Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5326
Peer-review started: April 27, 2020
First decision: September 24, 2020
Revised: October 6, 2020
Accepted: October 26, 2020
Article in press: October 26, 2020
Published online: November 6, 2020
Processing time: 193 Days and 0.8 Hours
Optimal treatment for iliopsoas tendinitis after total hip arthroplasty (THA) with cup malposition, iliopsoas release alone or with cup revision, is controversial, particularly in young, active patients. Moreover, arthroscopic iliopsoas tendon (IPT) release in these patients has been rarely described, and midterm effects of this procedure on THA longevity and groin pain recurrence remain unclear. We performed arthroscopic IPT release after THA and report midterm outcomes in two young patients with acetabular cup malposition.
In the two patients, groin pain started early after THA. Physical examination revealed nonspecific findings, and laboratory tests showed no evidence of infection. Radiography and computed tomography showed reduced acetabular component anteversion angle and anterior cup prominence of more than 16 mm. For therapeutic diagnosis, ultrasonography-guided lidocaine with steroid was injected into the IPT sheath. In both patients, groin pain improved initially but worsened after a few months. Therefore, the patients underwent arthroscopic IPT release under spinal anesthesia. Arthroscopy revealed synovitis with fibrous tissues around the IPT and various lesions related to the implants after THA. IPT tenotomy and debridement with biopsy were performed; histopathologic studies showed chronic inflammation with synovial hyperplasia. Both patients were encouraged to start walking immediately after surgery, and they returned to complete daily function early after surgery. They experienced no recurrence of groin pain or any implant-related problems 5 years postoperatively.
Arthroscopic IPT release for cup malposition produced excellent midterm outcomes without recurrence of groin pain and implant-related problems.
Core Tip: Optimal treatment for iliopsoas tendinitis combined with cup malposition is controversial. Ultrasonography-guided analgesic injection is useful in therapeutic diagnosis. If conservative treatment fails, cup revision or iliopsoas tendon (IPT) release with cup retention can be considered. Acetabular correction of malposition of well-fixed component might be ideal especially in young, active patients but is usually refused because of symptoms are subtle. Arthroscopic IPT release can provide better access to evaluate the exact location of lesions and other potential problems related to total hip arthroplasty and may be a useful alternative surgical option for preventing recurrence of groin pain.
- Citation: Won H, Kim KH, Jung JW, Kim SY, Baek SH. Arthroscopic treatment of iliopsoas tendinitis after total hip arthroplasty with acetabular cup malposition: Two case reports. World J Clin Cases 2020; 8(21): 5326-5333
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5326.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5326
The incidence of groin pain after total hip arthroplasty (THA) ranges from 0.4% to 18.3%[1]. Groin pain has been reported to follow aseptic loosening, periprosthetic joint infection, and periprosthetic fracture[2]. Since Trousdale et al[3] first described iliopsoas tendinitis (IPTs) as another cause of groin pain after THA, interest in causes and management has been growing[2]. Common cause of IPTs after THA reported in the literature included disruption of the anterior capsule, anterior osteophytes, retained cement, use of excessively long screw, acetabular cage reconstruction, femoral stem with prominent collar, malpositioned or oversized acetabular cup, and larger femoral head[2,4].
In spite of the reported prevalence as high as 4.3%[2], IPTs after THA may be overlooked because the symptoms are subtle and the physical findings are nonspecific. Patients usually complain of groin pain during active hip flexion, such as ascending stairs[3,5], and on physical examination, common findings are usually aggravated groin pain during resisted straight leg raise testing or passive stretching of the iliopsoas tendon (IPT)[2]; however, these findings are nonspecific and can be also demonstrated with other common causes of groin pain after THA, such as aseptic loosening and periprosthetic joint infection.
Surgical options for cases refractory to conservative treatment are another concern. Although open IPT tenotomy after conservative treatment had been proposed as a standard treatment for IPTs after THA, arthroscopic IPT release has recently become popular and has demonstrated better outcomes than have open procedures[2,6,7]. However, IPTs after THA in combination with acetabular cup malposition is an unusual situation, and additional considerations are necessary. Because component malposition can affect THA longevity and may lead to recurrence of groin pain, the optimal treatment for IPTs after THA, open iliopsoas release alone or with cup revision, has remained controversial, especially in young, active patients[3,5,6]. Moreover, arthroscopic IPT release in these patients has rarely been described in detail, and the midterm effects of this procedure on THA longevity and on recurrence of groin pain have not been reported previously. Therefore, we report the midterm outcome in two young patients with acetabular cup malposition who underwent arthroscopic release for IPTs after THA.
Case 1: A 49-year-old woman presented to the outpatient clinic with a 4-year history of left groin pain.
Case 2: A 40-year-old woman visited to the outpatient clinic with a 2-year history of left groin pain.
Case 1: The groin pain had started immediately after THA. This symptom was aggravated during walking, especially at the end of stance phase.
Case 2: The groin pain had started soon after THA, and the patient experienced a single episode of perioperative dislocation.
Case 1: The patient did not have any significant past illness.
Case 2: The patient reported that she did not have any past illness.
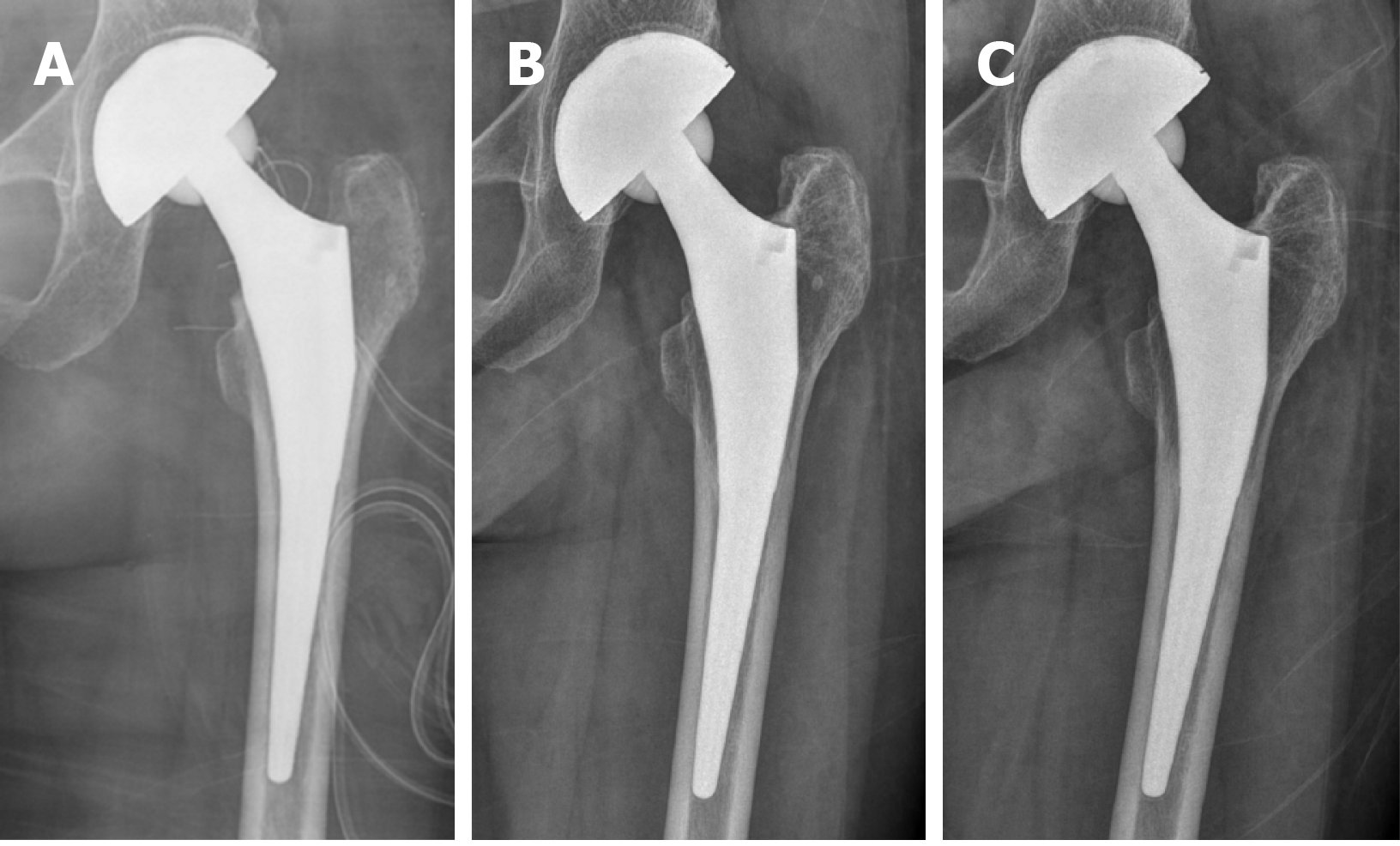
Case 1: The patient underwent THA for osteonecrosis of the femoral head in another hospital 4 years ago before visiting our institution (Figure 1A). The cementless prostheses implanted were a 52-mm Trilogy cup®, M/L stem (Zimmer®, Warsaw, IN, United States), and 28-mm Biolox® Alumina forte ceramic bearing couples (CeramTec®, Plochingen, Germany).
