Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.5902
Peer-review started: May 5, 2020
First decision: June 18, 2020
Revised: June 18, 2020
Accepted: September 23, 2020
Article in press: September 23, 2020
Published online: December 6, 2020
Processing time: 213 Days and 2.5 Hours
Focal intrahepatic strictures (FIHS) refer to local strictures of the small and medium intrahepatic bile ducts. FIHS are easily misdiagnosed due to their rare incidence, and few studies have focused on the diagnosis and treatment approaches.
To propose a new classification for FIHS in order to guide its diagnosis and treatment.
The symptoms, biochemistry results, imaging results, endoscopic examination results and initial and final diagnoses of 6 patients with FIHS admitted between January 2010 and December 2019 were retrospectively analyzed.
The 6 patients were diagnosed with intratubular growth-type intrahepatic cholangiocarcinoma (IG-ICC), recurrent multiple hepatocellular carcinoma (rmHCC) with bile duct tumor thrombus (BDTT), adenosquamous carcinoma (ASC), hepatolithiasis, small duct primary sclerosing cholangitis (SD-PSC) and autoimmune hepatitis (AIH). The initial and final diagnoses were not consistent in 4 patients. Hepatectomy was performed in patients with IG-ICC, ASC and hepatolithiasis according to the locations of their FIHS. Patients with rmHCC with BDTT received lenvatinib/sintilimab, while patients with SD-PSC and AIH received UDCA. We proposed the following classification system for FIHS: type I: FIHS located within one segment of the liver; type II: FIHS located at the confluence of the bile ducts of one segment or two adjacent segments; type III: FIHS connected to the left or right hepatic duct; and type IV: Multiple FIHS located in both lobes of the liver.
Our proposed classification system might help to guide the diagnosis and treatment of FIHS. Hepatectomy should be performed not only for malignant FIHS but also for benign strictures with severe secondary damage that cannot be improved by nonsurgical methods.
Core Tip: Focal intrahepatic strictures (FIHS) refer to local strictures of the small and medium intrahepatic bile ducts. FIHS are easily misdiagnosed due to their rare incidence, and few studies have focused on the diagnosis and treatment approaches. We proposed a new classification system to guide the diagnosis and treatment of FIHS. Hepatectomy should be performed not only for malignant FIHS but also for benign strictures with severe secondary damage that cannot be improved by nonsurgical methods.
- Citation: Zhou D, Zhang B, Zhang XY, Guan WB, Wang JD, Ma F. Focal intrahepatic strictures: A proposal classification based on diagnosis-treatment experience and systemic review. World J Clin Cases 2020; 8(23): 5902-5917
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/5902.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.5902
Focal intrahepatic strictures (FIHS) refer to local strictures or stenoses of the small and medium intrahepatic bile ducts caused by various factors, such as anatomical abnormalities, tumors, inflammation and trauma. The incidence rate of FIHS is extremely low without authoritative epidemiological data, and the number of admitted FIHS patients reported by only a few centers is < 5 annually[1-5].
FIHS are easily misdiagnosed or missed diagnosed due to the following reasons. First, when compared with extrahepatic or hilar bile strictures, FIHS usually only induce slight abdominal pain, rarely with jaundice and with occasional fever. It accounts for approximately 30%-40% of FIHS patients who go to see a doctor due to accidentally detected bile duct dilation or mildly abnormal liver function without obvious symptoms[1-4]. Second, the etiology of FIHS is complicated, and they are mainly categorized as benign or malignant strictures, of which the former accounts for 29% to 50% of cases[1]. The causes of benign FIHS include surgery or traumatic factors such as transcatheter arterial chemoembolization (TACE) and radiofrequency ablation (RFA), biliary inflammation, immune disease, cytotoxic injury, congenital development or anatomic abnormalities, pathogen infections (C. sinensis, tuberculosis, etc.) and benign tumors[3-8]. Malignant FIHS is also caused by various primary diseases, including peritubular infiltrating-type intrahepatic cholangiocarcinoma (PI-ICC), intratubular growth-type intrahepatic cholangiocarcinoma (IG-ICC), hepatocellular carcinoma (HCC) with bile duct tumor thrombus (BDTT) and metastatic cancer invading the intrahepatic system. Notably, it should be noted that special types or subtypes of some common diseases can also cause FIHS. For example, primary sclerosing cholangitis (PSC) generally involves the large bile duct; however, approximately 6%-16% of patients are categorized as having small duct primary sclerosing cholangitis (SD-PSC), in which the lesion mainly involves the small intrahepatic duct[9]. Similarly, localized intrahepatic IgG4-related sclerosing cholangitis (LIH-IgG4-SC, or type V IgG4-SC) is another rare etiological factor of FIHS[10]. Finally, because FIHS only has limited systemic effects and hepatobiliary damage in its early stage, current data have shown that liver function tests, tumor markers such as CA199 as well as routine computed tomography (CT magnetic resonance imaging (MRI), positron emission tomography (PET) imaging and endoscopic examinations almost do not have enough sensitivity or specificity to evaluate the localization and nature of the lesion[4,11,12].
Unlike in other common hepatobiliary diseases, the precise diagnosis of FIHS is sometimes difficult until surgery is performed. Therefore, surgeons themselves should answer the following four questions before initiating treatment for FIHS: (1) What are the indications for surgical intervention? (2) What is the optimal timing of treatment? (3) Which procedure is the best choice? And (4) What is the purpose or expected effect of treatment: Radical cure, diagnostic therapy, postponing development or improving symptoms? In the present retrospective study, we reviewed our diagnosis and treatment experience of 6 FIHS patients, including the misdiagnosed cases. We also proposed a classification system for FIHS attempting to clarify the diagnosis-treatment strategies according to its pathological characteristics, anatomical location and varying degrees of damage to the hepatobiliary system.
Six patients diagnosed with FIHS were admitted to our center between January 2010 and December 2019 (Table 1). Among them, three had complaints of mild abdominal pain, and only one had visible jaundice. One patient with a history of multiple recurrent HCC went to see the doctor due to his increasing level of AFP > 700 ng/mL and peripheral intrahepatic bile duct dilation detected by multidetector-row computed tomography (MDCT). Three patients received hepatectomy for treating adenosquamous carcinoma (ASC), ICC and hepatolithiasis. The remaining 2 patients were diagnosed with small duct primary sclerosing cholangitis (SD-PSC) and autoimmune hepatitis (AIH).
| No. | Sex | Age | Main symptoms | Bilirubin and ALP before treatment for FIHS | CA199 (ng/mL) | AFP (ng/mL) | History of surgery | Methods for initial diagnosis | Initial diagnosis | Final diagnosis | Location of FIHS | Treatment for FIHS | ||
| Abdominal pain | Fever | T-bil/D-bil (μmol/L) | ALP (U/L) | |||||||||||
| 1 | F | 65 | Mild | - | 16.1/0.0 | 0.0 | 20.55 | 8.99 | No | MDCT | Suspected ICC | ICC | LLIHD | Left lateral hepatectomy |
| 2 | M | 70 | - | - | 16.7/6.2 | 6.2 | 13.4 | 737.00 | Yes1 | MDCTMRCP | rHCC with BDTT/PVTTLung metastasis | rHCC with BDTT/PVTTLung metastasis | LLIHD | Lenvatinib + Sintilizumab |
| 3 | F | 60 | Mild | - | 16.8/8.6 | 8.6 | 2270.0 | 1.61 | No | MDCTMRCP | HepatolithiasisSuspected ICC | ASC of liver | LIHD | Left hepatectomy |
| 4 | F | 67 | Mild | - | 15.0/0.0 | 0.0 | 93.9 | 2.91 | No | USMDCTMRCPERCPSpyglass | Suspected ICC | Hepatolithiasis | LIHD | Left hepatectomy |
| 5 | F | 49 | - | - | 21.6/10.4 | 614.0 | 11.83 | 0.90 | No | MRCP | Hepatitis | SD-PSC(biopsy) | Multiple IHD | UDCA |
| 6 | F | 55 | - | - | 283.5/150.0 | 279.0 | 770.0 | 23.8 | No | MDCTMRCPERCP | Suspected PSC | AIH(biopsy) | Multiple IHD | UDCA + MP |
The study was performed in accordance with the declaration of Helsinki. Ethical approval for the present study was granted by XinHua Hospital affiliated to Shanghai Jiao Tong University, School of Medicine (Shanghai, China). The study was strictly in accordance with the Declaration of Helsinki and International Ethical Guidelines for Health-related Research Involving Humans. All the included patients signed an informed consent form. A multidisciplinary team made up of hepatobiliary surgeons, radiologists, oncologists, gastroenterologists and pathologists selected candidates for the treatment together.
All the patients received serum tumor marker tests (AFP, CEA, CA199, CA242, CA153, CA724 and CA50) and imaging examinations, including abdominal computed tomography (CT) scans or magnetic resonance cholangiopancreatography (MRCP). Both the images and diagnostic reports were reviewed by two experienced radiologists independently. Endoscopic retrograde cholangiopancreatography (ERCP) with the SpyGlass system was used to confirm or exclude cholangiolithiasis and cholangiocarcinoma. Specimens of the liver were obtained through ultrasound-guided needle biopsy or surgery. Similar to the process of imaging diagnosis, pathological reports were also completed and checked by two pathologists. This study was approved by the Institutional Review Board of Xinhua Hospital affiliated with Shanghai Jiaotong University, School of Medicine.
The patients were requested to be re-examined at outpatient visits every 1-2 mo after discharge. Routine physical as well as imaging examinations, full blood counts, and tests for liver function and tumor markers were performed for each patient. For patients diagnosed with AIH and PSC, detection of immunological indexes including antinuclear antibody (ANA), proliferating cell nuclear antigen (PCNA), double-stranded DNA (dsDNA), anti-Ro, nucleosome, IgG, IgA, IgM and IgE was also conducted. All of the living patients were followed until December 2019.
A literature search was performed using databases including PubMed, Embase, Ovid and Web of Science by two researchers independently. The relevant studies published from January 1980 until January 2020 were searched and gathered by the following terms: (Focal intrahepatic stricture OR FIHS OR local intrahepatic stricture OR intrahepatic bile duct stricture OR local intrahepatic stenosis OR intrahepatic bile duct stenosis OR local intrahepatic stenosis). Inclusion criteria: (1) Patients diagnosed as HCC with BDTT based on pathology or typical imaging findings; and (2) Patients with well-defined outcomes including total hospital stay and follow-up results of survival related data. Exclusion criteria: (1) Patients diagnosed as extrahepatic bile duct strictures and extensive strictures of the biliary system; (2) Patients did not have well-defined outcomes or follow-up results; and (3) Papers published in languages other than English.
The patients in the present study included 5 men and 1 woman who ranged in age from 49 to 70 years old. The clinicopathological characteristics of the patients are summarized in Table 1. The initial diagnoses were achieved based on the imaging manifestations and blood biochemistry results (Table 2).
| No. | Method of examination | Characteristics of FIHS lesion | Characteristics of secondary changes | |||||||
| Location of FIHS | Enhancement of FIHS lesion in different phases | Imaging diagnosis | Hepatatrophia | Intrahepatic bile duct dilation | Hepatolithiasis | |||||
| Plain | Arterial | Portal | Delayed | |||||||
| 1 | MDCT | Not clear | - | - | faint | faint | Left hepatic lobe atrophy, LIHD dilation, Suspected ICC | + | B2, B3 | - |
| 2 | MDCT | Confluence of B2/B3 | - | + | - | - | rHCC with BDTT/PVTT | - | B2, B3 | - |
| MRCP | - | + | - | - | - | B2, B3 | - | |||
| 3 | MDCT | Confluence of B2/B3/B4 | - | - | - | - | Hepatolithiasis, Suspected ICC | - | B2, B3, B4 | + |
| MRCP | - | - | - | - | - | B2, B3, B4 | + | |||
| 4 | US | Not clear | N/A | N/A | N/A | N/A | High-echo lesion in S4 | - | LIHD | - |
| MDCT | Not clear | - | - | - | - | LIHD dilation | - | LIHD | - | |
| MRCP | Not clear | - | - | - | - | High T2 signal in S4LIHD dilation, Suspected ICC | - | LIHD | - | |
| ERCP+Spyglass | Not clear | N/A | N/A | N/A | N/A | Acute cholangitis | N/A | Not clear | - | |
| IOUS, Choledochoscopy | Confluence of B2/B3/B4 | N/A | N/A | N/A | N/A | Acute cholangitis, Hepatolithiasis | - | B2, B3, B4 | + | |
| 5 | MRCP | Multiple small IHD | - | - | - | - | Hepatitis | - | - | - |
| 6 | MDCT | Multiple small IHD | - | - | - | - | Acute cholangitis | - | - | - |
| MRCP | - | - | - | - | Acute cholangitis, Suspected PSC | - | - | - | ||
| ERCP | N/A | N/A | N/A | N/A | PSC | N/A | - | - | ||
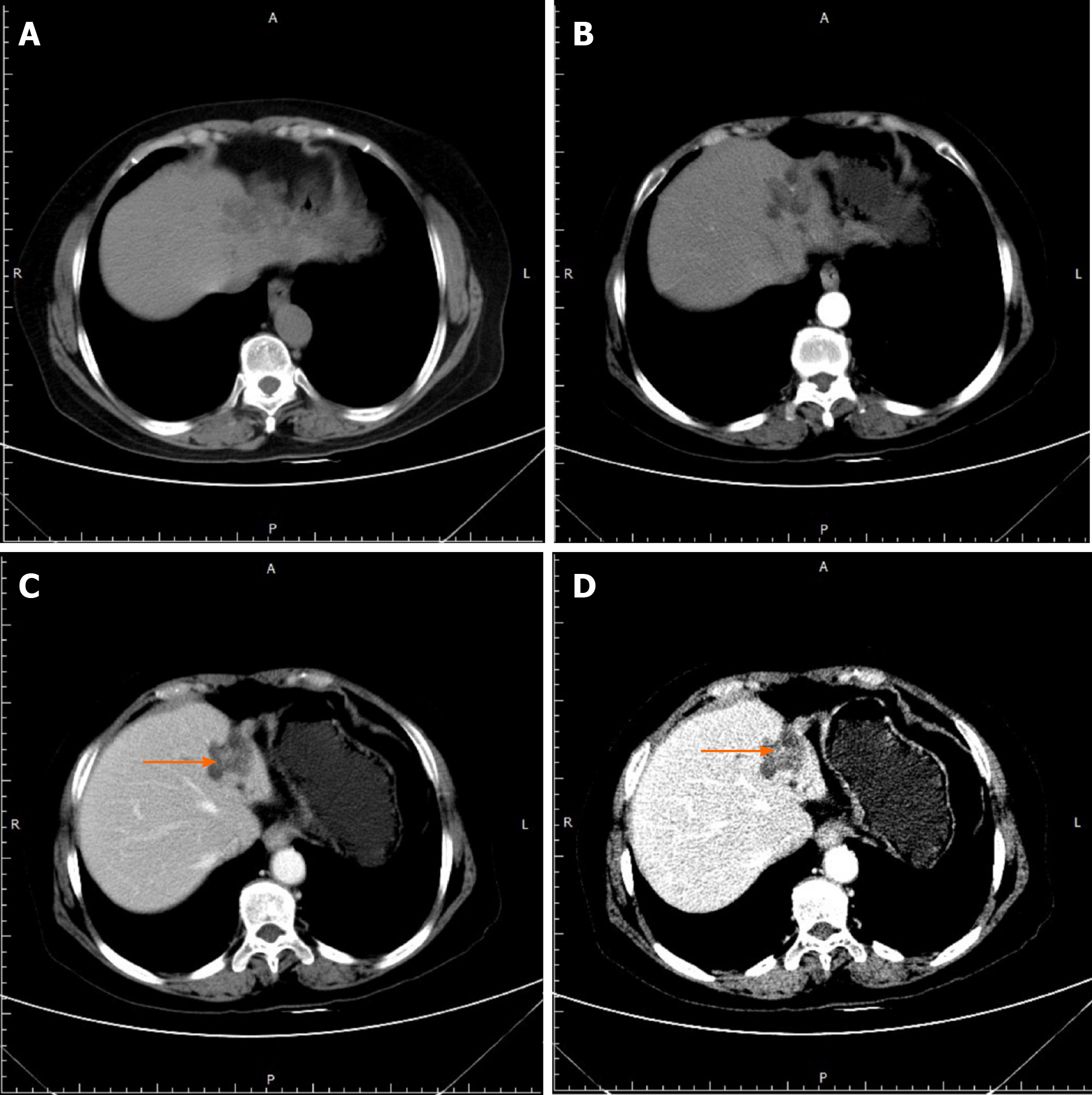
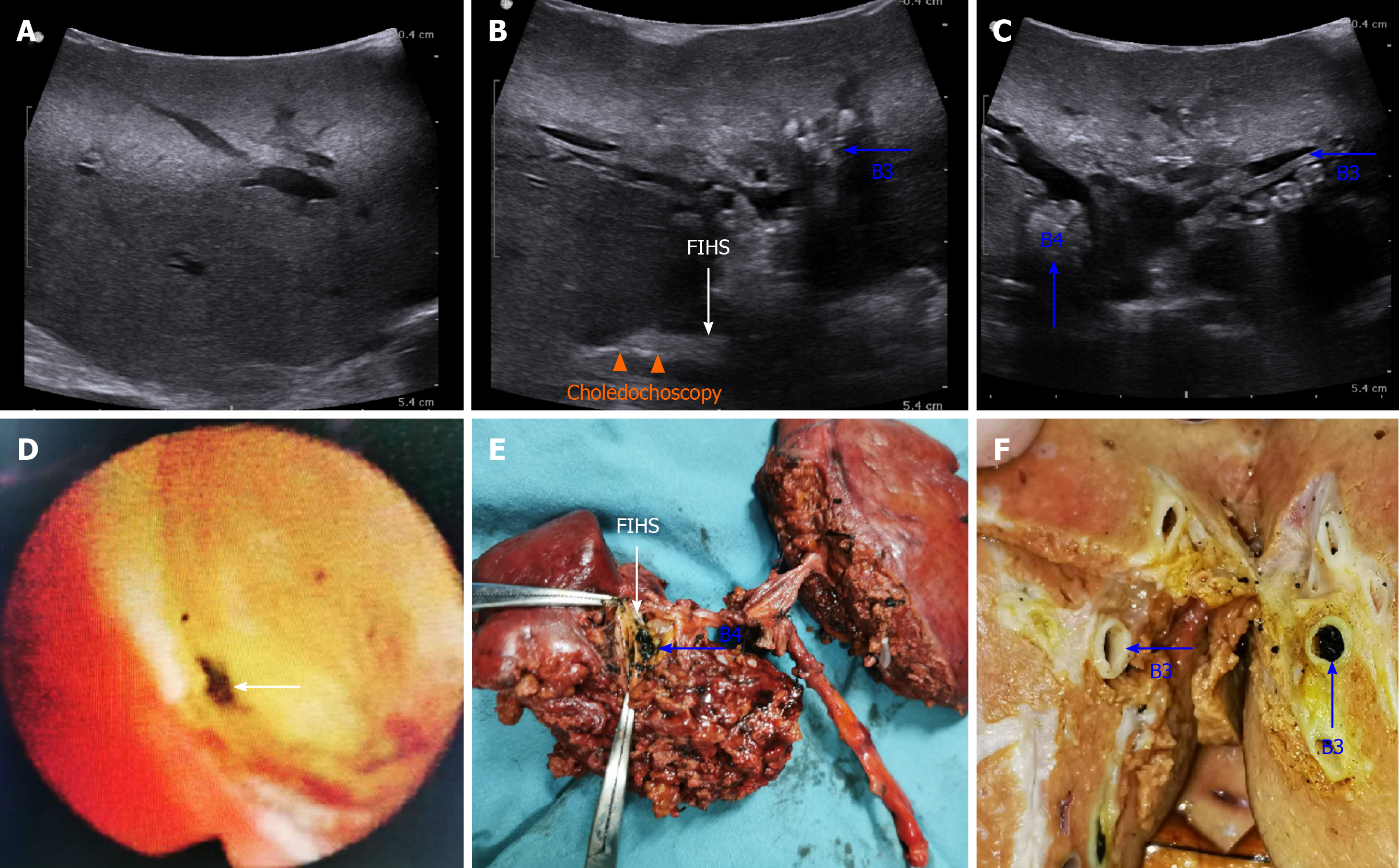
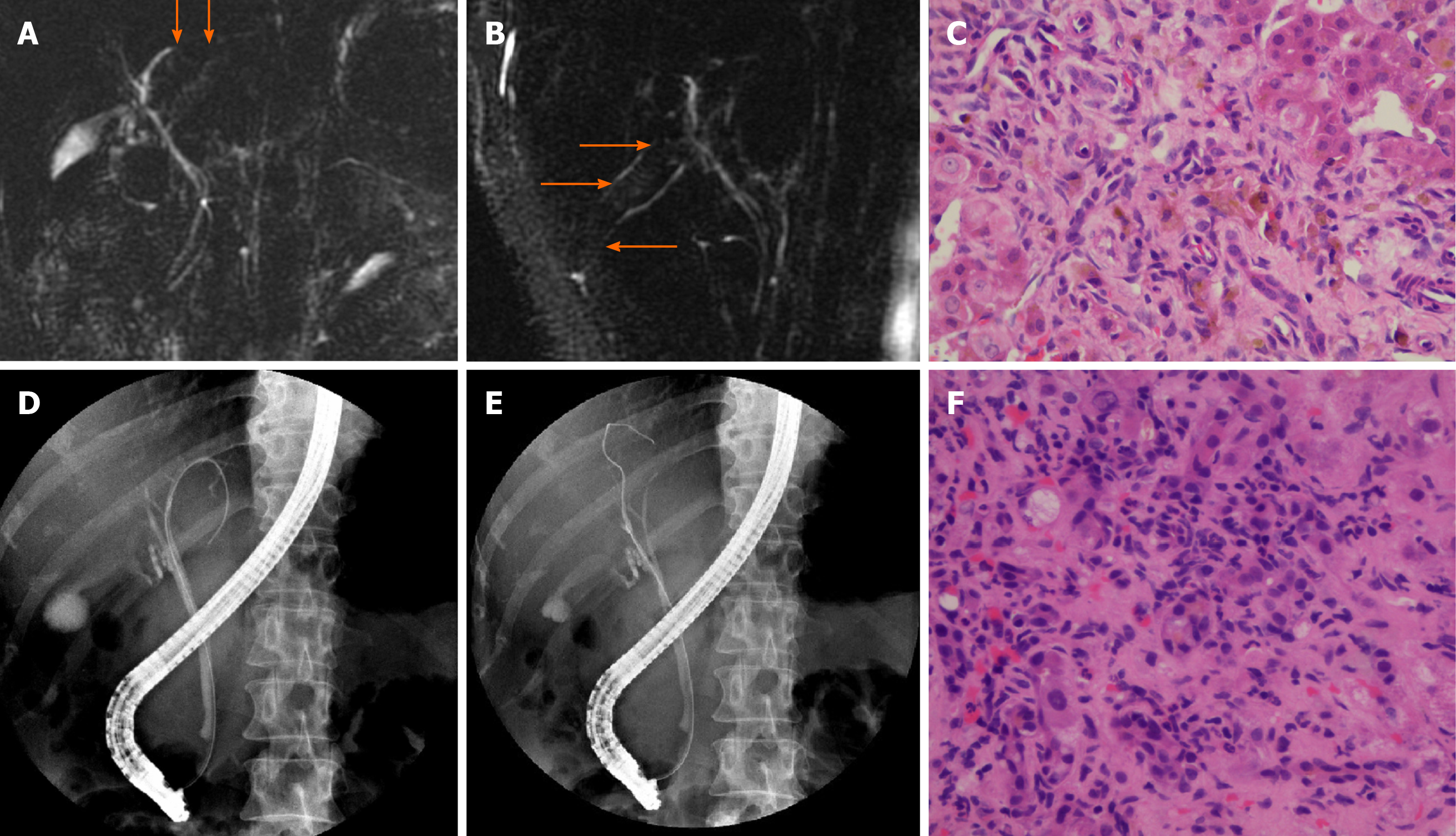
Notably, only 2 patients (No. 1# and 2#) who were initially diagnosed with ICC and recurrent HCC, respectively, maintained consistency with their final diagnoses. Patient No. 1# came to the local clinic to identify the reason for her mild abdominal pain. The results of liver function and tumor marker tests were all normal. Because of the extremely atrophied left lateral lobe and dilated left intrahepatic bile ducts of segment II/III (B2/B3) with a 0.8 cm faintly enhanced nodular lesion detected by MDCT, she received left lateral hepatectomy, and a preoperative diagnosis of suspected intratubular growth-type ICC was finally confirmed by pathology (Figure 1). Patient No. 2# was clinically diagnosed with HCC with BDTT. He had a history of two operations for the first appearance of recurrent HCC. The serum AFP level increased to over 700 ng/mL and dilated bile ducts of segment II/III (B2/B3) were observed, wherein enhanced punctate lesions could be detected in the arterial phase of the MDCT images (Figure 2).
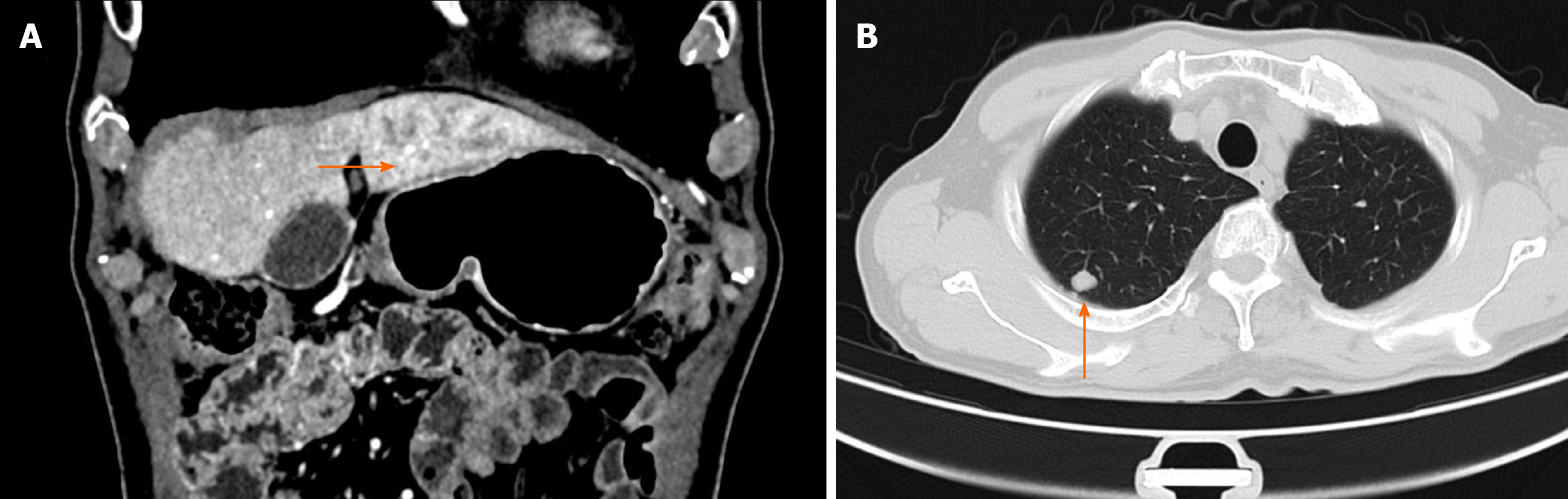
Corrections of the initial diagnoses occurred in the remaining 4 patients (patient No. 3#, 4#, 5#, and 6#). Patient No. 3# was a 39-year-old female with a complaint of mild abdominal pain, a nearly normal serum bilirubin level and an obviously elevated CA199 level (2270 ng/mL). MDCT and MRCP both showed filled stones in dilated B2/B3/B4 with thickened bile duct walls forming a massive lesion in the left lobe (Figure 3). The imaging diagnosis was hepatolithiasis and suspected ICC. However, the “massive lesion” as well as the strictured part of the bile duct were finally confirmed as ASC by pathology after surgery (Table 3).
| No. | Pathological characteristics of FIHS and related lesions | |||||||||
| Location of dilated bile duct | Macroscopic | Microscopic | ||||||||
| Location of FIHS | Features of related lesions | Structure | Pathological diagnosis | Differentiation of malignant FIHS | Surgical margin | |||||
| Location of related lesions | Size (cm) | Color | Texture | |||||||
| 1 | B2, B3 | Confluence of B2/B3 | ICC: left lateral lobe | ICC: 0.8 | Grey white | Jellylike | Tubulo-villous | Peritubular infiltrating type ICC; Partial mucinous adenocarcinoma | Moderate | - |
| 2 | - | - | - | - | - | - | - | - | - | - |
| 3 | B2, B3, B4 | Confluence of B2/B3/B4 | ASC: left lobe | ASC: 6.0 (Dilated bile ducts) | Grey white | Hard | Irregular nests of polygonal cells; intercellular bridges | ASC of liver; Hepatolithiasis | Moderate | - |
| 4 | B2, B3, B4 | Confluence of B2/B3/B4 | Hepatolithiasis: B2, B3, B4 | Stones: 0.1-0.2 | black brown | Hard | Lymphocytes, plasma cells, macrophages infiltration; Fibrosis | Cholangitis; Hepatolithiasis | N/A | N/A |
| 5 | - | - | - | - | - | - | Portal inflammation with edema, Fibrosis and proliferation | SD-PSC | N/A | N/A |
| 6 | - | - | - | - | - | - | Cloudy swelling of liver cells; cholestasis; inflammatory cell infiltration; proliferation of small bile ducts | AIH | N/A | N/A |
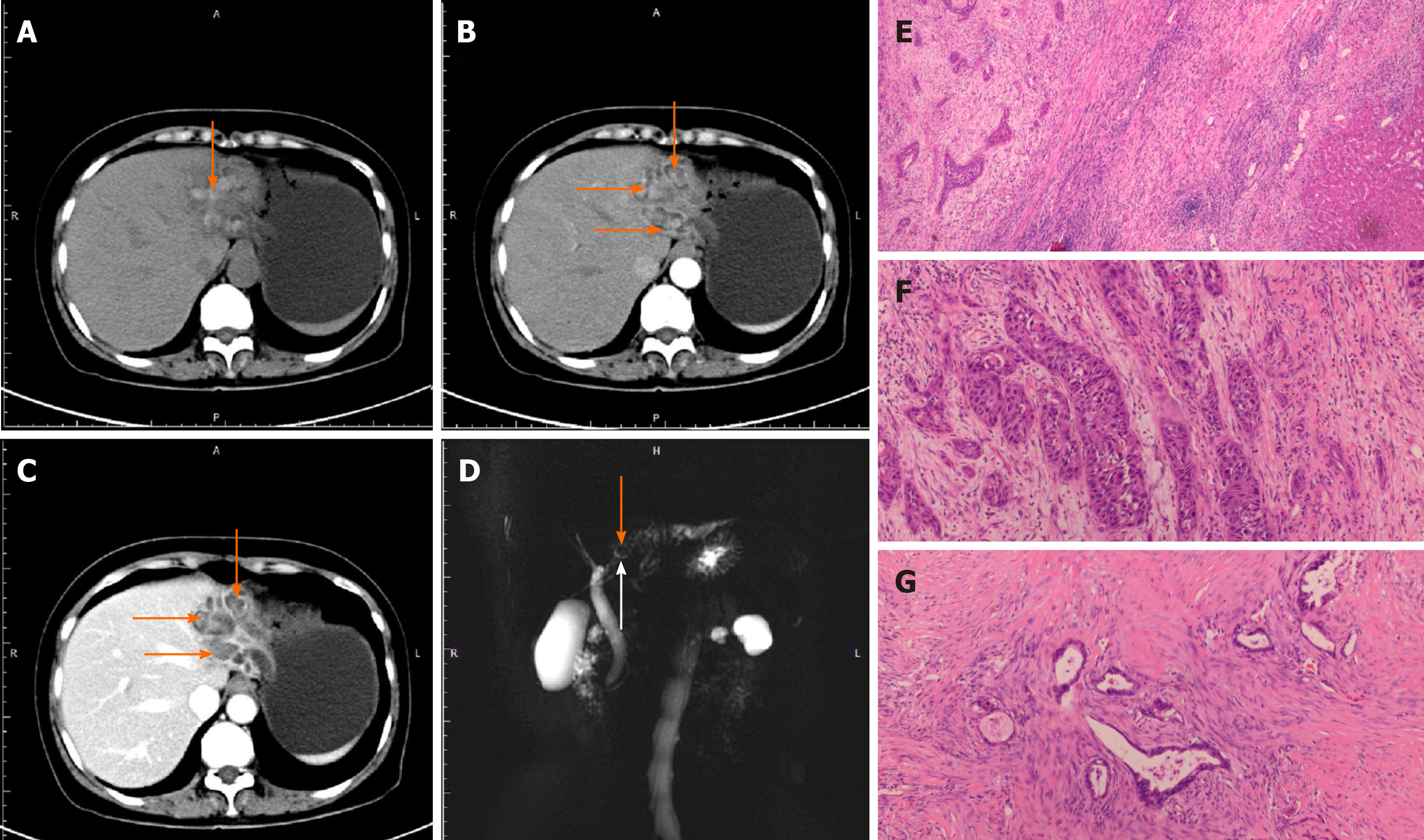
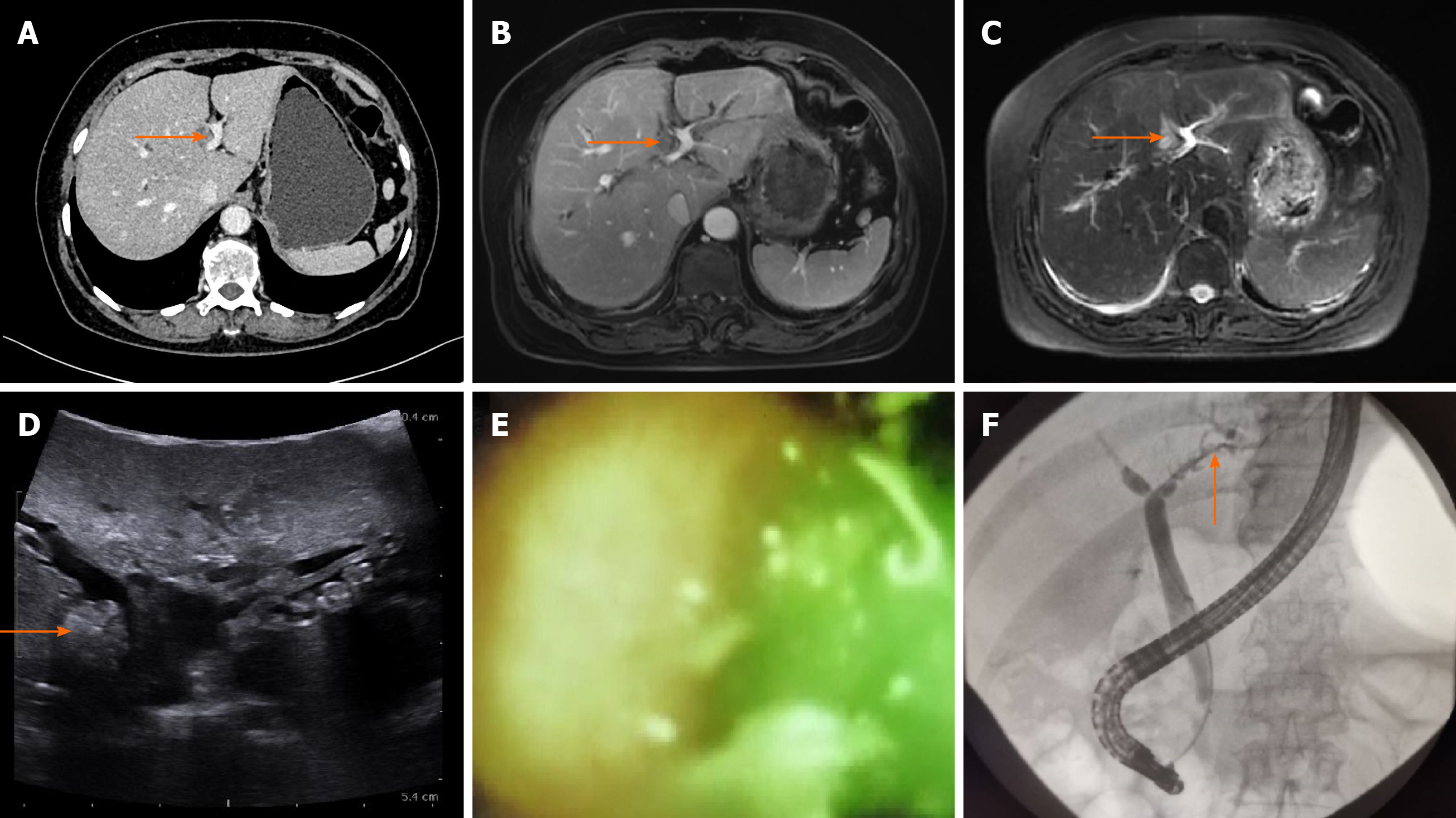
The causes of benign FIHS in three patients (No. 4#, 5#, and 6#) were also not definitely clarified until surgery or biopsy had been performed. Patient No. 4# with obesity was admitted to our department due to manifestations of mild cholangitis and a moderately elevated CA199 level (93.9 ng/mL). MDCT revealed obvious biliary dilation in the left lobe (B2/B3/B4), while an additional 1.0 cm × 1.0 cm mass-like lesion located in segment IV (B4) was detected