Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5670
Peer-review started: June 8, 2020
First decision: September 13, 2020
Revised: September 17, 2020
Accepted: September 26, 2020
Article in press: September 26, 2020
Published online: November 26, 2020
Processing time: 170 Days and 6.2 Hours
Biliary cystadenoma (BCA) is a rare benign tumor, accounting for only 5% of reported cystic lesions of the liver. Given its potential for malignancy and high rate of recurrence, surgical resection is the preferred treatment. Therefore, early and accurate preoperative diagnosis is critical to the choice of treatment. We here report the first male case of BCA in our hospital, diagnosed by our team and confirmed by pathological biopsy. This article aims to improve the understanding of this disease and help make a correct diagnosis to better manage it.
A 58-year-old man with irregular abdominal discomfort came to our clinic and was found to have a distended abdomen during physical examination. Computed tomography and magnetic resonance imaging both showed a huge cystic mass in the liver. The patient underwent left hepatic lobectomy, cholecystectomy, and liver cyst fenestration, and most of the masses had decreased in size as of the 6-mo follow-up. The pathological diagnosis was consistent with BCA, and no recurrence was detected after the surgery. BCA occurred mainly in middle-aged women. To the best of our knowledge, this patient is the 11th male case of BCA reported in the literature.
The combination of magnetic resonance imaging and magnetic resonance cholangiopancreatography is of great significance for the early accurate diagnosis of the disease and the choice of surgical methods.
Core Tip: We report the first male case of biliary cystadenoma (BCA) in our hospital confirmed by pathology, review its clinical, imaging, and pathological features, and compare them to those of past cases. There are certain image features of BCA. The combined use of magnetic resonance imaging and magnetic resonance cholangiopancreatography improves the rate of detection of BCA and facilitates the identification of hepatic cysts.
- Citation: Xu RM, Li XR, Liu LH, Zheng WQ, Zhou H, Wang XC. Intrahepatic biliary cystadenoma: A case report . World J Clin Cases 2020; 8(22): 5670-5677
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5670.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5670
Biliary cystadenoma (BCA) is a rare benign tumor that is difficult to distinguish from other types of hepatic cystic disease[1,2]. Given its potential for malignancy and high recurrence rate (less than 10%)[1], surgical resection is the preferred treatment. Therefore, early and accurate preoperative diagnosis is critical to the choice of treatment. Diagnosis of early-stage BCA is challenging because of the diversity of clinical manifestations and the lack of accordant imaging findings. This article reports a case confirmed by pathology, review its clinical, imaging, and pathological features, and compare them to those of past cases. The purpose of this work is to improve the understanding of this disease and help make a correct diagnosis to better manage it.
A 58-year-old man with intermittent abdominal discomfort lasting several months came to our clinic.
At a local hospital, abdominal ultrasound (US) revealed a huge liver cyst.
The patient had no previous medical history.
He was healthy without a personal or family history of tumors.
During a physical examination, he was found to have a distended abdomen and no palpable masses.
Laboratory tests revealed mild leukocytosis (11 × 109/L), with normal hematocrit and platelet count. Prothrombin and partial thromboplastin times were within normal limits except for a slight elevation of hepatic enzyme; his carbohydrate antigen-199 level was within the normal range.
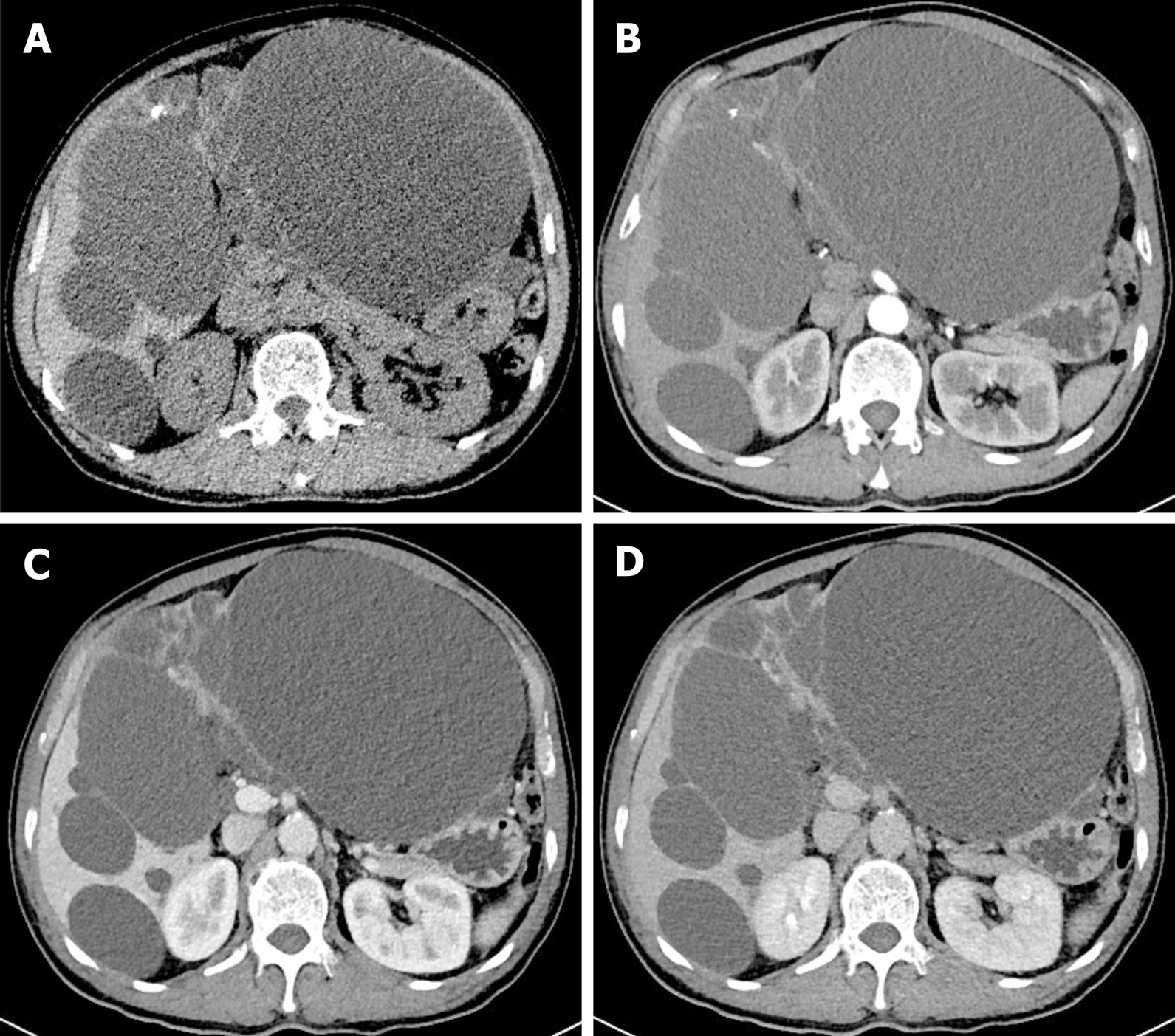
Multiple hypo-attenuating shadows in the liver were observed on abdominal computed tomography (CT) images, the largest of which measured 18.9 cm × 14.1 cm in size and occupied the left lateral lobe of the liver (Figure 1A), with a CT value about 0 HU and no enhancement (Figure 1B-D). Cystic masses of varying sizes with thin septa and nodular calcification were observed in the left lobe of the liver (Figure 1A). No nodular components or septum-like structures were identified in the cystic lesions of the right lobe of the liver (Figure 1A). The internal septa were mildly enhanced after intravenous administration of contrast medium (Figure 1C and D). It was diagnosed as polycystic liver based on CT features.
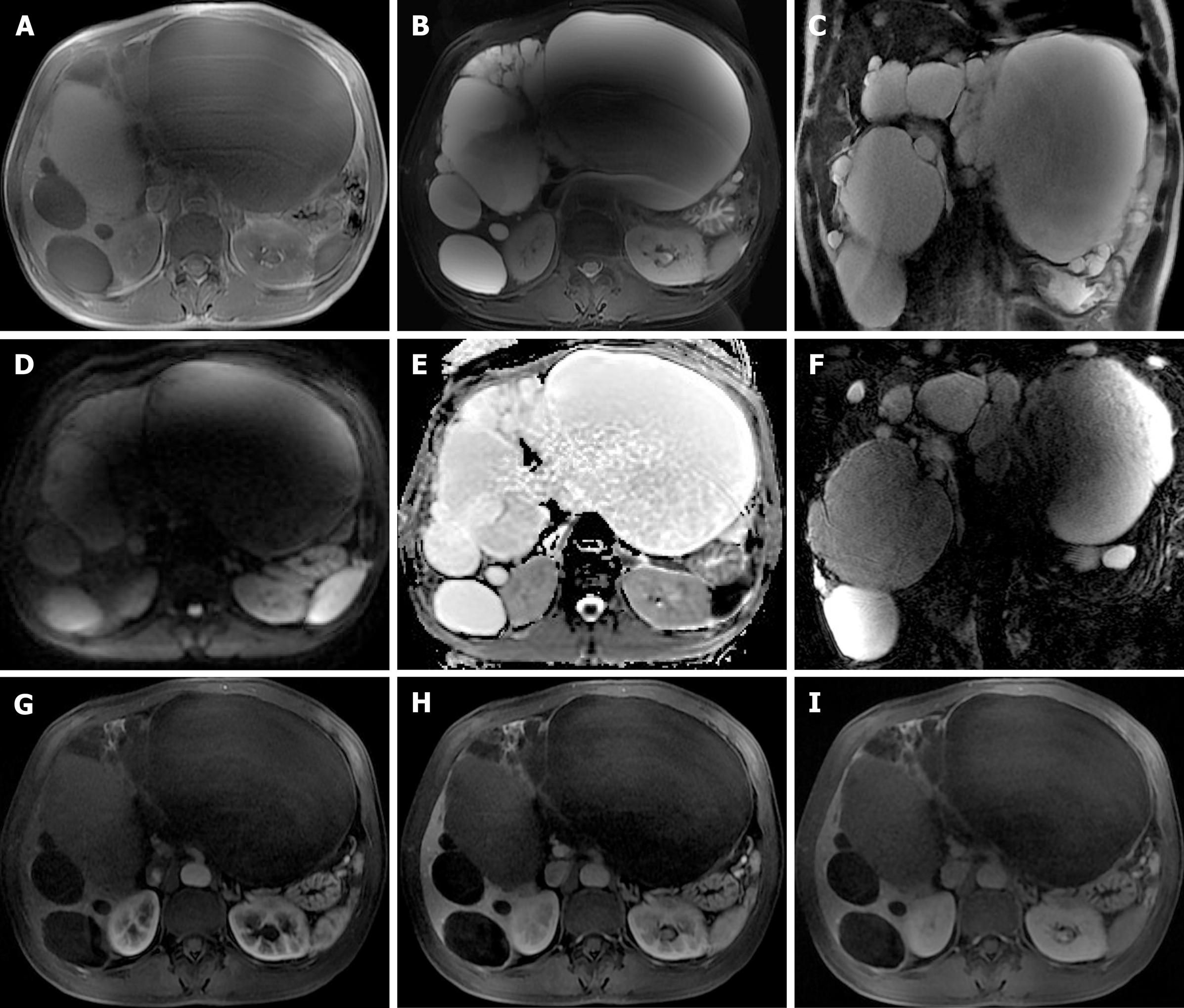
Magnetic resonance imaging (MRI) revealed a large cystic lesion measuring approximately 18.3 cm × 13.5 cm × 19.3 cm, originating from the left lobe of the liver. The signal of the cystic fluid was hypointense on T1-weighted images (T1WI) (Figure 2A) and hyperintense on T2-weighted images (T2WI) (Figure 2B and C). A circular lesion in the left inner lobe measuring 3.2 cm × 2.0 cm showed hyper-intensity on both T1WI and T2WI (Figure 2A and B). Multiple cystic lesions in the right lobe of the liver showed low signals on T1WI and apparent high intensity signals on T2WI delineated from the surrounding liver without enhancement (Figure 2A-C). Diffusion weighted imaging (Figure 2D) and apparent diffusion coefficient (Figure 2E) map showed no abnormal signal in the liver. On contrast-enhanced TIWI, there were internal separations in the capsule wall and significantly enhanced vascular shadow between the lesions (Figure 2G-I). Magnetic resonance cholangiopancreatography (MRCP) showed diffuse dilatation of the biliary tree (Figure 2F). According to MRI manifestations, cystadenoma was diagnosed.
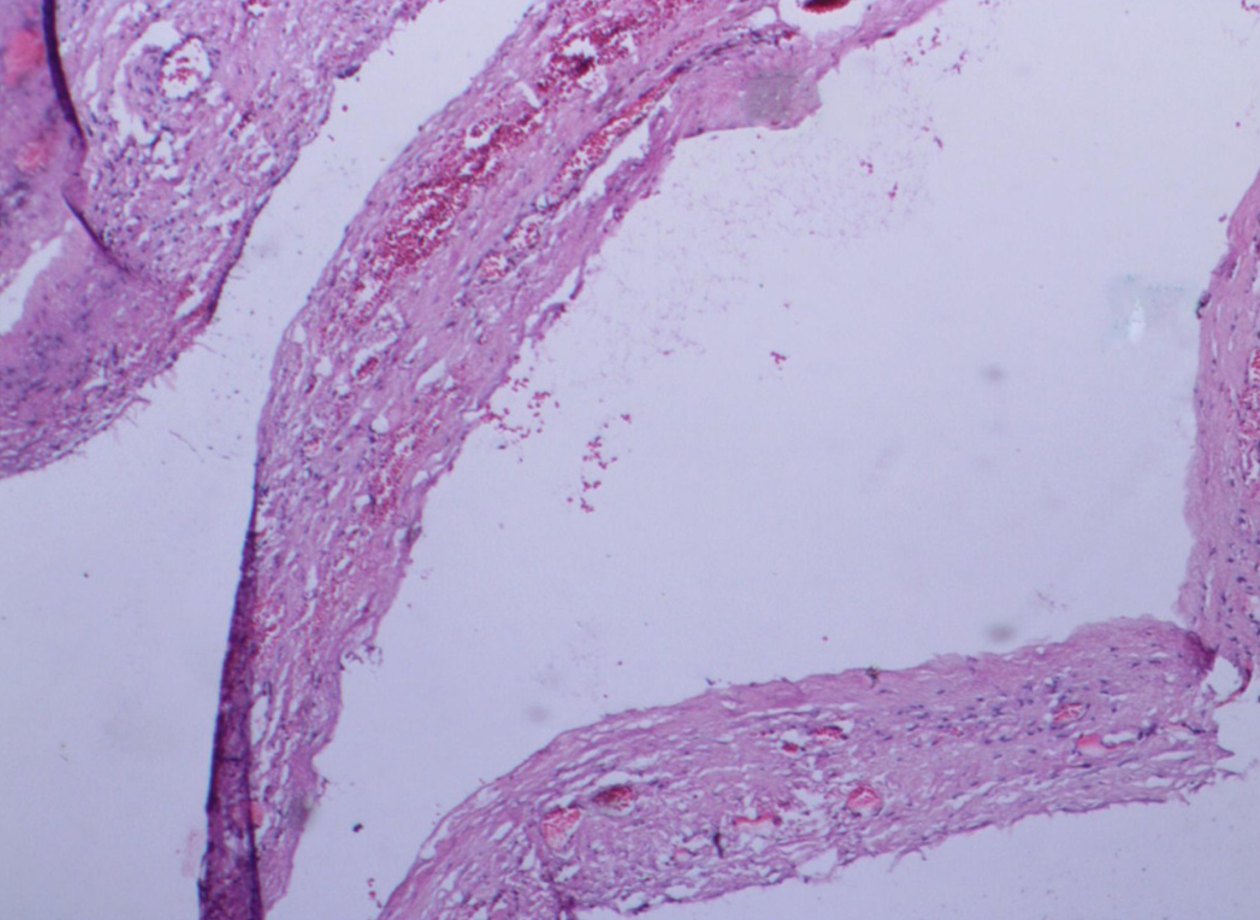
Pathologically, the cystic wall consisted of a single layer of cuboidal and columnar epithelial cells (Figure 3), and the capsular wall was attached to atrophic hepatocytes, with fibrosis, calcification, and inflammatory cell infiltration. There was no evidence of ovarian-like stromal invasion. It was consistent with a BCA.