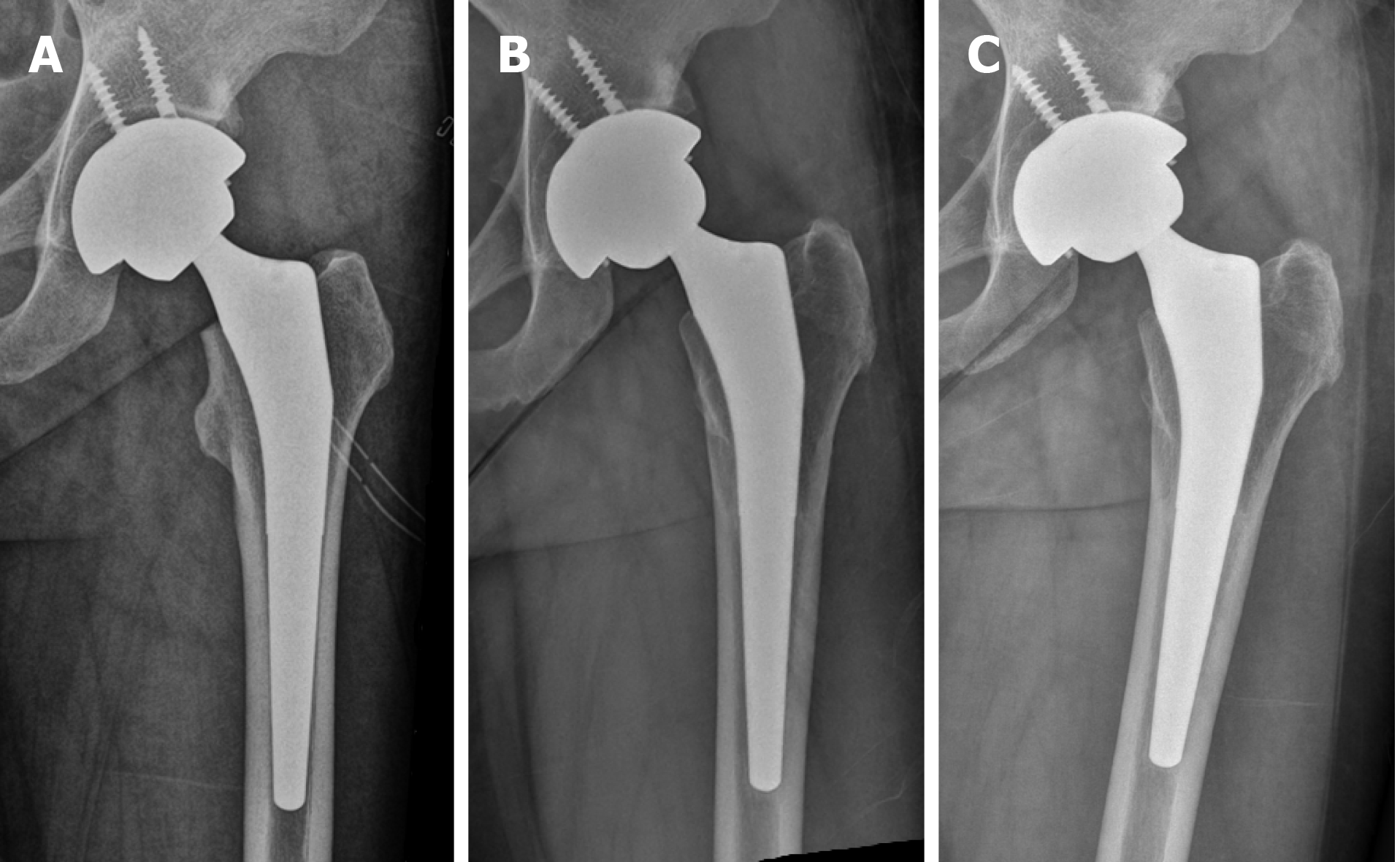
Case 2: The patient underwent THA for osteonecrosis of the femoral head 2 years ago before visiting our institution (Figure 2A). The cementless prostheses implanted were a 56-mm Bencox Hybrid Cup with ID stem (Corentec®, Cheonan, Korea) and 36-mm Biolox® Delta ceramic bearing couples (CeramTec®, Plochingen, Germany).
Case 1: The patient had pain when active hip flexion was more than 30 degrees, and pain was aggravated during passive extension-abduction-external rotation (Patrick test). Passive flexion-adduction-internal rotation (anterior impingement test) and active flexion-internal rotation were not performed due to the risk of posterior dislocation. Flexion muscle power was graded 4 because of pain. The Harris hip score was 80 points. Signs of clinical infection such as erythema and local heat were not observed.
Case 2: She had pain when active hip flexion was more than 30 degrees, and pain was aggravated during Patrick test. Anterior impingement test and active flexion-internal rotation were not performed due to the risk of posterior dislocation. Physical examination revealed a decreased flexion muscle power was graded between 3 and 4. The patient also reported subjective, painless squeaking. The Harris hip score was 75 points. Signs of clinical infection were not demonstrated.
Case 1: Results of routine laboratory tests, including serum erythrocyte sedimentation rate and C-reactive protein levels, were within normal ranges.
Case 2: Results of routine laboratory tests, including erythrocyte sedimentation rate and C-reactive protein levels, revealed no specific abnormality.
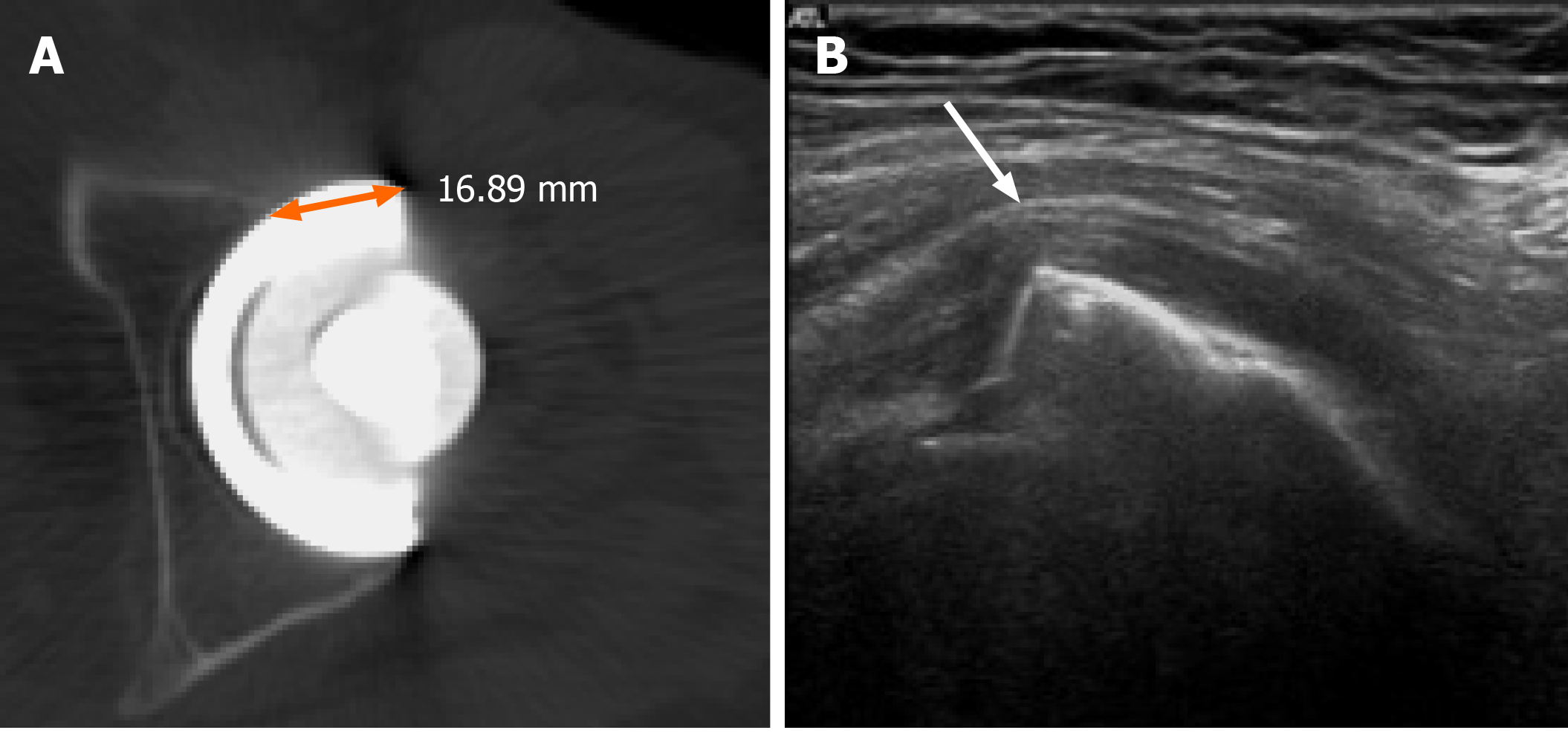
Case 1: Plain radiographs showed insufficient medialization and anteversion angle of the acetabular component, but neither periprosthetic osteolysis nor loosening was demonstrated (Figure 1B). Bone scans showed no abnormal sign, but computed tomography (CT) scans demonstrated reduced anteversion angle of 3 degrees with anterior cup prominence of more than 16 mm (Figure 3A). Ultrasonography showed tenting of the IPT over the anteromedial margin of acetabular component (Figure 3B). A solution containing 1 mL of triamcinolone 40 mg/mL and 4 mL of 0.2% ropivacaine was injected under ultrasonographic guidance into the IPT sheath. After injection, the visual analog scale (VAS) for pain was improved from 8 to 1.
