Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5389
Peer-review started: April 29, 2020
First decision: September 12, 2020
Revised: September 13, 2020
Accepted: September 23, 2020
Article in press: September 23, 2020
Published online: November 6, 2020
Processing time: 191 Days and 2.4 Hours
Conjoined twins are a rare occurrence, and the majority of these malformations are detected during second trimester screening.
Herein we report a case of conjoined twins, which was diagnosed by ultrasound at 8 wk gestation and was normal at 7 wk gestation. The two fetuses shared one heart and were diagnosed as thoracopagus twins. This is the first report of conjoined twins diagnosed at 8 wk gestation. The pregnancy was terminated electively at 9 wk gestation. Because some congenital malformations can be diagnosed earlier, a prenatal ultrasound examination at an early gestational stage cannot be dismissed.
This case demonstrates that a 7-8 wk gestation might be the earliest period when conjoined twins can be diagnosed by ultrasound.
Core Tip: A woman at 8 wk of pregnancy with low progesterone levels came to the hospital for a routine ultrasound examination. Ultrasound showed a twin pregnancy, and the two fetuses were conjoined by the chest and heart. However, the ultrasound performance showed a normal singleton pregnancy at her 7th wk of pregnancy. We found that ultrasound examination at 7-8 wk of pregnancy plays an important role in the early diagnosis of congenital malformation in twins.
- Citation: Liang XW, Cai YY, Yang YZ, Chen ZY. Early ultrasound diagnosis of conjoined twins at eight weeks of pregnancy: A case report . World J Clin Cases 2020; 8(21): 5389-5393
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5389.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5389
Conjoined twins are extremely rare fetal abnormalities with a reported prevalence of 1:50000-1:100000[1]. Conjoined twins result from postzygotic splitting 13 d after fertilization[2]. Approximately 70% of conjoined twins die within 24-48 h after birth or have a fatal congenital disease; thus, early diagnosis and treatment are desirable[3]. In a previous study, conjoined twins were diagnosed by ultrasound between 18 and 22 wk gestation[4]. More recent research has reported the diagnosis of fetal defects in twin pregnancies at 11-13 wk gestation[5]. Termination of pregnancy as early as possible continues to be the best treatment. Herein we report a case of conjoined twins suspected of cardiac fusion diagnosed by prenatal ultrasound at 8 wk gestation and confirmed by surgery.
At 8 wk gestation, a pregnant woman presented with low progesterone level.
A 30-year-old woman had a normal prenatal ultrasound examination at 7 wk gestation. The patient did not have any other discomfort.
The patient is G4P1. She delivered her first child vaginally.
The patient has no special family history.
The patient’s physical examination was normal.
Laboratory testing had revealed a low progesterone level.
The first prenatal transvaginal ultrasound was performed by CD-6 (Mindray, Shenzhen, China) at 7 wk gestation. Two-dimensional ultrasound images showed that the embryo was normal with crown-rump length of 12 mm (Figure 1).
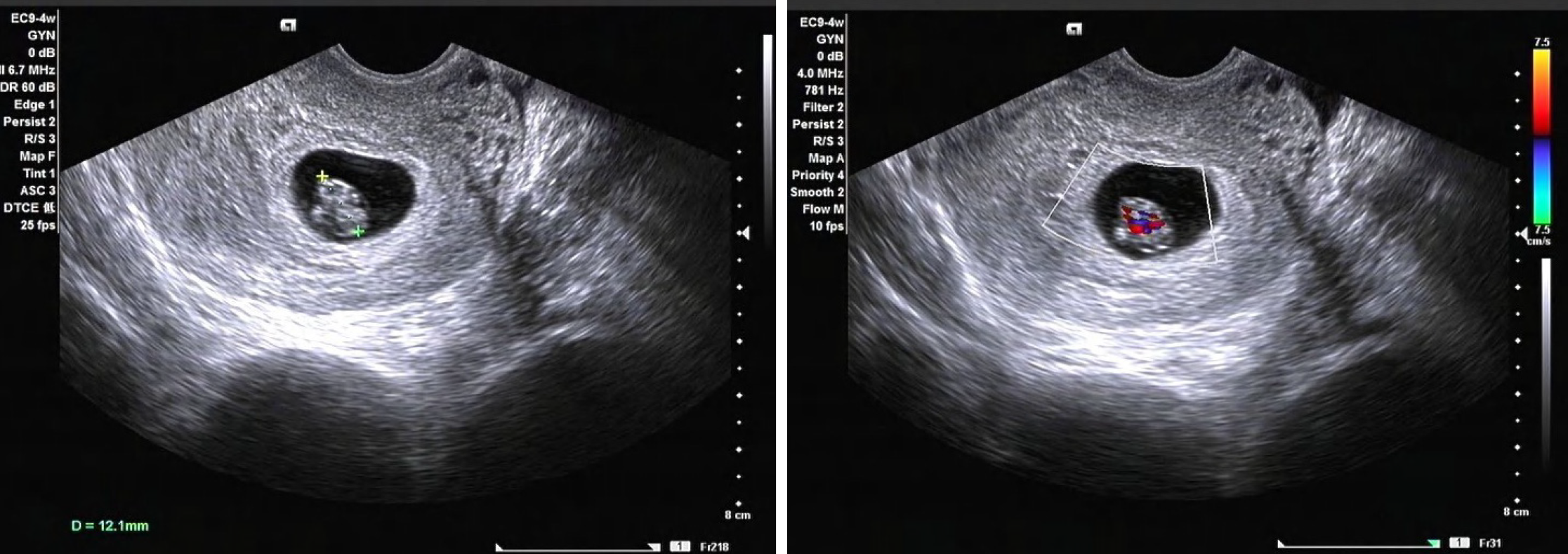
After 7 d, the prenatal ultrasound was performed again using a Volusion E8 (GE Healthcare, Milwaukee, WI, United States). Two-dimensional ultrasound images showed a single yolk and two embryos in the gestational sac. The lengths of the two embryos were 18 mm and 20 mm. The embryos were connected without distinct boundaries, and there was no fluid between them. The two embryos shared one heart. Color Doppler flow imaging showed that pulsating blood flow signals existed at the junction of the two embryos (Figure 2).
Conjoined twins (thoracopagus twins).
Terminated the pregnancy through abortion.
Discharge after a period of observation.
Conjoined twins are very rare monozygotic variants, most of which are monochorionic monoamniotic twins[6]. Although the basis of conjoined twins has not been established, there are two main theories. The first theory is that incomplete division of an early embryo produces identical twins with the same anatomic structures. The other theory is that conjoined twins are the result of two separate embryos reuniting again.
Conjoined twins are classified based on the conjoined body parts. The most common type of conjoined twins is an abdominal union, which accounts for 87% with a mortality rate of 51%, while dorsal unions occur in up to 13% of conjoined twins[7,8]. Cardiac fusion usually occurs in thoracopagus twins, but rarely occurs in ischiopagus, craniopagus, or pygopagus twins. Along with the improvements in surgical technique, survival rates for separation procedures have increased. Although cardiac fusion is relatively common in conjoined twins, the success rate of surgical separation and diagnostic accuracy for this type is extremely low.
In most cases of conjoined twins, a severely deformed connection is fatal for the surviving fetus[9]. However, severe malformations are always caused by the untimely diagnosis, which delays optimal surgical treatment. Chen et al[10] studied the outcomes of postnatal surgical separation of conjoined twins diagnosed before 15 wk gestation. The survival rate of emergency surgery (10%-29%) was reported to be much lower than nonemergent, planned surgery (81%-83%). Recently, Heuer et al[11] successfully separated total-fusion craniopagus twins at 10 mo of age. Dunaway[12] concluded that there are many unknowns regarding the research of separating craniopagus twins in stages. Moreover, in couples who opt to continue the pregnancy, a multidisciplinary team for prenatal and postnatal management is necessary because multiple malformations are often found[13].
It was also demonstrated that early diagnosis of conjoined twins is necessary. Early diagnosis of conjoined twins has the following advantages. First, through the early evaluation of the degree of fusion, the optimal treatment time and strategy can be selected. In addition, early diagnosis will minimize maternal and fetal mortality. Early evaluation will also help parents to choose early termination, thereby reducing the risk of trauma during vaginal delivery[14].
In conclusion, the incidence of conjoined twins is low, but the rate of mortality and malformations (such as severe congenital lung disease) is high. Termination of pregnancy may be a wise choice, especially when the vital organs of the body are connected. This study suggests that active and regular antenatal ultrasonic examinations provide a great opportunity for good prognosis. Interdisciplinary integration also plays an important role in the diagnosis and treatment of conjoined twins[15]. We suppose that an ultrasound examination at 7-8 wk of pregnancy plays an important role in the early diagnosis of congenital malformations in twins. Therefore, apart from the heartbeat and calculation of gestational age, sonographers should also notice the fetal structure in early examinations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ciccone MM S-Editor: Zhang L L-Editor: Filipodia P-Editor: Wang LL
| 1. | Mian A, Gabra NI, Sharma T, Topale N, Gielecki J, Tubbs RS, Loukas M. Conjoined twins: From conception to separation, a review. Clin Anat. 2017;30:385-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 42] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 2. | McNamara HC, Kane SC, Craig JM, Short RV, Umstad MP. A review of the mechanisms and evidence for typical and atypical twinning. Am J Obstet Gynecol. 2016;214:172-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Willobee BA, Mulder M, Perez EA, Hogan AR, Brady AC, Sola JE, Thorson CM. Predictors of in-hospital mortality in newborn conjoined twins. Surgery. 2019;166:854-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Morin L, Lim K; Diagnostic Imaging Committee; Special Contributor; Genetics Committee; Maternal Fetal Medicine Committee. Ultrasound in twin pregnancies. J Obstet Gynaecol Can. 2011;33:643-656. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Syngelaki A, Cimpoca B, Litwinska E, Akolekar R, Nicolaides KH. Diagnosis of fetal defects in twin pregnancies at routine 11-13-week ultrasound examination. Ultrasound Obstet Gynecol. 2020;55:474-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Spitz L, Kiely EM. Conjoined twins. JAMA. 2003;289:1307-1310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Shim JY, Joo DH, Won HS, Lee PR, Kim A. "Hugging sisters": thoracoomphalopagus with anencephaly confirmed by three-dimensional ultrasonography at 9 wk of gestation. J Clin Ultrasound. 2011;39:279-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Sabih D, Ahmad E, Sabih A, Sabih Q. Ultrasound diagnosis of cephalopagus conjoined twin pregnancy at 29 wk. Biomed Imaging Interv J. 2010;6:e38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Burans C, Smulian JC, Rochon ML, Lutte J, Hardin W. 3-dimensional ultrasound assisted counseling for conjoined twins. J Genet Couns. 2014;23:29-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Chen CP, Hsu CY, Su JW, Cindy Chen HE, Hwa-Ruey Hsieh A, Hwa-Jiun Hsieh A, Wang W. Conjoined twins detected in the first trimester: a review. Taiwan J Obstet Gynecol. 2011;50:424-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Heuer GG, Madsen PJ, Flanders TM, Kennedy BC, Storm PB, Taylor JA. Separation of Craniopagus Twins by a Multidisciplinary Team. N Engl J Med. 2019;380:358-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Dijk S, Lok P. Separating conjoined twins: five minutes with . . . David Dunaway. BMJ. 2019;366:l4790. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Gica N, Gana N, Mat C, Panaitescu AM, Peltecu G, Vayna AM. Conjoined twins-early prenatal diagnosis. J Obstet Gynaecol. 2020;40:723-724. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Wataganara T, Yapan P, Moungmaithong S, Sompagdee N, Phithakwatchara N, Limsiri P, Nawapun K, Rekhawasin T, Talungchit P. Additional benefits of three-dimensional ultrasound for prenatal assessment of twins. J Perinat Med. 2020;48:102-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Saw PE, Jiang S. The Significance of Interdisciplinary Integration in Academic Research and Application. BIO Integrat. 2020;1:2-5. [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |