Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5678
Peer-review started: June 13, 2020
First decision: September 13, 2020
Revised: September 22, 2020
Accepted: October 19, 2020
Article in press: October 19, 2020
Published online: November 26, 2020
Processing time: 165 Days and 9.5 Hours
Neurofibromatosis is an autosomal dominant genetic disorder with various manifestations. Systemic multiple neurofibromatosis is rare in infancy. The disease is difficult to identify in the early stage, and it is prone to misdiagnosis and missed diagnosis. In the presence of lower limb swelling with subcutaneous nodules of unknown cause, café-au-lait spots, and axillary freckles, this disease must be considered. This report presents the clinical manifestations, early detection, diagnosis and treatment, and prognosis of infantile neurofibromatosis type I (NF1).
The clinical manifestations, imaging examinations, and gene results of a 3-mo-old male infant with NF1 were analyzed retrospectively. He had “swelling of both legs” at the onset and developed café-au-lait spots, axillary freckles, and multiple neurofibromas later. He had a family history of similar conditions. Gene detection showed a heterozygous mutation of c.4537C>T in the NF1 gene, leading to a nonsense mutation of amino acids (p.R1513x), which originated from the mother of the infant. He was diagnosed with NF1.
Gene diagnosis plays an important role in the early diagnosis of NF1.
Core Tip: Neurofibromatosis type I (NF1) is a common autosomal dominant disorder with clinical symptoms in the skin, nervous system, skeleton, and eyes. NF1 development is related to gene deletion, and its incidence rate is about 1/3000. It is rare among children, especially infants. This report presents the case of a 3-mo-old male infant who was diagnosed with NF1. We believe that our study makes a significant contribution to the literature because this information will be of practical use to clinicians for management of similar conditions and encourage other researchers to validate our findings.
- Citation: Li MZ, Yuan L, Zhuo ZQ. Gene diagnosis of infantile neurofibromatosis type I: A case report. World J Clin Cases 2020; 8(22): 5678-5683
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5678.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5678
Neurofibromatosis type I (NF1) is a common autosomal dominant disorder, which can cause clinical symptoms in the skin, nervous system, skeleton, and eyes. The development of NF1 is related to gene deletion, and its incidence rate is about 1/3000[1]. It is rare among children, especially infants. Early clinical symptoms are often atypical; hence, it can be easily misdiagnosed. In this paper, we report the case of NF1 in an infant admitted to our hospital in April 2020 and describe the clinical characteristics, diagnosis, treatment, and prognosis of the infant with a brief review of relevant literature.
A 3-mo-old male infant reported to the hospital “5 d after discovery of masses in both lower limbs”.
Five days before admission, the family members found swelling of the child’s lower limbs. They brought him to a local hospital for treatment, and he was then referred to our hospital owing to the presence of multiple thrombi in the lower limbs. At present, except for skin changes and multiple neurofibromas, there are no other typical symptoms and complications.
At birth, brown spots of different sizes were noted on the skin of the patient’s trunk, limbs, and buttocks. With increase in age, the colored spots increased in number and size; however, the patient had not been hospitalized.
The patient was G2P2 with full term delivery and without abnormal birth history. He had a family history of similar conditions. Café-au-lait spots were noted on the skin of his maternal great-grandmother, maternal great-uncle, and mother. In addition to café-au-lait spots on the skin, the mother also had multiple skin nodules (Figure 1) without any self-perceived symptoms. An older female cousin of the child had epilepsy and mental retardation and had died at the age of 5 years. The uncle of the child (i.e. the older female cousin’s father) had chromosome abnormalities (according to the oral statement of the family members; test results were not available).
