Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6043
Peer-review started: June 30, 2020
First decision: September 29, 2020
Revised: October 19, 2020
Accepted: November 2, 2020
Article in press: November 2, 2020
Published online: December 6, 2020
Processing time: 157 Days and 1.2 Hours
Ureteral stent insertion is a relatively non-invasive procedure commonly used in the field of urology to resolve urinary obstruction. However, they are sometimes forgotten and the risk of complications increases with time.
A 43-year-old woman with a history of recurrent urinary tract infections visited our hospital for evaluation of persistent left flank pain, and lower urinary tract symptoms despite anti-biotic treatment. She had received urological surgery in her teens but did not know the details of her surgery. Kidney, ureter, and bladder X-ray and abdominopelvic computed tomography revealed a forgotten left ureteral stent with huge encrustation at both ends and a severely dilated left kidney with parenchymal thinning. In order to remove the ureteral stent, a laparoscopic nephroureterectomy was planned. The ureteral stent was successfully removed, and she was discharged after recovery. The patient was followed up for two years after surgery and did not show any signs of long-term complications.
Long indwelling stents can cause dire complications requiring radical interventions. Stent registry systems, novel stent material development, and proper patient education is important for complication prevention.
Core Tip: Ureteral stents are commonly used in urology and with appropriate care, it is considered a safe and easy procedure to manage ureter obstruction. However, due to multiple factors, its removal may be delayed which can result in stent calcification and infection. Even longer prolongation can lead to renal function decrease and parenchymal thinning from long-term obstruction which may require invasive procedures such as nephroureterectomy. Research on new stent material and specialized medical recordings dedicated to tracking stented patients are a few of the many ways that have been devised to prevent complications. Most importantly, thorough medical follow ups and detailed patient education is necessary in all cases to ensure the patients’ safety.
- Citation: Kim DS, Lee SH. Huge encrusted ureteral stent forgotten for over 25 years: A case report. World J Clin Cases 2020; 8(23): 6043-6047
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6043.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6043
Ureteral stents are commonly placed before or after urologic surgeries, such as pyeloplasty or ureteroureterostomy, and are especially indispensable in endourologic surgeries. They help establish and maintain ureteral patency, and aid in preventing ureteral injuries and post-operative strictures. However, ureteral stents can cause complications, such as stent encrustation, urinary tract infection, misplacement, and migration. They are sometimes even forgotten for a long time[1] and the risk of complications increases when the stent indwelling time is prolonged[2]. Many case reports have described and discussed the complications caused by forgotten ureteral stents, and endoscopic procedures are usually enough to remove the catheter[3]. However, only a handful of case reports have been published which described kidneys severely deteriorated by forgotten ureteral stents[4,5]. We present a case of a 43-year-old woman who presented with a left kidney that was non-functioning because of a severely encrusted ureteral stent that had been placed in her and forgotten for 25 years.
A 43-year-old female visited our hospital because of lower urinary tract symptoms and left flank pain.
She had experienced previous episodes of intermittent gross hematuria, dysuria, and urinary tenesmus. Whenever she had these symptoms, she visited a private clinic and was given oral antibiotics. Her symptoms usually improved after medication. Recently, her lower urinary tract symptoms had not improved despite treatment, and she came to our clinic for further evaluation and treatment.
A detailed review of her past medical history revealed that she had received urologic surgery when she was a teenager.
Her parents had passed away just after the surgery and the patient had no knowledge of what surgery was performed on her.
On admission her vital signs were normal, and she did not have fever. On physical examination she showed left costovertebral angle tenderness.
Her initial complete blood cell count and blood chemistry lab tests were normal. However, her urinalysis showed leukocytosis, and urine microscopy showed hematuria, pyuria, and bacteriuria.
A plain kidney, ureter, and bladder X-ray (Figure 1) and abdominopelvic computed tomography (CT) was taken for initial evaluation. On the kidney, ureter, and bladder X-ray and CT scans, a left ureteral stent with large calcifications at both the distal and proximal pigtail ends was detected. The CT scan also showed a severely dilated left kidney with parenchymal thinning, consistent with decreased renal function.
The final diagnosis of the patient was a non-functioning left kidney due to a forgotten severely calcified ureteral stent.
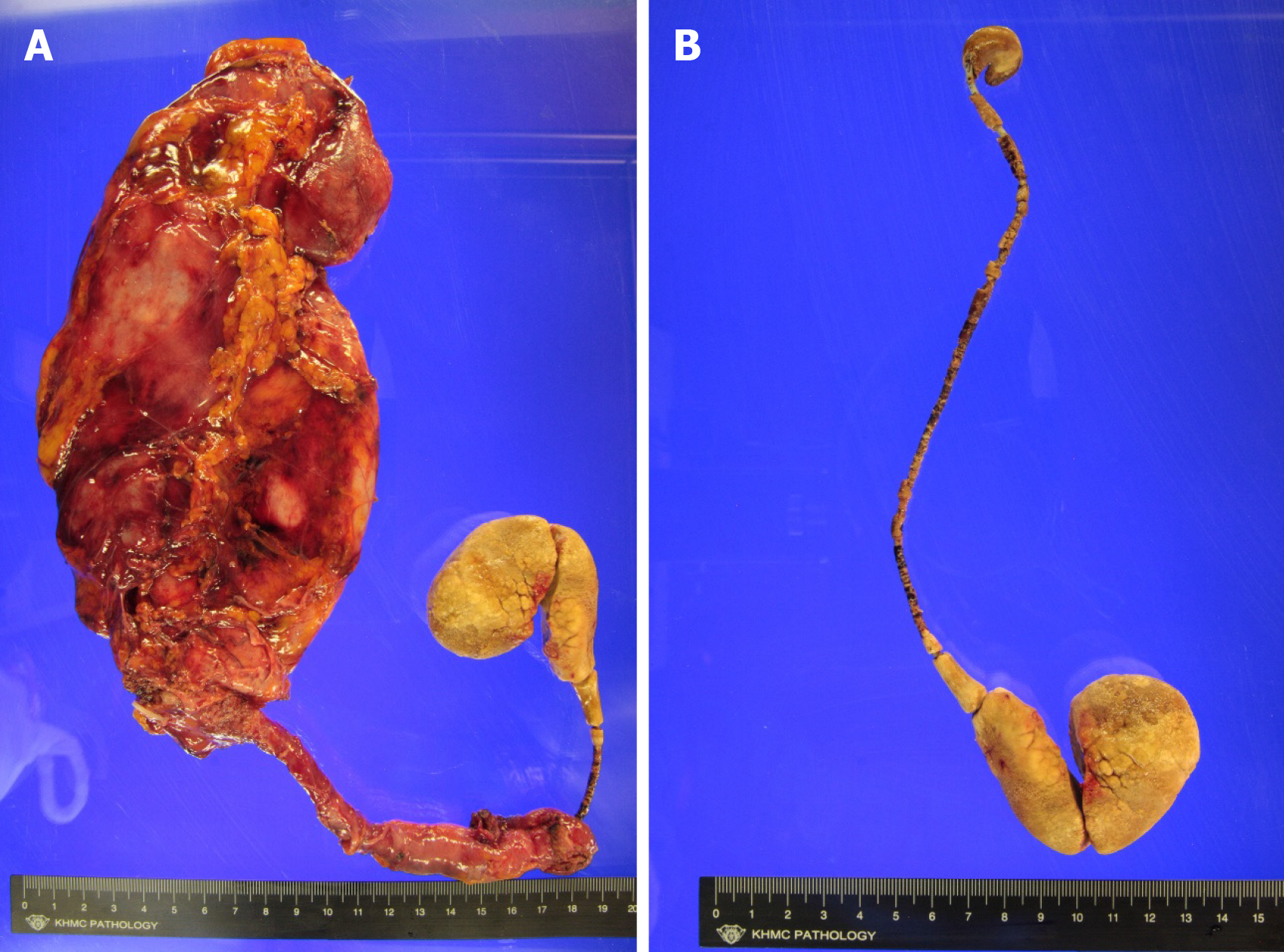
After consulting with the patient on her condition, we carried out a laparoscopic nephroureterectomy to remove the large, calcified ureter catheter and atrophied kidney (Figure 2).
She recovered from her surgery without complications and had no discomfort during the two-year follow-up.
Infection and encrustation of the ureteral catheters are the most common reasons for complications. For slight encrustation, stents can be simply removed using a cystoscope[6]. Larger encrustation may require multiple sessions and multiple modalities, such as extra-corporeal shock-wave lithotripsy, cystolitholapaxy, ureteroscopy, and percutaneous nephrolithotomy[7]. For more severe systemic situations, pretreatment with percutaneous nephrostomy with antibiotics may be needed for complicated urinary tract infections, and nephrectomy could be considered in patients with decreased renal function[2,4,5]. In our case, the patient had large encrustations of the ureteral catheter which had led to renal function deterioration, and laparoscopic nephroureterectomy was done to remove the non-functioning kidney and indwelling catheter.
The forgotten long-indwelling ureter catheter is a rare complication, because with proper patient education and appropriate planning, ureter stents will usually be removed or replaced within the recommended limit. However, as in our case, patients may forget of even be unaware of the presence of the stent and miss the opportunity to remove it. Considering the gravity of the consequences of missing a ureteral stent, many methods have been studied and developed for preventing such an error.
First, there have been many advances in ureter stent design and materials. Currently, polymers such as silicone and metals like nitinol (a nickel and titanium alloy) are commonly used as stent material because of their biocompatibility and effectiveness. Research on biodegradables such as chitosan, polyclycolic acid, and natural saccharides as candidates for ureteral stent materials is currently ongoing and will be able to prevent complications caused by long-term indwelling stents. However, more time will be needed for their use in the general population. Studies on stent coatings and stent design modifications also aim to decrease infection, encrustation, and pain[8].
Second, establishing a computerized electronic database to register stented patients will allow medical caretakers to keep track of those in need of management[9]. Many institutions keep logbooks or records of ureteral stent insertions in order to follow up on treated patients. However, no matter how dutiful the medical staff is, there is always room for clerical error or follow-up loss due to non-medical causes. Davis et al[9] compared the use of logbook tracking to a computerized registry with a “traffic-light” reminder about prolonged indwelling stents. They found that 4% of the patients registered in the logbook had prolonged stent insertions because of missed appointments or follow-ups at other clinics, but for the computerized registry group, all patients had their stents removed or changed within six months.
Third, patient education and direct reminders to alert them of their status will further help in preventing missed stents. Pre-stenting education about the risks and complications of stent insertion will help increase patients’ awareness of their status. Despite repeated counselling, some patients will still forget and be lost to future follow-ups. Withington et al[10] commented that they gave wrist bands to stented patients with a bar code that would serve as both a registry key and a visible reminder. Ziemba et al[11] describe using a mobile point-of-care application that can be accessed on mobile phones or through the internet. It allowed them to keep track of patients who had forgotten their scheduled visit for stent removal and to prevent further complications[11].
Forgotten stents are dangerous only if they are really forgotten by either the doctor or the patient. Education, along with dutiful planning by medical caregivers and backup with fail-proof automated systems, will help decrease the incidence of forgotten stents. Early retrieval of missed stents will prevent disastrous complications and lower the socio-economical burdens this rare complication imposes on the patients and the medical society.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng XW S-Editor: Zhang L L-Editor: A P-Editor: Li JH
| 1. | Sali GM, Joshi HB. Ureteric stents: Overview of current clinical applications and economic implications. Int J Urol. 2020;27:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Polat H, Yücel MÖ, Utangaç MM, Benlioğlu C, Gök A, Çift A, Kalyenci B, Lök U, Gülaçtı U. Management of Forgotten Ureteral Stents: Relationship Between Indwelling Time and Required Treatment Approaches. Balkan Med J. 2017;34:301-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Adanur S, Ozkaya F. Challenges in treatment and diagnosis of forgotten/encrusted double-J ureteral stents: the largest single-center experience. Ren Fail. 2016;38:920-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Bidnur S, Huynh M, Hoag N, Chew B. An Indwelling Ureteral Stent Forgotten for Over 12 Years. J Endourol Case Rep. 2016;2:135-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Barreiro DM, Losada JB, Montiel FC, Lafos N. Urinary Incontinence and Urosepsis due to Forgotten Ureteral Stent. Urol Case Rep. 2016;8:63-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Bostanci Y, Ozden E, Atac F, Yakupoglu YK, Yilmaz AF, Sarikaya S. Single session removal of forgotten encrusted ureteral stents: combined endourological approach. Urol Res. 2012;40:523-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Ulker V, Celik O. Endoscopic, Single-Session Management of Encrusted, Forgotten Ureteral Stents. Medicina (Kaunas). 2019;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 8. | Mosayyebi A, Manes C, Carugo D, Somani BK. Advances in Ureteral Stent Design and Materials. Curr Urol Rep. 2018;19:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 9. | Davis NF, Murray G, O'Connor T, Browne C, MacCraith E, Galvin D, Mulvin D, Quinlan D, Lennon G. Development and evaluation of a centralised computerised registry for ureteric stents: completing the audit cycle. Ir J Med Sci. 2017;186:1057-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Withington J, Wong K, Bultitude M, O'Brien T. The forgotten ureteric stent: what next? BJU Int. 2014;113:850-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Ziemba JB, Ludwig WW, Ruiz L, Carvalhal E, Matlaga BR. Preventing the Forgotten Ureteral Stent by Using a Mobile Point-of-Care Application. J Endourol. 2017;31:719-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |