Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5409
Peer-review started: June 16, 2020
First decision: July 25, 2020
Revised: August 5, 2020
Accepted: August 20, 2020
Article in press: August 20, 2020
Published online: November 6, 2020
Processing time: 142 Days and 18.5 Hours
Esophageal cancer is a common malignant tumor of the digestive system. At present, surgery is the most important treatment strategy. After esophagectomy and gastric esophagoplasty, the patients are prone to regurgitation. However, these patients currently do not receive much attention, especially from anesthesiologists.
A 55-year-old woman was scheduled for right lower lung lobectomy. The patient had undergone radical surgery for esophageal cancer under general anesthesia 6 mo prior. Although the patient had fasted for > 17 h, unexpected aspiration still occurred during induction of general anesthesia. Throughout the operation, oxygen saturation was 98%-100%, but the airway pressure was high (35 cmH2O at double lung ventilation). The patient was sent to the intensive care unit after surgery. Bedside chest radiography was performed, which showed exudative lesions in both lungs compared with the preoperative image. After surgery, antibiotics were given to prevent lung infection. On day 2 in the intensive care unit, the patient was extubated and discharged on postoperative day 7 without complications related to aspiration pneumonia.
After esophagectomy, patients are prone to regurgitation. We recommend nasogastric tube placement followed by rapid sequence induction or conscious intubation.
Core Tip: In patients undergoing esophagectomy and gastric esophagoplasty, there is a high risk of aspiration pneumonia during the perioperative period. Aspiration pneumonia is closely related to postoperative mortality and pulmonary complications, so anesthesiologists should pay extra attention to such patients.
- Citation: Tang JX, Wang L, Nian WQ, Tang WY, Xiao JY, Tang XX, Liu HL. Aspiration pneumonia during general anesthesia induction after esophagectomy: A case report. World J Clin Cases 2020; 8(21): 5409-5414
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5409.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5409
Esophageal cancer ranks eighth and sixth for morbidity and mortality, respectively, worldwide[1]. At present, surgery is the most important treatment, but even though surgical techniques are much improved, the incidence of postoperative complications is still high. Esophagectomy and gastric esophagoplasty for esophageal cancer cause reduction of gastric volume, removal of the esophageal sphincter, and impairment of vagal innervation of the stomach, so regurgitation and delayed gastric emptying after esophageal cancer surgery are two common complications[2,3].
However, these patients do not currently attract much attention, especially from anesthesiologists. Here, we report a patient who had undergone esophagectomy and gastric esophagoplasty before being scheduled for elective right lung lobectomy. Regurgitation and aspiration developed during induction of general anesthesia.
A 55-year-old woman was admitted to our hospital with complaints of a nodule of the lower lobe of the right lung found 1 mo ago.
The patient had undergone radical surgery for esophageal cancer 6 mo prior. The patient was admitted to the hospital for routine re-examination for esophageal cancer 1 mo ago. Through chest computed tomography (CT) a nodule of the lower lobe of the right lung was found. The patient denied any symptoms such as coughing and hemoptysis.
The patient had a history of coronary heart disease and right mastectomy. She had undergone radical surgery for esophageal cancer under general anesthesia 6 mo ago. During esophagectomy and gastric esophagoplasty, the esophagus was completely removed and replaced with a 2.5 cm diameter gastric tube, which started from the gastric antrum and anastomosed on the left neck.
On physical examination, patient's lungs breath sounds were clear and symmetrical on auscultation.
Preoperative blood gas analysis showed pH 7.43, partial pressure of carbon- dioxide 40.00 mmHg and partial pressure of oxygen 75.00 mmHg. Blood tests showed slightly low levels of hemoglobin (102 g/L; normal: ≥ 115 g/L). The results of blood biochemistry tests, coagulation function test, myocardial enzymes, urinalysis and stool analysis were normal.
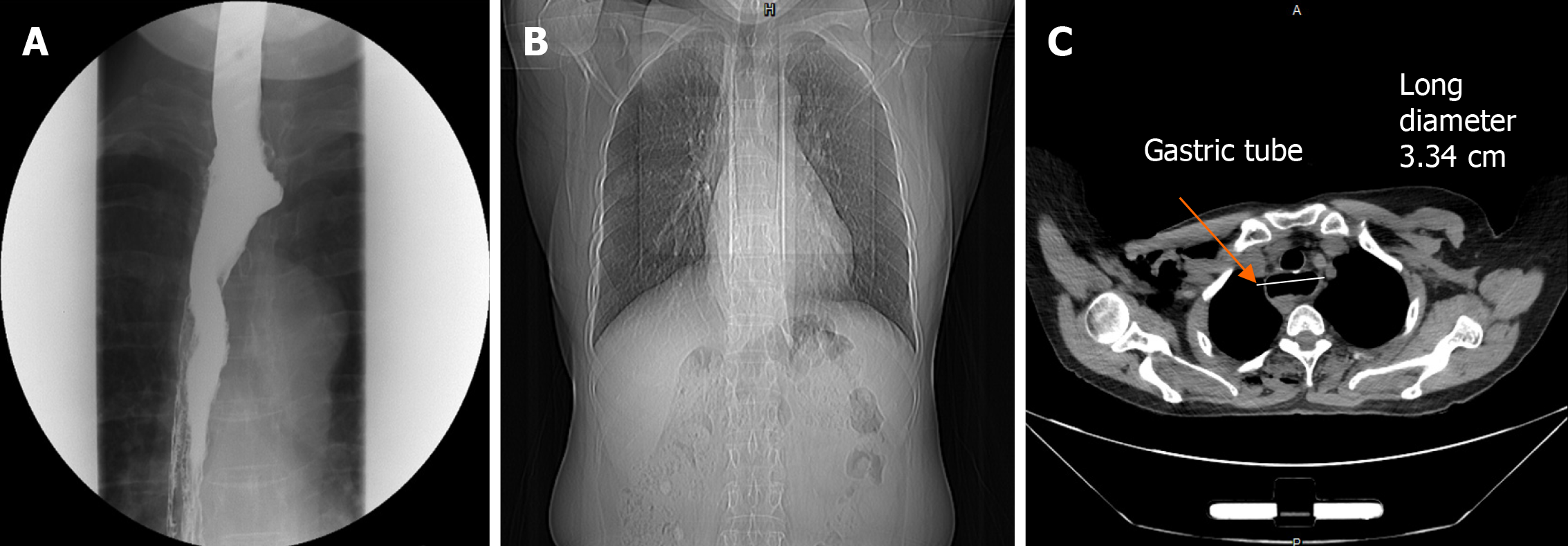
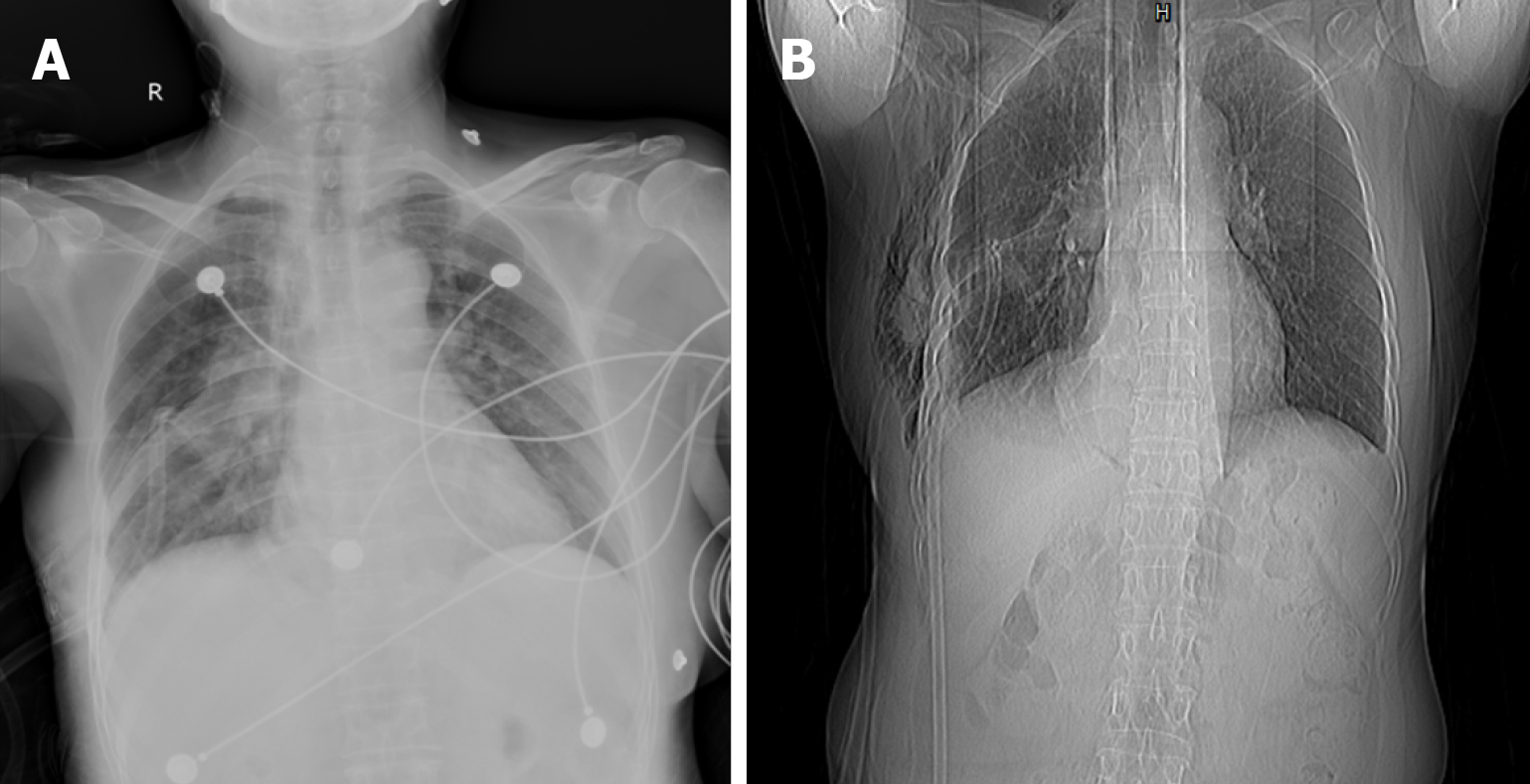
The preoperative esophagography showed that the contrast agent passed smoothly through the esophagogastric anastomosis, and no local fistula was observed (Figure 1A). Preoperative chest CT revealed a 2.0 cm × 1.5 cm × 0.5 cm nodule in the lower lobe of the right lung with no active lung lesion (Figure 1B), and gastric tube mild dilatation was shown (Figure 1C). Preoperative lung function, cardiac ultrasound and electrocardiography were normal. Immediate postoperative chest X-ray showed ill-defined frosted hyaline shadow with exudative lesions in both lungs (Figure 2A). At postoperative day 6, chest X-ray showed that the exudative lesions in both lungs were markedly reduced (Figure 2B).
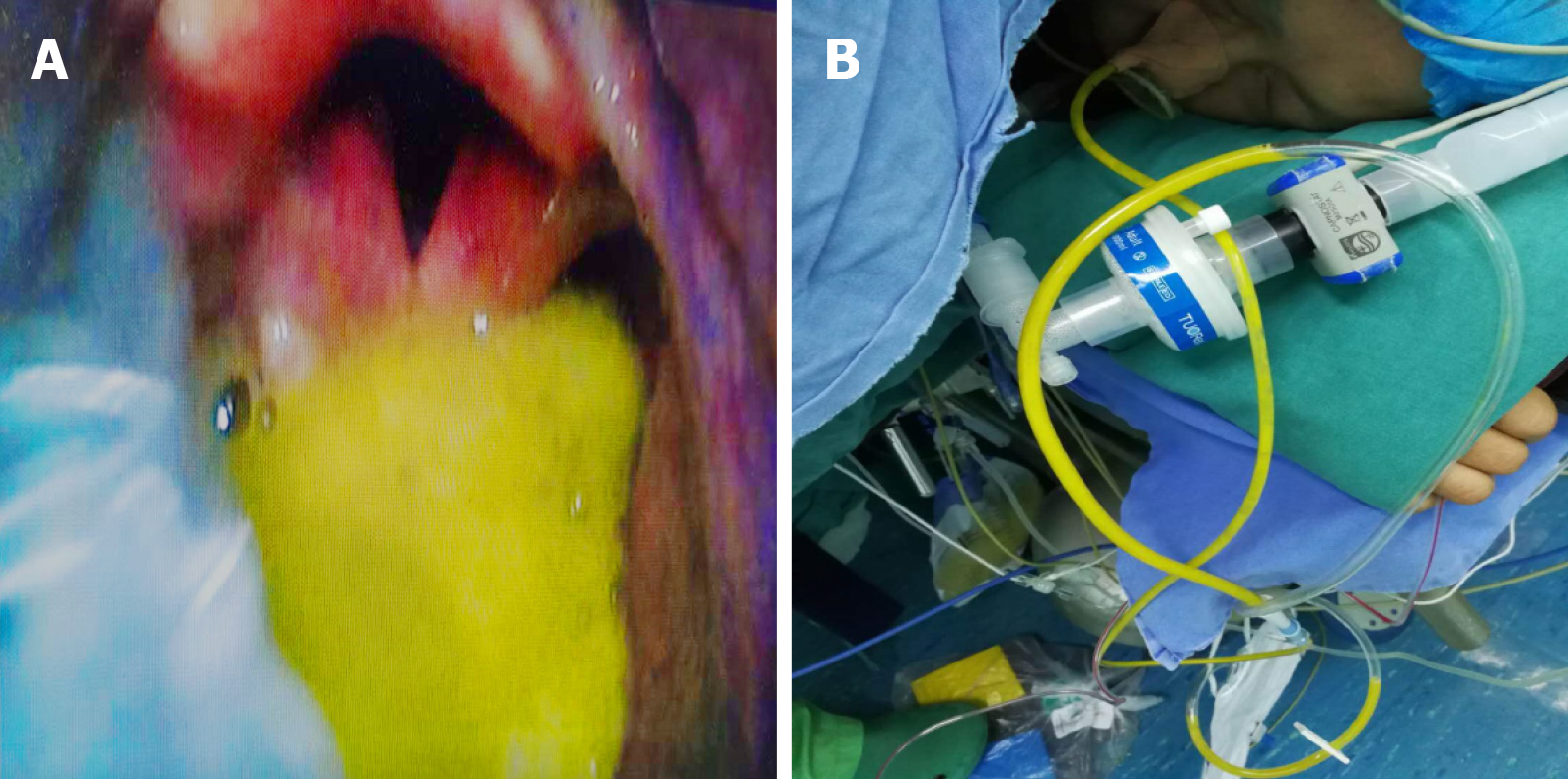
Before surgery, no premedication was given, the nasogastric tube was not placed and fasting was > 17 h. On admission to the operating room, heart rate, blood pressure, oxygen saturation (SpO2) and electrocardiography were monitored, and pure oxygen was administered at 8 L/min through a face mask. Three minutes later, 0.3 mg/kg sufentanil, 2 mg midazolam, 2 mg/kg propofol, 4 mg dexamethasone, 50 mg rocuronium and 40 mg lidocaine were administered intravenously for induction of general anesthesia. Mask ventilation was conducted, and the airway pressure was below 20 cmH2O. A video laryngoscope (Insight iS3; Insighters, Shenzhen, China) was inserted to expose the glottis for intubation, and yellow–green gastric content was found in the pharyngeal cavity (Figure 3A). We immediately withdrew the content and intubated the patient with a 35 Fr left-side double-lumen endobronchial tube, and 20 mL yellow–green fluid was withdrawn through the tube. A nasogastric tube was inserted into the stomach, and 100 mL liquid was drained out (Figure 3B). Throughout the procedure, SpO2 was 98%-100%, but the airway pressure was high (35 cmH2O at double lung ventilation). To manage the high airway pressure, 100 mg salbutamol was administered through the endobronchial tube, and 0.125 g aminophylline and 100 mg hydrocortisone were administered intravenously. One lung ventilation was performed with fraction of inspired oxygen of 50% and SpO2 of 98%-100%. Blood gas analysis showed pH 7.21, partial pressure of carbon dioxide 61.1 mmHg and partial pressure of oxygen 232.9 mmHg. At the end of the 2 h operation, the airway pressure at double lung ventilation was 19 cmH2O. The patient was sent to the intensive care unit (ICU) after surgery without removing the double-lumen endotracheal tube.
Bedside chest radiography was performed immediately in the ICU and showed exudative lesions in both lungs compared with the preoperative image (Figures 1B and 2A). Blood gas analysis showed pH 7.27, partial pressure of carbon dioxide 41.7 mmHg and partial pressure of oxygen 133.0 mmHg. After surgery, the antibiotic piperacillin/tazobactam was given for 3 d to prevent lung infection.
Aspiration pneumonia.
We immediately withdrew the reflux from the throat and intubated the patient with an endobronchial tube to protect the airway and sucked the reflux through the tracheal tube. A nasogastric tube was inserted into the stomach to drain gastric fluid. To manage the high airway pressure during the operation, 100 mg salbutamol was administered through the endobronchial tube, and 0.125 g aminophylline and 100 mg hydrocortisone were administered intravenously. After surgery, the antibiotic piperacillin/ tazobactam was given for 3 d to prevent lung infection.
On day 2 in the ICU, the patient was extubated, and discharged on day 7 after surgery without complications related to aspiration pneumonia (Figure 2B).
Although the incidence of perioperative aspiration pneumonia is low, it can cause severe pulmonary complications and even death[4]. Chest CT of aspiration pneumonia often shows multifocal consolidation, bronchial inflation and patchy ground-glass opacity[5]. From this case, it can be found that the right lung exudation was more serious than the left side. We speculate that the possible reason is that the right lung bronchial angle is smaller, and the gastric content is easier to enter the right side[5]. In addition, the operation of the right lower lobe of our patient may also be the cause of heavier right lung exudation.
To prevent perioperative aspiration pneumonia, we usually pay attention to patients’ fasting before surgery. For emergency patients with full stomachs, we also maintain a high level of vigilance against perioperative aspiration pneumonia. However, for patients undergoing elective surgery and sufficient fasting before surgery, our vigilance against aspiration pneumonia may be reduced. Radical resection of esophageal cancer is the main treatment for esophageal cancer, and esophageal reconstruction after esophagectomy is a major problem for esophageal surgery. At present, the gastric tube replacement of the esophagus is mainly used clinically[6]. During esophagectomy and gastric esophagoplasty, the esophageal sphincter is removed. During the process of making the gastric tube, the gastric vagus nerve is excised, and gastric peristalsis is reduced. Additionally, the gastric tube is placed in the chest and may be in a state of passive expansion[7]. In the present case, we found that the patient had gastric tube mild dilatation before surgery (Figure 1C)[8]. These factors lead to delayed gastric emptying and an increase in the incidence of gastroesophageal reflux[7,9,10].
At present, for the prevention of aspiration pneumonia, there are many methods to be recommended: Nasogastric tube placement; high head induction; rapid sequence induction with cricoid pressure and mask free ventilation and conscious tracheal intubation[11]. There are also some controversies regarding the above measures. The purpose of nasogastric tube insertion is to reduce the pressure in the stomach, but there are also concerns that the cardia cannot be closed and about the ineffectiveness of cricoid pressure. Therefore, whether the nasogastric tube is still in place during anesthesia induction is controversial[12]. Induction in high head position can increase the pressure difference between the stomach and pharyngeal cavity and can theoretically reduce the occurrence of reflux. Therefore, if the anesthesia is induced in high head position and regurgitation still occurs, the possibility of aspiration may be higher. Therefore, when faced with patients with high risk of reflux aspiration, some anesthesiologists tend to use head-down induction[13]. The technique of cricoid pressure was first proposed by Sellick in 1961 and can largely prevent reflux of gastroesophageal contents[14]. However, variation in individual anatomy and anatomical abnormalities caused by neck anastomosis in esophageal cancer surgery may make cricoid pressure ineffective[15]. At present, ultrasound visualization has been widely used in anesthesia, and it is worth trying ultrasound-guided cricoid pressure[16]. The use of gastric ultrasound to assess gastric contents before induction may help guide anesthesia strategies[17]. However, the use of ultrasound to assess gastric contents for this case whose gastric tube in the thoracic cavity may be very difficult. In our case, due to lack of experience, we failed to give the patient rapid sequence induction with maskless ventilation. However, even if we did, aspiration could not be completely avoided[18,19]. The nasogastric balloon tube may be a good alternative to rapid sequential induction and awake intubation[20], but whether it is effective in patients undergoing esophagectomy remains to be verified. In addition, since the severity of aspiration pneumonia is related to pH and amount of gastric content[21], the prophylactic use of stomach stimulants and acid inhibitors may reduce mortality of aspiration pneumonia[22].
After esophagectomy and gastric esophagoplasty, there is a high risk of aspiration pneumonia during the perioperative period. There is still insufficient evidence to support the use of various methods to prevent aspiration in this high-risk group. However, aspiration pneumonia is closely related to postoperative mortality and pulmonary complications, so anesthesiologists should pay more attention to such patients. Based on current evidence, we recommend nasogastric tube placement before induction followed by rapid sequence induction or conscious intubation for these patients to prevent aspiration pneumonia.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bäcker HC, Kurokawa T, Lee J, Nakano T S-Editor: Zhang L L-Editor: Filipodia P-Editor: Wang LL
| 1. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20108] [Cited by in RCA: 20504] [Article Influence: 2050.4] [Reference Citation Analysis (20)] |
| 2. | Mboumi IW, Reddy S, Lidor AO. Complications After Esophagectomy. Surg Clin North Am. 2019;99:501-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Predescu D, Constantinoiu S. Esophageal Reconstruction with the Stomach, a Functional Dilemma? Chirurgia (Bucur). 2018;113:83-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Sakai T, Planinsic RM, Quinlan JJ, Handley LJ, Kim TY, Hilmi IA. The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis. Anesth Analg. 2006;103:941-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Lee KH, Kim WS, Cheon JE, Seo JB, Kim IO, Yeon KM. Squalene aspiration pneumonia in children: radiographic and CT findings as the first clue to diagnosis. Pediatr Radiol. 2005;35:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Zhang W, Yu D, Peng J, Xu J, Wei Y. Gastric-tube versus whole-stomach esophagectomy for esophageal cancer: A systematic review and meta-analysis. PLoS One. 2017;12:e0173416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Hasegawa D, Komura H, Katsuta K, Kawaji T, Nishida O. Thoracic stomach syndrome after whole-stomach esophagectomy for esophageal cancer mimicking tension pneumothorax: a case report. J Med Case Rep. 2019;13:324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Yamasaki T, Tomita T, Mori S, Takimoto M, Tamura A, Hara K, Kondo T, Kono T, Tozawa K, Ohda Y, Oshima T, Fukui H, Watari J, Miwa H. Esophagography in Patients With Esophageal Achalasia Diagnosed With High-resolution Esophageal Manometry. J Neurogastroenterol Motil. 2018;24:403-409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Kim D, Min YW, Park JG, Lee H, Min BH, Lee JH, Rhee PL, Kim JJ, Zo JI. Influence of esophagectomy on the gastroesophageal reflux in patients with esophageal cancer. Dis Esophagus. 2017;30:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Poghosyan T, Gaujoux S, Chirica M, Munoz-Bongrand N, Sarfati E, Cattan P. Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J Visc Surg. 2011;148:e327-e335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Knoth S, Weber B, Croll M, Lotz H, Eberhart L. [Anaesthesiologic Techniques for Patients at Risk of Aspiration]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2019;54:589-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Salem MR, Khorasani A, Saatee S, Crystal GJ, El-Orbany M. Gastric tubes and airway management in patients at risk of aspiration: history, current concepts, and proposal of an algorithm. Anesth Analg. 2014;118:569-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Klucka J, Kosinova M, Zacharowski K, De Hert S, Kratochvil M, Toukalkova M, Stoudek R, Zelinkova H, Stourac P. Rapid sequence induction: An international survey. Eur J Anaesthesiol. 2020;37:435-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | SELLICK BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet. 1961;2:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 705] [Cited by in RCA: 562] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003;99:60-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 123] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Baskin PL, Kimura BJ. Use of point-of-care ultrasound to assess esophageal insufflation during bag mask ventilation: A case report. Respir Med Case Rep. 2019;28:100928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Gagey AC, de Queiroz Siqueira M, Desgranges FP, Combet S, Naulin C, Chassard D, Bouvet L. Ultrasound assessment of the gastric contents for the guidance of the anaesthetic strategy in infants with hypertrophic pyloric stenosis: a prospective cohort study. Br J Anaesth. 2016;116:649-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 18. | Koh GH, Kim SH, Son HJ, Jo JY, Choi SS, Park SU, Kim WJ, Ku SW. Pulmonary aspiration during intubation in a high-risk patient: A video clip and clinical implications. J Dent Anesth Pain Med. 2018;18:111-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Kiyohara Y, Fujita Y, Shimizu T, Aoki M. [Unexpected vomiting during anesthetic induction in a patient with a history of anterosternal esophageal reconstruction]. Masui. 2010;59:97-100. [PubMed] |
| 20. | Roewer N. Can pulmonary aspiration of gastric contents be prevented by balloon occlusion of the cardia? Anesth Analg. 1995;80:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | James CF, Modell JH, Gibbs CP, Kuck EJ, Ruiz BC. Pulmonary aspiration--effects of volume and pH in the rat. Anesth Analg. 1984;63:665-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 84] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Hussain A, Al-Saeed AH, Habib SS. Effect of single oral dose of sodium rabeprazole on the intragastric pH & volume in patients undergoing elective surgery. Indian J Med Res. 2008;127:165-170. [PubMed] |