The patient underwent left hepatic lobectomy, cholecystectomy, and liver cyst fenestration. Grossly, the surface of the liver was covered with cystic masses, and the left lateral lobe of the liver had become completely cystic. There were many large blood vessels in the capsule wall. The cystic lesions sowed blurred outlines into the adjacent hepatic parenchyma, in which about 4300 mL of transparent fluid was aspirated. On the premise of maximizing the resection of the lesion to prevent a recurrence, and meeting the patient’s requirement for preserving part of the liver function, the surgeon chose this procedure.
The patient recovered well and was discharged from the hospital on postoperative day 30. New MRI scan revealed that most of the masses had decreased in size as of the 6-mo follow-up.
BCA is a cystic benign tumor originating from the epithelia of the intrahepatic or extrahepatic biliary ducts[3]. It is also known as hepatobiliary cystadenoma. It has been reported that BCAs have a slight predilection for the right lobe of the liver[3,4], accounting for less than 5% of all of the cystic lesions of the liver[5,6]. The majority of tumors occurred in middle-aged women, with a median age of 50 years[6,7]. To our knowledge, the patient described here is the 11th male case of BCA[6,8]. BCAs range in size from 1.5 cm to 30 cm.
BCA is usually asymptomatic, and the tumor is usually already sizable at the time of observation[5,7]. Patients with symptoms usually present with upper abdominal pain and distension, abdominal mass, anorexia, and nausea or vomiting. Jaundice may occur in larger tumors due to cyst compression of the common bile duct as well as minor vena cava obstruction and thrombosis[5,7,9]. More rarely reported manifestations include intracapsular hemorrhage and rupture from secondary bacterial infections[5,7]. Hepatic cysts that recur after surgical fenestration should be considered likely BCA[5,10].
BCA may be unilocular or multilocular, and both grow slowly[8]. Laboratory results in most BCA patients are normal, but levels of serum liver enzyme and bilirubin may be slightly elevated. Serum alpha-fetoprotein, CA-199, CA-125, and carcinoma embryonic antigen levels are usually distributed within the normal range[4,6,11]. Recently, it has been reported that the level of CA-199 in the cyst fluid may increase, and this can make it easier to diagnose BCA[4,5], but cystic fluid analysis is not a diagnostic tool[8].
Histologically, the cystic walls are arranged from cuboidal to columnar epithelium and ovarian-type stroma is seen subepithelially, which is exclusively present in women and is immunoreactive for estrogen and progesterone receptors[12]. In tumors in males, the supporting stroma is composed of fibrous tissue[4]. The patient lacked ovarian-type stroma but instead had fibrous stroma.
We searched the pertinent work in the database (time frame from 1988 to 2019, keywords: Biliary cystadenoma, magnetic resonance imaging, magnetic resonance cholangiopancreatography, computed tomography, and biliary cystadenocarcinoma) and conducted a literature review. A thorough review of the literature is provided in Table 1 and 2.
| Ref. | Case number | Mean age (yr) | Sex | Clinical manifestation | CA199 (iu/mL) | Treatment |
| Lewis et al[9], 1988 | 15 | 41 | F (13), M (2) | Abdominal pain (12), sepsis/cholangitis (4), lower-extremity edema (2), abdominal mass (2), no symptom (2) | NA | Left lateral segmentectomy (2), right trisegmentectomy (1), liver transplant (1), wedge resection of cyst (2), central hepatic resection (1), left trisegmentectomy (2), right hepatic lobectomy (2), marsupialization of cyst (1), hepatic cystectomy (3) |
| Stoupis et al[3], 1994 | 1 | 37 | F | Jaundice, pruritus | NA | Mass resection |
| Hara et al[11], 2001 | 1 | 48 | F | No symptom | Normal | Left hepatectomy |
| Kazama et al[6], 2005 | 1 | 68 | M | Abdominal fullness, nausea, vomiting | NA | Right hepatic lobectomy |
| Lewin et al[15], 2006 | 6 | 55 | F (6) | Abdominal pain (3), jaundice (2), no apparent symptom (1) | Normal (6) | Mass resection (6) |
| Yu et al[8], 2008 | 2 | 63.5 | M (2) | Abdominal pain (2) | 107 (1), normal (1) | Left lobectomy plus cholecystectomy (1), resection was not performed due to the metastatic disease |
| Delis et al[5], 2008 | 4 | 51 | F (4) | Abdominal pain, occasionally vomiting | Increased (4) | Left hepatectomy (3), right hepatectomy and left hepaticojejunostomy (1) |
| Romagnoli et al[13], 2011 | 1 | 53 | F | Obstructive jaundice | Normal | Liver transplant |
| Gonzalez et al[1], 2009 | 1 | 32 | F | Abdominal pain, jaundice, diarrhoea | 43 | Left hepatectomy |
| Sang et al[10], 2011 | 19 | 44.2 | F (17), M (2) | Abdominal pain (9), vomiting (1), palpable abdominal mass (1), jaundice (1), no symptom (10) | Increased (9) | Cyst enucleation (3), laparoscopic fenestration (1), right hemihepatectomy (1), mentectomy (2), left lateral sectionectomy (2), left medial sectionectomy (1), right segmentectomy (1), right anterior sectionectomy (1), right posterior sectionectomy (1) |
| Williamson et al[7], 2013 | 3 | 45.3 | F (3) | No symptom (1), abdominal pain (1), epigastric mass (1), hepatic cyst infection (1) | NA (1), increased (2) | Wedge resection (1), surgery (1), left hemihepatectomy (1) |
| Yang et al[4], 2013 | 1 | 57 | F | Intermittent abdominal pain | Normal | Left hepatic lobectomy |
| Liu et al[2], 2018 | 1 | 59 | F | Jaundice, palpable abdominal mass | Increased | Left hemihepatectomy |
| This case | 1 | 58 | M | Abdominal fullness | Normal | Left hepatic lobectomy, cholecystectomy, liver cyst fenestration |
| Ref. | Location | Imaging findings (US, CT, MRI, MRCP) |
| Lewis et al[9], 1988 | Left lobe (5), right lobe (8), porta hepatis (1), central (2) | US demonstrated fluid-filled lesions with internal septation and nodularity consistent with the papillary infoldings. CT revealed a smooth, thick walled cyst with thin internal septations |
| Stoupis et al[3], 1994 | Right lobe | CT showed a large septate, hypoattenuating mass with enhancement of the septations. MRI showed multilocular lesion with different signal intensities in the locules |
| Hara et al[11], 2001 | Left lobe | CT demonstrated a multiple low density mass. MRI showed multilocular cysts, with homogeneous signals on T1WI and T2WI |
| Kazama et al[6], 2005 | Right lobe | CT demonstrated a giant, well-circumscribed, low-density mass with internal septa |
| Lewin et al[15], 2006 | Left lobe | MRI revealed a homogeneous cystic lesion in the six BCAs. Three BCAs showed a hypointensity on T1WI and an isointensity in the other three. A fluid/fluid level consistent with internal hemorrhage was found in one BCA. MRCP showed ductal dilatation upstream to cystic lesion in two BCAs |
| Yu et al[8], 2008 | Left lobe | MRI showed a cystic mass in the left hepatic lobe. MRCP showed diffuse dilatation of the biliary tree with different signals in the bile ducts |
| Left lobe | CT revealed a large cystic mass with septations and multiple papillary projections | |
| Delis et al[5], 2008 | Left lobe (3), right lobe (1) | US revealed various sizes of cysts with septations and infolding projections originating from the cystic wall. CT revealed cysts with internal septations and mural nodules with contrast enhancement |
| Romagnoli et al[13], 2011 | Segments 4 and 8 | CT and MRI revealed a cystic mass with septations in its caudal portion, lying on the Glissonian bifurcation, causing dislocation of the portahepatis and compression of the main right and left hepatic ducts with peripheral bile duct dilatation |
| Gonzalez et al[1], 2009 | Left lobe | CT showed a large water density mass with internal septa and without calcifications |
| Sang et al[10], 2011 | CT and MRI revealed fluid-containing, well-defined, lobulated, multilocular, thick walled cystic masses with enhanced internal septation and convex papillae | |
| Williamson et al[7], 2013 | Left lobe (2), central lobe (1) | CT confirmed a large hepatic cyst with calcification. MRI showed a cystic lesion containing proteinaceous fluid or blood, which had a solid component with papillary projections |
| Yang et al[4], 2013 | Left lobe | CT revealed a hypoattenuating shadow with internal septae and enhanced after intravenous administration of contrast medium |
| Li et al[2], 2018 | Left lobe | CT revealed a hypoattenuating shadow with slight enhanced internal septations. Fluid on MRI revealed a low signal intensity on T1WI and high signal intensity on T2WI without enhancement |
| This case | CT revealed multiple sizes of hypoattenuating shadows with nodular calcification and internal septations and slight enhancement. MRI showed that internal septation separated the fluid-filled spaces and was enhanced |
Although BCAs are considered benign cystic tumors of the liver, the risk of recurrence and malignancy remains high[4], and they may develop into biliary cystadenocarcinoma (BCAC). Correct diagnosis and timely surgical resection are critical for treatment[13]. However, due to the lack of specific clinical manifestations and laboratory tests, the differential diagnosis of BCA and other cystic lesions in the liver is difficult. CT and MRI should be performed when hepatic cystic lesions, especially large hepatic cysts, are detected by US. On CT images, BCA was large in volume and well encapsulated. The density of each cyst may be different, and intracystic hemorrhage may increase its density and create an interface between liquid and gas fluids[14]. Part of the cystic wall may be associated with wall nodules and septa, and the number of nodules varies with a small amount of calcification on the walls or septa[14]. The wall of BCA is thinner and more regular than that of BCAC, while the existence of solid nodular masses or major calcifications in the walls and the septa suggests malignancy[6]. Convex papillae can be observed on the septation, although it is more common in BCAC[4].
According to MRI, BCA mostly appears as a hypointense lesion on T1WI and hyperintense cystic fluid on T2WI, whereas the signal intensity may vary depending on the properties of the cyst fluid, protein concentration, and intracapsular hemorrhage[15]. The internal separation of BCA is characterized by low signal intensity on T2WI. The capsule wall, separation, and nodules showed gradual and uniform enhancement on contrast-enhanced TIWI. MRCP is a suitable means of evaluating the relationship between lesions and bile ducts, providing information about any obstructed biliary tree[7,15], and intracapsular separation can also be observed[15]. Gadolinium-enhanced MRI combined with MRCP is an effective tool for the diagnosis of BCA and BCAC, but further studies are needed[8].
Typical manifestations of BCA from the literature were fluid-filled, well-defined, lobulated, multilocular, and thick septated cystic masses with enhanced internal septation and convex papillae. Preoperative diagnosis of this patient was based on these features. Total excision is strongly recommended for the patients, allowing a proper histological examination of the cyst to distinguish BCA and BCAC accurately and a detailed classification[10].
This article reports a case of BCA misdiagnosed as a liver cyst by ultrasound, suggesting that the differentiation of BCA from a large hepatic cyst is generally challenging. BCA should be suspected when hepatic cysts recur after surgery or other treatments. The use of MRI and MRCP in combination improves the detection rate of BCA and facilitates the identification of hepatic cysts. These can provide a basis for preoperative accurate diagnosis and help clinicians choose the optimal surgical procedure for complete resection of BCA.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karaca CA S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Gonzalez M, Majno P, Terraz S, Morel P, Rubbia-Brandt L, Mentha G. Biliary cystadenoma revealed by obstructive jaundice. Dig Liver Dis. 2009;41:e11-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Liu LS, Song T, Huang JW. Intrahepatic biliary cystadenoma: A case report and literature review. Zhongguo CT He MRI Zazhi. 2018;16:150-152. [DOI] [Full Text] |
| 3. | Stoupis C, Ros PR, Dolson DJ. Recurrent biliary cystadenoma: MR imaging appearance. J Magn Reson Imaging. 1994;4:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Yang ZZ, Li Y, Liu J, Li KF, Yan YH, Xiao WD. Giant biliary cystadenoma complicated with polycystic liver: a case report. World J Gastroenterol. 2013;19:6310-6314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Delis SG, Touloumis Z, Bakoyiannis A, Tassopoulos N, Paraskeva K, Athanassiou K, Safioleas M, Dervenis C. Intrahepatic biliary cystadenoma: a need for radical resection. Eur J Gastroenterol Hepatol. 2008;20:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Kazama S, Hiramatsu T, Kuriyama S, Kuriki K, Kobayashi R, Takabayashi N, Furukawa K, Kosukegawa M, Nakajima H, Hara K. Giant intrahepatic biliary cystadenoma in a male: a case report, immunohistopathological analysis, and review of the literature. Dig Dis Sci. 2005;50:1384-1389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Williamson JM, Rees JR, Pope I, Strickland A. Hepatobiliary cystadenomas. Ann R Coll Surg Engl. 2013;95:507-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Yu FC, Chen JH, Yang KC, Wu CC, Chou YY. Hepatobiliary cystadenoma: a report of two cases. J Gastrointestin Liver Dis. 2008;17:203-206. [PubMed] |
| 9. | Lewis WD, Jenkins RL, Rossi RL, Munson L, ReMine SG, Cady B, Braasch JW, McDermott WV. Surgical treatment of biliary cystadenoma. A report of 15 cases. Arch Surg. 1988;123:563-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Sang X, Sun Y, Mao Y, Yang Z, Lu X, Yang H, Xu H, Zhong S, Huang J. Hepatobiliary cystadenomas and cystadenocarcinomas: a report of 33 cases. Liver Int. 2011;31:1337-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Hara H, Morita S, Sako S, Dohi T, Iwamoto M, Inoue H, Tanigawa N. Hepatobiliary cystadenoma combined with multiple liver cysts: report of a case. Surg Today. 2001;31:651-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Weihing RR, Shintaku IP, Geller SA, Petrovic LM. Hepatobiliary and pancreatic mucinous cystadenocarcinomas with mesenchymal stroma: analysis of estrogen receptors/progesterone receptors and expression of tumor-associated antigens. Mod Pathol. 1997;10:372-379. [PubMed] |
| 13. | Romagnoli R, Patrono D, Paraluppi G, David E, Tandoi F, Strignano P, Lupo F, Salizzoni M. Liver transplantation for symptomatic centrohepatic biliary cystadenoma. Clin Res Hepatol Gastroenterol. 2011;35:408-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Song B, Liu Y, Tu WG, Wang L, Zhang Y, Shi QQ, Chen XY. Intrahepatic biliary cystadenoma and cystadenocarcinoma with spiral CT and pathological comparison. J Diagn Concepts Pract. 2014;13:94-97. |
| 15. | Lewin M, Mourra N, Honigman I, Fléjou JF, Parc R, Arrivé L, Tubiana JM. Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol. 2006;16:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 3.2] [Reference Citation Analysis (0)] |