The head circumference was 39.2 cm, height 61.0 cm, and weight 5.6 kg. He had a clear mind, and fair spirit and response. Scattered oval café-au-lait spots of different sizes could be seen on the trunk and limbs, which were light brown with clear boundaries, not protruding from the skin surface, and with a diameter of 0.5-3.0 cm. Freckle-like depigmentation spots were seen on the chest, abdomen, neck, and left shoulder and armpit (Figure 2). Large areas of brown pigmentation were noted on the lower limbs, feet, buttocks, and perineum (Figure 3). Both calves and feet were swollen, which was significant on the right side. Solid nodules, which had a soft texture, could be palpated. There were no other abnormal signs.
No abnormalities were found in the blood coagulation tests performed at admission.
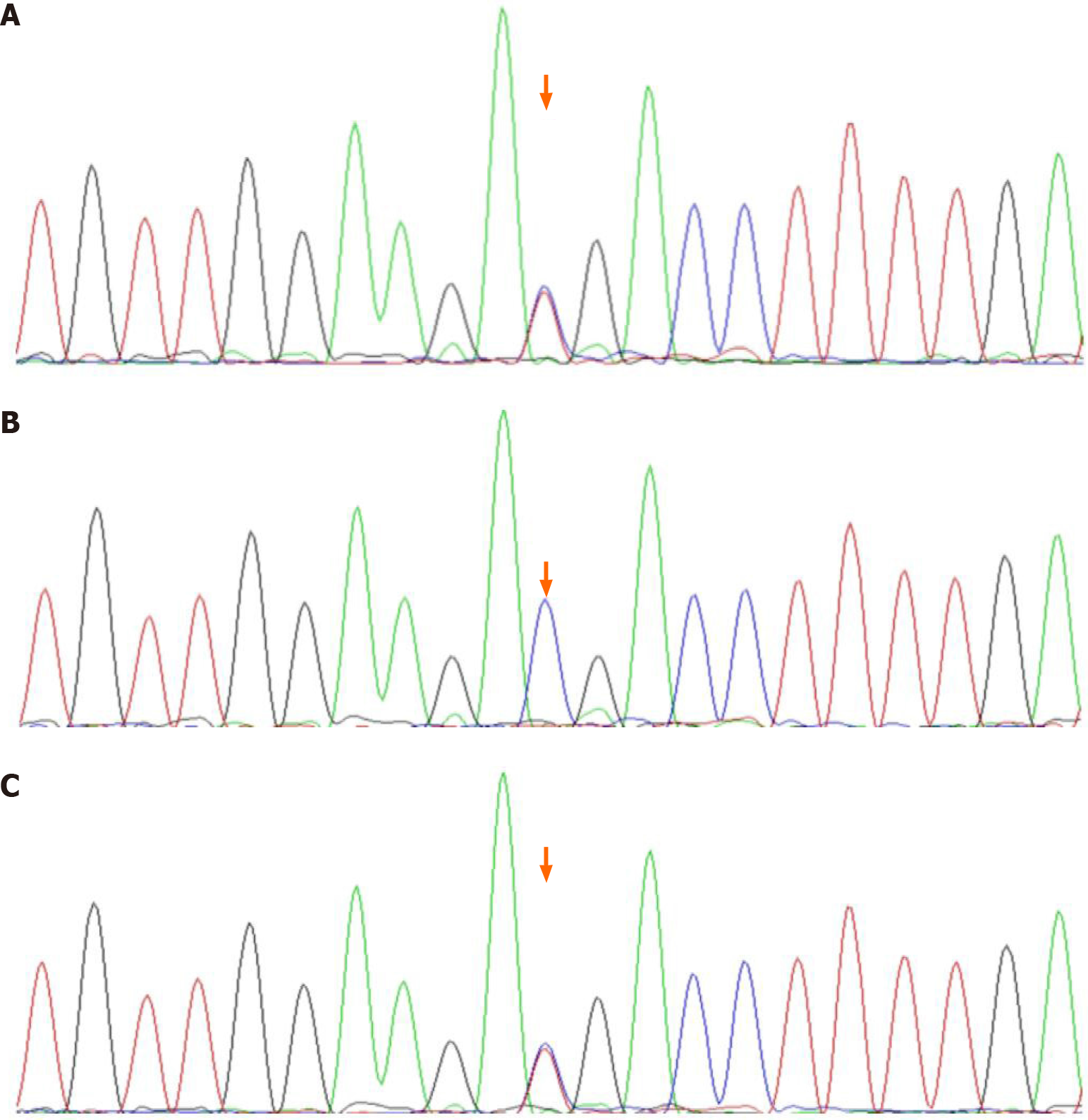
Vascular ultrasonography showed multiple cord-like solid lesions in both lower limbs and right upper limb and solid lesions on the right side of the shallow portion of the retroperitoneal spine. Enhanced computed tomography of the thorax and abdomen showed multiple lesions beside the spine, suggesting the possibility of neurofibromatosis. No abnormality was found on head magnetic resonance imaging (MRI), and enhanced MRI of the entire spine and limbs showed multiple space-occupying lesions in the posterosuperior mediastinum, lower abdomen, and pelvic cavity beside the spine with significant enhancement; some of the lesions grew into the spinal canal. The muscles and muscular spaces of both upper limbs, buttocks, thighs, calves, and feet had multiple masses with significant enhancement. Based on the above results, thrombi were excluded, and neurofibromatosis was suspected. Ophthalmic examination showed no iris hamartoma (Lisch nodule); evaluation of growth and development revealed development of motor function at 2 mo, social adaptation at 1 mo, and intelligence at 2 mo, with delayed development indicators; normal brainstem auditory evoked potential in both ears. No abnormalities were noted on tandem mass spectrometry of blood and urine. Gene sequencing analysis and validation of the child and his parents showed a heterozygous mutation of the tumor suppressor gene (NF1) c.4537C>T. Further pedigree validation showed that the mutation originated from the mother of the child (Figure 4).
On the basis of the clinical characteristics, imaging results, and genetic examination of the child, the diagnosis was NF1.
No special treatment has been provided.
No change has occurred in the 1-mo follow-up until the present.
The child had café-au-lait spots and pigmentation upon birth and had a family history of similar conditions, but the parents did not pay attention to these symptoms. This time, he was brought to the hospital because of lower limb swelling and was definitively diagnosed with NF1 after a short period of exclusion of thrombosis.
NF1 is a clinical syndrome caused by mutation of the pathogenic gene NF1. NF1 is mainly characterized by café-au-lait spots on the skin, multiple neurofibromas, hamartomas, and bone abnormalities[2]. It has been reported that about 16% of patients with NF1 have hypertension[3]. There have also been cases with infantile spasm as the first symptom[1] and cases showing learning difficulties. Uncommon symptoms include reticuloneurofibromas, optic nerve gliomas and other central nervous system gliomas, malignant peripheral nerve sheath tumors[4], precocious puberty, short stature, periodic abdominal pain, urogenital system abnormalities, and hematologic tumors[5].
This infant had multiple café-au-lait spots, axillary freckles, multiple neurofibromas, and a family history, which met the clinical diagnostic criteria of NF1[6]. Genetic examination provides an important basis for the diagnosis of this disease. The mutation types of the NF1 gene were diversified, and there were no hot spots[4].Currently, there are more than 2600 different NF1 genetic mutation points in the Human Gene Mutation Database[7]. Although the NF1 mutant spectrum was clearly defined as missense/nonsense (27.7%), splicing (16.3%), microdeletion (26.9%), microinsertion (11.1%), total deletion (> 20 bp; 13.3%), total insertion (> 20 bp; 2.0%), and complex rearrangement (0.6%), there is no evidence of any local mutant cluster in NF1[8]. This patient’s gene report showed a heterozygous mutation of NF1 exon 34, c.4537C>T. The cytosine changed to a thymine at nucleotide 4537, resulting in the nonsense mutation of amino acid (p.R1513X), which is a pathogenic mutation. The frequency in the normal population database is 0.0000082, which is a low frequency variation. To the best of our knowledge, this is the first report of such a case of NF1 in China. It was confirmed by pedigree validation that the variation originated from the mother of the child.
At the time of diagnosis, the patient was only 3 mo old, which is the youngest case reported in China. Early gene diagnosis plays an important role in NF1. The disease has a progressive development process, with mild clinical symptoms in infancy and childhood; with increase in age, other clinical symptoms may appear[1]. However, this patient had multiple neurofibromas at the age of 3 mo, and the growth of the tumors and disease progression were fast, which was rare and required attention. Most of the tumors are benign with a good prognosis.
At present, there is no effective treatment plan for NF1, and the treatment mainly focuses on genetic counseling, early detection of treatable complications, and symptomatic treatment[9]. Although the patient had multiple neurofibromas, there were no other typical symptoms and complications, except skin manifestations. Regular follow-up is needed to identify and systematically address related complications in time.
Early clinical diagnosis and prenatal diagnosis are very important, which requires the development and clinical application of the gene diagnosis research. Therefore, it is of great significance to provide genetic counseling and eugenic guidance for the parents of children[10].
Manuscript source: Unsolicited manuscript
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tomita Y S-Editor: Zhang H L-Editor: Filipodia P-Editor: Liu JH
| 1. | Li Q, Zhang YQ. Neurofibromatosis type I with infantile spasm as initial symptom: a case report and literature review. Ya Zhou Er Ke Bing Li Yan Jiu. 2019;7:21-25. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Lu XG, Han CX, Hu Y, Chen L, Huang TS, Wen JL, Liao JX. A rare NF1 gene mutation in neurofibromatosis type I. Zhongguo Xiaoer Jijiu Yixue. 2014;21:336. |
| 3. | Wei LY, Gong CX, Cao BY, Wu D. Neurofibromatosis type I with hypertension as its main manifestation: a case report and literature review. Linchuang Erke Zazhi. 2018;36:587-589. [DOI] [Full Text] |
| 4. | Liu Y, Yuan YH, Ma MS, Wang W, Qiu ZQ. Clinical Analysis of 8 cases of neurofibromatosis type I caused by NF1 gene mutation. Linchuang Erke Zazhi. 2016;34:819-824. [DOI] [Full Text] |
| 5. | Zhou L, Wu HS. New progress in clinical and monitoring of neurofibromatosis type I in Children. Zhonghua Shiyong Erke Linchuang Zazhi. 2000;15:355-356. [DOI] [Full Text] |
| 6. | Wu XR, Lin Q. Basis and Clinical Practice of Pediatric Neurological Diseases. Second Edition Beijing: People's Medical Publishing House, 2009: 920-922. |
| 7. | Messiaen LM, Callens T, Mortier G, Beysen D, Vandenbroucke I, Van Roy N, Speleman F, Paepe AD. Exhaustive mutation analysis of the NF1 gene allows identification of 95% of mutations and reveals a high frequency of unusual splicing defects. Hum Mutat. 2000;15:541-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Stenson PD, Mort M, Ball EV, Evans K, Hayden M, Heywood S, Hussain M, Phillips AD, Cooper DN. The Human Gene Mutation Database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Hum Genet. 2017;136:665-677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 852] [Cited by in RCA: 981] [Article Influence: 122.6] [Reference Citation Analysis (0)] |
| 9. | Zeng Y, Xiong F, Hu H. A case of urogenital neurofibromatosis in female infants. Zhonghua Erke Zazhi 2013; 51: 865-866. . [DOI] [Full Text] |
| 10. | Sun ZH, Li M, Guo YY, Yao ZR. Genetic diagnosis of sporadic neurofibromatosis type 1 with cafe-au-lait spots as the only presentation in a child. Zhonghua Pifuke Zazhi. 2013;46:511-512. [DOI] [Full Text] |