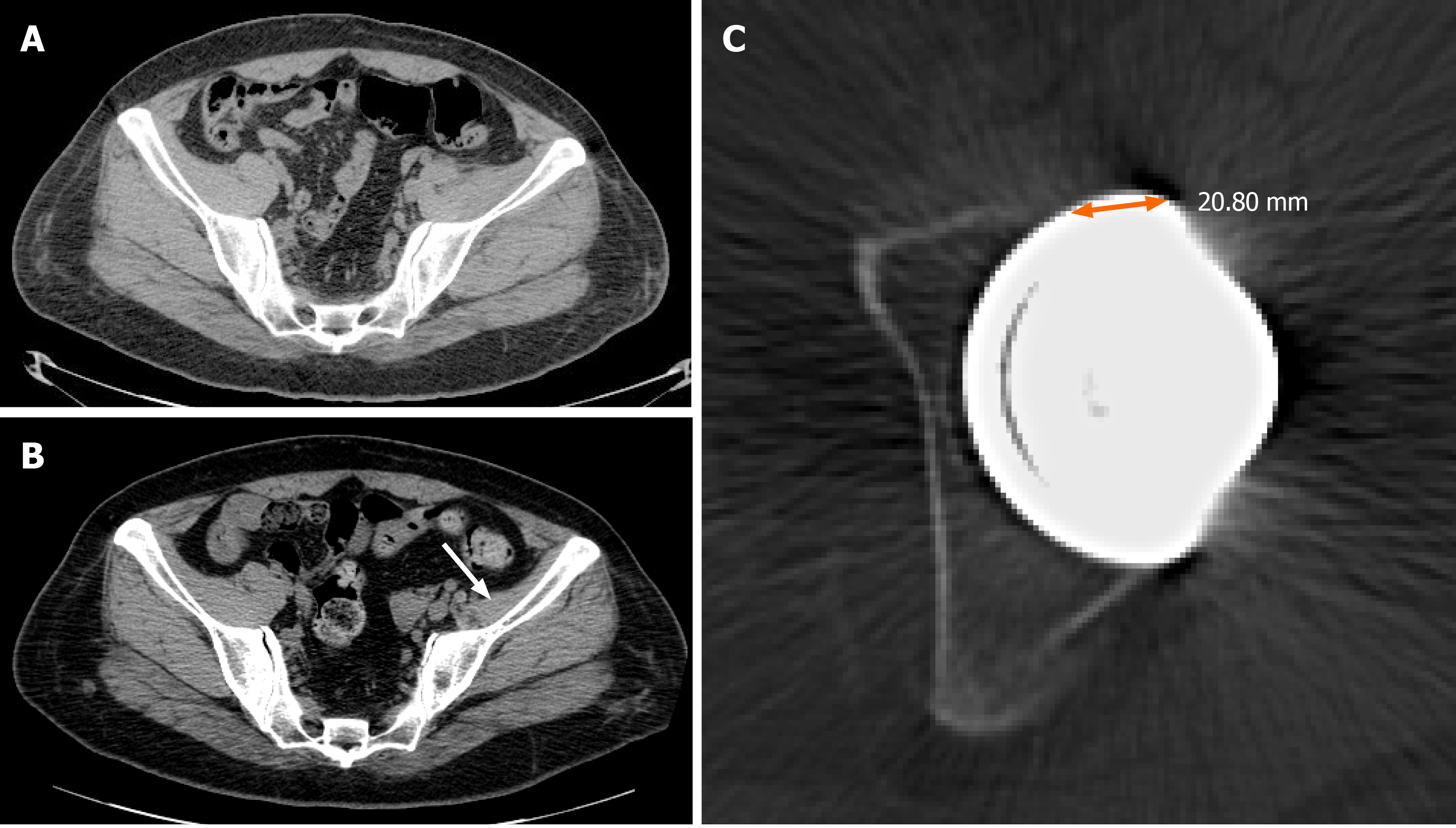
Case 2: Radiographs showed insufficient medialization and decreased anteversion of the acetabular component but not osteolysis or loosening (Figure 2B). Bone scans showed no abnormal sign. In comparison with the CT scan taken immediately after perioperative dislocation (Figure 4A), the CT scan taken 2 years after THA demonstrated atrophy of the left iliacus muscle (Figure 4B) and an anteversion angle of 4 degrees with anterior cup prominence of more than 20 mm (Figure 4C). A solution containing 1 mL of triamcinolone 40 mg/mL and 4 mL of 0.2% ropivacaine was injected under ultrasonographic guidance into the IPT sheath. After injection, the VAS was improved from 7 to 1, and range of motion of the hip joint improved for 1 mo.
Case 1: The final diagnosis was IPT after THA with malpositioned acetabular component.
Case 2: The final diagnosis was IPT after THA with malpositioned acetabular component.
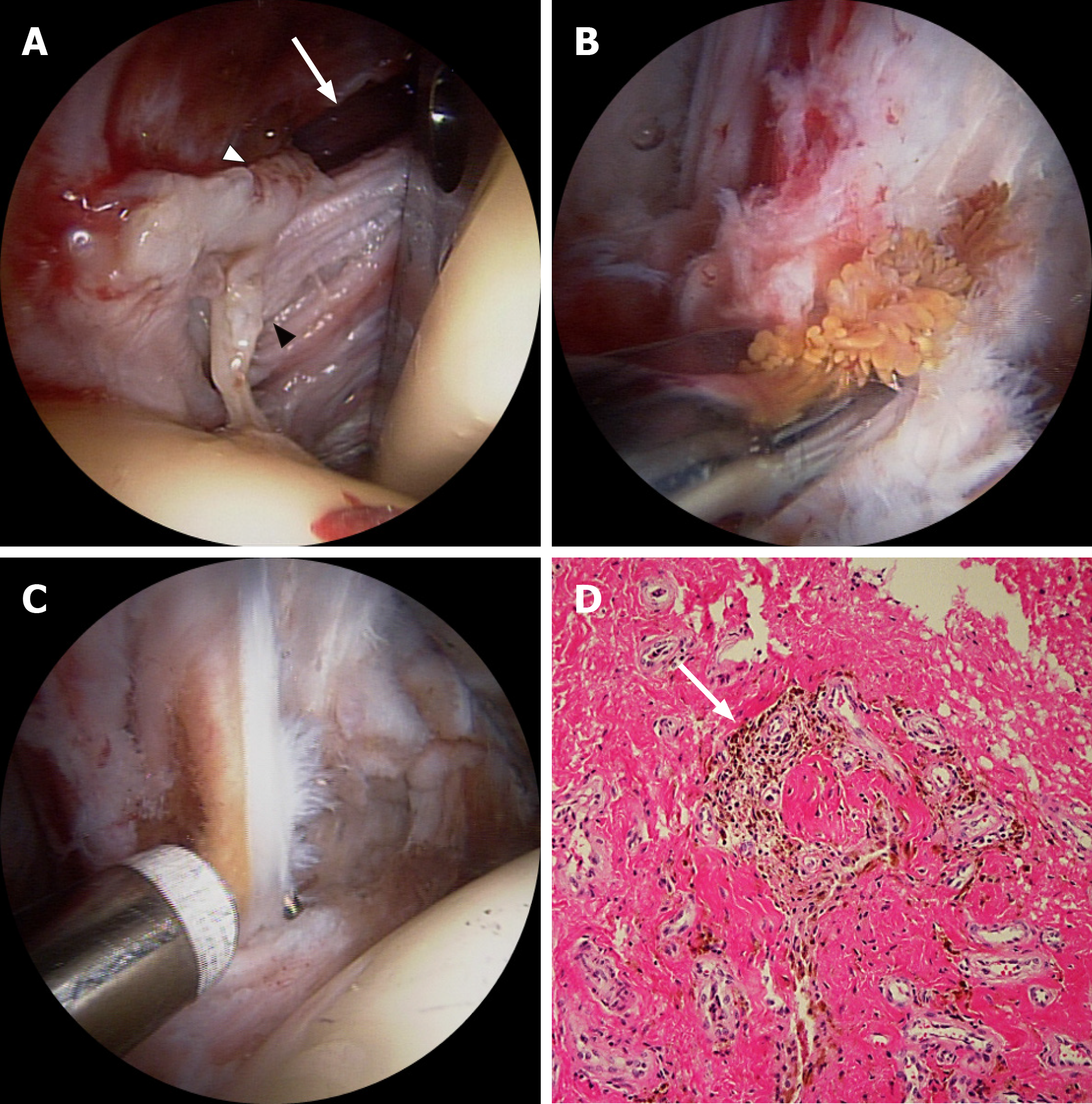
Case 1: In spite of conservative treatment with nonsteroidal anti-inflammatory drugs and analgesics for 3 mo, left groin pain gradually worsened. The patient refused cup revision, and arthroscopic IPT release was planned instead. Dry arthroscopy showed that the capsular opening corresponding to the iliopsoas bursa was enlarged and surrounded by frayed fibrous tissues and dark yellow amorphous materials, which looked like granulation tissue (Figure 5A). With the patient under spinal anesthesia, partial synovectomy with biopsy (Figure 5B), IPT release (Figure 5C), and bursectomy were performed. Because tendon release was performed in the central compartment with applying hip joint traction, any dynamic test to identify impingement between the tendon and anterior edge of the cup was not performed during IPT release. However, after releasing tendon and hip joint traction, IPT tenting over the cup was not demonstrated with hip extension in the peripheral compartment. Histopathologic study showed chronic inflammation with synovial hyperplasia (Figure 5D). There were no neurovascular complications after surgery. The patient was encouraged to start walking immediately after surgery.
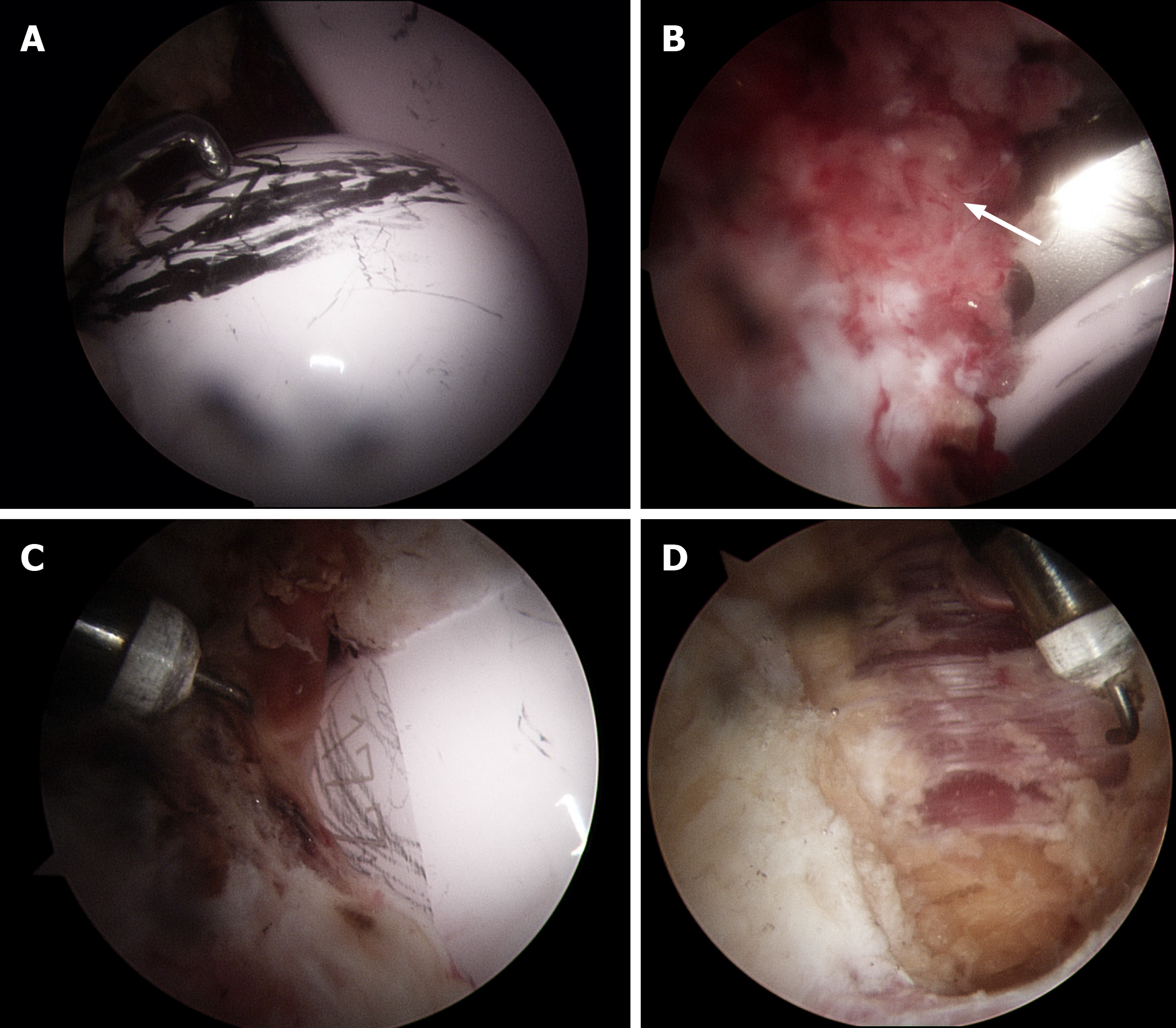
Case 2: Six weeks later, the left groin pain recurred, and arthroscopic IPT release was undertaken after 4 mo of conservative treatment. Arthroscopic evaluation revealed copious metal transfer on the ceramic head, which might have originated from the previous dislocation-and-reduction maneuver (Figure 6A). Metal transfer was also demonstrated on the margin of the liner (Figure 6B) and the bottom of ceramic head (Figure 6C), which might have indicated impingement of the implants on one another. Chronic synovitis underneath IPT was identified (Figure 6B), and tendon release with partial synovectomy was performed (Figure 6D). No dynamic test was performed during procedure, but IPT tenting over the cup was not observed after releasing the traction. Histopathologic study showed chronic synovial inflammation and fibrosis. There were no neurovascular complications after surgery.
Case 1: Groin pain subsided by 6 wk after surgery, and flexion muscle power returned to grade 5 at 6 mo postoperatively. The Harris hip score improved to 96 points 5 years after arthroscopic release, and radiographs taken at the final follow-up visit did not show osteolysis or loosening (Figure 1C).
Case 2: Groin pain subsided at 4 wk postoperatively. Flexor muscle power improved to grade 4 to 5 at 6 mo postoperatively, but did not return completely to the same level as that of the opposite side at the final follow-up visit. The Harris hip score improved from 75 to 97 points, and radiographs showed no abnormal findings 5 years postoperatively (Figure 2C).
Diagnosis and management of IPTs after THA still remain challenging. In the two patients with acetabular cup malposition after THA who underwent arthroscopic IPT release with cup retention, midterm clinical outcomes were excellent, with successful pain relief.
In comparison with open tenotomy, arthroscopic IPT release has many advantages in terms of skin incision, surgical trauma, blood loss, operation time, hospital stay, and rehabilitation[7]; thus it has become popular in the treatment of IPTs after THA. A recent systematic review showed that arthroscopic IPT release after THA was a safe procedure with a higher success rate (92%) than that of open tenotomy (78%)[7].
Anterior cup prominence as a result of reduced anteversion or cup lateralization may hamper IPT excursion and lead to IPTs after THA[2,5,8]. For patients who have IPTs in combination with component malposition, other surgical options have been controversial. Dora et al[6] concluded that open iliopsoas tenotomy was a better option, providing the same final functional results as did revision of protruded acetabular component and avoiding the risks of revision surgery as well. Recently, Chalmers et al[5] reported that open IPT tenotomy was highly successful in patients with minimal cup prominence, whereas acetabular revision was more successful in alleviating groin pain in patients with 8 mm or more of anterior cup prominence.
In theory, acetabular revision in which component position is corrected might be an ideal surgical option, especially for young, active patients with implant malposition, in terms of THA longevity and potential risk for recurrence of groin pain. However, if no serious complications such as recurrent dislocation are present with IPTs after THA, the groin pain is not severe enough for patients to be willing to undergo open procedures, including acetabular revision of a well-fixed cup or even open tenotomy. Moreover, the use of ceramic bearings in THA has become popular for young, active patients because they exhibit less wear and osteolysis, and they might have potential to compensate the negative effect of component malposition on THA longevity. However, in view of the potential risk for recurrence of groin pain as a result of high activity and the need for THA longevity as a result of long life expectancy in these young patients, a well-designed study with a longer duration of follow-up would be necessary to determine the effect of isolated IPT release with retaining a malpositioned cup.
In contrast to the outcomes after open IPT tenotomy reported by Chalmers et al[5], we achieved excellent midterm outcomes without recurrence of groin pain in patients with anterior cup prominence more than 16 mm and 20 mm. In addition to minimal invasiveness, another advantage of arthroscopic procedure over open procedures is that it can help pinpoint the exact location of lesions causing groin pain and other potential problems related to THA. In one patient, our technique demonstrated chronic synovitis with fibrosis or granulation tissue around IPT (Figure 5A and D) and enabled us to perform IPT release and debridement where actual impingement occurred (Figures 5C and 6D). These findings are compatible with a previous report by McCarthy et al[9], who showed anterior scar tissue in 64% of patients with groin pain after THA. On the other hand, open IPT tenotomy, a fundamentally outside-in approach, does not facilitate identifying the exact location of lesions and is usually performed around the insertion site of the IPT. We speculated that these differences were the reasons why arthroscopic release achieved better results than did open tenotomy in patients with more anterior component prominence[5].
Our second patient reported hearing squeaking, and the arthroscopic findings demonstrated copious metal transfer, particularly on the ceramic head, which might have originated from the previous dislocation-and-reduction maneuver (Figure 6A). Although many factors such as liner chipping fracture, metal transfer, micro-separation, edge loading, and impingement were suggested as potential risks[10], the cause, as well as clinical implication, of the squeaking were not determined, and our findings might help to improve our understanding of this phenomenon.
In conclusion, arthroscopic IPT release with cup retention produced excellent midterm outcomes without recurrence of groin pain and implant-related problems in two patients with cup malposition after THA. A well-designed study with longer duration of follow-up would be necessary to determine the effect of this procedure on the recurrence of groin pain and THA longevity, particularly in young, active patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tripathy SK S-Editor: Chen XF L-Editor: A P-Editor: Xing YX
| 1. | Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? BMJ Open. 2012;2:e000435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 866] [Cited by in RCA: 1004] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 2. | Lachiewicz PF, Kauk JR. Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Trousdale RT, Cabanela ME, Berry DJ. Anterior iliopsoas impingement after total hip arthroplasty. J Arthroplasty. 1995;10:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 126] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Nazal MR, Parsa A, Martin SD. Arthroscopic Diagnosis and Treatment of Chronic Hip Pain After Total Hip Arthroplasty and the Role of Anterior Capsule Disruption in Iliopsoas Tendinopathy. Orthop J Sports Med. 2019;7:2325967119854362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Chalmers BP, Sculco PK, Sierra RJ, Trousdale RT, Berry DJ. Iliopsoas Impingement After Primary Total Hip Arthroplasty: Operative and Nonoperative Treatment Outcomes. J Bone Joint Surg Am. 2017;99:557-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Dora C, Houweling M, Koch P, Sierra RJ. Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg Br. 2007;89:1031-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 147] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 7. | O'Connell RS, Constantinescu DS, Liechti DJ, Mitchell JJ, Vap AR. A Systematic Review of Arthroscopic Versus Open Tenotomy of Iliopsoas Tendonitis After Total Hip Replacement. Arthroscopy. 2018;34:1332-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Park KK, Tsai TY, Dimitriou D, Kwon YM. Three-dimensional in vivo difference between native acetabular version and acetabular component version influences iliopsoas impingement after total hip arthroplasty. Int Orthop. 2016;40:1807-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | McCarthy JC, Jibodh SR, Lee JA. The role of arthroscopy in evaluation of painful hip arthroplasty. Clin Orthop Relat Res. 2009;467:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Stanat SJ, Capozzi JD. Squeaking in third- and fourth-generation ceramic-on-ceramic total hip arthroplasty: meta-analysis and systematic review. J Arthroplasty. 2012;27:445-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |