Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5722
Peer-review started: August 2, 2020
First decision: August 21, 2020
Revised: August 24, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: November 26, 2020
Processing time: 115 Days and 4.3 Hours
Annular pancreas (AP) is a rare congenital abnormal rotation of the pancreas. AP rarely occurs in adults. Pancreatic tumors and ampullary tumors are related to AP, so the discovery and treatment of AP are essential.
This study investigated the clinical manifestations, imaging features, complications, and treatment of six patients diagnosed with AP at the Department of Hepatobiliary and Pancreatic Surgery, First Hospital of Jilin University from January 2010 to June 2020. There were four males and two females, with an average age of 56.00 ± 9.86 years old. In this study, abdominal pain and jaundice were the main clinical manifestations. Imaging can show the “crocodile jaw sign” or “double bubble sign”.
For patients with duodenal or biliary obstruction, physicians should give priority to AP when imaging examinations suggest that the duodenum is wrapped with tissue similar to the density of the pancreas. Symptomatic patients should actively undergo surgical treatment.
Core Tip: Annular pancreas (AP) is a rare congenital abnormal rotation of the pancreas. AP is related to the occurrence of duodenal ulcers, pancreatitis, and digestive system tumors. In this study, the clinical manifestations, imaging features, complications, and treatment of AP were analyzed. If the imaging results show the “crocodile jaw sign”, the vigilance of congenital malformed AP should be increased for patients with digestive system obstruction.
- Citation: Yi D, Ding XB, Dong SS, Shao C, Zhao LJ. Clinical characteristics of adult-type annular pancreas: A case report . World J Clin Cases 2020; 8(22): 5722-5728
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5722.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5722
Annular pancreas (AP) is a rare congenital abnormal rotation of the pancreas, which is a ring of ectopic pancreatic tissue partially or completely surrounding the duodenum. During autopsy, the prevalence rate is 0.005%-0.015%[1]. The ring-shaped pancreas occurs mostly in neonates, presents with bilious vomiting due to duodenal obstruction[2], and is often associated with other congenital anomalies, including Down’s syndrome, tracheoesophageal fistula, intestinal atresia, pancreas division, and pancreaticobiliary malrotation[3,4]. AP rarely occurs in adults, presenting with the symptoms related to chronic pancreatitis and biliary obstruction, and some patients have no obvious clinical manifestations[1]. However, pancreatic tumors and ampullary tumors are related to AP, so the discovery and treatment of AP are essential[5,6]. This study retrospectively analyzed the clinical data of six patients with AP admitted to the Department of Hepatobiliary and Pancreatic Surgery, First Hospital of Jilin University from January 2010 to June 2020 and summarized the imaging manifestations, clinical manifestations, and treatment methods of AP to improve doctors' understanding and treatments of this rare entity.
Of the six patients, five had abdominal pain as the main complaint, and four of them had jaundice. Only one patient had vomiting as the main clinical manifestation.
One patient was diagnosed with duodenal ulcers due to abdominal pain half a month before being seen at our hospital. One patient was admitted to a local hospital for acute pancreatitis 1 mo prior. Later, he was transferred to our hospital for further treatment. The remaining four patients did not receive other treatments and received the first treatment at our hospital.
Of the six patients, three had a history of hypertension, and two had a history of type 2 diabetes. One case had silt-like stones in the bile duct without symptoms. One case had an unremarkable medical history.
Five patients had mild upper abdominal tenderness, and four had yellow skin and sclera. The other tests did not show obvious abnormal manifestations.
The levels of total bilirubin and glutamine transferase were elevated in four patients (Table 1).
| Gender | Age (yr) | Complaint | TBIL | GGT | Concomitant diseases |
| Male | 70 | A + J | 56.5 | 486 | Ampullary tumor, dilatation of the bile duct |
| Male | 48 | A + J | 92.6 | 964.1 | Dilatation of the bile duct |
| Female | 52 | A + J | 86.9 | 1256.8 | Dilatation of the bile duct |
| Female | 51 | V | 29.1 | 45.6 | Duodenal ulcer |
| Male | 48 | A + J | 74.5 | 1929.5 | Dilatation of the bile duct, bile duct stones, pancreatitis |
| Male | 67 | A | 21.6 | 60.8 | Ductal adenocarcinoma of the pancreas |
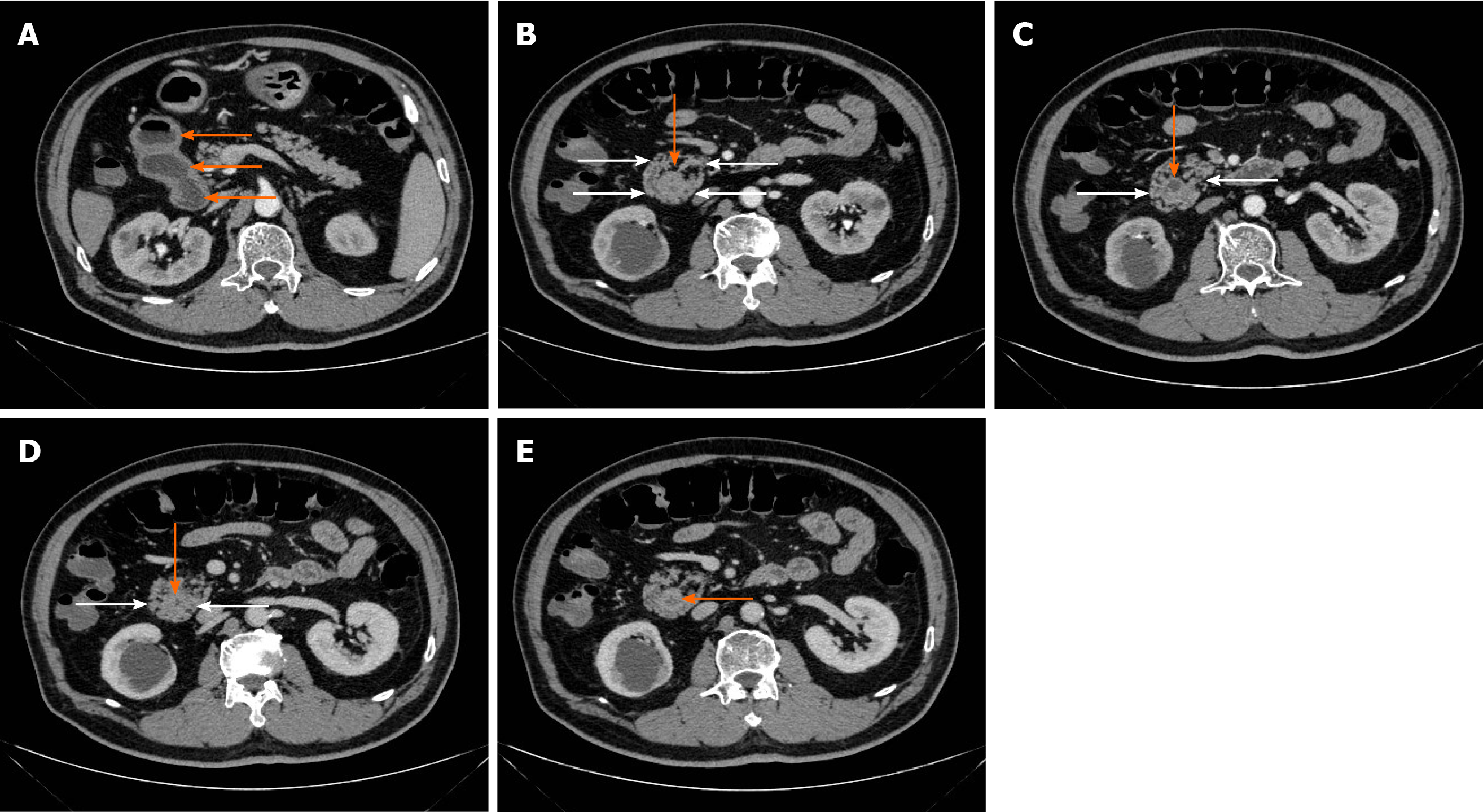
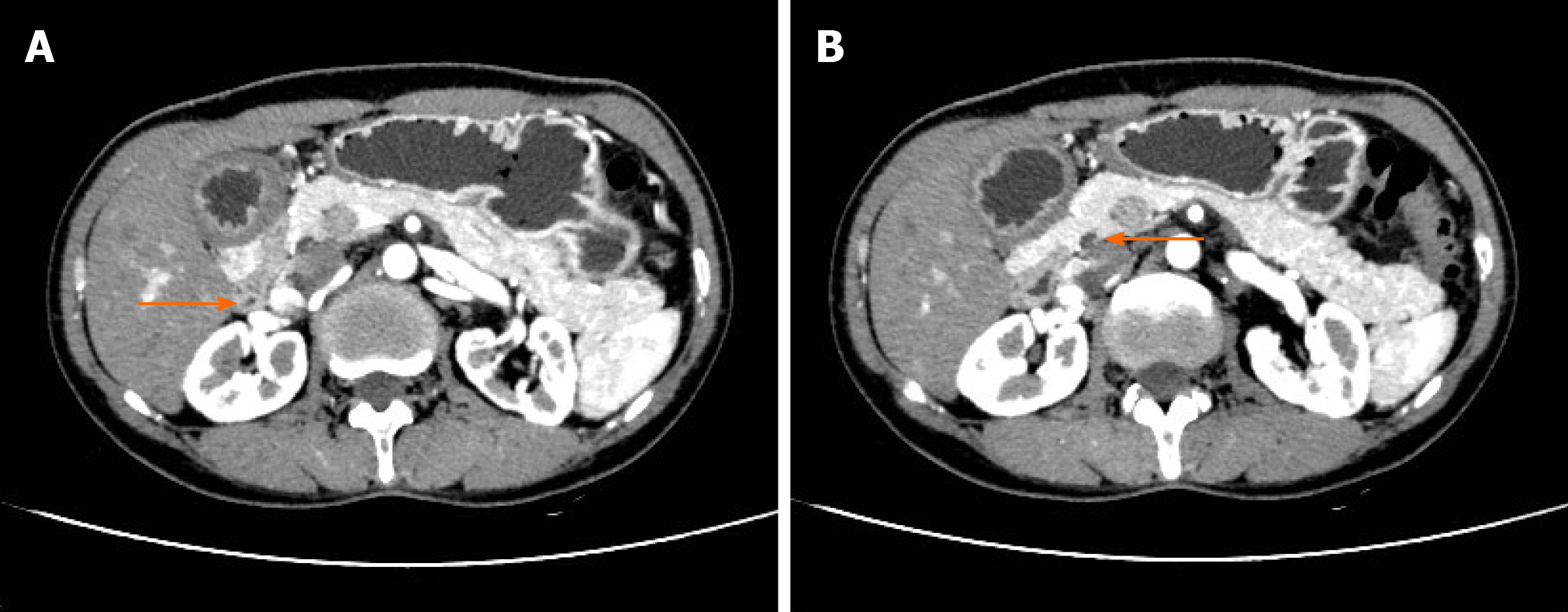
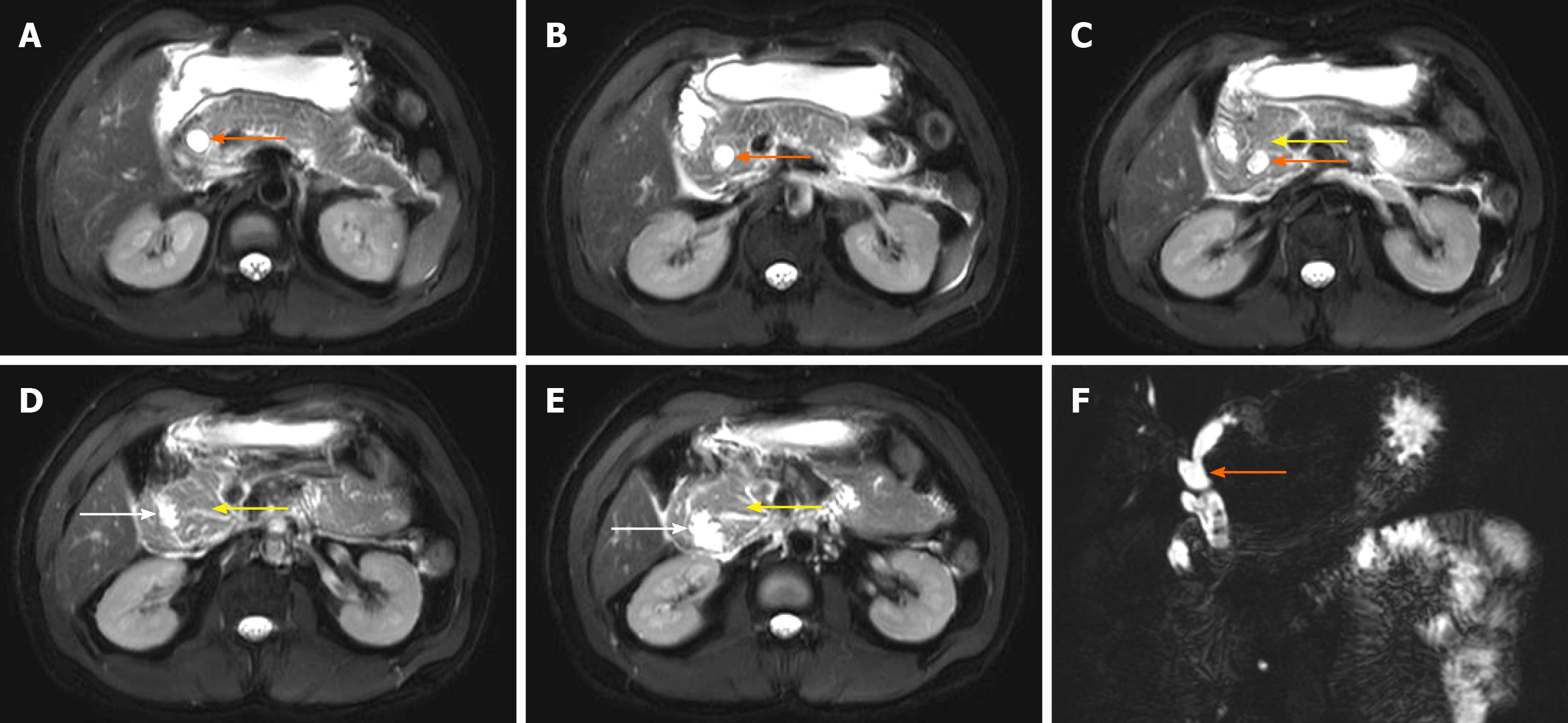
Abdominal contrast-enhanced computed tomography (CT) showed that all of the six cases had the pancreas wrapping around the duodenum; in five of them, it surrounded the descending section of the duodenum, and in one case, it surrounded the duodenal bulb. Four patients had biliary dilatation. The “double bubble sign” was observed in two cases (Figures 1-3). Magnetic resonance cholangiopancreatography (MRCP) examination performed in two patients showed similar signal of the soft tissue surrounding the duodenum to pancreatic tissue (Figures 4 and 5).
One patient had pancreatitis, one had bile duct stones, one had ampullary tumors, and one had pancreatic ductal adenocarcinoma.
A clear diagnosis was based on imaging examination and intraoperative findings. Surgery is the gold standard for the diagnosis of AP. Four patients were diagnosed with AP during the operation. Two patients were diagnosed with AP based on imaging examination.
During treatment, two patients underwent cholecystectomy, cholangiojejunostomy, and duodenojejunostomy. One patient underwent duodenojejunostomy. One patient underwent laparoscopic pancreaticoduodenectomy. Two other patients refused further treatment.
The patients received follow-up visits one year after being discharged from the hospital. Two patients who had not undergone surgery had symptoms of upper abdominal pain, but they still refused surgery. Among the four patients who underwent surgical treatment, three had good quality of life and no adverse complications. The other patient died after being diagnosed with pancreatic head cancer, bilateral lung metastasis, and abdominal lymph node metastasis.
AP is a congenital malformation. At approximately 6-7 wk of gestation, the duodenum rotates 90 degrees from the left to right, and the ventral side usually moves back and down around the duodenum[2,7-9]. The ventral pancreas then approaches the dorsal pancreas. Finally, ventral and dorsoventral fusion forms the pancreas[8]. The ventral pancreas forms most of the head of the pancreas. The dorsal pancreas forms a small part of the head of the pancreas and the body and tail of the pancreas. The ducts of the ventral and dorsal pancreas are connected. The original anterior pancreatic duct becomes the accessory pancreatic duct. The original dorsal pancreatic duct forms the main pancreatic duct and the accessory duct of the accessory pancreatic duct[4,9,10].
If the fusion position of the ventral pancreas and the dorsal pancreas is abnormal, all or part of the pancreas tissue surrounds and compresses the duodenum, causing complete or incomplete duodenal obstruction; the latter is more common. An incomplete AP means that the AP only surrounds 2/3 to 4/5 of the diameter of the duodenum. Six patients with AP in this study were recruited from a single center over 10 years, and all of them had incomplete AP, confirming that adult-type AP is rare and mainly incomplete duodenal obstruction.
AP in adults is characterized by peptic ulceration, duodenal obstruction, pancreatitis, and obstructive jaundice[1,11]; 70% of patients present with abdominal pain, 60% with nausea and vomiting, and a few with jaundice[3]. In this study, four patients had abdominal pain and jaundice, one only had abdominal pain, and one had nausea and vomiting. The clinical manifestations were related to the degree of duodenum compression by the AP, whether it compresses the common bile duct, and the degree of compression of the common bile duct. Compression of the duodenum and common bile duct directly leads to local obstruction of the duodenum, edema, and chronic inflammation of the bile duct and pancreas. This finding is consistent with the clinical manifestations reported by Kim et al[12] and Huddleston et al[9]. These studies suggested that, for patients with duodenal obstruction or biliary obstruction, pathological disease should be considered, and the vigilance of congenital malformed AP should be increased.
Imaging examination has a suggestive role in preoperative diagnosis. CT examination showed that the head of the pancreas was enlarged, and pancreatic tissue went from the back of the duodenum to its descending portion. The texture, density, and enhancement of the AP tissue are similar to those of normal pancreatic tissue, completely or partially surrounding the duodenum. When it is found that the pancreatic head is located in front of or behind the duodenum, or the pancreas tissue is located on the back and outside of the duodenum, it is called the “crocodile jaw sign”[9,13]. The results of preoperative imaging examinations in this study were similar to those reported in the literature. CT enhancement of the upper abdomen revealed pancreatic tissue rings, dilation of the common bile duct, and double bubble signs, which meant that the duodenum and stomach expanded due to duodenal obstruction. Bile duct calculus and peripancreatic exudation can also be seen in some cases.
Endoscopic retrograde cholangiopancreatography (ERCP) and MRCP can show an annular pancreatic duct trend, but as the ERCP is an invasive operation, MRCP combined with CT is preferred. MRCP examination has guiding significance in the diagnosis of AP. In this study, MRCP showed that the signal intensity of soft tissue extending along the pancreatic head and surrounding the duodenum was similar to that of normal pancreas. The fine-line tubular signal can be seen in the soft tissue, communicating with the main pancreatic duct, and the main pancreatic duct is slightly dilated. The upper part of the enveloping duodenum and the common bile duct are slightly dilated. In this study, part of the pancreas was observed around the duodenum during the operation. Therefore, surgery is the gold standard for the diagnosis of AP.
Adult-type AP should be differentiated from pancreatic cancer and duodenal cancer. Pancreatic head cancer is characterized by a lack of blood supply, mild heterogeneous enhancement, unclear border, invasion of blood vessels, and metastases to the liver, lymph nodes, and peritoneum. Duodenal cancer is characterized by a concentric narrowing of the duodenal cavity, thickening of the duodenal wall, and irregular masses. Besides, it can metastasize to the liver, peritoneum, and lymph nodes[9].
Adult-type AP is associated with pancreatitis, malignant tumors of the digestive system, and duodenal ulcers[14,15]. In this study, one case of AP patient was complicated with duodenal ulcers due to the gastric retention and high acidity caused by duodenal stenosis[16]. In this case, the duodenal bulb and the back of the bulb were surrounded by the pancreatic head from the rear. The obstructed bile and alkaline digestive fluid of pancreatic juice entered the intestinal cavity, causing damage to the intestinal mucosa. One patient with AP was complicated by pancreatitis and bile duct stones. The reason may be due to the compression of the common bile duct and pancreatic duct, as the pancreatic juice cannot be discharged smoothly, and cholestasis could lead to pancreatitis and cholelithiasis. One case of AP complicated with pancreatic duct adenocarcinoma and one case complicated with ampulla tumor were included in this study. It is speculated that the duodenal obstruction caused by AP will lead to the continuous loss of cells in the ampulla area, and the rapid renewal of mucosa may lead to abnormal proliferation and metaplasia in this area[17]. At the same time, the occurrence of pancreatic cancer may be related to chronic pancreatitis, but it is currently impossible to prove its causal relationship. Therefore, patients with AP with clinical manifestations should be operated on in a timely manner to avoid serious complications and reduce mortality.
Asymptomatic AP does not need treatment[18]. Duodenojejunostomy is preferred for patients with severe duodenal stricture[19]. Pancreatoduodenectomy should be considered for AP associated with chronic pancreatitis, pancreatic duct stones, or malignant tumors[3].
AP in adults is characterized by duodenal obstruction, pancreatitis, and obstructive jaundice. Imaging can show the “crocodile jaw sign” or “double bubble sign”. MRCP shows that the signal of annular pancreatic is similar to normal pancreatic. Adult circular pancreas is associated with pancreatitis, malignant tumors of the digestive system, and duodenal ulcers. Surgical treatment should be performed for AP with clinical symptoms in time.
The authors thank all the patients who participated in the survey.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tabibian JH S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Li JH
| 1. | Mittal S, Jindal G, Mittal A, Singal R, Singal S. Partial annular pancreas. Proc (Bayl Univ Med Cent). 2016;29:402-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Agrawal H, Gupta N, Krishengowda U, Gupta AK, Naskar D, Durga CK. Transmural Migration of Gossypiboma: a Rare Cause of Acute Abdomen. Indian J Surg. 2018;80:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Rondelli F, Bugiantella W, Stella P, Boni M, Mariani E, Crusco F, Sanguinetti A, Polistena A, Avenia N. Symptomatic annular pancreas in adult: Report of two different presentations and treatments and review of the literature. Int J Surg Case Rep. 2016;20S:21-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Jovani M, Lee LS. Annular Pancreas. Clin Gastroenterol Hepatol. 2020;18:A26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Nunley B, Collins H, Weber F. Gastroparesis Mimicry: Thinking Beyond the Pylorus. Gastroenterology. 2019;157:610-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Komine R, Shimizu A, Mori K, Minamimura K, Hirata T, Kobayashi T, Toda N, Mori M. Pancreaticoduodenectomy for an Ampullary Region Carcinoma Occurred in Annular Pancreas Coexistent with Replaced Common Hepatic Artery. Case Rep Med. 2018;2018:3258141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Sato N, Shimura T, Kenjo A, Kimura T, Watanabe J, Muto M, Marubashi S. Pancreaticobiliary maljunction diagnosed long after laparotomy in the neonatal period for annular pancreas: report of a case. Surg Case Rep. 2019;5:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Kobayashi S, Hoshino H, Segami K, Koizumi S, Ooike N, Otsubo T. Incomplete Annular Pancreas with Ectopic Opening of the Pancreatic and Bile Ducts into the Pyloric Ring: First Report of a Rare Anomaly. Case Rep Gastroenterol. 2016;10:373-380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Huddleston VS, Lippuner V, Dyer AW. Annular Pancreas in an Adult Presenting with Acute Pancreatitis. J Radiol Case Rep. 2018;12:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Etienne D, John A, Menias CO, Ward R, Tubbs RS, Loukas M. Annular pancreas: a review of its molecular embryology, genetic basis and clinical considerations. Ann Anat. 2012;194:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Mielko J, Kurylcio A, Skórzewska M, Ciseł B, Polkowska B, Rawicz-Pruszyński K, Sierocińska-Sawa J, Polkowski WP. Duodenal obstruction due to annular pancreas associated with carcinoma of the duodenum. Prz Gastroenterol. 2016;11:139-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kim SB, Kim KH, Kim TN. Annular Pancreas in Adult. Korean J Gastroenterol. 2018;71:294-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Xiang H, Han J, Ridley WE, Ridley LJ. Crocodile jaw sign: Annular pancreas. J Med Imaging Radiat Oncol. 2018;62 Suppl 1:69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Gromski MA, Lehman GA, Zyromski NJ, Watkins JL, El Hajj II, Tan D, McHenry L, Easler JJ, Tirkes T, Sherman S, Fogel EL. Annular pancreas: endoscopic and pancreatographic findings from a tertiary referral ERCP center. Gastrointest Endosc. 2019;89:322-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Wood CG, Lopes Vendrami C, Craig E, Mittal PK, Miller FH. Pancreatitis in the developmentally anomalous pancreas. Abdom Radiol (NY). 2020;45:1316-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Alahmadi R, Almuhammadi S. Annular pancreas: a cause of gastric outlet obstruction in a 20-year-old patient. Am J Case Rep. 2014;15:437-440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Tewari M, Verma A, Shukla HS. Carcinoma of the Ampulla of Vater Associated with Annular Pancreas. Indian J Surg. 2016;78:409-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Ji FJ, Tian XF, Wei L, Fang XD, Cao H, Jin HY. A case of annular pancreas accompanied with intraductal papillary mucinous neoplasm-case report. Int J Clin Exp Med. 2015;8:3332-3337. [PubMed] |
| 19. | Chittawadagi B, Senthilnathan P, Jankar SV, Sabnis SC, Parthasarathi R, Palanivelu C. Laparoscopic Roux-en Y duodenojejunostomy: A safe and physiological treatment for symptomatic annular pancreas in adults. J Minim Access Surg. 2019;16:121-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |