Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6136
Peer-review started: June 27, 2020
First decision: September 23, 2020
Revised: October 5, 2020
Accepted: October 19, 2020
Article in press: October 19, 2020
Published online: December 6, 2020
Processing time: 160 Days and 8.2 Hours
Posterior atlantoaxial dislocation (PAD) is a rare type of upper cervical spine disease. We sought to describe a unreported case of old PAD with os odontoideum (OO) and atlas hypoplasia (AH) and our unique treatment approach consisting of C1 single door laminoplasty with C1-3 posterior fixation and fusion.
A 70-year-old male patient who suffered from progressive aggravating numbness and limb weakness for 4 years without trauma, was diagnosed with old PAD with OO and AH. The patient underwent closed reduction and C1 single door laminoplasty with C1-3 posterior fixation and fusion instead of C1 laminectomy with occipitocervical fusion. During the 3-year follow-up, he was able to walk by himself instead of using a wheelchair and with a ± 25° range of head rotation as well as a ± 10° range of flexion-extension. Three-year follow-up images showed satisfactory reduction and fusion.
C1 single door laminoplasty with cervical fusion in PAD combined with spinal cord compression could be a suitable and effective surgical option. Compared with laminectomy and occipitocervical fusion, it retains more cervical range of motion, has a smaller incision and provides an adequate bone grafting space for atlantoaxial fusion.
Core Tip: This article describes an unreported case of old posterior atlantoaxial dislocation with os odontoideum and atlas hypoplasia. C1 single door laminoplasty with C1-3 posterior fixation and fusion was performed as surgical treatment, which retained partial range of motion, decreased operative trauma and provided an adequate bone grafting space for atlantoaxial fusion compared with laminectomy and occipitocervical fusion.
- Citation: Zhu Y, Wu XX, Jiang AQ, Li XF, Yang HL, Jiang WM. Single door laminoplasty plus posterior fusion for posterior atlantoaxial dislocation with congenital malformation: A case report and review of literature. World J Clin Cases 2020; 8(23): 6136-6143
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6136.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6136
Posterior atlantoaxial dislocation (PAD) is a rare disease which only accounts for approximately 0.3% of all cervical spine injuries and 1.7% of upper cervical spine injuries[1]. To date, only 29 cases of PAD of several types have been reported, all of which have been due to traumatic accidents[2-29]. Herein, a unreported case of old PAD with os odontoideum (OO) and atlas hypoplasia (AH) is introduced, as well as our unique treatment approach consisting of C1 single door laminoplasty with C1-3 posterior fixation and fusion.
A 70-year-old male patient suffered from progressive aggravating numbness and weakness of limbs.
The patient’s symptoms started 5 years ago without any trauma or accident. When admitted to our hospital, he could only move using a wheelchair.
The patient had no previous relevant medical history.
The patient had no previous relevant family history.
The results of physical examination revealed that the grip strength in both hands was grade 3, the muscle tension of both lower limbs was high, bilateral Hoffman sign was positive, knee and ankle reflexes were hyperactive, and ankle clonus was positive.
Laboratory examinations showed no obvious deficits.
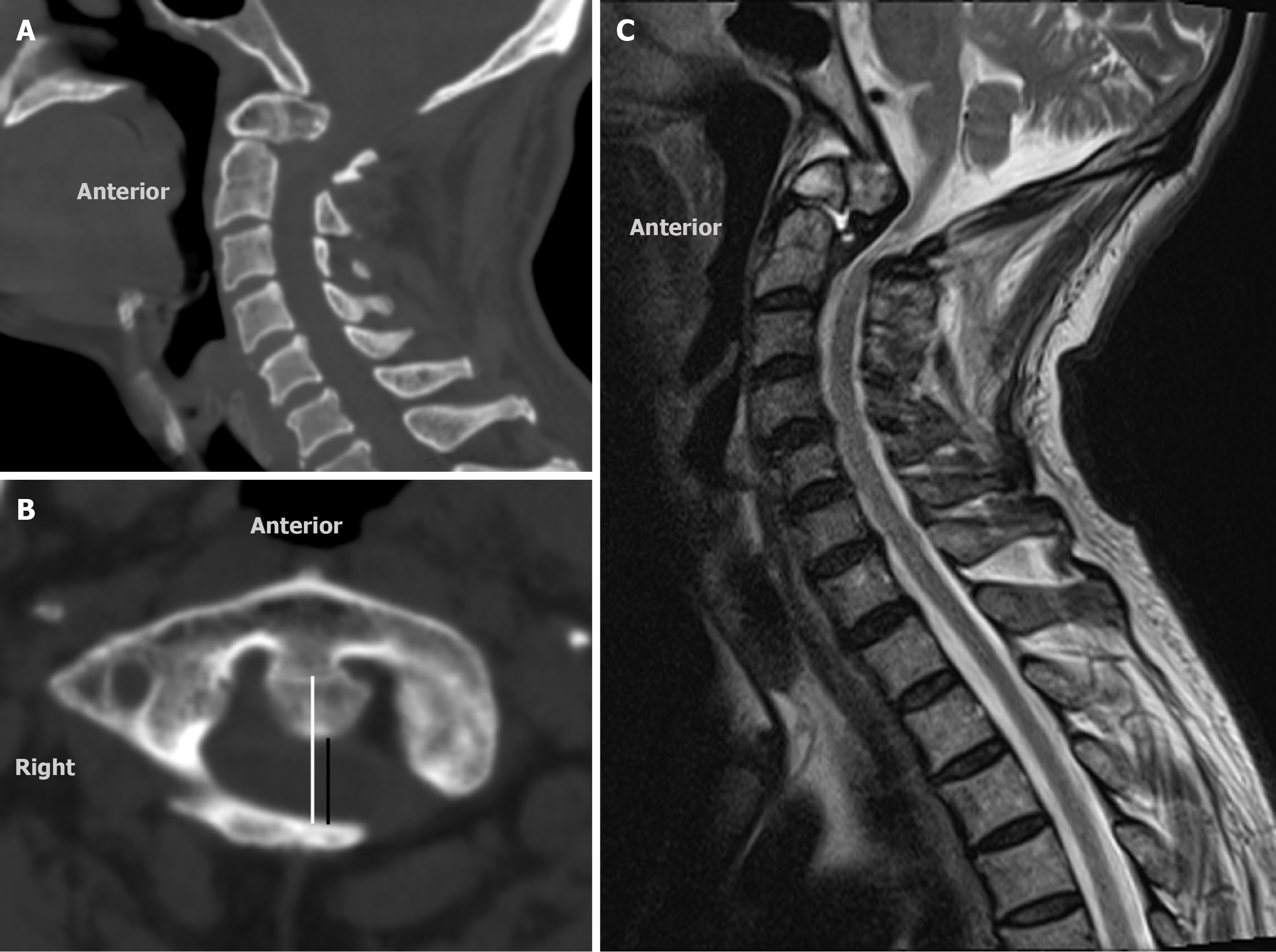
Considering that there was no history of trauma, and the borders of the odontoid free body and basis were smooth and rounded, an old PAD combined with OO was diagnosed based on computed tomography (CT) results (Figure 1A). The C1 inner sagittal diameter was 22.51 mm (Figure 1B) which supported the diagnosis of AH[30]. The results of magnetic resonance imaging (MRI) (Figure 1C) showed that the spine cord was constricted by the odontoid process and the signal of the spine had changed at the level of atlantoaxial dislocation.
The final diagnosis in the presented case was an old PAD combined with OO and AH.
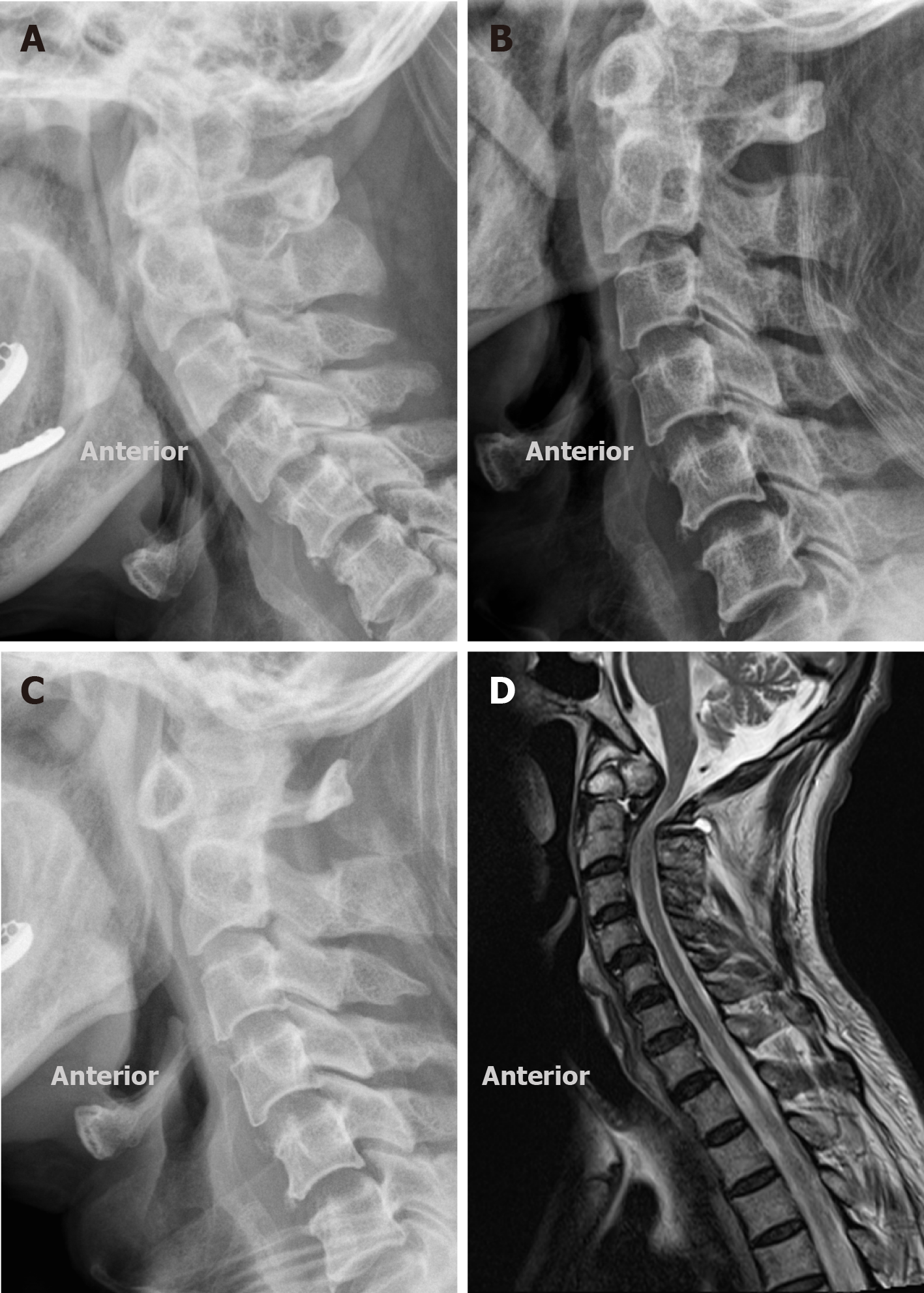
Due to the mechanism of posterior dislocation, skull traction was performed under a flexed position of the cervical spine with an initial weight of 3.5 kg and gradually increased to 7.5 kg, and the flexed angle also increased synchronously. Lateral radiographs (Figure 2A-C) were obtained on the fourth day, the eighth day and the twelfth day after skull traction. MRI (Figure 2D) after skull traction demonstrated satisfactory reduction of the dislocation, but the cervical canal was compressed again by the posterior arch of C1 due to AH. Therefore, decompression surgery was necessary.
The surgery was performed under general anesthesia and in the prone position. Cortical somatosensory evoked potential (CSEP) was utilized to monitor the neurological condition. The reference frame of the 3-dimensional navigation system was placed on the spinous process of C4 through an isolated small incision. Then the surgeons inserted 5 pedicle screws in C1, C2 (right side) and C3 under the guidance of the O-arm machine and navigation. The C1 single door laminoplasty was performed with the assistance of a surgical electric grinder and a piezosurgery osteotomy. Bone autograft mixed with bone allograft was placed between C1 and C2 posterior arch as an atlantoaxial fusion. There was no specific medication except routine methylprednisolone, omeprazole, antibiotics and dehydration.
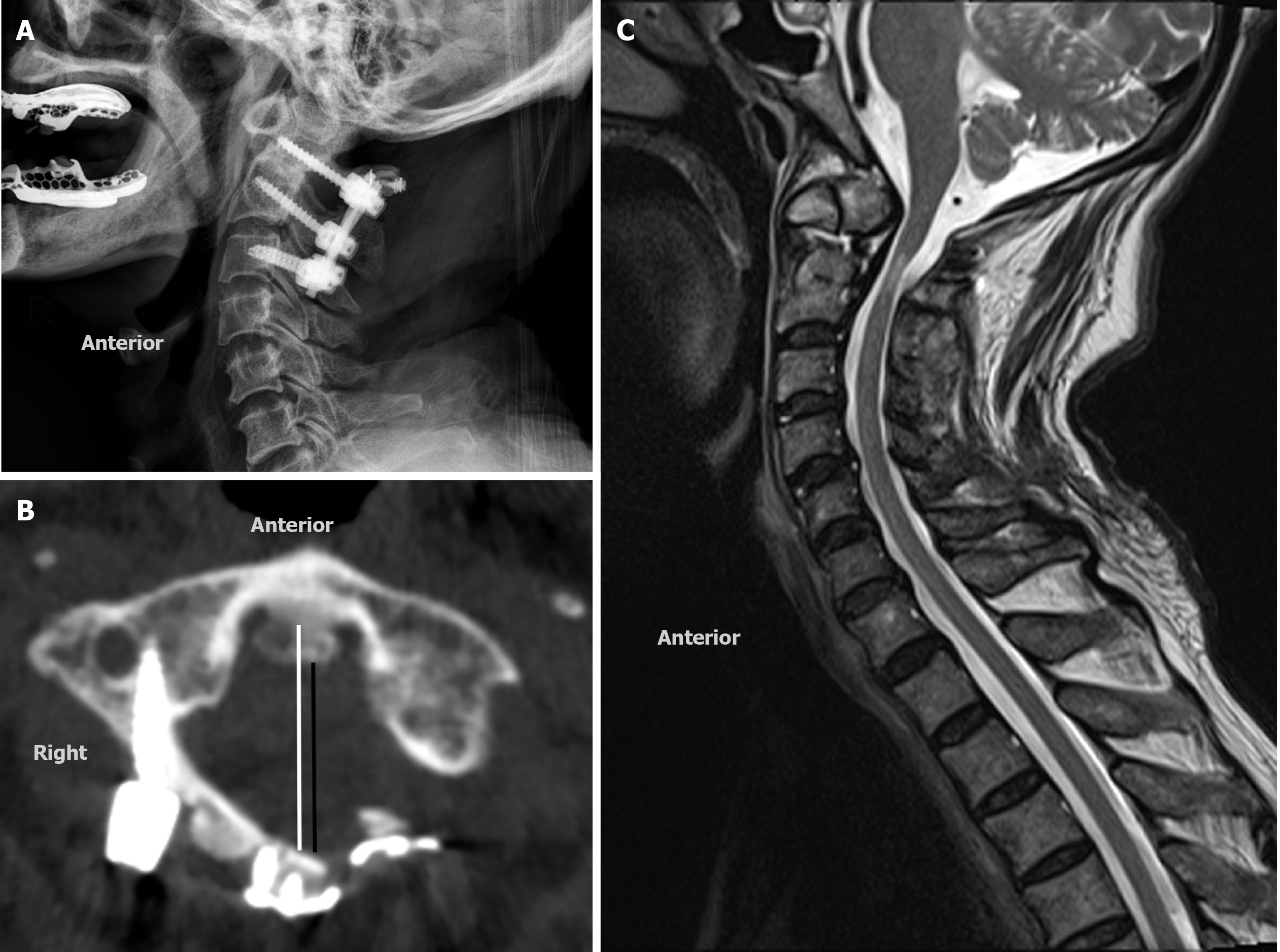
The grip strength in both hands was improved after skull traction and surgery, as well as muscle tension of the lower limbs. Neurological signs including Hoffman, Babinski and ankle clonus returned to normal. During the 3-year follow-up, he was able to walk by himself instead of using a wheelchair and with a ± 25° range of head rotation as well as a ± 10° range of flexion-extension. Three-year follow-up images showed satisfactory reduction and fusion (Figure 3).
A total of 29 PAD patients with or without fracture and neurological deficit were found following a thorough literature review of PubMed, Elsevier, MEDLINE and Web of Science (Table 1). The rarity of this dislocation is mainly due to the anatomical locking structure as the dorsal ligament of the osseo-ligamentous ring is easily damaged compared to the odontoid process and hence anterior atlantoaxial dislocation occurs more frequently[31]. The treatment methods for PAD include closed reduction (mostly skull traction), open reduction (mostly odontoidectomy), anterior odontoid screw fixation and posterior fusion. Skull traction was first reported in a case of PAD without fracture or neurological deficit by Haralson et al[2] and gradually became the first choice for conservative treatment and preoperative reduction. However, closed reduction was considered to be a risky procedure especially when the patient was under anesthesia. Sud et al[11] reported a case who developed quadriparesis during traction which might lead to transient over-distraction of the spinal cord. Open reduction was considered a second choice after ineffective closed reduction[13,15-19,23-25,28].
| No. | Ref. | Patient | Fracture | Neurological deficit | Treatment |
| 1 | Haralson et al[2], 1969 | 30, M | N | N | CR + WF |
| 2 | Sassard et al[3], 1974 | 20, F | N | Y | CR |
| 3 | Patzakis et al[4], 1974 | 37, M | N | N | CR |
| 4 | Fox et al[5], 1977 | 65, M | Y | Y | OR + WF |
| 5 | Jamshidi et al[6], 1983 | 22, M | N | N | CR + WF |
| 6 | Autricque et al[7], 1986 | 45, M | Y | Y | CR |
| 7 | Autricque et al[7], 1986 | 63, M | Y | N | CR + OCF |
| 8 | Wong et al[8], 1991 | 23, M | N | Y | CR + AAF |
| 9 | Fujimura et al[9], 1997 | 54, M | N | N | CR |
| 10 | Carroll et al[10], 2001 | 19, F | N | Y | CR |
| 11 | Sud et al[11], 2002 | 38, M | N | N | OR + SF |
| 12 | Neumann et al[120], 2003 | 22, M | N | N | CR |
| 13 | Yoon et al[13], 2003 | 64, M | N | Y | OR + AAF |
| 14 | Chaudhary et al[14], 2008 | 35, F | N | Y | CR |
| 15 | Amirjamshidi et al[15], 2009 | 31, M | N | Y | OR + AAF |
| 16 | Jiang et al[16], 2010 | 48, M | N | N | OR + SF |
| 17 | Zhen et al[17], 2011 | 44, M | N | N | OR + AAF |
| 18 | Zhang et al[18], 2012 | 38, M | Y | Y | OR1 |
| 19 | Moreau et al[19], 2012 | 65, M | Y | N | OR + OCF |
| 20 | Kambali et al[20], 2013 | 32, M | N | Y | CR + AAF |
| 21 | Riouallon et al[21], 2014 | 25, M | Y | N | CR + SF |
| 22 | Meng et al[22], 2014 | 47, F | Y | N | CR + WF |
| 23 | Xu et al[23], 2015 | 54, M | N | Y | OR + AAF |
| 24 | Hu et al[24], 2015 | 50, M | N | Y | OR + AAF |
| 25 | He et al[25], 2016 | 72, M | Y | Y | OR + C1-3 F |
| 26 | Minyu et al[26], 2018 | 30, M | Y | N | CR + AAF |
| 27 | Ghailane et al[27], 2019 | 89, M | Y (C1 fracture) | N | CR |
| 28 | Ning et al[28], 2019 | 52, M | N | N | OR + AAF |
| 29 | Nowell et al[29], 2019 | 71, M | Y (Jefferson fracture) | N | CR + AAF |
| 30 | Our case | 70, M | Y (OO) | Y (AH) | CR + C1-3 F |
To date, there is no consensus as to whether surgical fixation and fusion should be performed. An atypical case of PAD with C1 anterior arch fracture was treated by closed reduction under anesthesia without fusion because it was believed that there was no ligamentous instability due to the mechanism of PAD[27]. Hu et al[24] concluded that the need for fusion after successful closed reduction depends on the integrity of the transverse ligament and the stability of the cervical spine. However, evaluation of the condition of ligaments and stability of the cervical spine remains to be solved. Of these previously published cases, 21/29 underwent fixation or fusion, which indicated that most of the doctors were inclined to strengthen the stability by fusion.
What distinguishes our case from previous cases is the existence of OO and AH, as well as the adoption of decompression and fusion as the surgical strategy. Hypoplasia occurs when the sagittal diameter of the atlas is less than or equal to 26 mm[30]. Fareed et al[32] indicated that PAD was more likely to occur in OO patients due to deficient ossification of the odontoid and hyperlaxity of the ligament ring.
During the treatment of our patient, two important points should be noted. One was the preoperative flexed-positional skull traction. Soft and scar tissue adhesion caused by an old PAD could form a strong counterforce against rapid reduction, and long-term high weight traction could stretch the bound tissue gently and gradually. Additionally, the mildness and progressivity of sustained traction might effectively reduce the risk of transient over-distraction and stimulation of the spinal cord. Preoperative closed reduction is safer than intraoperative closed reduction under anesthesia, especially for old dislocations.
The other point is the unique surgical procedure. The conventional surgical procedure might be C1 laminectomy with occipitocervical fusion[33], which has the disadvantages of larger surgical injury and less range of head motion compared with C1 laminoplasty with cervical fusion that has not been reported so far. Boniello et al[34] suggested that laminoplasty results in decreased length of stay, readmissions and complications compared with laminectomy. Noguchi et al[35] indicated that laminoplasty was a safe and useful procedure for AH. To the best of our knowledge, C1 laminoplasty can retain one side of the pedicle, which makes atlantoaxial fusion possible and results in an adequate bone grafting space to increase the success rate of fusion. Yang et al[36] demonstrated that bone grafting of the atlantoaxial joint plays an important role in increasing the fusion rate of atlantoaxial fusion. Conversely, C1 laminectomy would inevitably lead to occipitocervical fusion, which would lead to the loss of more cervical range of motion with increased operative injury.
C1 single door laminoplasty with fusion for PAD combined with spinal cord compression could be a suitable and effective surgical option. Compared with laminectomy and occipitocervical fusion, it retains partial range of motion, decreases operative injury and provides an adequate bone grafting space for atlantoaxial fusion. An effective flexed-positional skull traction is vital in patients diagnosed with PAD. These findings require verification by further prospective, randomized studies.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kung WM, Widmer KH S-Editor: Gao CC L-Editor: Webster JR P-Editor: Wang LL
| 1. | Gleizes V, Jacquot FP, Signoret F, Feron JM. Combined injuries in the upper cervical spine: clinical and epidemiological data over a 14-year period. Eur Spine J. 2000;9:386-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Haralson RH 3rd, Boyd HB. Posterior dislocation of the atlas on the axis without fracture. Report of a case. J Bone Joint Surg Am. 1969;51:561-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Sassard WR, Heinig CF, Pitts WR. Posterior atlanto-axial dislocation without fracture. Case report with successful conservative treatment. J Bone Joint Surg Am. 1974;56:625-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Patzakis MJ, Knopf A, Elfering M, Hoffer M, Harvey JP Jr. Posterior dislocation of the atlas on the axis; a case report. J Bone Joint Surg Am. 1974;56:1260-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Fox JL, Jerez A. An unusual atlanto-axial dislocation. Case report. J Neurosurg. 1977;47:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Jamshidi S, Dennis MW, Azzam C, Karim N. Traumatic posterior atlantoaxial dislocation without neurological deficit: case report. Neurosurgery. 1983;12:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Autricque A, Lesoin F, Villette L, Franz K, Pruvo JP, Jomin M. [Fracture of the odontoid process and C1-C2 Lateral luxation. 2 cases]. Ann Chir. 1986;40:397-400. [PubMed] |
| 8. | Wong DA, Mack RP, Craigmile TK. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine (Phila Pa 1976). 1991;16:587-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Fujimura Y, Nakamura M, Kobayashi K. Posterior dislocation of the atlas on the axis without fracture: a case report. J Orthopaedic Surg. 1997;5:81-84. |
| 10. | Shih WJ. Sample size re-estimation - journey for a decade. Stat Med. 2001;20:515-8; discussion 519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Sud S, Chaturvedi S, Buxi TB, Singh S. Posterior atlantoaxial dislocation without associated fracture. Skeletal Radiol. 2002;31:529-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Neumann U, Urbanski H, Riedel K. Posterior atlantoaxial dislocation without fracture of the odontoid. A case report. J Bone Joint Surg Am. 2003;85:1343-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Yoon DH, Yang KH, Kim KN, Oh SH. Posterior atlantoaxial dislocation without fracture. Case report. J Neurosurg. 2003;98:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Chaudhary R, Chaudhary K, Metkar U, Rathod A, Raut A, Sanghvi D. Posterior atlantoaxial dislocation without odontoid fracture. Skeletal Radiol. 2008;37:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Amirjamshidi A, Abbassioun K, Khazenifar M, Esmailijah A. Traumatic rotary posterior dislocation of the atlas on the axis without fracture. Report of a case and review of literature. Surg Neurol. 2009;71:92-97; discussion 98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Jiang LS, Shen L, Wang W, Wu H, Dai LY. Posterior atlantoaxial dislocation without fracture and neurologic deficit: a case report and the review of literature. Eur Spine J. 2010;19 Suppl 2:S118-S123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Zhen P, Lan X, Yang LW. Traumatic posterior atlantoaxial dislocation without associated fracture and neurological deficit. Arch Orthop Trauma Surg. 2011;131:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Zhang K, Xu J, Wang Q, Wang G, Wu Z, Xia H, Yin QS. Treatment of dens fractures with posterior atlantoaxial dislocation with transoral atlantoaxial reduction plate surgery: case report and introduction of a novel treatment option. Spine (Phila Pa 1976). 2012;37:E451-E455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Moreau PE, Nguyen V, Atallah A, Kassab G, Thiong'o MW, Laporte C. Traumatic atlantoaxial dislocation with odontoid fracture: A case report. Orthop Traumatol Surg Res. 2012;98:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Kambali M, Anand HV, Priyamargavi H, Varma RB. Traumatic posterior atlantoaxial dislocation without related fractures of C1-C2. Indian J Orthop. 2013;47:624-629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Riouallon G, Pascal-Moussellard H. Atlanto-axial dislocation complicating a type II odontoid fracture. Reduction and final fixation. Orthop Traumatol Surg Res. 2014;100:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Meng H, Gao Y, Li M, Luo Z, Du J. Posterior atlantoaxial dislocation complicating odontoid fracture without neurologic deficit: a case report and review of the literature. Skeletal Radiol. 2014;43:1001-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Xu Y, Li F, Guan H, Xiong W. Traumatic Posterior Atlantoaxial Dislocation Without Associated Fracture but With Neurological Deficit: A Case Report and Literature Review. Medicine (Baltimore). 2015;94:e1768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Hu D, Yang X, Wang J. Traumatic Posterior Atlantoaxial Dislocation Without Fracture of Odontoid Process: A Case Report and Systematic Analysis of 19 Cases. J Orthop Trauma. 2015;29:e342-e345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | He DW, Huang WJ, Sheng XY, Wu LJ, Fan SW. Atlantoaxial Joint Interlocking Following Type II Odontoid Fracture Associated with Posterolateral Atlantoaxial Dislocation: a Case Report and Review of Published Reports. Orthop Surg. 2016;8:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Minyu Z, Shiyang W, Suraj C, Kelun H, Chaowei L, Honglin T. Traumatic Posterolateral C1-C2 Dislocation Complicated with Locked Lateral Mass and Type II Odontoid Fracture-5-Year Follow-up. World Neurosurg. 2018;114:330-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Ghailane S, Alsofyani MA, Pointillart V, Bouloussa H, Gille O. Traumatic posterior Atlanto-axial dislocation: case report of an atypical C1-C2 dislocation with an anterior arch fracture of C1. BMC Musculoskelet Disord. 2019;20:612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Ning S, Yang S, Ding W, Ma T, Wu Z. Posterior atlantoaxial dislocation without fracture or neurological symptoms treated by transoral-posterior approach surgery: a case report and literature review. Eur Spine J. 2019;28:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Nowell M, Nelson R. Traumatic posterior atlantoaxial dislocation with associated C1 Jefferson fracture and bilateral vertebral artery occlusion without odontoid process fracture or neurological deficit. Eur Spine J. 2019;28:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Kelly MP, Oshima Y, Yeom JS, Agarwal R, Bajwa NS, Riew KD. Defining hyoplasia of the atlas: a cadaveric study. Spine (Phila Pa 1976). 2014;39:E1243-E1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61:1119-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 497] [Cited by in RCA: 395] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 32. | Jumah F, Alkhdour S, Mansour S, He P, Hroub A, Adeeb N, Hanif R, Mortazavi MM, Tubbs RS, Nanda A. Os Odontoideum: A Comprehensive Clinical and Surgical Review. Cureus. 2017;9:e1551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Tarukado K, Ikuta K, Iida K, Tono O, Doi T, Harimaya K. Radiographic and Clinical Results of C1 Laminoplasty for the Treatment of Compressive Myelopathy. Asian Spine J. 2020;14:459-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Boniello A, Petrucelli P, Kerbel Y, Horn S, Bortz CA, Brown AE, Pierce KE, Alas H, Khalsa A, Passias P. Short-term Outcomes Following Cervical Laminoplasty and Decompression and Fusion With Instrumentation. Spine (Phila Pa 1976). 2019;44:E1018-E1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Noguchi A, Harada Y, Okabe S, Kohno T, Kamata K, Takahashi H. [A surgical case of cervical canal stenosis caused by atlas hypoplasia in an elderly patient]. No Shinkei Geka. 1998;26:623-626. [PubMed] |
| 36. | Yang JS, Chen H, Chu L, Liu P, Yan L, Liu TJ, Tian F, Zhang JN, Hao DJ. Does Additional Bone Grafting of Atlantoaxial Joint Increase Bone Fusion Rate of Iliac Crest Autograft in Posterior Occipitocervical Fusion? World Neurosurg. 2019;125:e29-e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |