Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.4930
Peer-review started: May 14, 2020
First decision: June 4, 2020
Revised: June 11, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 26, 2020
Processing time: 164 Days and 16.8 Hours
About 90% of perianal infection is caused by cryptoglandular infection. Only a few cases of peritonitis or intra-abdominal abscesses secondary to perforation of the digestive tract by an ingested foreign body have been reported. The most common sites of impaction and perforation include the appendix, cecum and the terminal ileum. The rectum is an unusual site of foreign body impaction. This report intends to highlight that ingested foreign body impacted in the rectum is an extremely rare cause of perianal abscess and subsequent fistula in infants.
Two cases of perianal abscess and fistula due to ingested jujube pit impacted in the rectum are reported. Both cases are infants with free previous medical history suffered from recurrent perianal infection. The caregivers of the two patients denied ingestion of a foreign body or any history of trauma. Physical examination combined with ultrasound or computed tomography scan established the diagnosis. Both of the patients underwent operation under general anesthesia. In case 1, a jujube pit with sharp ends was discovered embedded within a subcutaneous fistula. The jujube pit was then removed intact along with fistula resection. The wound was successfully laid open to allow healing by secondary intention. In case 2, a jujube pit was found with its sharp end puncturing the rectum, surrounded by pus and necrotic tissue. Subsequent incision and adequate drainage were performed. The whole jujube pit was then removed from the abscess cavity at the same time. Both patients received colonoscopy to rule out inflammatory bowel disease or other potential damages by the ingested jujube pit. The postoperative period was uneventful. At 1.5 year follow-up, no recurrent abscess or fistula were found in either patient.
An impacted foreign body must not be overlooked as an unusual cause of perianal abscess and fistula, especially in young children.
Core Tip: A vast majority of perianal abscesses and subsequent fistula are caused by an infection in the anal glands. Impaction of an ingested foreign body in the rectum is an extremely rare cause of perianal abscess and subsequent fistula formation in an infant. This report intends to highlight the ultimate importance of assuring every object accessible to kids is appropriate for their age to avoid potentially serious complications. Also, impacted foreign bodies should not be overlooked as an unusual cause of perianal infection especially in refractory cases.
- Citation: Liu YH, Lv ZB, Liu JB, Sheng QF. Perianorectal abscesses and fistula due to ingested jujube pit in infant: Two case reports. World J Clin Cases 2020; 8(20): 4930-4937
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/4930.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.4930
A perianal abscess is a collection of pus under the skin around the anus. About 90% of these cases are caused by an infection in the anal glands[1]. Approximately 10% of perianal abscesses are not caused by infected anal glands and result from conditions such as: Skin appendage infection; Crohn’s disease; tuberculosis; trauma; chronic inflammation and infection of sweat glands (hidradenitis suppurativa); human immunodeficiency virus infection; sexually transmitted diseases; radiation therapy; malignancy; and foreign bodies[1].
Foreign body ingestion is a worldwide problem. According to the literature, 80%-90% of ingested foreign bodies will pass through the entire alimentary canal uneventfully[2]. However, foreign bodies may become lodged in areas of normal narrowing or curvatures, such as the upper esophageal sphincter, mid esophagus (crossover of aorta), lower esophageal sphincter, pylorus, ligament of Treitz, Meckel’s diverticulum, ileocecal valve and appendix[3-5], which may lead to alimentary canal perforation and subsequent abscess and fistula formation. The rectum is a very unusual site of foreign body impaction by ingestion.
Two reports have been published detailing the cases of adults who had a foreign body impacted in the rectum that migrated to the perianal tissues, which subsequently led to the development of perianal abscess and fistula formation[6,7]. We present herein, the first two cases of perianal abscess and subsequent fistula caused by an ingested jujube pit in infants, discuss management and review the literature.
Case 1: Perianal pain and purulent discharge.
Case 2: Perianal pain, purulent discharge, intermittent fever, decreased appetite and inconsolable crying.
Case 1: A 2-year-old girl with refractory perianal abscess for 6 mo was presented to our pediatric surgery clinic. Six months ago, the patient underwent an abscess incision and drainage at a local hospital after being diagnosed with a perianal abscess. There was pus discharged through the incision almost every day although she received dressing change regularly.
Case 2: A 14-month-old boy was taken to our pediatric emergency department after 23-d history of perianal pain and purulent discharge during defecation. He was also noted to have intermittent fever (highest 38.5 ºC), decreased appetite and inconsolable crying.
Both of the two patients had a free previous medical history.
Both of the patients did not have a history of perianal abscess or perianal trauma before or any family history of inflammatory bowel disease, immunosuppression or immune deficiency.
Case 1: Vitals: Within normal limits; General: Alert, cooperative; Abdomen: Soft, nontender, bowel sounds normal, no masses, no organomegaly; Careful inspection of her perianal region revealed an external opening at 8 o’clock on supine lithotomy position. Digital rectal examination showed no sign of internal opening but with only minimal discomfort. The remainder of the physical examination was normal.
Case 2: Vitals: Within normal ranges; General: Alert, uncooperative; Abdomen: Soft, nontender, bowel sounds normal, no masses, no organomegaly. There was an infectious foci at 1-3 o’clock on supine lithotomy position, which was localized with a size of 3 cm × 3 cm × 2 cm, tender, erythematous swellings, and there was pus discharge through anus when the lesion was pressed. Digital rectal examination was impossible due to severe pain. The remainder of the physical examination was normal.
In both patients, the complete blood count and stool examination were within normal ranges as were the serum complement and levels of immunoglobulin. Serology tests for human immunodeficiency virus, rapid plasma reagin tests and T-SPOT.TB test were all negative. Pus cultures for Escherichia coli were positive in both patients.
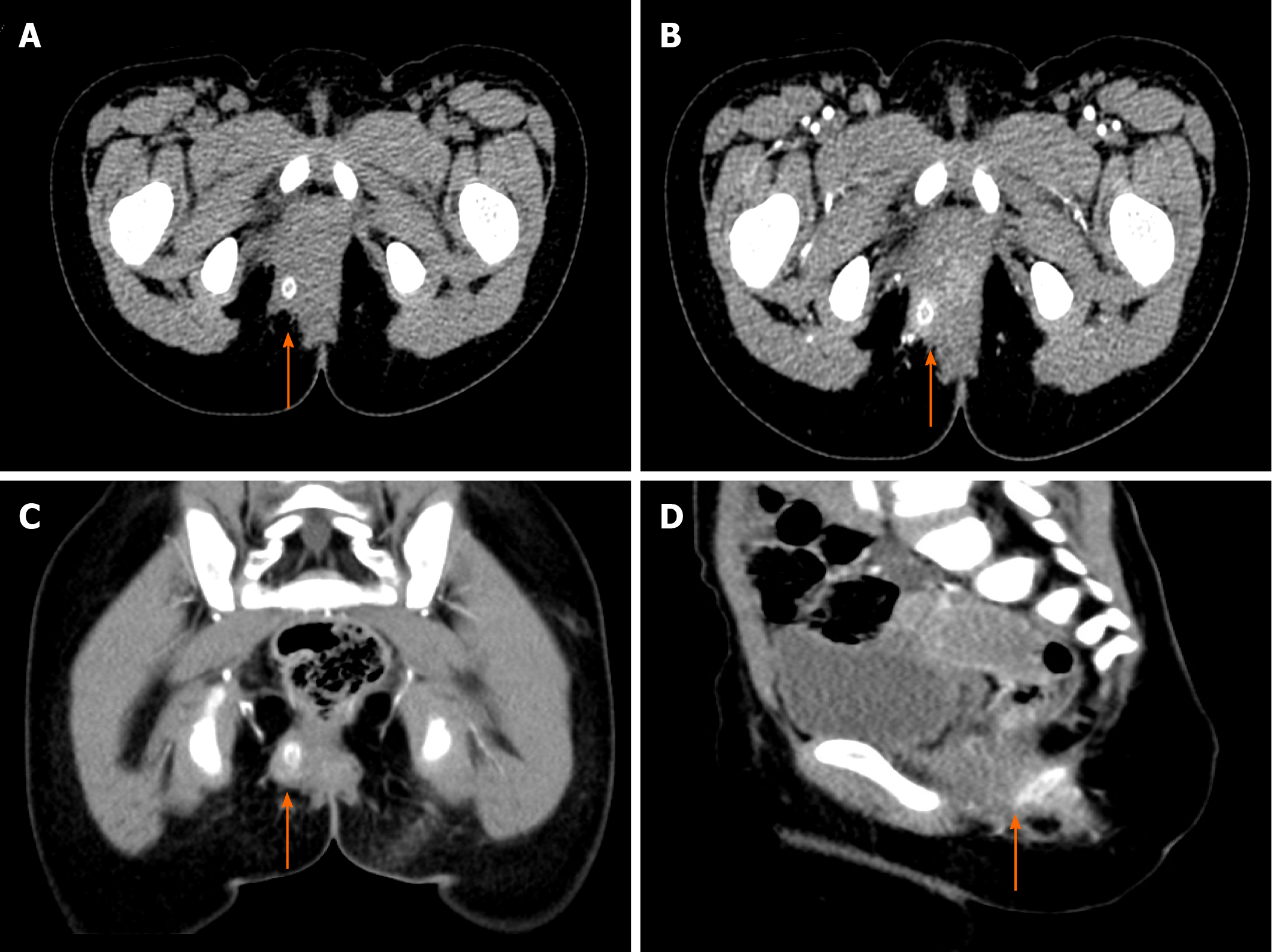
Case 1: An initial pelvic computed tomography (CT) scans with intravenous contrast media administration revealed a perianal fistula with a foreign object inside it (Figure 1).
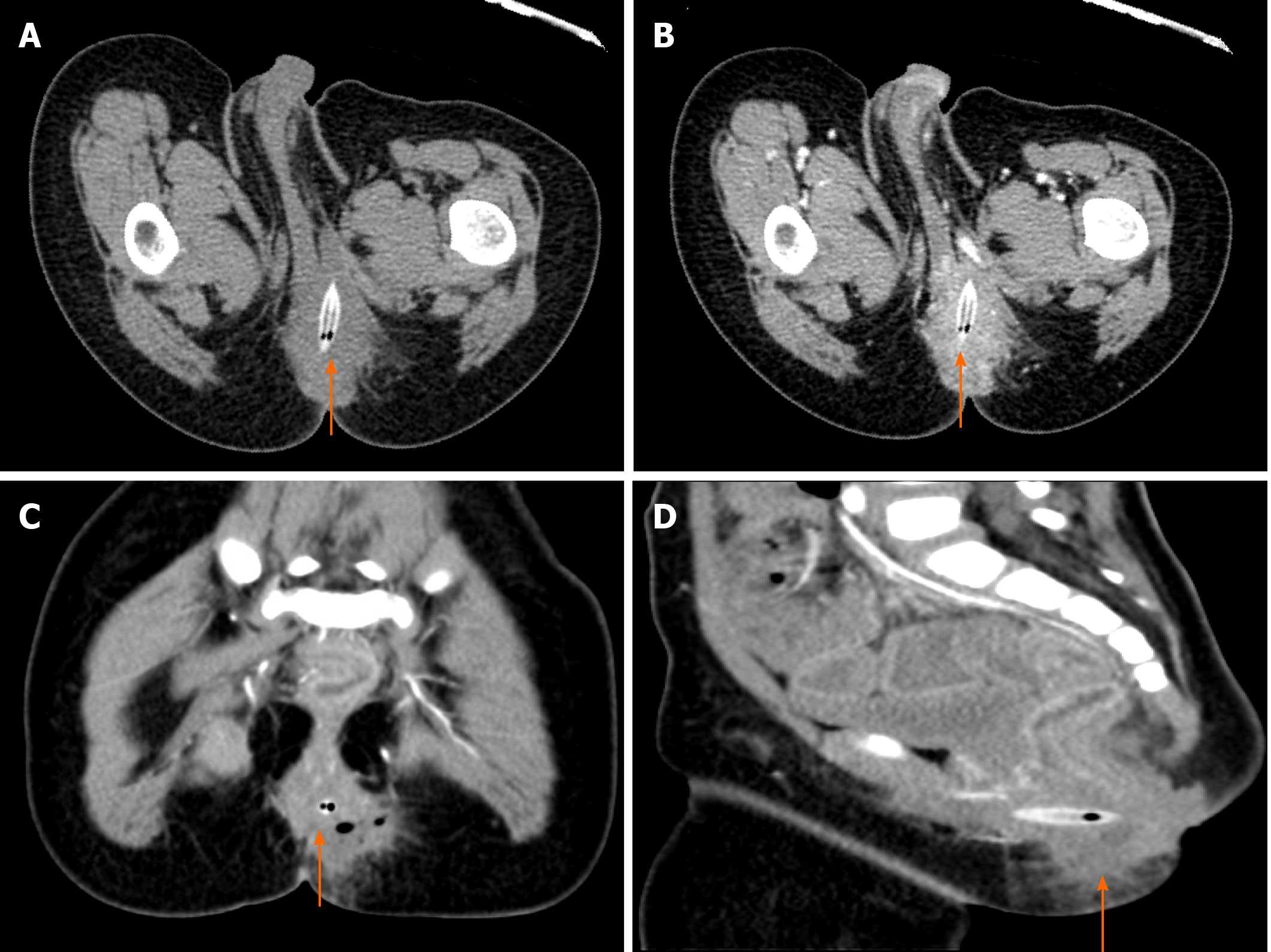
Case 2: An initial ultrasound showed an inflammatory lesion in subcutaneous tissue near the anus, which contained gas. The gas came in and out of the anus when he cried. The lesion was further evaluated with a pelvic CT scan. The latter revealed the pointed end of the foreign body exceeded the rectum wall and punctured the neighboring tissue, which showed significant brim enhancement in intravenous contrast-enhanced images (Figure 2).