as a high signal intensity on T2-weighted MRI/MRCP images and high echo on ultrasound (Figure 4A-D). Although ERCP combined with SpyGlass was performed, we could not clarify the abovementioned mass-like lesion because endoscopy was not able to reach confluence between the left hepatic duct (LHD) and peripheral intrahepatic bile ducts (Figure 4E). Endoscopic nasobiliary drainage (ENBD) of the LHD was conducted, but neither symptoms nor liver function was improved. On account of the test results described above, a diagnosis of suspected ICC originating from the background of intrahepatic cholangitis was considered first. Unexpectedly, during the operation, intraoperative ultrasonography (IOUS) and choledochoscopy suggested extensive biliary inflammation with multiple left intrahepatic lithiasis (Figure 5). It was pathologically confirmed as benign stenosis, which was unascertainable in the preoperative examinations (Table 3).
For patients No. 5# and 6#, their MRCP or ERCP images both showed signs of multiple local biliary strictures distributed in two lobes without abnormal filling defects or stenoses in the hilar or extrahepatic bile ducts (Figure 6). We detected that various serum antibodies and ANAs were positive for both patients at titers of 1:40 and 1:80 as well as 1:40, 1:80, 1:160, and 1:320, respectively. Their FIHS were initially diagnosed as hepatitis and PSC but finally corrected to SD-PSC and AIH, respectively, by pathology after biopsy (Table 3).
In the present study, the initial localization diagnoses of FIHS were achieved according to the patients’ imaging manifestations and were finally confirmed through intraoperative exploration or pathology. The multiple suspected strictures of patient No. 5# and 6# were detected directly based on CT/MRI or ERCP (Figure 6), whereas for the remaining 4 patients, the locations of FIHS were roughly judged by their secondary changes, such as dilated bile ducts (Patient No. 1#, 2#, 3#, and 4#), intrahepatic lithiasis (patient No. 3# and 4#), tumor lesion (Patient No. 1# and 2#) and hepatic lobe atrophy (Patient No. 1# and 3#). For example, the FIHS of patient No. 3 and No. 4# were both located between the confluence part of the LHD and its peripheral dilated bile ducts (B2/B3/B4) (Figures 3 and 4). It was noted that for patient No. 4#, the initial part of the FIHS was directly observed intraductally by choledochoscopy while at the same time was positioned through the surface of the liver parenchyma by IOUS during the operation (Figure 5B-F).
According to the location of FIHS and related lesions, left lateral hepatectomy was performed for patient No. 1# with ICC, and left lobotomy was performed for patient No. 3# with ASC and No. 4# with hepatolithiasis. The two patients (No. 1# and No. 3) with malignant FIHS died 18 and 12 mo after surgery, respectively, due to systemic metastasis and recurrence. Lenvatinib + sintilimab was utilized as adjuvant therapy for patient No. 2# with recurrent HCC and BDTT, and his AFP level decreased to 59.8 ng/ml at the time of the last follow-up in December 2019. For patient No. 5# (SD-PSC) and No. 6# (AIH), UDCA was given to alleviate their autoimmune damage, and both patients were still alive.
There were 17 studies which described the natural courses, causes, characteristics, factors, etiologies, pathologies and mechanisms of FIHS in detail (Table 4 and Supplementary Figure 1). The most common cause of FIHS was hepatolithiasis with biliary infection[5]. The incidence rates of FIHS varied significantly between 0.3% and 70.6% among different causes and diseases[3-20]. Parasites, SD-PSC, LIH-IgG4-SC, follicular cholangitis, IBPMC, ASC of the liver and thrombus of colorectal liver metastasis (CLM) were also reported to be rare etiologies of FIHS[6,9,10,14,17,19,20].
| Nature of FIHS | Causes and factors | Etiology | Pathology and mechanisms | Incidence rate |
| Benign | Surgery and trauma | Hepatobiliary surgery | Physical injury of bile duct and hepatic artery; Ischemia of bile duct | Unknown |
| TACE | Chemical injury;Ischemia of bile duct | 0.3%[3] | ||
| RFA | Heat damage; Ischemia of bile duct | 17%[4] | ||
| Chronic inflammation | Hepatolithiasis/Bacterial infection | Inflammatory response; Mechanical obstruction | 70.6%[5] | |
| Parasite | Inflammatory response; Mechanical obstruction | Case report[6] | ||
| Mycobacterium tuberculosis | Secondary cholangitis and granuloma | 16.7%[7] | ||
| HIV cholangiopathy | Inflammatory and immune response caused by cryptosporidium and cytomegalovirus; Ischemia of bile duct caused by injury of hepatic artery | 15%-20%[8] | ||
| SD-PSC | Autoimmune response; Bile duct fibrosis | Case report[9] | ||
| LIH-IgG4-SC | Autoimmune response; Bile duct fibrosis | Case report[10] | ||
| Autoimmune pancreatitis | Autoimmune response; Bile duct fibrosis | 24.3%[13] | ||
| Follicular cholangitis | Dense fibrosis of muscularis mucosae with follicular hyperplasia | Case report[14] | ||
| Congenital diseases | Caroli's disease | Hepatic fibrosis; Secondary bile duct sclerosis | 13%-80%[15,16] | |
| Benign tumor | IBPMC | Intraductal growth and mechanical obstruction | Case report[17] | |
| Malignant | Primary malignant tumor | Peritubular infiltrating type of ICC | Periductal infiltration and mechanical obstruction | 50%-53%[11,18] |
| Intratubular growth type of ICC | Intraductal growth and mechanical obstruction | |||
| HCC | Tumor thrombus | 11.8%[11] | ||
| ASC of liver | Chronic cholangitis and mechanical obstruction | Case report[19] | ||
| Metastatic malignancy | Metastatic hepatic carcinoma | Intraductal biliary metastasis and mechanical obstruction | Case report[20] |
In the present study, we reported the clinical courses of 6 patients with FIHS caused by ICC, recurrent HCC with BDTT, ASC of the liver, hepatolithiasis, SD-PSC and AIH. From our experience, the accurate localization and qualitative diagnosis of FIHS are often difficult to make because of the complicated etiology, rare incidence rate, limited lesion range and obscure symptoms.
Pathologically, FIHS mainly occurs in the left lateral or right posterior lobe of the liver. The pathological manifestations of FIHS can be categorized into two patterns: Chronic inflammation and tumors. Notably, a large portion of malignancies originate based on the background of chronic inflammation; thus, the two patterns actually coexist in many FIHS patients. Hyperplasia, fibrosis and inflammatory cell infiltration of the bile duct mucosa accompanied by peripheral biliary dilation, segmental atrophy of the liver and hepatolithiasis are typical chronic inflammatory changes in FIHS. On this basis, some special types of biliary tract inflammatory diseases have their own microscopic pathological features, which helps to achieve differential diagnosis. For example, LIH-IgG4-SC and SD-PSC both have the general morphology of “onion skin-like fibrosis” of the bile duct, but the former is characterized by massive IgG4-positive plasma cell infiltration, while the latter is characterized by detectable anti-neutrophil cytoplasmic antibodies (ANCAs)[10,11]. PI-ICC and IG-ICC are the most common primary biliary malignancies that result in FIHS[11,18]. PI-ICC usually infiltrates the blood vessels and connective tissue, leading to narrowing of the bile duct cavity, while IG-ICC mainly grows intraductally as a granular, papillary lesion and forms a thrombus. HCC and metastatic liver tumors can also cause FIHS in the form of BDTT through direct invasion into the biliary system or via the microvasculature, lymphatic vessels or plexus around the bile duct. The locations of FIHS might not be adjacent to their primary or main lesions when cancer cells metastasize via the latter two pathways[14-18]. In our study, primary ASC of the liver was also found to be the cause of FIHS. ASC is a rare malignancy of the liver that contains the cellular components of both adenocarcinoma and squamous cell carcinoma. ASC might occur based on biliary chronic inflammation or choledochocysts[19].
The existing diagnostic methods for detecting FIHS include blood tests (liver function, tumor markers), imaging tests (ultrasound, CT, MRI/MRCP, PET), endoscopy (ERCP, PTCS) and pathological biopsy (aspiration tissue sampling, cell brush, tissue biopsy). However, the sensitivity and specificity of the above methods for differential detection still need to be improved. When compared with other liver function indexes almost within the normal range, in approximately 65% of FIHS patients, values of alkaline phosphatase (ALP) and γ-glutamyl transpeptidase (GGT) might increase to different degrees. Kim et al[4] suggested that an ALP value > 200 U/L could be used as an indicator of malignant FIHS, but its specificity was not proven by large-scale investigations. A similar situation was observed for CA199, where it had no value for distinguishing FIHS caused by ICC[11]. The serum level of CA199 is much more likely to be affected by acute or chronic cholangitis and biliary obstruction as well as hyperplasia than the differences between benign and malignant FIHS. CA199 can serve as an objective criterion for the follow-up of biliary drainage efficiency, and its indicative function for malignant FIHS might be effective on the premise that strictures have been fully relieved.
To date, routine imaging examinations such as ultrasound, CT and MRI have not had sufficient sensitivity and specificity required for diagnosing FIHS. Even so, careful analysis of the secondary changes caused by FIHS is still important for its localization and qualitative diagnosis. Taking intratubular growth-type ICC as an example, Chung et al[21] summarized its 5 types of imaging manifestations as follows: (1) Diffuse bile duct dilatation with visible tumor lesions; (2) Diffuse bile duct dilatation without obvious tumors; (3) Limited bile duct dilatation with polyp-like tumor lesions; (4) Mild bile duct dilatation with suspected tumor lesions; and (5) Focal stenosis with mild proximal bile duct dilatation without visible tumor lesions. Signs including a dilated bile duct, hepatolithiasis, enhanced tumor-like lesions and an atrophied hepatic lobe might contribute to the localization of FIHS but have limited value in evaluating the accurate length and range of strictures. It has been shown that the sensitivity and specificity of positron emission tomography (PET) for detecting mass-type ICC > 1 cm both approach 100%. However, it is not a reliable technique for diagnosing PI-ICC and IG-ICC due to its high rate of false-negative results[22].
In recent years, ERCP combined with the SpyGlass system and percutaneous transhepatic cholangioscopy (PTCS) have been gradually used for the pathological diagnosis of FIHS. Ramchandani et al[23] reported their experience of achieving intrahepatic bile duct mucosa biopsy diagnosis in 4 cases of FIHS by SpyGlass. Seo et al[11] successfully differentiated benign and malignant FIHS lesions in 17 patients by biopsy via PTCS and indicated the diagnostic efficacy of FIHS caused by early ICC without jaundice. When comparing the above two methods, SpyGlass is less invasive and can avoid the complications such as intrahepatic tumor spread along the percutaneous catheter drainage tube associated with PTCD. However, SpyGlass often fails to detect FIHS lesions deep in the center of the segment of the liver because the optical fiber is too weak to adapt to the complex angles and directions of the peripheral intrahepatic bile duct. In patients with FIHS far from the hilar bile duct, PTCS might have advantages over ERCP in terms of the pathological diagnosis.
At present, aspiration, brush cytology and biopsy are the three main methods for obtaining preoperative pathology for biliary malignancy. For malignant strictures associated with CBD or near porta hepatis, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for aspiration are 47.8%-56.4%, 93.9%-100%, 91.7%-100% and 17.0%-64.6%, respectively. Brush cytology can be performed by moving metal brushes back and forth for 10 to 20 times at stricture sections of the biliary tract to collect tumor cell samples. The sensitivity, specificity, PPV, and NPV of Brush cytology are 33%-60%, 53%-100%, 94.7%-100% and 27.0%-66.1%, respectively. For biopsy, the specificity approaches 100%, and the biopsy forceps attached to SpyGlass have a significantly higher sensitivity of 76.5% than general forceps (29.4%)[24,25]. Unfortunately, there has been little evidence supporting the efficacy of the diagnostic techniques described above for FIHS.
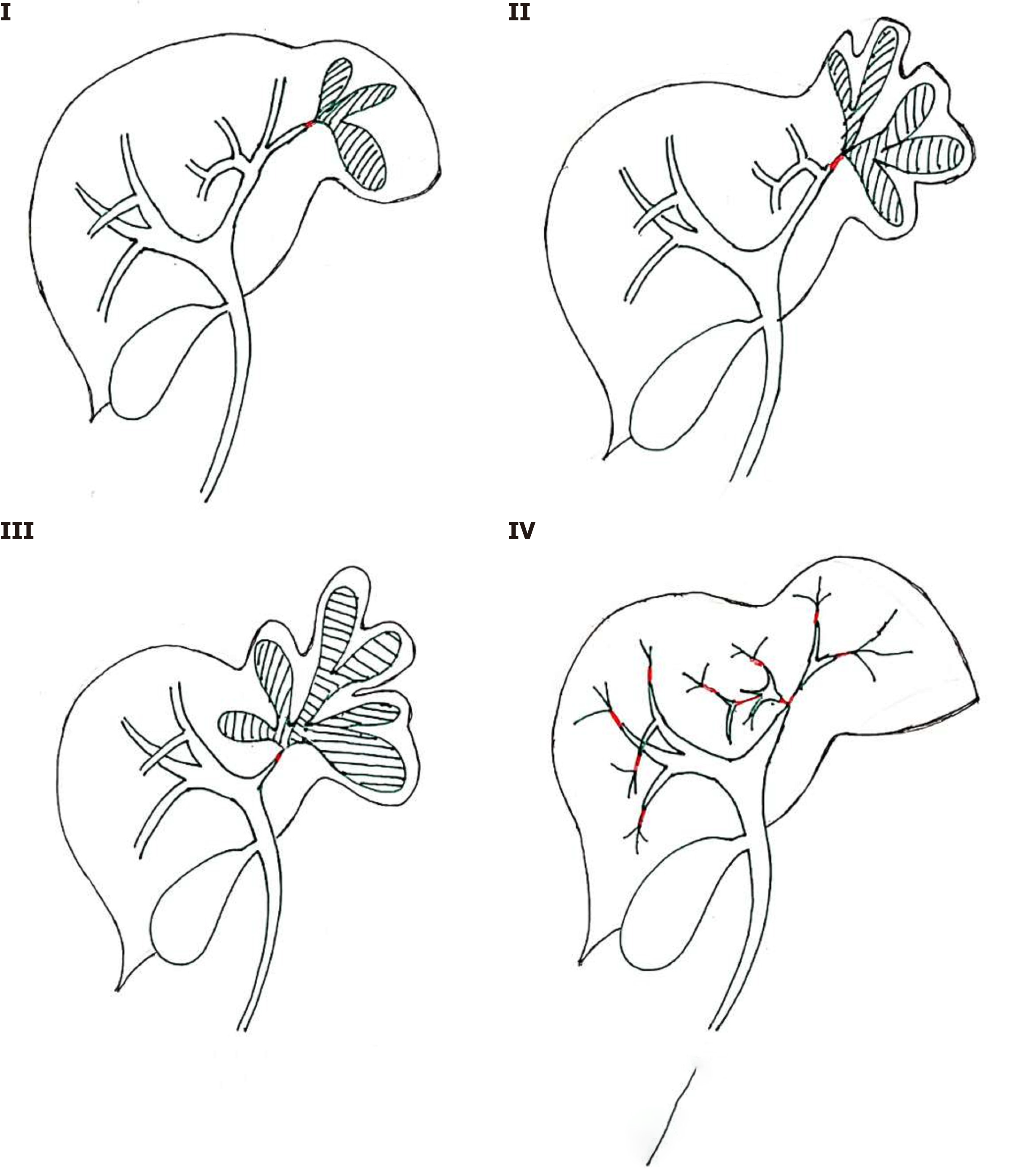
Patients with FIHS with definite malignant pathological evidence and those with benign biliary strictures that cannot be improve unless surgery is performed are strong indications for hepatectomy. We suggest that the following factors should be taken into account when selecting treatment approaches. (1) The anatomical location of FIHS in the liver might significantly affect the resection range as well as the residual liver function. (2) The stenosis degree of FIHS directly determines the feasibility of drainage for biliary strictures. FIHS with obvious secondary changes, such as lobe atrophy and filled hepatolithiasis, regardless of whether they are benign or malignant, should be resected if dilation or drainage is impossible through endoscopy. And (3) for multiple FIHS in both lobes, immune diseases of the hepatobiliary system, such as SD-PSC, AIH and LIH-IgG4-SC, should be considered first. Based on the factors described above, we proposed the following classification system for FIHS to guide its diagnosis and treatment (Figure 7): Type I: FIHS located within one segment of the liver; type II: FIHS located at the confluence of the bile ducts of one segment or two adjacent segments; type III: FIHS connected to the left or right hepatic duct; and type IV: Multiple FIHS located in both lobes of the liver. PTCD might be more reasonable for type I or II patients whose FIHS are located close to the surface of the liver or the abdominal wall to achieve drainage or pathological diagnosis. Correspondingly, ERCP might be more suitable for FIHS connected to the LHD and RHD (type III). Ultrasound or CT-guided puncture biopsy is the most commonly used method for the qualitative diagnosis of type IV FIHS. For the surgical approaches, partial hepatectomy, segmentectomy and hemihepatectomy are applicable for type I, II and III patients, respectively. For type IV patients, surgeons should first exclude diagnoses of immune-mediated hepatobiliary diseases.
In conclusion, FIHS is a relatively rare sign caused by various hepatobiliary diseases. Comprehensive analysis of the results of biochemistry, imaging, endoscopy and pathological examination might help to achieve a correct diagnosis of FIHS. We proposed a classification system to guide treatment approaches for FIHS based on its anatomical and histopathological features. We suggest that surgery should be performed in cases of not only malignant FIHS but also benign strictures with severe secondary damage that cannot be dilated or drained by nonsurgical methods.
Focal intrahepatic strictures (FIHS) refer to local strictures of the small and medium intrahepatic bile ducts. FIHS are easily misdiagnosed due to their rare incidence, and few studies have focused on the diagnosis and treatment approaches.
No diagnosis and treatment guideline for FIHS has been published so that misdiagnosed and mistreatment frequently occurs.
This study aims to propose a new classification for FIHS in order to guide its diagnosis and treatment.
The symptoms, biochemistry results, imaging results, endoscopic examination results and initial and final diagnoses of 6 patients with FIHS admitted between 2010/01 and 2019/12 were retrospectively analyzed.
The 6 patients were diagnosed with intratubular growth-type intrahepatic cholangiocarcinoma (IG-ICC), recurrent multiple hepatocellular carcinoma (rmHCC) with bile duct tumor thrombus (BDTT), adenosquamous carcinoma (ASC), hepatolithiasis, small duct primary sclerosing cholangitis (SD-PSC) and autoimmune hepatitis (AIH). The initial and final diagnoses were not consistent in 4 patients. Hepatectomy was performed in patients with IG-ICC, ASC and hepatolithiasis according to the locations of their FIHS. Patients with rmHCC with BDTT received lenvatinib/sintilimab, while patients with SD-PSC and AIH received UDCA. We proposed the following classification system for FIHS: type I: FIHS located within one segment of the liver; type II: FIHS located at the confluence of the bile ducts of one segment or two adjacent segments; type III: FIHS connected to the left or right hepatic duct; and type IV: Multiple FIHS located in both lobes of the liver.
Our proposed classification system might help to guide the diagnosis and treatment of FIHS. Hepatectomy should be performed not only for malignant FIHS but also for benign strictures with severe secondary damage that cannot be improved by nonsurgical methods.
The classification system and its guiding significance in the treatment of FIHS.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Matowicka-Karna J, Nacif L, Tarazov PG S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Li JH
| 1. | Yeo D, Perini MV, Muralidharan V, Christophi C. Focal intrahepatic strictures: a review of diagnosis and management. HPB (Oxford). 2012;14:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Chari ST, Smyrk TC, Levy MJ, Topazian MD, Takahashi N, Zhang L, Clain JE, Pearson RK, Petersen BT, Vege SS, Farnell MB. Diagnosis of autoimmune pancreatitis: the Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006;4:1010-6; quiz 934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 656] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 3. | Miyayama S, Yamashiro M, Okuda M, Yoshie Y, Nakashima Y, Ikeno H, Orito N, Notsumata K, Watanabe H, Toya D, Tanaka N, Matsui O. Main bile duct stricture occurring after transcatheter arterial chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2010;33:1168-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Kim SH, Lim HK, Choi D, Lee WJ, Kim SH, Kim MJ, Lee SJ, Lim JH. Changes in bile ducts after radiofrequency ablation of hepatocellular carcinoma: frequency and clinical significance. AJR Am J Roentgenol. 2004;183:1611-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Ni T, Shang XS, Wang WT, Hu XX, Zeng MS, Rao SX. Different MR features for differentiation of intrahepatic mass-forming cholangiocarcinoma from hepatocellular carcinoma according to tumor size. Br J Radiol. 2018;91:20180017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Kim BG, Kang DH, Choi CW, Kim HW, Lee JH, Kim SH, Yeo HJ, Lee SY. A case of clonorchiasis with focal intrahepatic duct dilatation mimicking an intrahepatic cholangiocarcinoma. Clin Endosc. 2011;44:55-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ch'ng LS, Amzar H, Ghazali KC, Siam F. Imaging appearances of hepatic tuberculosis: experience with 12 patients. Clin Radiol 2018; 73: 321.e11-321. e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Tonolini M, Bianco R. HIV-related/AIDS cholangiopathy: pictorial review with emphasis on MRCP findings and differential diagnosis. Clin Imaging. 2013;37:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 9. | Yimam KK, Bowlus CL. Diagnosis and classification of primary sclerosing cholangitis. Autoimmun Rev. 2014;13:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Mo Z, Ramen K, Shan Y, Zhou M, Zheng X, Wu X, Yu Z, Ji X, Zhang Q, Zeng Q. Localized intrahepatic IgG4-related sclerosing cholangitis (IgG4-SC) as an additional type of IgG4-SC: a systematic analysis of 12 cases. Scand J Gastroenterol. 2018;53:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Seo DW, Kim MH, Lee SK, Myung SJ, Kang GH, Ha HK, Suh DJ, Min YI. Usefulness of cholangioscopy in patients with focal stricture of the intrahepatic duct unrelated to intrahepatic stones. Gastrointest Endosc. 1999;49:204-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Chung YE, Kim MJ, Park YN, Choi JY, Pyo JY, Kim YC, Cho HJ, Kim KA, Choi SY. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics. 2009;29:683-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 276] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 13. | Nakazawa T, Ohara H, Sano H, Ando T, Imai H, Takada H, Hayashi K, Kitajima Y, Joh T. Difficulty in diagnosing autoimmune pancreatitis by imaging findings. Gastrointest Endosc. 2007;65:99-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Saito R, Fukuda T, Amano H, Nakahara M, Yoshida M, Yamaki M, Hanada K, Yonehara S, Noriyuki T. Follicular cholangitis associated with focal biliary stricture treated with left hepatectomy after 8 years of follow-up: A rare case report. Mol Clin Oncol. 2016;4:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Ishibashi H, Shimada M, Kamisawa T, Fujii H, Hamada Y, Kubota M, Urushihara N, Endo I, Nio M, Taguchi T, Ando H; Japanese Study Group on Congenital Biliary Dilatation (JSCBD). Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. 2017;24:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 16. | Saito T, Hishiki T, Terui K, Sato Y, Mitsunaga T, Terui E, Nakata M, Takenouchi A, Matsuura G, Yahata E, Ohno S, Sato H, Yanagawa N, Masuda Y, Yoshida H. Use of preoperative, 3-dimensional magnetic resonance cholangiopancreatography in pediatric choledochal cysts. Surgery. 2011;149:569-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Li H, Peng B. Laparoscopic Anatomical Left Hepatectomy for Intrahepatic Bile Duct Papillary Mucinous Cystadenoma With Intraoperative Vascular Repair: A Case Report. Medicine (Baltimore). 2016;95:e2802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Kim HJ, Lee KT, Kim SH, Lee JK, Lim JH, Paik SW, Rhee JC. Differential diagnosis of intrahepatic bile duct dilatation without demonstrable mass on ultrasonography or CT: benign versus malignancy. J Gastroenterol Hepatol. 2003;18:1287-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Zhu KL, Li DY, Jiang CB. Primary squamous cell carcinoma of the liver associated with hepatolithiasis: a case report. World J Gastroenterol. 2012;18:5830-5832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Nanashima A, Tobinaga S, Araki M, Kunizaki M, Abe K, Hayashi H, Harada K, Nakanuma Y, Nakagoe T, Takeshita H, Sawai T, Nagayasu T. Intraductal papillary growth of liver metastasis originating from colon carcinoma in the bile duct: report of a case. Surg Today. 2011;41:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Cheung MT, Kwok PC. Liver resection for intrahepatic stones. Arch Surg. 2005;140:993-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Wakabayashi H, Akamoto S, Yachida S, Okano K, Izuishi K, Nishiyama Y, Maeta H. Significance of fluorodeoxyglucose PET imaging in the diagnosis of malignancies in patients with biliary stricture. Eur J Surg Oncol. 2005;31:1175-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Darisetty S, Sekaran A, Rao GV. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: a single-center, prospective study. Gastrointest Endosc. 2011;74:511-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 133] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 24. | Navaneethan U, Hasan MK, Lourdusamy V, Njei B, Varadarajulu S, Hawes RH. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: a systematic review. Gastrointest Endosc 2015; 82: 608-14. e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 198] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 25. | Fior-Gozlan M, Giovannini D, Rabeyrin M, Mc Leer-Florin A, Laverrière MH, Bichard P. Monocentric study of bile aspiration associated with biliary brushing performed during endoscopic retrograde cholangiopancreatography in 239 patients with symptomatic biliary stricture. Cancer Cytopathol. 2016;124:330-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |