Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5401
Peer-review started: February 25, 2020
First decision: July 4, 2020
Revised: July 14, 2020
Accepted: September 3, 2020
Article in press: September 3, 2020
Published online: November 6, 2020
Processing time: 255 Days and 0.5 Hours
Candidal periprosthetic joint infection is a rare and difficult to diagnose complication of total knee arthroplasty. The treatment of such complications is inconclusive and may include prosthesis removal, debridement, arthrodesis, and extensive antifungal therapy to control the infection.
A 62-year-old male with a history of total knee arthroplasty (TKA) in his left knee presented with ipsilateral knee pain and a sinus discharge 20 mo after TKA. The patient was previously evaluated for left knee pain, swelling, and a transient fever one month postoperatively. Prothesis removal and insertion of a cement spacer were performed in a local hospital six months prior to the current presentation. Medical therapy included rifampicin and amphotericin which were administered for 4 wk following prosthesis removal. A second debridement was performed in our hospital and Candida parapsilosis was detected in the knee joint. Fourteen weeks following the latter debridement, the patient suffered a left intertrochanteric fracture and received closed reduction and internal fixation with proximal femoral nail anterotation. Two weeks after fracture surgery, a knee arthrodesis with autograft was performed using a double-plate fixation. The patient recovered adequately and was subsequently discharged. At the two-year follow-up, the patient has a stable gait with a pain-free, fused knee.
Fungal periprosthetic joint infection following TKA may be successfully and safely treated with prosthesis removal, exhaustive debridement, and arthrodesis after effective antifungal therapy. Ipsilateral intertrochanteric fractures of the affected knee can be safely fixated with internal fixation if the existing infection is clinically excluded and aided by the investigation of serum inflammatory markers.
Core Tip: We report a unique case of fungal periprosthetic joint infection further complicated by ipsilateral intertrochanteric fracture following total knee arthroplasty. We demonstrate that therapy including prosthesis removal, exhaustive debridement, and arthrodesis after effective antifungal therapy may be adequate for controlling such infections. Additionally, internal fixation of ipsilateral intertrochanteric fractures following such infections may be safe if clinical and laboratory investigations suggest resolution of the former infection.
- Citation: Xin J, Guo QS, Zhang HY, Zhang ZY, Talmy T, Han YZ, Xie Y, Zhong Q, Zhou SR, Li Y. Candidal periprosthetic joint infection after primary total knee arthroplasty combined with ipsilateral intertrochanteric fracture: A case report. World J Clin Cases 2020; 8(21): 5401-5408
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5401.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5401
Periprosthetic joint infection (PJI) is one of the most serious complications of total knee arthroplasty (TKA)[1]. With the improvement of surgical techniques and conditions, the incidence of periprosthetic infection is decreasing. However, with the rapid increase in the total number of arthroplasties, the absolute number of PJI has also increased. Fungal PJIs are rarely reported, accounting for less than 1% of all PJIs[2]. However, fungal infections may result in disastrous consequences for the patient. Many factors may increase the risk for fungal PJIs following arthroplasties, including impaired host immunity, malignant tumors, excessive or inappropriate use of antibiotics, and catheter retention (urinary or extra-intestinal hypertrophic tubes). Due to atypical early clinical signs and lack of specificity in laboratory examinations, the early diagnosis of fungal PJIs is difficult. In addition, due to the lack of high-level evidence, no standard management has been determined. Although a two-stage exchange arthroplasty is preferred by most surgeons[3], controversies still exist with regard to the ideal interval between implant removal and reimplantation, the usefulness of antifungal-loaded cement spacers and the duration of systemic antifungal treatment. If other fractures occur in the interval between implant removal and reimplantation, the case would be more complicated.
Here, we report a case of candidal PJI following TKA combined with ipsilateral intertrochanteric fracture after the first stage of implant removal and cement spacer insertion.
A 62-year-old male presented with pain and a sinus effusion in the left replaced knee for 3 mo.
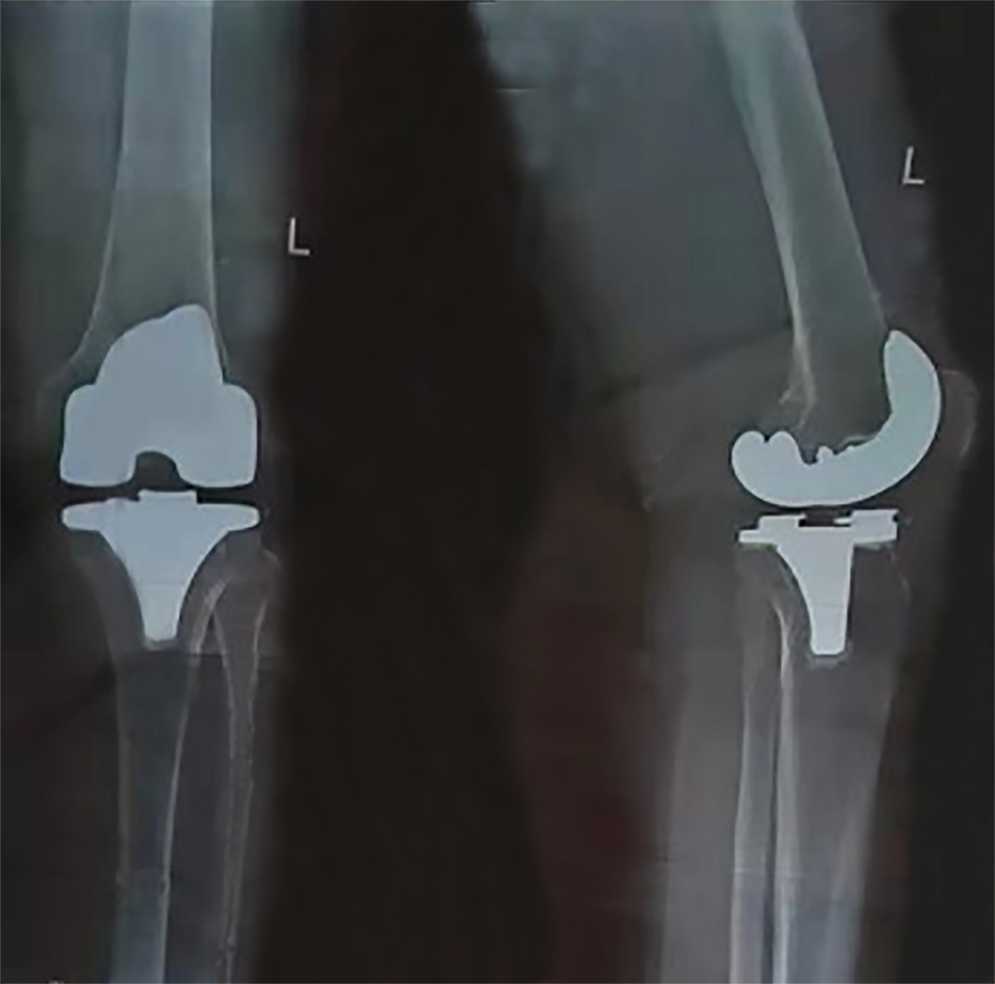
A TKA of the left knee was performed 20 mo prior to the current admission. One month postoperatively, the patient experienced pain and swelling of the left knee with transient fever. The patient was administered amoxicillin for one week by a local community clinic without abatement of the symptoms. Three months after the TKA, he was referred to the operating hospital where a knee aspiration was performed with no indicative findings. Radiography of the left replaced knee did not reveal any notable abnormalities (Figure 1). Gentamicin and vancomycin were given empirically without a clinically significant response. The knee was re-aspirated without any indicative findings. The patient was then discharged without a definitive diagnosis. Fourteen months after TKA, the patient experienced left knee pain with further exacerbation of joint swelling and an inability to walk. Thus, the hospital chose to remove the implant and insert an antibiotic-impregnated (vancomycin) acrylic bone cement spacer (Figure 2). Bacterial cultures were performed on the intraoperative excised tissue and the result remained negative. Rifampicin was administered for another four weeks post-operatively. Three months later, a draining sinus with effusion appeared on the left knee and the patient was referred to our hospital.
The patient had no history of cardiovascular disease, diabetes, immune deficiency, or long-term steroid use.
Upon examination, a drainage sinus tract with effusion was observed superomedial to the patellar tendon. The local temperature was slightly elevated, with a terminally restricted range of motion upon flexion and pain associated with both passive and active motion of the knee. The patient was neurologically intact and distal pulsations were well felt.
Laboratory evaluation including complete blood count, procalcitonin, interleukin-6, erythrocyte sedimentation rate, and urine microscopy revealed no significant abnormalities besides an elevated C-reactive protein (31.1 mg/L). Knee joint aspiration was sent for analysis. Gram staining of the bacterial culture was negative, but fungal culture was positive for Candida parapsilosis (C. parapsilosis).
No abnormalities were found in the anteroposterior lateral radiographs of the knee after primary TKA.
Candidal periprosthetic joint infection after primary total knee arthroplasty.
Considering the recurrent failure in obtaining a definitive diagnosis or clinically significant findings from cultured samples, we decided to perform an additional operation to replace the cement spacer. During the operation, necrotic tissue with a white cheesy appearance was observed on the surface of the spacer which had an unpleasant odor (Figure 3). The intraoperative specimen was sent for aerobic, anaerobic, acid-fast bacilli, and fungal cultures. After removal of the spacer, exhaustive debridement was performed. After the debridement, examination revealed mediolateral knee instability. Therefore, a cross-knee external fixator was applied to optimize stabilization, followed by the insertion of a new cement spacer (Figure 4). Fungal culture was positive for C. parapsilosis sensitive to voriconazole and itraconazole with bacterial cultures remaining negative. Post-operative medical therapy included intravenous voriconazole for 4 wk followed by oral itraconazole for 12 wk. Unfortunately, 14 wk postoperatively (2 wk before completion of the anti-fungal treatment course), the patient suffered a fall resulting in a left intertrochanteric fracture (AO classification: 31A2.2) (Figure 5). Upon examination of the left knee, we found that it was free of any sinuses or signs of surgical wound infection, with an intact range of motion. The patient’s C-reactive protein, procalcitonin, and erythrocyte sedimentation rate were all within the normal reference ranges. The patient underwent a closed reduction and internal fixation with proximal femoral nail anterotation for the fracture and was able to walk on crutches the following day (Figure 6). Two weeks after the latter operation, no signs of infection were observed, and inflammatory markers all declined or were within the normal range. Considering the extensive soft-tissue defect around the knee joint, a knee arthrodesis with autograft was performed using a double-plate fixation (Figure 7). The patient recovered adequately and was subsequently discharged.
At the two-year follow-up, the patient is able to walk without crutches for more than 3 km with a pain-free fused knee. However, radiography shows significantly worsened contralateral knee degeneration (Figure 8).
Fungal PJIs are rarely reported worldwide. Thus, evidence-based guidelines on the treatment of fungal PJIs have yet to be established[4]. The presence of a persistent fungal infection is thought to be a result of an often delayed diagnosis[5,6]. Several different treatment methods, including antifungal drugs, debridement with retained prosthesis, resection arthroplasty, one-stage or two-stage exchange arthroplasty and arthrodesis have been reported, with variable outcomes[3,5].
Currently, the trigger of fungal infection remains unclear. Patients who are immunocompromised, have an underlying systemic illness or have been subject to prolonged antibiotic regimens may have a higher risk of fungal infection. Prolonged wound drainage has also recently been identified as a potential risk factor[7]. The most likely cause of fungal infection in the reported case is the extensive use of antibiotics before identifying a definitve cause of the prosthetic joint infection.
In previous studies, Candida albicans was reported to be the most common pathogen in PJIs followed by C. parapsilosis[8]. Candidal PJI was reported in patients with preoperative cutaneous candidiasis[9]. However, No primary source of candidal infection was identified in our case. It should be noted that C. parapsilosis infections are characterized by the creation of highly resolute biofilms, making eradication of the mycotic infection a significant obstacle[5,6].
Fungal infections are characterized by a subtle onset of symptoms, and typical local and systemic signs of infection such as swelling, fever, erythema and pain are often absent. The progression of symptoms is often slow, usually manifesting weeks to years after arthroplasty[10]. In this case, the patient’s initial symptoms were not obvious and without systemic symptoms, further obscuring early diagnosis.
Fungal culture is not considered a routine test in many hospitals. Negative bacterial culture results of synovial fluid aspiration cannot exclude infection. For patients with potential risk factors such as long-term use of antibiotics, immunosuppressants, catheterization, and cutaneous fungal infections, one should expand beyond the spectrum of bacterial cultures to consider the possibility of a fungal etiology[11].
In the presented case, the fracture occurred during the late stage of the anti-fungal course after the second debridement. The fracture was managed under the assumption that the fungal infection had resolved. After weighing the risks of the complication of the fracture and infection, we decided to fixate the fracture with minimally invasive surgery to avoid the complication of long-term immobilization.
Due to exhaustive debridement, a considerable amount of affected tissue was resected and mediolateral instability of the knee was present intraoperatively. Thus, reimplantation was unsuitable for this patient. Considering the high non-fusion rate, we used a double-plate fixation arthrodesis with autograft. Follow-up radiography showed successful fusion after one year.
The choice and the duration of antifungal therapy remains unclear. Amphotericin B and fluconazole are the most commonly used antifungal drugs, but their side effects are greater while voriconazole and itraconazole are less toxic[12]. Keuning et al[6] recently reported a case of C. parapsilosis PJI following revision of TKA, successfully treated with a combination of voriconazole and micafungin. The lack of evidence regarding the choice of antifungals warrants further research in order to optimize treatment protocols for mycotic PJI.
Another controversial issue is the duration of antifungal treatment. A long period of oral antifungal treatment has been recognized as being an essential factor for the success of staged reimplantation after a fungal peri-prosthetic joint infection. However, no evidence was found for the routine use of arthrodesis. Theoretically, arthrodesis is much safer than reimplantation. Therefore, a protocol of intravenous voriconazole for 4 wk followed by oral itraconazole for 12 wk was selected for this case. As of the writing of this report, the patient did not experience recurrence of symptoms.
Fungal PJI following TKA can be successfully and safely treated by prosthesis removal, exhaustive debridement, and arthrodesis after effective antifungal therapy. Ipsilateral intertrochanteric fractures of the affected knee can be safely fixated using internal fixation if resolution of the existing fungal infection can be established via clinical and laboratory investigations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mousa HAL S-Editor: Zhang L L-Editor: Webster JR P-Editor: Xing YX
| 1. | Hwang BH, Yoon JY, Nam CH, Jung KA, Lee SC, Han CD, Moon SH. Fungal peri-prosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br. 2012;94:656-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Selmon GP, Slater RN, Shepperd JA, Wright EP. Successful 1-stage exchange total knee arthroplasty for fungal infection. J Arthroplasty. 1998;13:114-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Jakobs O, Schoof B, Klatte TO, Schmidl S, Fensky F, Guenther D, Frommelt L, Gehrke T, Gebauer M. Fungal periprosthetic joint infection in total knee arthroplasty: a systematic review. Orthop Rev (Pavia). 2015;7:5623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 4. | Azzam K, Parvizi J, Jungkind D, Hanssen A, Fehring T, Springer B, Bozic K, Della Valle C, Pulido L, Barrack R. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: a multi-institutional experience. J Bone Joint Surg Am. 2009;91 Suppl 6:142-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Nace J, Siddiqi A, Talmo CT, Chen AF. Diagnosis and Management of Fungal Periprosthetic Joint Infections. J Am Acad Orthop Surg. 2019;27:e804-e818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Keuning MC, Al Moujahid A, Zijlstra WP. Prosthetic Joint Infection of a Revision Knee Arthroplasty with Candida parapsilosis. Case Rep Orthop. 2019;2019:3634519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Riaz T, Tande AJ, Steed LL, Demos HA, Salgado CD, Osmon DR, Marculescu CE. Risk Factors for Fungal Prosthetic Joint Infection. J Bone Jt Infect. 2020;5:76-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Kwong CA, Puloski SK, Hildebrand KA. Fungal periprosthetic joint infection following total elbow arthroplasty: a case report and review of the literature. J Med Case Rep. 2017;11:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Wu MH, Hsu KY. Candidal arthritis in revision knee arthroplasty successfully treated with sequential parenteral-oral fluconazole and amphotericin B-loaded cement spacer. Knee Surg Sports Traumatol Arthrosc. 2011;19:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Reddy KJ, Shah JD, Kale RV, Reddy TJ. Fungal prosthetic joint infection after total knee arthroplasty. Indian J Orthop. 2013;47:526-529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Kuo FC, Goswami K, Shohat N, Blevins K, Rondon AJ, Parvizi J. Two-Stage Exchange Arthroplasty Is a Favorable Treatment Option Upon Diagnosis of a Fungal Periprosthetic Joint Infection. J Arthroplasty. 2018;33:3555-3560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Wang QJ, Shen H, Zhang XL, Jiang Y, Wang Q, Chen YS, Shao JJ. Staged reimplantation for the treatment of fungal peri-prosthetic joint infection following primary total knee arthroplasty. Orthop Traumatol Surg Res. 2015;101:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |