Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6103
Peer-review started: June 10, 2020
First decision: September 24, 2020
Revised: October 1, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: December 6, 2020
Processing time: 176 Days and 22.9 Hours
Single-port laparoscopy has been used in a variety of abdominal operations. We report the first case of single-port laparoscopic left lateral sectionectomy in pediatric laparoscopic living donor liver transplantation.
A 28-year-old man volunteered for living liver donation to his daughter who was diagnosed with liver cirrhosis and portal hypertension after the Kasai procedure for biliary atresia. His body mass index was 20.5 kg/m2. Liver dynamic computed tomography showed: (1) Left lateral graft volume of 232.76 cm3 with a graft-to-recipient weight ratio of 2.59%; and (2) Right hepatic artery derived from the superior mesenteric artery. A single-port access system was placed through a transumbilical incision, including four trocars: two 12-mm ports for a camera and endoscopic stapler and two 5-mm working ports. Liver parenchyma was dissected by a Harmonic and Cavitron Ultrasonic Surgical Aspirator, while bipolar was used for coagulation. The bile duct was transected above the bifurcation by indocyanine green fluorescence cholangiography. The specimen was retrieved from the umbilical incision. The total operation time was 4 h without blood transfusion. The final graft weight was 233.6 g with graft-to-recipient weight ratio of 2.60%. The donor was discharged uneventfully on postoperative day 4.
Single-port laparoscopic left lateral sectionectomy is feasible in pediatric laparoscopic living donor liver transplantation in an experienced transplant center.
Core Tip: Due to the accumulated experience of laparoscopic hepatectomy in living donor liver transplantation, laparoscopic left lateral sectionectomy (L-LLS) has been acknowledged as a standard practice in pediatric living donor liver transplantation. The single-port laparoscopic technique has been used in a variety of abdominal surgeries, especially the single-port L-LLS. We report the first case of L-LLS in pediatric laparoscopic living donor liver transplantation by the single-port approach, focusing on the surgical procedure and how to achieve feasible manipulation due to the challenge of little operative space through the transumbilical port.
- Citation: Li H, Wei L, Zeng Z, Qu W, Zhu ZJ. Laparoscopic left lateral sectionectomy in pediatric living donor liver transplantation by single-port approach: A case report. World J Clin Cases 2020; 8(23): 6103-6109
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6103.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6103
Laparoscopic hepatectomy has been proved to be a feasible and safe procedure in liver surgery in recent decades[1]. Since the first single-port laparoscopic hepatectomy was reported in 2010 by Kobayashi et al[2], single-port laparoscopy has been applied to a variety of abdominal operations, especially laparoscopic left lateral sectionectomy (L-LLS)[3]. In 2002, Cherqui et al[4] first described L-LLS for adult-to-pediatric donation. The safety and feasibility of the technique was similar to those obtained by conventional approaches for both donors and recipients[5]. Nowadays, L-LLS is acknowledged as a standard practice in pediatric living donor liver transplantation (PLDLT)[6,7]. Decreasing donors’ perioperative risks is essential in LDLT. Compared to standard multiport laparoscopic hepatectomy, single-port laparoscopic hepatectomy has been adopted to reduce the number of ports and corresponding abdominal incisions, which may lead to rapid recovery and superior cosmetic results, conferring potential advantages over multiport procedures[8]. As a result, single-port L-LLS is considered to potentially benefit donors. We report the first case of L-LLS in PLDLT using a single-port approach.
The donor was a 28-year-old man who volunteered for living liver donation to his daughter. The recipient was a 14-mo-old girl who presented to our center with the complaint of repeated hematemesis for 2 wk.
The donor had no significant present medical condition. The recipient was diagnosed with biliary atresia 1 mo after birth. A Kasai operation was performed. Approximately 2 wk before presenting to our center, she suffered from repeated hematemesis three times. Hepatosplenomegaly and esophagogastric varices were detected after physical and endoscopic examination.
The donor and recipient had no other significant medical history. A history of hypertension, diabetes, coronary heart disease and other chronic disease was denied.
The donor and recipient had no significant personal and family history.
The donor’s weight was 62 kg and height was 174 cm, with a body mass index (BMI) of 20.5 kg/m2. The recipient’s physical examination showed liver disease with mild jaundice, poor nutrition, abdominal swelling and hepatosplenomegaly. Her weight was 9 kg and height was 75 cm, with a BMI of 16 kg/m2.
For the donor, laboratory examinations showed no abnormal results, and he was Child–Pugh Grade A (score 5). For the recipient, laboratory examinations on admission revealed a hemoglobin level of 91 g/L, platelet count of 163 × 109/L, white blood cell count of 7.66 × 109/L, alanine aminotransferase (ALT) 28 U/L, albumin 30.8 g/L, total bilirubin (TBIL) 16.78 µmol/L, direct bilirubin 7.61 µmol/L, and creatinine 22.9 µmol/L. Her prothrombin time was 14.50 s, and international normalized ratio was 1.29. Combined with imaging examination, she was Child–Pugh Grade B (score 7) and pediatric end-stage liver disease score was 8.
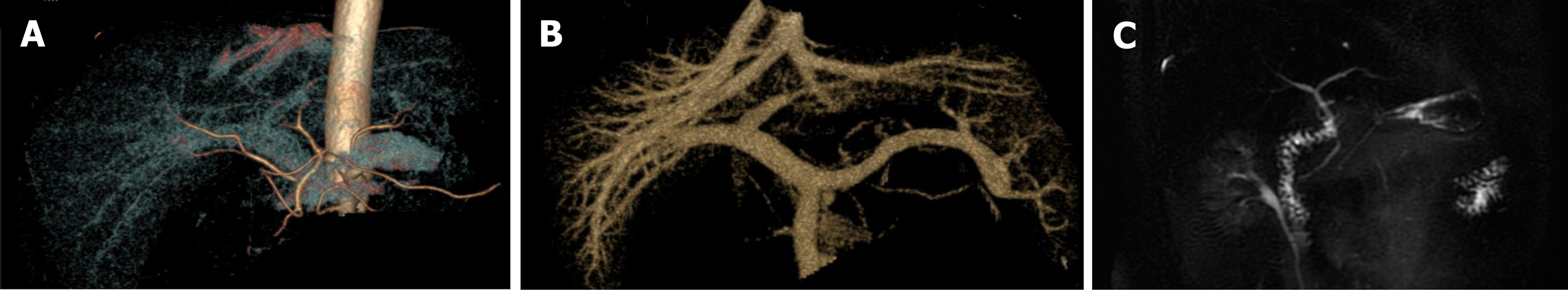
For the donor, liver dynamic computed tomography and magnetic resonance imaging showed: (1) Left lateral graft volume of 232.76 cm3 with a graft-to-recipient weight ratio of 2.59%; (2) Right hepatic artery derived from the superior mesenteric artery; and (3) No anatomical variation in the portal vein, hepatic vein and bile duct (Figure 1).
The recipient was diagnosed with liver cirrhosis and portal hypertension after the Kasai operation due to biliary atresia.
A single-port L-LLS was scheduled and performed on the donor for the following reasons: (1) the donor was thin with a BMI of 20.5 kg/m2, which facilitated hepatoduodenal ligament exposure during laparoscopy; (2) he had a shared arterial trunk of the middle and left hepatic arteries, while the right hepatic artery derived from the superior mesenteric artery, which made dissection and preservation easier; and (3) there was no anatomical variation in the left bile duct, portal vein and hepatic vein. Intraoperative indocyanine green (ICG) fluorescence cholangiography was used to determine the bifurcation and division point of the bile duct. The operation was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University.
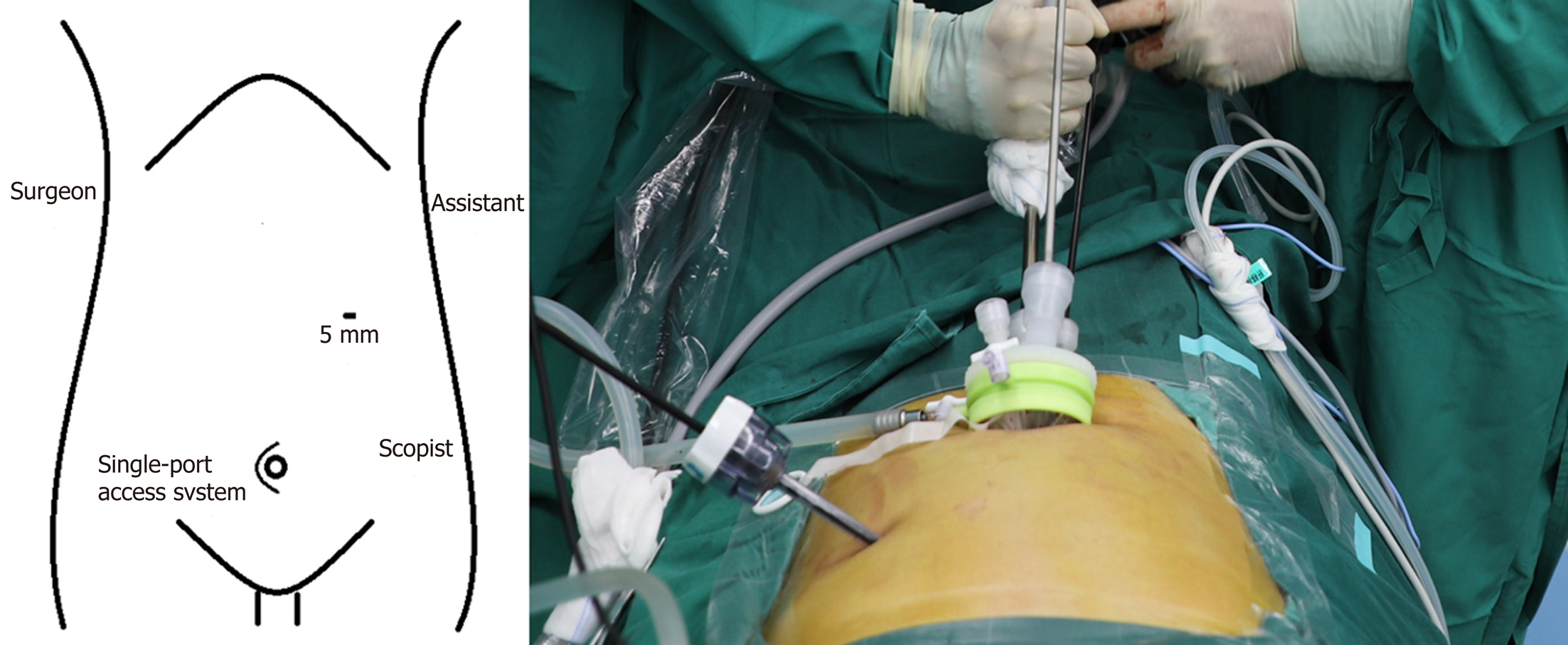
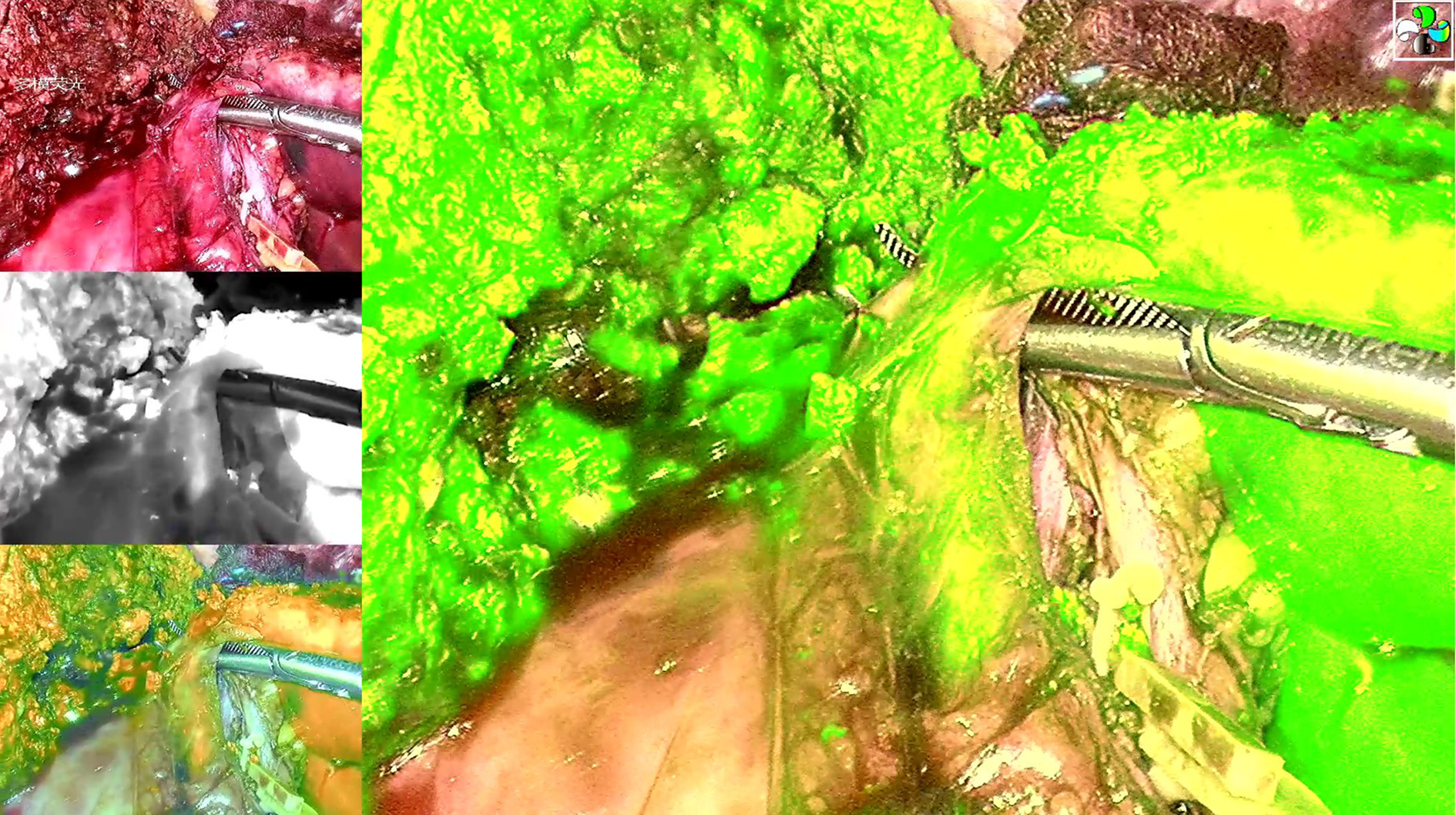
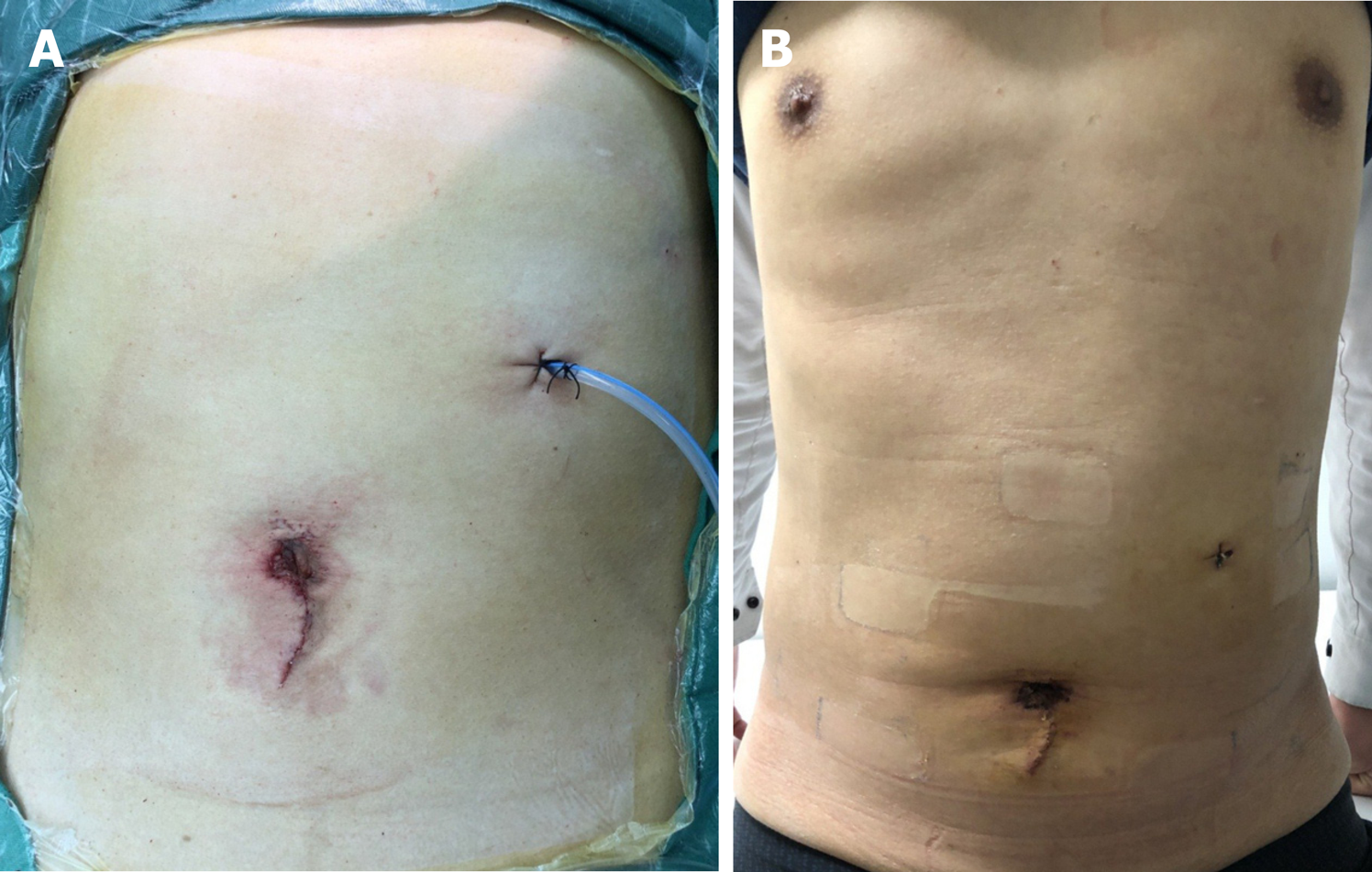
Laparoscopy was performed under carbon dioxide pneumoperitoneum. The insufflation pressure was set at 13 mmHg throughout the surgery. The patient was placed in the supine position in the 30° left and 30° reversed Trendelenburg position. The surgeon stood by the patient’s right side and the assistant and scopist stood by the patient’s left side. A single-port access system was placed through a transumbilical incision, including four trocars: two 12-mm ports for a camera and endoscopic stapler and two 5-mm working ports. A small incision in the right side of the anterior axillary line for the surgical drain was used to place an additional 5-mm port for further assistance (Figure 2). The left portal vein and hepatic artery were temporarily clamped to control bleeding. The liver parenchyma was dissected by the Harmonic and Cavitron Ultrasonic Surgical Aspirator, while bipolar was used for coagulation. The bile duct was transected above the bifurcation by intraoperative ICG fluorescence cholangiography (Figure 3). A one-side linear stapler was used to transect the left hepatic vein. The specimen was retrieved from the umbilical incision. The total operation time was 4 h without blood transfusion. The final graft weight was 233.6 g with graft-to-recipient weight ratio of 2.60%.
The patient-controlled analgesia pump was retrieved within the first 24 h after surgery. The donor’s ALT was 239 U/L, aspartate aminotransferase (AST) was 116 U/L, gamma-glutamyltransferase (GGT) was 22 U/L, and TBIL was 22.57 µmol/L on postoperative day 1, while ALT was 107 U/L, AST was 63 U/L, GGT was 26 U/L, and TBIL was 17.0 µmol/L on postoperative day 3. No complications were observed. The donor was discharged uneventfully on postoperative day 4 (Figure 4). The graft function almost recovered to normal in the recipient on postoperative day 14 (ALT: 44 U/L, AST: 25.9 U/L, GGT: 53 U/L and TBIL: 9.22 µmol/L) without any surgical complications, such as biliary and vascular complications that could theoretically have been caused by imperfect graft procurement.
Due to the advantages of little trauma, reduced postoperative pain, rapid recovery, shorter hospital stay, and minimal incision, single-port L-LLS has been proved to be a safe and feasible approach in liver surgery when treating liver lesions, especially for benign, small and peripheral lesions[9,10]. A recent study revealed that single-port L-LLS incurred a shorter operating time and postoperative hospital stay compared to multiport surgery[11]. Cherqui et al[4] first reported a comparative analysis of L-LLS, resulting in a longer operating time in the laparoscopic group, with significantly decreased blood loss and a trend towards lower overall morbidity compared to the open surgery group. In another retrospective study, Kim et al[5] reported that the laparoscopic group had a significantly shorter hospital stay, whereas the operating time, blood loss, warm ischemic time, and out-of-pocket medical costs were comparable between the open and laparoscopic groups. After a propensity score matching analysis by Broering et al[12], the L-LLS group showed a significant lower blood loss and overall donor complication rate, lower postoperative pain scores, and shorter hospital stay, whereas the operating time and warm ischemic time were significantly longer compared to those in the open group. Therefore, hypothetically, single-port L-LLS should be the most minimally invasive approach for donor surgery in LDLT, compared to either a multiport approach or open surgery.
Most previous comparisons between single-port and traditional multiport laparoscopic hepatectomy were based on liver tumor resection[3,10,11]. Although cirrhosis related to hepatitis virus infection and tumor proximal to major vessels might affect the surgical procedure, single-port procedures still show advantages over multiport approaches. In LDLT, with strict selection criteria, donors are volunteers with normal liver function and liver parenchyma. This might decrease the difficulty with dissection of the liver hilum and parenchyma. In addition, intraoperative bleeding can be controlled more effectively in the donor’s operation. Thus, single-port L-LLS should be an appropriate procedure in PLDLT.
Although the “chopstick effect” and loss of instrumental triangulation are the main barriers in developing single-port laparoscopic hepatectomy[13], according to a technical feature of the surgical intervention of the “caudal” approach, L-LLS should be a good indication for the single-port approach[14]. The parenchymal division can be completed “bottom-up” to the hepatic venous entry after liver mobilization and vessel dissection[14,15]. Compared to right hemihepatectomy or posterosuperior sectionectomy, because the resection can only be performed along the plane of a linear field of view, single-port L-LLS can be performed more easily and safely from the transumbilical incision, without the help of articulation of traditional laparoscopic instruments. This may not increase intraoperative risks in graft procurement.
According to the consensus when adopting a single-port approach in laparoscopic hepatectomy, a small incision is acceptable in the upper abdomen for the surgical drain and is used to place an additional 5-mm port for the safe preparation and resection of the liver[3,10,11]. In our case, in the right side of the anterior axillary line, an additional 5-mm trocar was placed to facilitate liver mobilization and exposure during the parenchymal division.
Donor safety is the primary concern in LDLT. Intraoperative bleeding control and bile duct transection are two major manipulations. Hypothetically, in the case of severe intraoperative bleeding, the transumbilical port could easily be converted into a hand-assisting port and thus be used for manual compression of the liver[3]. After mild dissection of the liver hilum, intraoperative ICG fluorescence cholangiography can be used to determine the bifurcation and division point of the bile duct[16].
An experienced and skilled surgical team (both for donor hepatectomy and advanced laparoscopic surgery) is important for this procedure. Our surgical team had extensive experience in PLDLT (> 1000 cases), laparoscopic liver resection (> 300 cases) and L-LLS (> 60 cases). In addition, L-LLS by the single-port approach should be adopted under strict selection criteria. A suitable donor should meet the following conditions: (1) A thin donor who facilitates better exposure and easier dissection of the hepatic hilum during laparoscopy; (2) Shared arterial trunk of the middle and left hepatic arteries, while the right hepatic artery is derived from the superior mesenteric artery, which makes it easier to be dissected and preserved; and (3) No anatomical variation in the left bile duct, portal vein and hepatic vein.
The success of PLDLT in our case was determined by the outcomes of both donor and recipient. The donor was discharged on postoperative day 4 without any complications, including liver dysfunction, bile leakage or postoperative bleeding. No incisional hernia was found after 3-mo follow up. The recipient’s liver function almost recovered to normal on postoperative day 14 and she was discharged on postoperative day 21 without biliary and vascular complications. The strict selection of donor and recipient and the experienced surgical team might have contributed to these results.
This is the first report of L-LLS for PLDLT using a single-port approach. However, large randomized controlled trials and large case-controlled comparative studies are needed to evaluate the techniques and potential benefits of single-port L-LLS.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Casanova Rituerto D, Kirnap M, Papalois V S-Editor: Zhang L L-Editor: Webster JR P-Editor: Zhang YL
| 1. | Ishizawa T, Gumbs AA, Kokudo N, Gayet B. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg. 2012;256:959-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 274] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 2. | Kobayashi S, Nagano H, Marubashi S, Wada H, Eguchi H, Takeda Y, Tanemura M, Sekimoto M, Doki Y, Mori M. A single-incision laparoscopic hepatectomy for hepatocellular carcinoma: initial experience in a Japanese patient. Minim Invasive Ther Allied Technol. 2010;19:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Struecker B, Haber P, Öllinger R, Bahra M, Pascher A, Pratschke J, Schmelzle M. Comparison of Single-Port Versus Standard Multiport Left Lateral Liver Sectionectomy. Surg Innov. 2018;25:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, Branchereau S, Chardot C, Gauthier F, Fagniez PL, Houssin D. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 2002;359:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 306] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 5. | Kim KH, Jung DH, Park KM, Lee YJ, Kim DY, Kim KM, Lee SG. Comparison of open and laparoscopic live donor left lateral sectionectomy. Br J Surg. 2011;98:1302-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Broering DC, Berardi G, El Sheikh Y, Spagnoli A, Troisi RI. Learning Curve Under Proctorship of Pure Laparoscopic Living Donor Left Lateral Sectionectomy for Pediatric Transplantation. Ann Surg. 2020;271:542-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Soubrane O, de Rougemont O, Kim KH, Samstein B, Mamode N, Boillot O, Troisi RI, Scatton O, Cauchy F, Lee SG, Griesemer A, Ahmed Z, Clavien PA, Cherqui D. Laparoscopic Living Donor Left Lateral Sectionectomy: A New Standard Practice for Donor Hepatectomy. Ann Surg. 2015;262:757-761; discussion 761-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | Benzing C, Krenzien F, Atanasov G, Seehofer D, Sucher R, Zorron R, Pratschke J, Schmelzle M. Single incision laparoscopic liver resection (SILL) - a systematic review. GMS Interdiscip Plast Reconstr Surg DGPW. 2015;4:Doc17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 9. | Hu M, Zhao G, Wang F, Xu D, Liu R. Single-port and multi-port laparoscopic left lateral liver sectionectomy for treating benign liver diseases: a prospective, randomized, controlled study. World J Surg. 2014;38:2668-2673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Pan Y, Chen J, Chen J, Xu L, Zhou Z, Chen M, Zhang Y. Single-Port Laparoscopic Hepatectomy for Liver Tumor: Operative Steps (With Video). Surg Laparosc Endosc Percutan Tech. 2019;29:e98-e101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Tsai KY, Chen HA, Wang WY, Huang MT. Long-term and short-term surgical outcomes of single-incision laparoscopic hepatectomy on anterolateral liver segments. Surg Endosc. 2020;34:2969-2979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Broering DC, Elsheikh Y, Shagrani M, Abaalkhail F, Troisi RI. Pure Laparoscopic Living Donor Left Lateral Sectionectomy in Pediatric Transplantation: A Propensity Score Analysis on 220 Consecutive Patients. Liver Transpl. 2018;24:1019-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 948] [Cited by in RCA: 1407] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 15. | Gautier S, Monakhov A, Gallyamov E, Tsirulnikova O, Zagaynov E, Dzhanbekov T, Semash K, Khizroev K, Oleshkevich D, Chekletsova E. Laparoscopic left lateral section procurement in living liver donors: A single center propensity score-matched study. Clin Transplant. 2018;32:e13374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 16. | Hong SK, Tan MY, Worakitti L, Lee JM, Cho JH, Yi NJ, Lee KW, Suh KS. Pure Laparoscopic Versus Open Right Hepatectomy in Live Liver Donors: A Propensity Score-matched Analysis. Ann Surg. 2015;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |