Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5715
Peer-review started: July 28, 2020
First decision: August 7, 2020
Revised: September 15, 2020
Accepted: September 22, 2020
Article in press: September 22, 2020
Published online: November 26, 2020
Processing time: 120 Days and 5.6 Hours
An atrial septal defect is a common condition and accounts for 25% of adult congenital heart diseases. Transcatheter occlusion is a widely used technique for the treatment of secondary aperture-type atrial septal defects (ASDs).
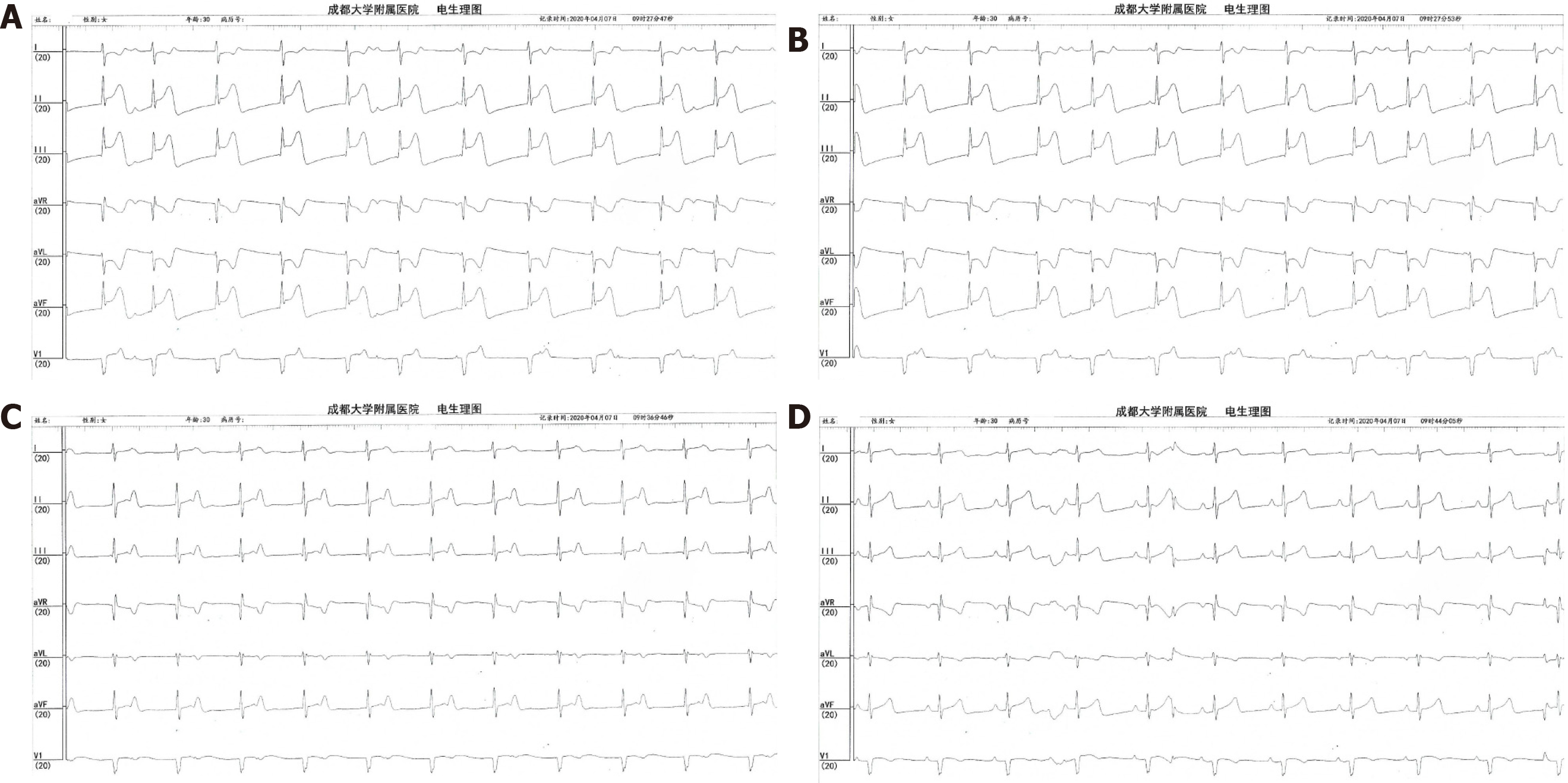
A 30-year-old female patient was diagnosed with ASD by transthoracic echocardiography (TTE) 1 year ago. The electrocardiogram showed a heart rate of 88 beats per minute, normal sinus rhythm, and no change in the ST-T wave. After admission, TTE showed an atrial septal defect with a left-to-right shunt, aortic root short-axis section with an ASD diameter of 8 mm, a parasternal four-chamber section with an ASD diameter of 9 mm, and subxiphoid biatrial section with a diameter of 13 mm. Percutaneous occlusion was proposed. The intraoperative TTE scan showed that the atrial septal defect was oval in shape, was located near the root of the aorta, and had a maximum diameter of 13 mm. A 10-F sheath was placed in the right femoral vein, and a 0.035° hard guidewire was used to establish the transport track between the left pulmonary vein and the inferior vena cava. A shape-memory alloy atrial septal occluder with a waist diameter of 20 mm was placed successfully and located correctly. TTE showed that the double disk unfolded well and that the clamping of the atrial septum was smooth. Immediately after the disc was revealed, electrocardiograph monitoring showed that the ST interval of the inferior leads was prolonged, the P waves and QRS waves were separated, a junctional escape rhythm maintained the heart rate, and the blood pressure began to decrease. After removing the occluder, the elevation in the ST segment returned to normal immediately, and the sinus rhythm returned to average approximately 10 min later. After consulting the patient’s family, we finally decided to withdraw from the operation.
Compression of the small coronary artery, which provides an alternative blood supply to the atrioventricular nodule during the operation, leads to the emergence of a complete atrioventricular block.
Core Tip: This report introduces a case of complete atrioventricular block caused by atrial septal defect occluder. During the placement of the occluder, a complete atrioventricular block suddenly appeared. Electrocardiograph monitoring showed that the ST interval in the inferior wall lead was prolonged, P wave and QRS complex were separated, the heart rate was maintained by junctional escape rhythm, and the blood pressure began to decrease.
- Citation: He C, Zhou Y, Tang SS, Luo LH, Feng K. Completed atrioventricular block induced by atrial septal defect occluder unfolding: A case report. World J Clin Cases 2020; 8(22): 5715-5721
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5715.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5715
An atrial septal defect (ASD) is a common adult congenital heart disease. Adult patients with atrial septal defects are often associated with pulmonary hypertension. Due to the traditional treatment of surgical trauma, the postoperative recovery is slow, so it is faced with many dilemmas in clinical application. Transcatheter closure of secundum ASD is a widely used technique for the treatment of secundum ASD. Compared with surgery, it is less invasive, has a faster recovery, and has less impact on the physical and mental health of patients. Nowadays, a considerable number of secondary secundum ASDs can be closed by a transcatheter approach, and its application fields are vast. However, despite the low probability of occurrence, there are still some severe complications in percutaneous ASD occlusion. This paper introduces a case of complete atrioventricular block caused by ASD occluder.
A 30-year-old-female patient presented with ASD, which was confirmed by transthoracic echocardiography (TTE) about 1 year ago without obvious symptoms.
The patient was in good overall health and had normal vital signs.
There is no history of surgery or allergy.
Electrocardiography showed heart rate of 88 bpm, normal sinus rhythm, and no ST-T change.
Blood test is normal.
The TTE examination after admittance revealed there was an ASD with left to right shunt with a diameter of 8 mm in aortic root short-axis view, 9 mm in parasternal four-chamber views, and 13 mm in subxiphoid biatrial view.
Completed atrioventricular block induced by ASD occluder unfolding.
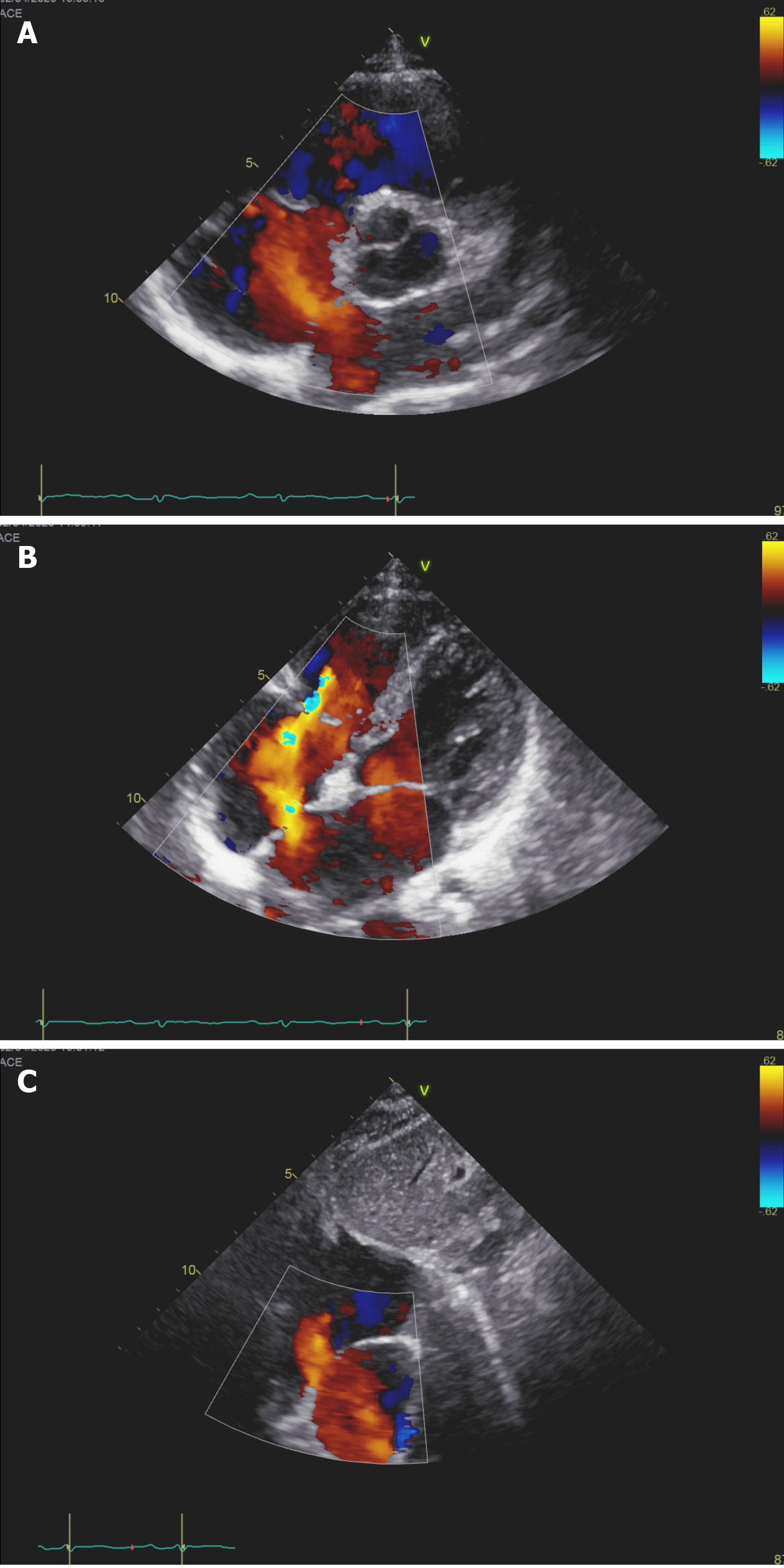
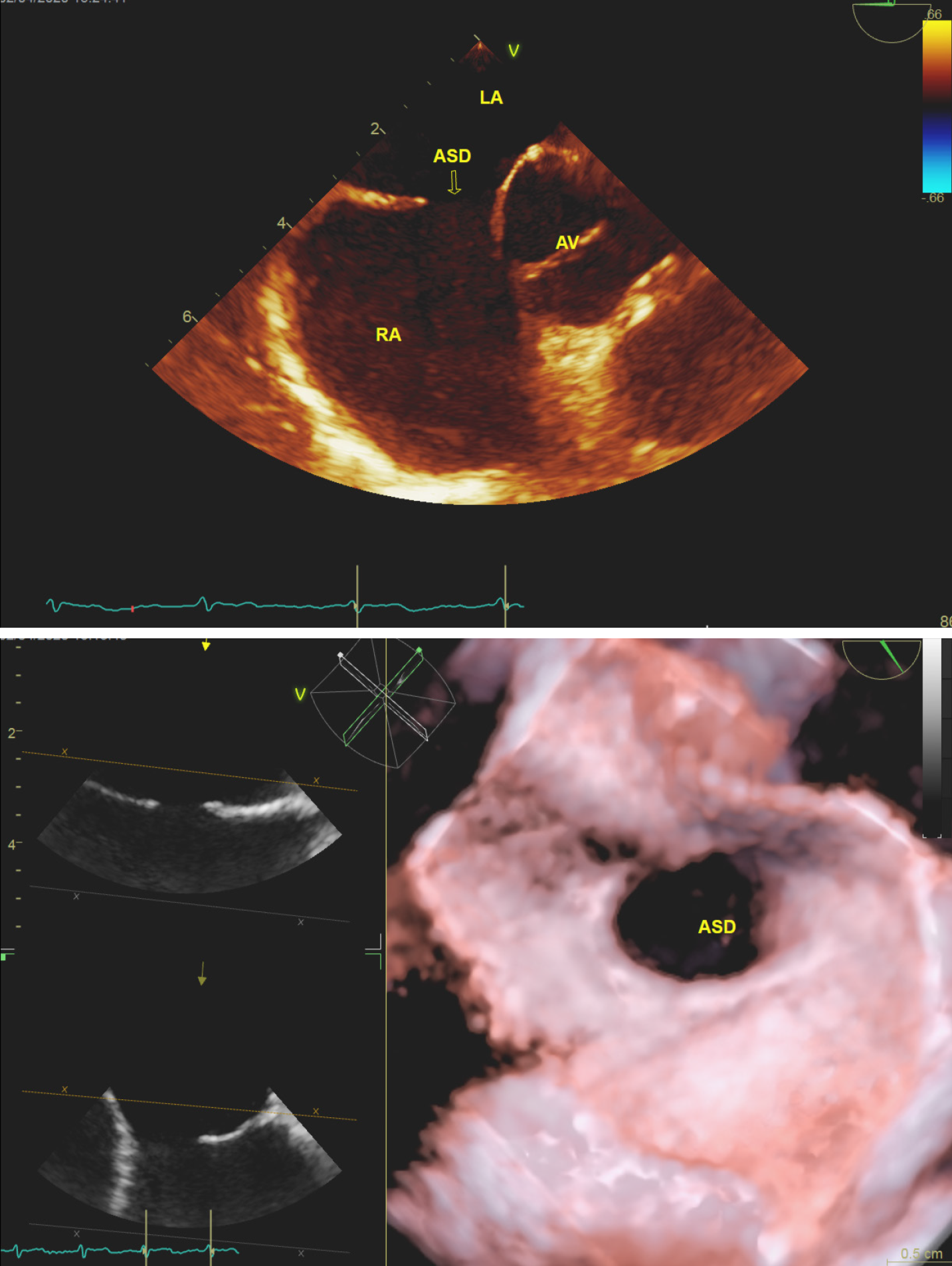
The procedure was performed under continuing venous anesthesia [Remifentanil, 0.1 μg/(kg·min)], and monitored by three-dimensional transthoracicechocardiography (3D-TEE). TEE rendered morphology of the ASD as oval, next to the aortic root, and diameter of 13 mm (Figures 1 and 2). A 10-F sheath [SteerEase, Lifetech Scientific (Shenzhen) Co., Ltd, China] was inserted into the right femoral vein, and the delivery track between the left pulmonary vein and the vena cava was established through a 0.035 angled stiff guidewire (Asahi intecc.co., Ltd, Japan). The atrial septal occlusion device based on shape-memory alloys [CeraTM ASD occlude, Lifetech Scientific (Shenzhen) Co., Ltd, China] with a waist diameter of 20 mm was successfully deployed with proper positioning. TEE showed the dual disc unfolding well and clamping atrial septal smoothly. Just after the disc was revealed, the electrocardiograph monitor showed that ST duration elevated in inferior leads and dissociated of the P wave and QRS complex, and the heart rate was maintained by junctional escape rhythm. When we wonder what has happened, the blood pressure began to fall. We gave the patient methylprednisolone (40 mg) intravenous injection immediately and expedited fluid infusion. The situation was not relieved after several minutes of close observation, and then we retrieved the occluder. The elevated ST duration had fallen to a reasonable level, almost at the same time when the occluder retreated. About 10 min later, the sinus rhythm came back (Figure 3).
According to the response of the patient to the occlusion device, and discussion with the family of the patient, we decided to quit the procedure.
An ASD is a common condition, accounting for 25% of adult congenital heart diseases[1]. Adult patients with ASDs are often complicated with pulmonary hypertension[2]. The traditional treatment method is surgery to repair the ASD after cardiopulmonary bypass. The trauma is enormous, and the recovery after surgery is slow but not accepted by the patient. Transcatheter occlusion is a widely used technique for the treatment of secondary aperture-type ASDs[3-6]. Compared with surgery, it is a less invasive method with faster recovery and fewer psychological side effects[7,8].
Today, almost 85%-90% of secondary hole-type ASDs can be closed by the transcatheter approach. However, several limiting factors may have a significant impact on the feasibility and success of percutaneous ASD closure. The limiting factors can be divided into the following categories: (1) Anatomical limitations: Anatomical limitations exist for all available equipment. The devices consist of two discs and a connecting segment, which keeps them together across the ASD. All currently available equipment requires a surrounding wall structure to support its stability. In particular, the diameter of nonself-centering discs should be 1.8 to 2 times the diameter of the defect so that the defect can be completely closed, avoiding misalignment or embolism[9]. The main anatomical limitations of percutaneous ASD occlusion may be insufficient peripheral margins, multiplicity, and excessively dilated atrial septal aneurysms. The main anatomical limitations of percutaneous ASD closure may be insufficient peripheral margins, multiple defects, and over dilated atrial septal aneurysms. This type of limitation is typical for sinus venous ASDs near the openings of the venae cavae. Defects on the surrounding edges may affect the placement of the device[10]; (2) Device-related limitations: In most patients with a secondary ASD, transcatheter closure is the preferred treatment strategy. In rare cases, transcatheter closure of the ASD may cause significant complications, including perforation of the wall, device embolism, and atrial arrhythmia[11-15]. Although these adverse events occur in less than 2% of patients, if a large device is required to close the defect, the incidence of complications may increase. More significant ASDs have less residual tissue and smaller edges, and the use of larger devices may increase the risk of atrial perforation[16]; (3) Related defects and issues related to natural medical history[17]; (4) Physiological restrictions; and (5) Complications[10,16]. Complications may limit the feasibility and success rate of transcatheter closure of the ASD. They include device embolism, a new complete atrioventricular block (CAVB) attack, and myocardial erosion[18]. Occlusion or displacement of the occluder is a common, serious complication of ASD occluders. It is often caused by the occluder being too small, the anatomical location of the lesion being in a difficult location, and the inappropriate determination of indications. Approximately 80% of these complications are caused by insufficient inferior margins.
It has been reported that CAVB occurs sporadically at the time of surgery or a few hours or days later and requires initial steroid therapy. If there is no response, the device is subsequently surgically removed, and the ASD is left open. CAVB is usually thought to be due to compression of the atrioventricular node and inflammatory foreign body reaction or scar formation at the Koch triangle level due to the presence of the device. The risk factors for CAVB after the closure of the ASD include a small posterior margin, the use of excessively large equipment in children, and atrioventricular nodal conduction disorder[19].
In this case, the ST-segment elevation of the inferior lead occurred at the exact moment the occluder disc was deployed, followed by a complete atrioventricular block, and blood pressure decreased throughout. All abnormal signals returned to normal after the occluder was removed. Atrioventricular node-compression or inflammatory foreign body reaction is difficult to explain, given no history of atrioventricular block. When we reviewed the literature, we found that a single case of compression of a small coronary artery that provides an alternative blood supply to atrioventricular nodules has been described[20]. If this mechanism does exist, the entire event can be fully explained.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berger BM, Greenwood MP S-Editor: Wang DM L-Editor: Filipodia P-Editor: Li JH
| 1. | Alkashkari W, Albugami S, Hijazi ZM. Current practice in atrial septal defect occlusion in children and adults. Expert Rev Cardiovasc Ther. 2020;18:315-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Pratama RS, Hartopo AB, Anggrahini DW, Dewanto VC, Dinarti LK. Serum soluble suppression of tumorigenicity-2 Level associates with severity of pulmonary hypertension associated with uncorrected atrial septal defect. Pulm Circ. 2020;10:2045894020915832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Schiavone M, Forleo GB. Standing on the ledge: Atrial fibrillation ablation in patients with atrial septal closure devices. J Cardiovasc Electrophysiol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Kadirogullari E, Onan B, Timur B, Birant A, Reyhancan A, Basgoze S, Aydin U. Transcatheter closure vs totally endoscopic robotic surgery for atrial septal defect closure: A single-center experience. J Card Surg. 2020;35:764-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Sievert H, Babic UU, Hausdorf G, Schneider M, Höpp HW, Pfeiffer D, Pfisterer M, Friedli B, Urban P. Transcatheter closure of atrial septal defect and patent foramen ovale with ASDOS device (a multi-institutional European trial). Am J Cardiol. 1998;82:1405-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 122] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Ghaderian M, Sabri MR, Ahmadi AR, Alipour MR, Dehghan B, Mehrpour M. Midterm Follow-up Results of Transcatheter Interatrial Septal Defect Closure. Heart Views. 2019;20:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Ooi YK, Kelleman M, Ehrlich A, Glanville M, Porter A, Kim D, Kogon B, Oster ME. Transcatheter Versus Surgical Closure of Atrial Septal Defects in Children: A Value Comparison. JACC Cardiovasc Interv. 2016;9:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Shi D, Kang Y, Zhang G, Gao C, Lu W, Zou H, Jiang H. Biodegradable atrial septal defect occluders: A current review. Acta Biomater. 2019;96:68-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Nassif M, Abdelghani M, Bouma BJ, Straver B, Blom NA, Koch KT, Tijssen JG, Mulder BJ, de Winter RJ. Historical developments of atrial septal defect closure devices: what we learn from the past. Expert Rev Med Devices. 2016;13:555-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Faccini A, Butera G. Atrial septal defect (ASD) device trans-catheter closure: limitations. J Thorac Dis. 2018;10:S2923-S2930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Yang MC, Wu JR. Recent review of transcatheter closure of atrial septal defect. Kaohsiung J Med Sci. 2018;34:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Wang J, Patel M, Xiao M, Xu Z, Jiang S, Sun X, Xu L, Wang H. Incidence and predictors of asymptomatic pericardial effusion after transcatheter closure of atrial septal defect. EuroIntervention. 2016;12:e250-e256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Olasinska-Wisniewska A, Grygier M. Antithrombotic/Antiplatelet Treatment in Transcatheter Structural Cardiac Interventions-PFO/ASD/LAA Occluder and Interatrial Shunt Devices. Front Cardiovasc Med. 2019;6:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | López-Fernández T, Gómez de Diego JJ, Monedero MC, Cabestrero D, Mesa JM, Moreno I, Moreno Yangüela M, López de Sa E, López-Sendoón JL. Aortic wall erosion after percutaneous closure of atrial septal defect. J Am Soc Echocardiogr 2011; 24: 227.e5-227. e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Lopez K, Dalvi BV, Balzer D, Bass JL, Momenah T, Cao QL, Hijazi ZM. Transcatheter closure of large secundum atrial septal defects using the 40 mm Amplatzer septal occluder: results of an international registry. Catheter Cardiovasc Interv. 2005;66:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Meyer MR, Kurz DJ, Bernheim AM, Kretschmar O, Eberli FR. Efficacy and safety of transcatheter closure in adults with large or small atrial septal defects. Springerplus. 2016;5:1841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Albæk DHR, Udholm S, Ovesen AL, Karunanithi Z, Nyboe C, Hjortdal VE. Pacemaker and conduction disturbances in patients with atrial septal defect. Cardiol Young. 2020;30:980-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Moore J, Hegde S, El-Said H, Beekman R 3rd, Benson L, Bergersen L, Holzer R, Jenkins K, Ringel R, Rome J, Vincent R, Martin G; ACC IMPACT Steering Committee. Transcatheter device closure of atrial septal defects: a safety review. JACC Cardiovasc Interv. 2013;6:433-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 153] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 19. | Asakai H, Weskamp S, Eastaugh L, d'Udekem Y, Pflaumer A. Atrioventricular block after ASD closure. Heart Asia. 2016;8:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Yamamoto T, Kanazawa H, Tanosaki S, Goto S, Kimura M, Tsuruta H, Itabashi Y, Murata M, Kunitomi A, Aizawa Y, Nishiyama T, Kohno T, Maekawa Y, Takatsuki S, Sano M, Igawa O, Fukuda K. A Novel Mechanism of Atrioventricular Block Following Transcatheter Closure of an Atrial Septal Defect. JACC Cardiovasc Interv. 2016;9:2067-2069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |