of NF are a short course of disease, usually less than 3 mo, and rapid progression, usually 1-2 wk. It is rare for patients to present with a history of more than 1 year[7]. More than half of the patients show single, solid, fast-growing subcutaneous nodules and poor mobility, often accompanied by local pain and tenderness. Some of the lesions were deep and could be located in the skeletal muscle under the fascia or showed an oval mass in the space of the deep muscle group, which was difficult to detect in the early stage. This case of NF was located under the skin of the left occipital area and was progressively enlarged, which were beneficial for early detection and treatment.
Clinically and radiologically, NF can be divided into subcutaneous, fascial, and intramuscular types depending on the relationship to anatomic location[1]. Subcutaneous type is the most common, while other rare types include intradermal type and intravascular type[8]. There is a certain correlation between NF imaging classification and anatomical site: (1) The superficial position of subcutaneous NF is easy to find, and most show local protuberance of the face and neck and a nodular shape; (2) Fascial NF can grow inward or outward along the subcutaneous fascia layer or extend around, but it does not break through the fascia layer, similar to inflammatory lesions; some of the nodules can also be located in the deep muscle space and are difficult to detect in the early stage, so the lesion is larger when found, similar to soft tissue tumors. In this case, the nodule grew close to the superficial fascia of the left occipital and pushed the subcutaneous fat outward, so it should belong to the fascia type; and (3) The intramuscular NF is often located in the subcutaneous skeletal muscle, which is round or oval in shape, large in size, easily associated with peritumoral edema, and similar to soft tissue tumors.
In previous reports, on CT, NF showed a round or oval soft tissue dense mass growing close to the fascia, with a clear boundary with the surrounding fat space and muscle, and a few lesions showed invasive signs, such as unclear boundaries with the surrounding muscle group or adjacent bone destruction[5]. In this case, the fascia surface where the mass was attached could be clearly seen on CT; some of the fascia thickened and extended to both ends, but the fascia layer was not damaged and the adjacent fat space was clear (Figure 1A). We speculate that the above signs reflect the benign growth pattern of NF. The lesion originated from the fascia, and the fascia is a layer of dense connective tissue, so it did not destroy the fascia layer. Moreover, no adjacent bone destruction was found in this case (Figure 1B). The density of NF was slightly lower than or equal to that of muscle, the boundary was clear, and it showed obvious uniform or inhomogeneous enhancement after contrast-enhancement. We speculate that the difference in the enhancement modes may be related to the difference in the tissue content in the image focus and to the time of disease progression.
There is a certain correlation between the MRI findings of NF and the pathological classification. Pathologically, lesions in NF can be separated into three types: Myxoid, cellular, and fibrous[9]. The lesion composition reflects the different stages of the disease. NF often contains more mucus in the early stage, which gradually decreases with the maturity of the lesion, and the cellular components are gradually increasing, while NF contains more collagen fibers in the late stage. Different pathological composition types can be seen in the same focus, which is the basis for the difference in MRI signals[10]. In this case, the central signal of the lesion on T2WI was higher than that of the periphery, and the peripheral enhancement was more significant than that of the center, showing a characteristic "inverted target sign" (Figure 1D and E). We hypothesize that the appearance of this sign may reflect that there are more mucous components in the central part of the focus and more cellular structures in the periphery, so the signal intensity in the central area of the T2WI is higher than that in the peripheral area, and the degree of vascularization in the area with rich peripheral cells is higher than that in the area with more central mucus content, so there was circular enhancement after contrast-enhancement. Some scholars[11] think that the "fascial tail sign" is a sign unique to NF, which shows that the focus extends linearly along the fascia facing both ends and shows obvious enhancement after contrast-enhancement. This sign can also be seen in this case (Figure 1F).
Nodular fasciitis should be distinguished from neurogenic tumors, desmoid fibromatosis, malignant fibrous histiocytoma, fibrosarcoma, and other diseases. Imaging examination is helpful, while histopathology and immuno-histochemistry play a key role in differential diagnosis. Because NF is neither an inflammatory disease nor a true tumor, it is considered a fibroblast proliferative benign disease, so local surgical resection is the first choice for the treatment of this disease. At present, there is no case report of postoperative recurrence. Of course, some scholars[12] proposed that NF has a self-limited course of disease, but the specific results need to be further explored in future clinical follow-up.
In summary, the possibility of NF should be considered for nodules or masses with rapid growth and tenderness in the subcutaneous or intermuscular space of the head and neck. CT and MRI examinations, combined with clinical manifestations and histopathological examination, can improve the diagnostic accuracy for the disease.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vinh-Hung V S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Shin JH, Lee HK, Cho KJ, Han MH, Na DG, Choi CG, Suh DC. Nodular fasciitis of the head and neck: radiographic findings. Clin Imaging. 2003;27:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Hu PA, Zhou ZR. Imaging findings of radiologically misdiagnosed nodular fasciitis. Acta Radiol. 2019;60:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Fang SG. WHO (2017) Classification of head and neck tumors. Zhenduan Binglixue Zazhi. 2017;24:638-641. [DOI] [Full Text] |
| 4. | Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91:1427-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 237] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Singh S, Paul S, Dhall K, Khichy S. Nodular fasciitis: a diagnostic challenge. Indian J Pathol Microbiol. 2013;56:288-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Cui ZY. Clinical analysis of 28 cases of nodular fasciitis. Shiyong Shou Waike Zazhi. 2018;32:401-403+406. [DOI] [Full Text] |
| 7. | Shi ST. Diagnosis and treatment of nodular fasciitis: a report of 27 cases. Zhejiang Chaungshang Waike Zazhi. 2013;18:843-844. [DOI] [Full Text] |
| 8. | Liu YH, Zhang SX, Luo JY, Chen JC, Zhou GC. CT and MRI Manifestations of nodular fasciitis. Fangshexue Shijian Zazhi. 2014;29:433-436. [DOI] [Full Text] |
| 9. | Wang XL, De Schepper AM, Vanhoenacker F, De Raeve H, Gielen J, Aparisi F, Rausin L, Somville J. Nodular fasciitis: correlation of MRI findings and histopathology. Skeletal Radiol. 2002;31:155-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 88] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Liu ZS, Wang JM, Huang YH, Luo XM, Li ZY, Long WS, Li RG. Comparative analysis of MRI features and histopathological classification of nodular fasciitis. Zhongguo Yixue Yingxiang Jishu Zazhi. 2016;32 (5):781-784. [DOI] [Full Text] |
| 11. | Jiao CL, Wang YX, Liu H, Chen ZJ. Clinical and CT diagnosis of nodular fasciitis. Fangshexue Shijian Zazhi. 2015;30:378-380. [DOI] [Full Text] |
| 12. | Wu XF, Huang JC, Yang QT, Liu X, Zhang GH. Diagnosis and treatment of nodular fasciitis in external nose. Zhongguo Erbi Yanhou Toujiang Waike Zazhi. 2016;23:476-478. [DOI] [Full Text] |