Both patients were further evaluated for potential underlying disease with colonoscopy because perianal abscesses and fistula are potential complications in Crohn’s disease.
Case 1: On colonoscopy, the colon displayed normal anatomy with no evidence of inflammatory bowel disease or internal opening.
Case 2: A jujube pit was found with its sharp end puncturing the rectum wall surrounded by pus and necrotic tissue.
The final diagnosis of the presented patient in case 1 was perianal fistula due to impacted foreign body (FB).
The final diagnosis of the presented patient in case 2 was perianal abscess due to impacted jujube pit.
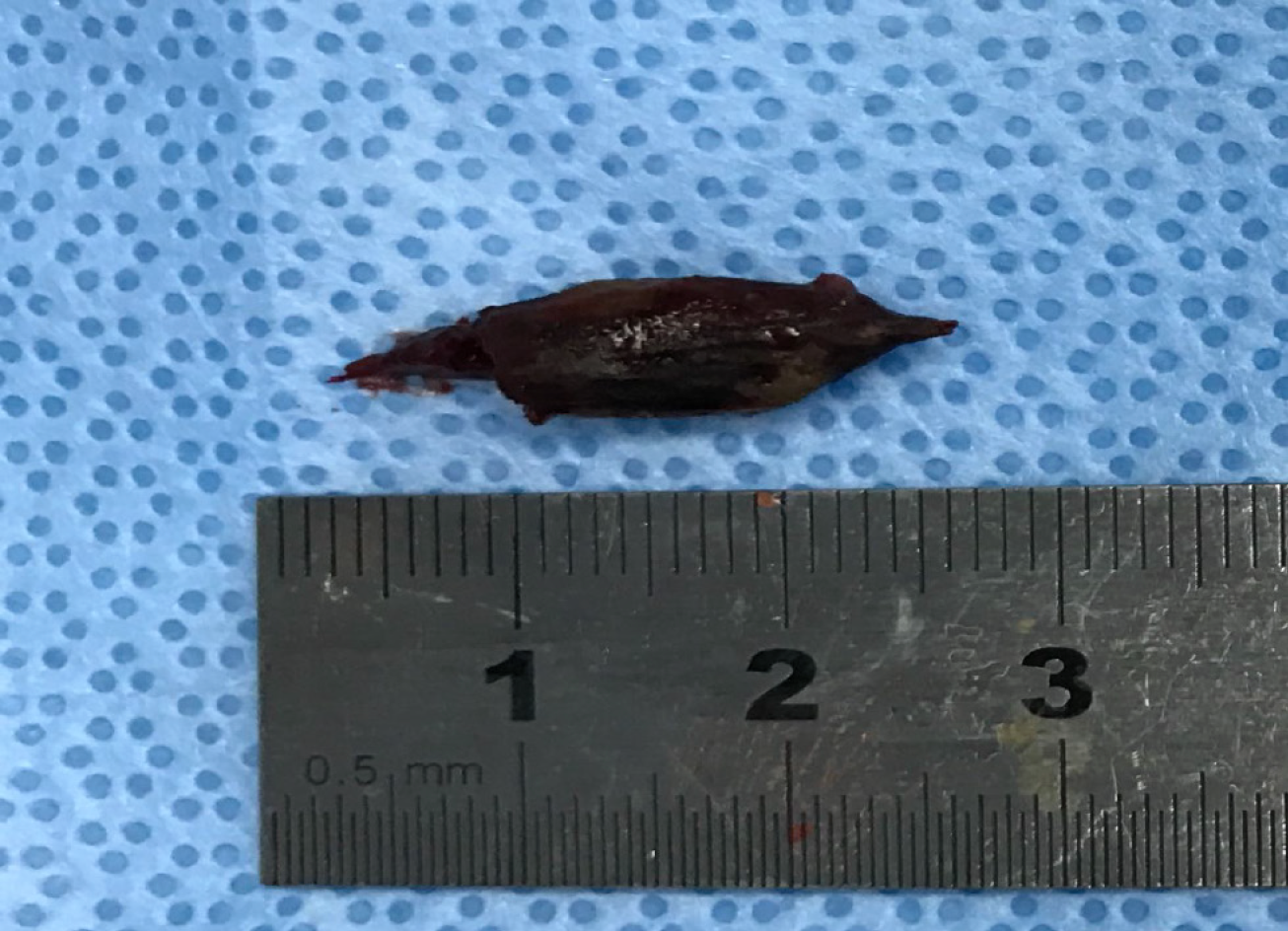
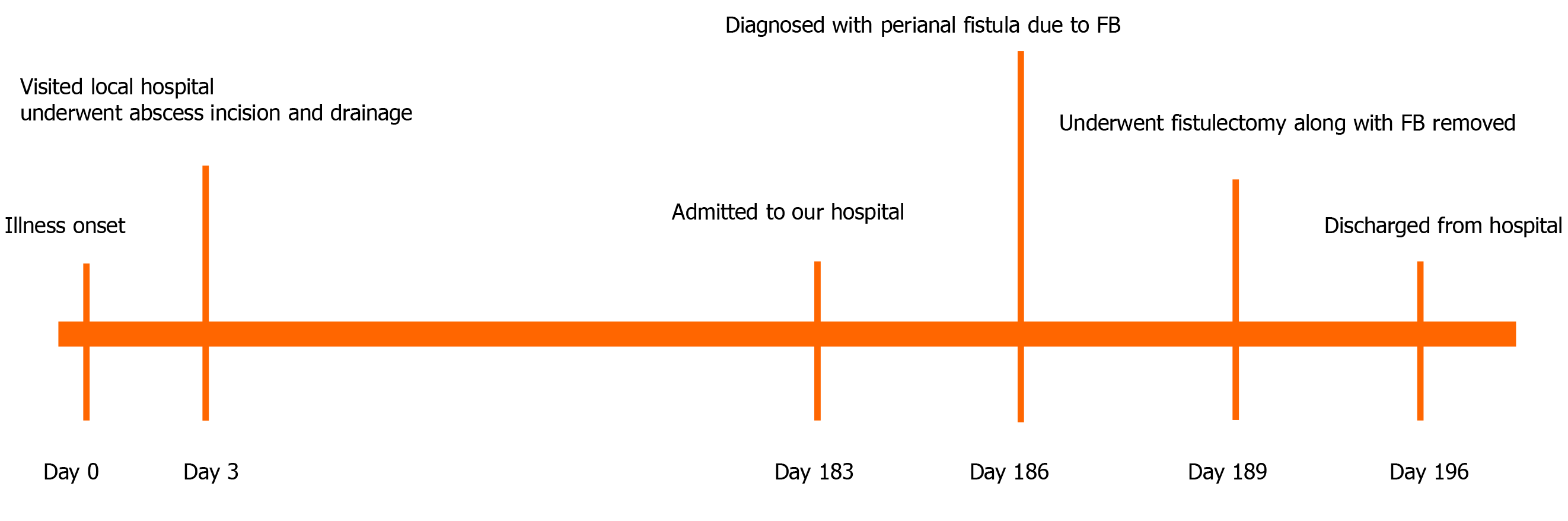
After adequate bowel preparation, the patient underwent an operation in a supine lithotomy position under general anesthesia. Then a probe was inserted through the external opening for about 4 cm. A subcutaneous fistula was demonstrated through the passage onto the external opening. A 3 cm jujube pit (Figure 3) with sharp ends was discovered embedded within the fistula. The jujube pit was then removed intact from the fistula with long forceps. Subsequently, the patient underwent fistula resection and the wound was successfully laid open to allow healing by secondary intention. The patient was then discharged without complication one week after the surgery (Figure 4).
Case 2: After examination, intravenous broad-spectrum antibiotic (cefoperazone-sulbactam combined with metronidazole) therapy was administered to the patient initially. After adequate preparation for surgery, the patient underwent emergent surgical exploration under general anesthesia. Intraoperatively, the abscess was drained, and the whole jujube pit was then removed from the abscess cavity. Pus as well as the necrotic tissue was then cleared. The abscess cavity was lavaged with 3% hydrogen peroxide and packed to heal by secondary intention. Pus culture grew Escherichia coli 4 d after sampling, which was sensitive to the antibiotics we used. The patient was then discharged from hospital free of symptoms on the sixth hospital day (Figure 5).
Postoperative pathology confirmed a fistula. The postoperative course was uneventful. Fortnightly follow-up was undertaken at the outpatient department until the cavity closed and the skin re-epithelialized, which constituted healing. At 2 yrs follow-up, no recurrent abscess or fistula was found.
The patient did well after surgery. At 1.5 yrs follow-up, no recurrent abscess or fistula was found.
Perianal abscesses are mostly caused by cryptoglandular infection, especially for infants, with peak onset at ages < 1 year. Impacted FB in the rectum by ingestion is an extremely rare cause of perianal abscess and subsequent fistula formation. In our patients, ingested jujube pit with sharp ends did penetrate through the rectum wall to lodge in the perianal tissues, which subsequently led to the development of perianal abscess and fistula formation.
Pediatric FB ingestion is a common and serious problem worldwide with a peak of incidence between 6 mo and 4 yrs in relation to the oral stage of learning, inadequate dentition, the relatively high position of the epiglottis, immature swallowing coordination and the inability to distinguish edible objects from nonedible ones[3,8,9]. Although a vast majority of swallowed FBs pass naturally through the gastrointestinal tract without complications or damage, sharp objects (including jujube pit in our cases) do pose a high risk of mucosal injury. Adverse events may include perforation, abscess, fistula, peritonitis or generalized septicemia and even death[2,8,9]. Therefore, early diagnosis and prompt management are of great importance to prevent morbidity and mortality.
However, despite the severity of this type of injury, the availability of high quality evidence on perianal abscess resulting from impacted jujube pit by ingestion is lacking. Most of the available data come from the publication of single case studies. Clinical presentation differs in each of the studies. At present, we could not identify any specific clinical manifestation related to perianal abscess caused by jujube pit ingestion from the published literature.
Traditional approaches to diagnose rectum jujube pit impaction including physical examination and plain radiograph may be ineffective. Digital rectal examination might be an easy and effective approach to reveal the presence of an abscess but often fails to detect the presence of a FB in the abscess cavity[10]. Imaging methods are of paramount importance in identifying the exact location of the FB impaction. It is important for patients with a history or suspicion of FB ingestion to undergo radiographic evaluation because the majority (83%) of FBs in the current investigation were radiopaque[11]. In addition to a high sensitivity and specificity, CT may provide more useful information than plain radiograph not only for the existence and the location of ingested FBs but also for the detection of any resulting damage to neighboring structures[3,12]. However, regarding the radiation, X-rays and CT scan are only indicated when impaction of an ingested FB is suspected. As for the radiolucent object, the ultrasound may be a better option.
Management of perianal abscess resulting from jujube pit impaction should focus on early incision and adequate drainage of the abscess along with removal of the FB. If there is a fistula, resection or laid open is also needed. Antibiotics are recommended in patients with systemic symptoms. Once the abscess is clinically evident, urgent drainage on the day of presentation is required because of the risk of deep infection, sepsis and necrotizing soft tissue infection[13]. If there is no evidence of systemic sepsis, incision and drainage is usually done immediately at the outpatient department after infiltration of the area with 1% lidocaine. Local anesthesia is generally less effective in the presence of inflammation. Thus adequate exploration of the abscess cavity is not allowed, which may miss the underlying cause of the abscess such as impacted FBs. If the jujube pit ingestion is not witnessed, the absence of specific symptoms and signs indicating the occurrence of jujube pit impaction may lead to a significant delay in diagnosis and in management, thereby increasing the risk of complications, especially in young children[9].
Undoubtedly, primary prevention is the most effective way to prevent injuries from FB ingestion. Given the risk of misdiagnosis of FB injuries due to nonspecific clinical presentation and the severity of complications to which a FB injury may be associated, it is crucial to develop primary prevention strategies for FB injuries. In particular, educational programs should be carried out for parents and caregivers to stress the importance that every substance (including food) accessible to children is appropriate for their age (e.g. avoiding nuts and seeds and more generally small objects that could be swallowed or inhaled in children younger than four years of age, guaranteeing adult supervision when kids are eating or playing). Hazardous objects must be stored in childproof containers. Primary prevention is also represented by the involvement of manufacturers and consumer associations to provide strict regulation on manufacturing, packaging and commercialization of hazardous objects[3,9].
To the best of our knowledge, this is the first report of perforation of the rectum by an ingested FB (jujube pit) followed by migration of the FB to the surrounding space, which resulted in perianal abscess and fistula formation in infants. Children are prone to ingest substances due to their exploratory nature and tendency to put everything in the mouth. Impacted FB must not be overlooked as an unusual cause of perianal infection. Once treated, emphasis must be placed upon prevention of recurrence, which includes meticulous history-taking, careful examination, adequate exposure of the abscess cavity and education of patient and caretakers[9,10].
Ingested FB is a rare but significant cause of perianal abscess and fistula. Only scarce reports of perianal abscess and fistula resulted from FB impacted in rectum and migrated to the perianal tissues have been previously published, all in adults[6,10]. To our knowledge, this is the first cases of perianal abscess and subsequent fistula caused by ingested jujube pit in infants reported in the literature. This report intends to highlight the ultimate importance of ensuring every object accessible to kids is appropriate for their age to avoid potentially serious complications and second, impacted FBs should not be overlooked as an unusual cause of perianal infection especially in refractory cases[6].
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coskun A S-Editor: Zhang L L-Editor: Filipodia P-Editor: Wang LL
| 1. | Smith SR, Newton K, Smith JA, Dumville JC, Iheozor-Ejiofor Z, Pearce LE, Barrow PJ, Hancock L, Hill J. Internal dressings for healing perianal abscess cavities. Cochrane Database Syst Rev. 2016;CD011193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Gurevich Y, Sahn B, Weinstein T. Foreign body ingestion in pediatric patients. Curr Opin Pediatr. 2018;30:677-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Hesham A-Kader H. Foreign body ingestion: children like to put objects in their mouth. World J Pediatr. 2010;6:301-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Wong JH, Suhaili DN, Kok KY. Fish bone perforation of Meckel's diverticulum: a rare event? Asian J Surg. 2005;28:295-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Hartin CW, Lau ST, Caty MG. Metallic foreign body in the appendix of 3-year-old boy. J Pediatr Surg. 2008;43:2106-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Delikoukos S, Zacharoulis D, Hatzitheofilou C. Perianal abscesses due to ingested foreign bodies. Int J Clin Pract. 2005;59:856-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Juth Karlsson A, Salö M, Stenström P. Outcomes of Various Interventions for First-Time Perianal Abscesses in Children. Biomed Res Int. 2016;2016:9712854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Grassi R, Faggian A, Somma F, De Cecco CN, Laghi A, Caseiro-Alves F. Application of imaging guidelines in patients with foreign body ingestion or inhalation: literature review. Semin Ultrasound CT MR. 2015;36:48-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Passali D, Gregori D, Lorenzoni G, Cocca S, Loglisci M, Passali FM, Bellussi L. Foreign body injuries in children: a review. Acta Otorhinolaryngol Ital. 2015;35:265-271. [PubMed] |
| 10. | Kocierz L, Leung E, Thumbe V. An unusual cause of perianal fistula. J Surg Case Rep. 2011;2011:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Sink JR, Kitsko DJ, Mehta DK, Georg MW, Simons JP. Diagnosis of Pediatric Foreign Body Ingestion: Clinical Presentation, Physical Examination, and Radiologic Findings. Ann Otol Rhinol Laryngol. 2016;125:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Ozbilgin M, Arslan B, Yakut MC, Aksoy SO, Terzi MC. Five years with a rectal foreign body: A case report. Int J Surg Case Rep. 2015;6C:210-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK. Perianal abscess. BMJ. 2017;356:j475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (1)] |