Published online Nov 26, 2020. doi: 10.12998/wjcc.v8.i22.5632
Peer-review started: July 17, 2020
First decision: August 8, 2020
Revised: August 17, 2020
Accepted: October 12, 2020
Article in press: October 12, 2020
Published online: November 26, 2020
Processing time: 131 Days and 5.6 Hours
Acanthosis nigricans (AN), Leser–Trélat sign, and tripe palm are all skin diseases. To date, reports of these appearing as a paraneoplastic syndrome in a gastric cancer patient are quite rare.
We report the case of a 61-year-old man with darkened skin color in the face and torso with no obvious inducement after 1 year of treatment for Riehl’s melanosis. He had 40 brown maculopapular eruptions on his face and the top of his head with obvious itching. Papillary wart-like hyperkeratosis with dark brown pigmentation was also observed on both sides of the areola. He had papilloma-like lesions on the face, around the orbit, and on the neck. His bilateral palms had small, smooth, papillary projections with millet-like appearance. Histopathological examination of the skin showed that the patient was suffering from AN, tripe palms, and Leser–Trélat sign. Gastroscopy showed the patient’s cardia was affected, and pathological biopsy revealed that he had moderate-to-poorly differentiated adenocarcinoma. Computed tomography test results showed that his cardia wall had thickened. Based on these histological and skin characteristics, the patient was diagnosed with gastric cancer with AN, tripe palms, and Leser–Trélat sign.
Researchers should follow up on patients with malignant AN, Leser–Trélat sign, and tripe palms.
Core Tip: Acanthosis nigricans associated with malignant tumor is rare, and mainly occurs in middle-aged and elderly patients. Patients with malignant acanthosis nigricans accompanied by malignant tumor, Leser–Trélat sign, and tripe palms are even rarer. In light of this, references to the clinical features and pathology of various paraneoplastic syndromes, such as malignant acanthosis with Leser–Trélat sign and tripe palms, are very limited.
- Citation: Wang N, Yu PJ, Liu ZL, Zhu SM, Zhang CW. Malignant acanthosis nigricans with Leser–Trélat sign and tripe palms: A case report. World J Clin Cases 2020; 8(22): 5632-5638
- URL: https://www.wjgnet.com/2307-8960/full/v8/i22/5632.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i22.5632
Acanthosis nigricans (AN) was first discovered and named by Pollitzer and Jaurorky in l891. The disease features skin keratosis characterized by skin pigmentation, hyperkeratosis, velvet-like hyperplasia, and the formation of verrucous vegetations. It is more likely to occur in areas where the skin wrinkles, such as the armpit, back, neck, cubital fossa, groin, and labia[1]. The disease is mostly related to metabolic disorders, genetic and autoimmune factors, iatrogenic diseases, drug metabolism, etc. Its etiology is not yet clear, and it can be divided into non-malignant and malignant cases. Non-malignant cases can occur at any age[2,3]. Malignant AN, also known as paraneoplastic AN, mainly occurs in middle-aged and elderly patients. It is often accompanied by malignant tumors, and its symptoms include the rapid development of skin lesions and obvious pigmentation[4]. Not only is thickened skin accompanied with skin lesions, but typical skin lesions are also found at the junction of the mucous membrane and skin mucosa. Patients also have papilloma-like hyperplasia around the eyes and lips, and their nails become brittle and have longitudinal crests. Most patients show characteristic “velvet-like” changes in the palmoplantar, and their skin lesions are often accompanied by itching or irritation[5].
Multiple seborrheic senile keratoses (Leser–Trélat sign) are a paraneoplastic syndrome of the skin first reported by Edmund and Ulisse. It manifests as the sudden appearance of seborrheic keratosis or as a sudden increase in skin lesions of the original seborrheic keratosis. Of the tumors that often occur with the disease, one-third are gastrointestinal adenocarcinomas and one-quarter are lymphoproliferative diseases. Pregnancy and some benign tumors can also have the syndrome[6].
Tripe palms was first reported and named by Breathnach in 1963. It is characterized by a wrinkled surface of the palm similar to that of the foregut of cattle, which gives it its name. It has been referred to as acanthosis palmaris, hyperkeratosis palmaris, acanthosis palmaris nigra, and keratoma palmaris. It can exist alone or in combination with AN, with more than 50% of cases associated with lung and gastric cancers. The histological diagnosis is mainly of cutaneous acanthosis, hyperkeratosis, and inflammatory mucin deposition around the blood vessels[7].
To date, most cases of AN have been reported without paraneoplastic syndrome, and cases of malignant AN with Leser–Trélat sign and tripe palms are extremely rare. Because of this, the clinical features and pathological data of malignant AN with multiple paraneoplastic syndromes are very limited.
A 61-year-old male patient presented with itching. His face and torso had hyperpigmented a year before he presented with this symptom, and he had been experiencing upper abdominal pain for more than 1 mo. Nonetheless, he did not have abdominal distention, hematemesis, black stool, anorexia, anemia, or other related positive symptoms and signs.
The patient had gone to his local hospital, where he was diagnosed with Riehl’s melanosis. After 1 year of treatment, his condition did not improve. He later went to the Fourth Military Medical University’s Xijing Hospital for further evaluation and was diagnosed with gastric cancer. After this, he visited our hospital for further evaluation.
There was no obvious abnormality in any past illness.
The patient had smoked one pack of cigarettes a day, on average, for more than 20 years, but had quit 8 years previously. In addition, he denied having any other related diseases and family history.
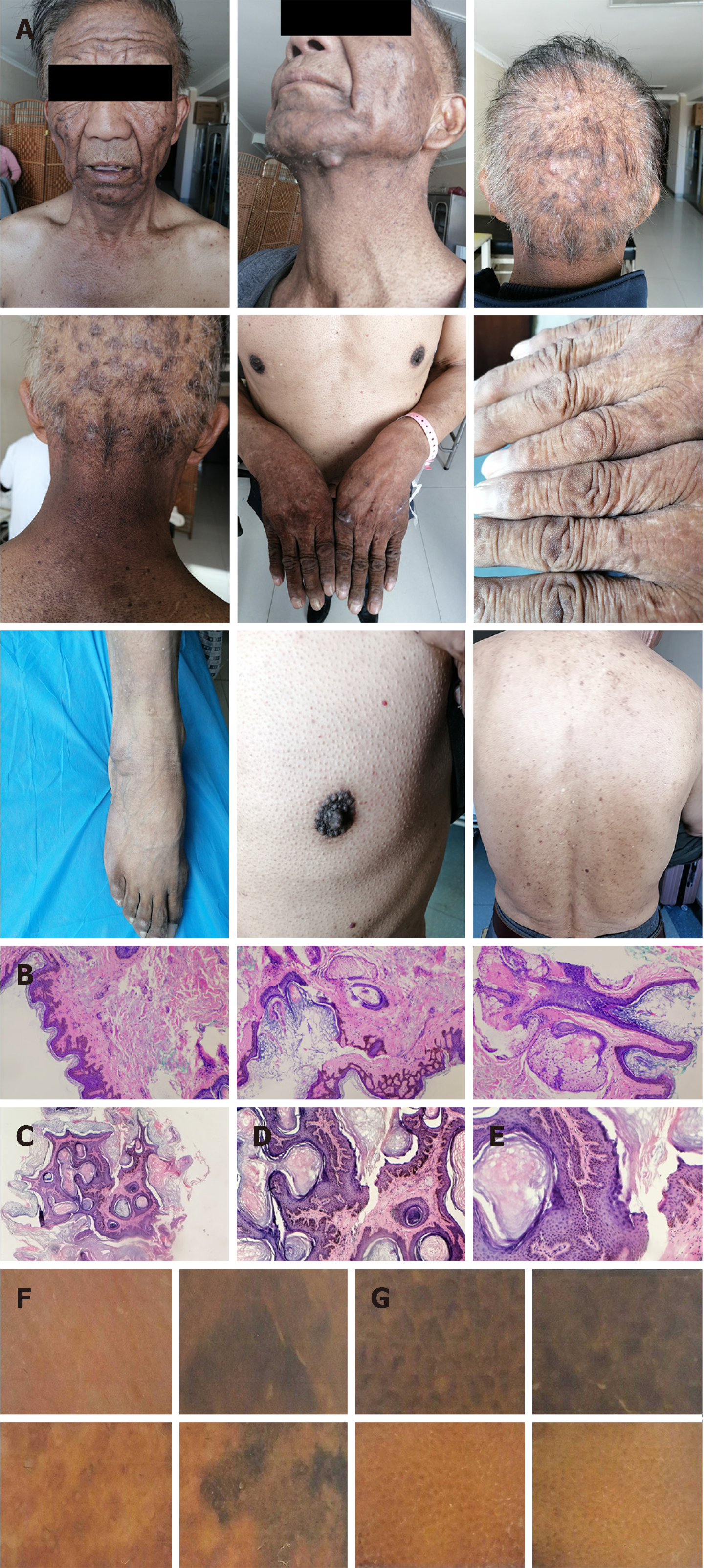
In an examination of the skin, the patient's face, neck, chest, back, and head were found to have more than 40 rice-to-soybean sized, flat brown maculopapular papules that were round or oval with a rough and greasy surface. The patient's face and neck were hyperpigmented, with papilla and areola verrucous hyperkeratosis and dark brown pigmentation. There were papilloma-like lesions on his face, around the orbit, and on the neck. His palms on both sides had scattered millet-like small and smooth papillary bulges that had a tripe palm-like appearance (Figure 1). The patient tested positive for epigastric tenderness; however, he did not exhibit other related positive signs and symptoms.
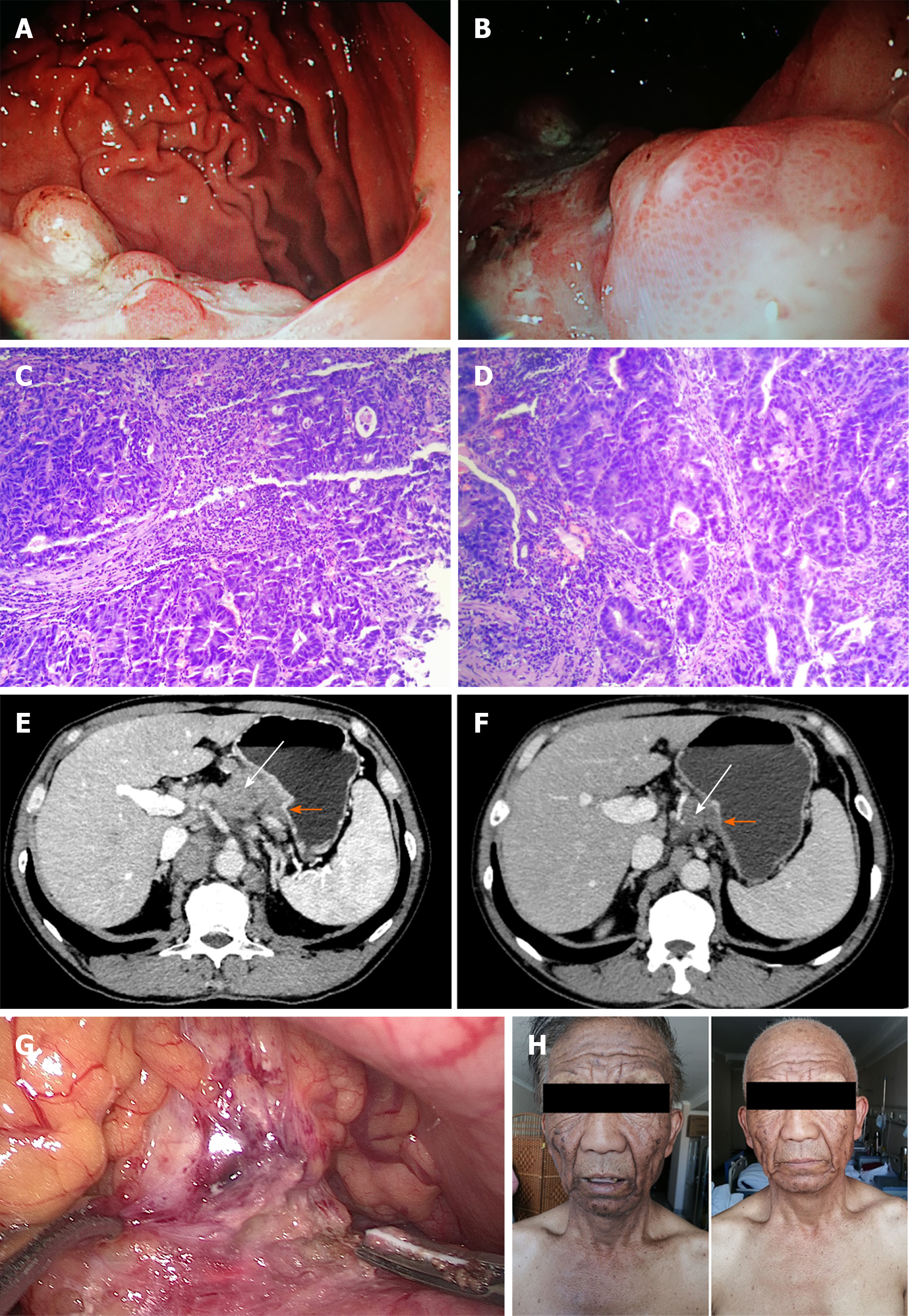
Laboratory results revealed the patient's blood routine, urine routine, stool routine, extractable nuclear antigen spectrum, biochemistry, fasting blood glucose, erythrocyte sedimentation rate, immunoglobulin, complement, and thyroid function (triiodothyronine, thyroxine, thyroid-stimulating hormone) test results to be normal. His blood pressure (120/70 mmHg) and heart rate (78 beats/min) were normal. Tumor marker carcinoembryonic antigen (CEA) was detected at 25.43 ng/mL (reference value 0.0-5.0 ng/mL). A biopsy of his neck skin showed epidermal hyperkeratosis, basal cell hyperplasia, pigmentation, and dermal papilla protrusions (Figure 1). There was a flat brown maculopapular rash on his face, basal cell papilloma, hyperpigmentation, and hyperkeratosis (Figure 1). A microscope examination of the palm and face skin showed gray–brown papillary hyperplasia with consistent distribution in the lesions, along with some diffuse dark brown to dark-gray pigmentation with slight scaly dandruff (Figure 1). Gastroscope biopsy pathology showed medium-low differentiated adenocarcinoma in the gastric cardia and body (Figure 2). Considering these clinical and pathological features, a final diagnosis of AN, gastric cancer (CT3N3bMx), Leser–Trélat sign, and tripe palms was reached. After three cycles of chemotherapy, the patient’s tumor marker CEA had lowered to 3.48 ng/mL. During surgery, it was found that the tumor had invaded the pancreas (Figure 2).
Gastroscopy of the upper part of the stomach under the patient’s cardia showed a large mucous membrane bulge near the posterior wall with an uneven surface and large areas of ulceration (Figure 2). A diagnosis of cardiac gastric cancer was made. Computed tomography examination showed a thickened and strengthened wall of the cardia with many swollen lymph nodes around it, leading cardia cancer to be considered, (Figure 2). We suspected that the affected area had a malignant tumor after the relevant examination.
A final diagnosis of AN, gastric cancer (CT3N3bMx), Leser–Trélat sign, and tripe palms was reached.
After admission, considering the late stage of the patient and the high risk of direct surgery, we administered three cycles of neoadjuvant chemotherapy preoperatively to shrink the tumor lesion and reduce the clinical stage[8]; then, we further evaluated the need for surgical treatment. The patient received 135 mg/m2 paclitaxel, 135 mg/m2 oxaliplatin, and oral tegafur capsules twice a day, from days 1-14. After three cycles of neoadjuvant chemotherapy along with this regimen, we performed laparoscopic assisted total gastrectomy. During the procedure, it was found that the tumor had invaded the pancreas. The patient’s family refused to allow further surgical treatment, thus a cycle of palliative chemotherapy was performed after the operation.
After three cycles of chemotherapy, the patient’s skin lesions partially improved (Figure 2). However, 6 mo after the end of chemotherapy, the lesions worsened again. The patient was subjected to imaging of the chest, abdomen, and pelvis, as well as gastroscopy, every 3 mo. It was found that the tumor did not undergo abdominal metastasis, which is still being followed up.
At present, the etiology of AN is not yet clear. Some people consider that the occurrence of malignant tumors is related to growth-promoting factors, including platelet-derived growth factor, and epidermal growth factor[9]. In addition, hormones released by tumors can stimulate an increase in melanocyte-stimulating hormones, which in turn trigger the growth of melanocytes, fibroblasts, and keratinocytes[10]. AN can be divided into benign and malignant forms. Non-malignant tumors can occur at any age[2,3] and are mostly related to metabolic disorders, genetic and autoimmune factors, iatrogenic infections, and drug side-effects, among others. Malignant AN, also known as paraneoplastic AN, mainly occurs in middle-aged and elderly patients[4] . Not only is thickened skin accompanied with skin lesions in such cases, but typical skin lesions are also found at the junction of the mucous membrane and skin mucosa. Patients have papilloma-like hyperplasia around the eyes and lips, and their nails become brittle and have longitudinal crests. Most patients have characteristic "velvet-like" changes in the palmoplantar, and their skin lesions often itch or show symptoms of irritation. There are malignant tumors that manifest with accompanying skin lesions that are more likely to occur in patients with gastric adenocarcinoma (55%-61%)[10,11]. In 61% of patients, skin lesions and tumor occur at the same time, while 22% have tumor before the skin lesions, and 17% have skin lesions before the tumor[12]. As a paraneoplastic syndrome, AN has been seen to appear with Leser–Trélat sign, dermal papillomatosis, tripe palm, and other diseases, though diseases accompanied by AN, tripe palms, and Leser–Trélat sign rarely coexist in patients with single gastric adenocarcinoma. The progress of the skin lesions reflects the development of the tumor, and effective treatment should lead to regression of the tumor and skin lesions, though a recurrence of the lesion may mean a recurrence of the tumor[13].
This patient had gastric adenocarcinoma with ANs, Leser–Trélat sign, and tripe palms. His rash occurred before the gastric cancer, and dermatological treatment for this had been ineffective after 1 year. Later, upper abdominal pain reported by the patient was clearly diagnosed by gastroscopy as gastric adenocarcinoma. In this case, AN mainly appeared on the face and neck and as papillary wart-like hyperkeratosis with dark brown pigmentation on the areola. These manifestations are different from the extensive rash in most patients in previous reports[14,15]. Furthermore, the lesions of Leser–Trélat sign were mainly distributed on the face, neck, chest, back, and head, reaching more than 40 lesions, thereby not completely consistent with the typical Leser–Trélat sign[14,15]. Meanwhile, tripe palms mainly occurred on both palms; small, smooth, papillary projections in the shape of tripe palm were observed, consistent with the typical tripe palm[16]. Theoretically, if gastric cancer is diagnosed and treated at an early stage, when symptoms of skin lesions mentioned above are present, AN will improve and the tumor will be effectively controlled. In such cases, the patient's prognosis will be better. For this patient, it was decided that the removal of the gastric tumors would be the best treatment option. Neoadjuvant chemotherapy would normally performed over one to three cycles before surgery to reduce the focus and provide favorable conditions for surgery and postoperative recovery of the patient. However, because the lesion was identified late in this case, and it had also been found during the operation that the tumor had invaded the pancreas, the optimal time for surgical treatment of the gastric tumor had been missed. Fortunately, after three cycles of chemotherapy, the patient’s skin symptoms were significantly relieved. Considering that the evolution of malignant AN is closely related to the evolution of cancer, it will regress after surgical resection of the tumor or some cell suppression treatment. Such treatment may even become a valuable parameter for monitoring the effectiveness of treatment, since AN will be reactivated when the tumor recurs or metastases develop[17]. The treatment in this case also served to illustrate that AN and other paraneoplastic syndromes presenting on the skin are of high value in the diagnosis of tumors. Hence, the three special manifestations, namely, AN, Leser–Trélat sign, and tripe palms, must be considered before or during the occurrence of tumor or skin lesions. If a patient has skin lesions, especially multiple lesions, and the symptoms worsen, or if progressive emaciation, which highly suggests malignancy in the internal organs, the healthcare team should undertake a comprehensive medical examination, determine the potential of visceral tumor, and provide the necessary treatment as soon as possible to achieve the best curative effect. Our case suggests that clinicians should pay more attention to these special manifestations, search for rare diseases, and monitor closely these patients to make timely diagnosis and treatment and improve the prognosis.
In summary, we report the clinical manifestations and pathological features in a case of a primary gastric malignant tumor with multiple paraneoplastic syndromes and review the skin manifestations and pathological features of AN, Leser–Trélat sign, and tripe palms. As for the etiology, pathogenesis and related biological behavior of the disease, we are not yet clear, and there is currently no specific treatment for the skin symptoms. The treatment is still mainly based on malignant tumor surgery, radiotherapy and chemotherapy, targeted drugs, and other treatment methods. If these methods are effective in treating the tumors, they can also significantly improve the skin symptoms. Further research on these rare tumors with paraneoplastic syndrome will help in understanding their biological behavior and pathogenesis. Therefore, researchers should follow up on patients with malignant AN, Leser–Trélat sign, and tripe palms.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Qinghai Anti-Cancer Association, No. M162805076M.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tanabe K S-Editor: Wang JL L-Editor: Filipodia P-Editor: Li X
| 1. | Kuner N, Hartschuh W. [First descriptions in the "International atlas of rare skin diseases" of 1886]. Hautarzt. 2003;54:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Ng HY. Acanthosis nigricans in obese adolescents: prevalence, impact, and management challenges. Adolesc Health Med Ther. 2017;8:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Kutlubay Z, Engin B, Bairamov O, Tüzün Y. Acanthosis nigricans: A fold (intertriginous) dermatosis. Clin Dermatol. 2015;33:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Oh CW, Yoon J, Kim CY. Malignant Acanthosis Nigricans Associated with Ovarian Cancer. Case Rep Dermatol. 2010;2:103-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Yu Q, Li XL, Ji G, Wang Y, Gong Y, Xu H, Shi YL. Malignant acanthosis nigricans: an early diagnostic clue for gastric adenocarcinoma. World J Surg Oncol. 2017;15:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Wick MR, Patterson JW. Cutaneous paraneoplastic syndromes. Semin Diagn Pathol. 2019;36:211-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Silva JA, Mesquita Kde C, Igreja AC, Lucas IC, Freitas AF, Oliveira SM, Costa IM, Campbell IT. Paraneoplastic cutaneous manifestations: concepts and updates. An Bras Dermatol. 2013;88:9-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Das M. Neoadjuvant chemotherapy: survival benefit in gastric cancer. Lancet Oncol. 2017;18:e307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Blomberg M, Jeppesen EM, Skovby F, Benfeldt E. FGFR3 mutations and the skin: report of a patient with a FGFR3 gene mutation, acanthosis nigricans, hypochondroplasia and hyperinsulinemia and review of the literature. Dermatology. 2010;220:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Krause W. Skin diseases in consequence of endocrine alterations. Aging Male. 2006;9:81-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Schadt CR. The cutaneous manifestations of gastrointestinal malignancy. Semin Oncol. 2016;43:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Cohen PR, Grossman ME, Silvers DN, Kurzrock R. Tripe palms and cancer. Clin Dermatol. 1993;11:165-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Schwartz RA. Acanthosis nigricans. J Am Acad Dermatol. 1994;31:1-19; quiz 20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 192] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Zhang N, Qian Y, Feng AP. Acanthosis nigricans, tripe palms, and sign of Leser-Trélat in a patient with gastric adenocarcinoma: case report and literature review in China. Int J Dermatol. 2015;54:338-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Pentenero M, Carrozzo M, Pagano M, Gandolfo S. Oral acanthosis nigricans, tripe palms and sign of leser-trélat in a patient with gastric adenocarcinoma. Int J Dermatol. 2004;43:530-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Chen WT, Chu CH. Tripe palm: a paraneoplastic manifestation of gastric cancer. CMAJ. 2019;191:E366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Gorisek B, Krajnc I, Rems D, Kuhelj J. Malignant acanthosis nigricans and tripe palms in a patient with endometrial adenocarcinoma--a case report and review of literature. Gynecol Oncol. 1997;65:539-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |