Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.4807
Peer-review started: June 19, 2020
First decision: August 23, 2020
Revised: August 26, 2020
Accepted: September 11, 2020
Article in press: September 11, 2020
Published online: October 26, 2020
Processing time: 129 Days and 8.1 Hours
Acute traumatic spinal cord injury (ATSCI) usually results in disability, yet data on contemporary national trends of ATSCI incidence are limited.
To provide a systematic and basic theoretical basis for improving the treatment of acute spinal cord injury.
Data from the Peking University Third Hospital Inpatient Sample databases were analyzed. A total of 304 patients with ATSCI were included from 2012 to 2017. The epidemiological data, treatment, complications and clinical outcomes of these patients were reviewed.
Of the 304 patients, 257 (84.5%) were male, and 75% of the patients were 55 years old or younger. 135 patients had improved follow-up American Spinal Injury Association (ASIA) grades (44.4%). Only 14 patients with ASIA grade A improved. A statistically significant difference in prognosis between patients who underwent surgery within 72 h and those who underwent surgery after 72 h was observed (P < 0.05). Surgery within 72 h resulted in better prognosis. The Steroid group and the Non-Steroid group showed a significant difference in outcome among patients with ASIA grades A and B (P < 0.05). Patients with pneumonia had a poorer prognosis than patients without pneumonia (P < 0.05). Surgery within 72 h resulted in better prognosis.
This study found that there was no significant difference in hospitalization time and prognosis between the Steroid group and the Non-Steroid group, but the patients with severe spinal cord injury (ASIA grades A and B) who underwent surgery combined with steroid therapy had a better prognosis than those who underwent surgery alone. The disastrous consequences of ATSCI and lack of consensus on the management strategy are obvious. Further improvements in treatment planns are needed in order to obtain more reliable functional outcomes.
Core Tip: Our study describes the present treatment of acute traumatic spinal cord injury. This study found that surgery within 72 h resulted in a better prognosis. Patients with American Spinal Injury Association (ASIA) grades A and B had a significantly better prognosis when treated with steroids. The present study demonstrates that patients with severe spinal cord injury (ASIA grades A and B) may benefit from early surgery and steroid administration. These findings have implications for future clinical practice.
- Citation: Tian C, Lv Y, Li S, Wang DD, Bai Y, Zhou F, Ma QB. Factors related to improved American Spinal Injury Association grade of acute traumatic spinal cord injury. World J Clin Cases 2020; 8(20): 4807-4815
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/4807.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.4807
Acute spinal cord injury (ASCI) is a common type of severe trauma in the emergency department, which results in catastrophic consequences for patients. The vast majority of patients are disabled due to severe neurological damage, or can even result in fatalities. This places an enormous financial burden and emotional stress on families and society.
The most recent model systems estimate of 12500 new cases per year was revised recently from 11000 new cases per year based on the increase in the United States population. The number of individuals with acute traumatic spinal cord injury (ATSCI) is increasing, mostly in young and middle-aged men[1]. Patients get paralyzed or even die, causing huge medical and economic burdens on families and society.
Research in this area is extensive, including the continuous improvement in surgical techniques and protocols, the clinical application of hormones, clinical research on drugs to protect and promote nerve growth, and the exploration of emerging stem cell transplantation treatments, etc[2-7]. However, there is currently no mature and effective measures that can improve the patient's functional outcome[8,9].
This article reviews the epidemiology and treatment of patients with ATSCI in our hospital over the past 5 years, in order to provide a systematic and basic theoretical basis for improving the treatment of ASCI.
A single-center retrospective cohort study was conducted in an urban tertiary hospital. Patients with ATSCI were recruited from 2012 to 2017 using the following inclusion and exclusion criteria: (1) Age > 18 years old; (2) ASCI diagnosed based on American Spinal Injury Association (ASIA) criteria; (3) ASIA grade A to D; and (4) Surgical intervention during hospital stay. Patients with acute cerebrovascular disease were excluded. The patients were followed-up at one year after discharge, the ASIA score was recalculated, and the recovery of neurological function was evaluated according to the ASIA criteria.
Statistical data processing was performed using SPSS 22.0 (IBM Inc., Armonk, NY, United States). Analysis of variance (ANOVA) was used for measurement data. The t-test was used for quantitative data, and the Chi-square test was used for categorical data. P < 0.05 was considered statistically significant.
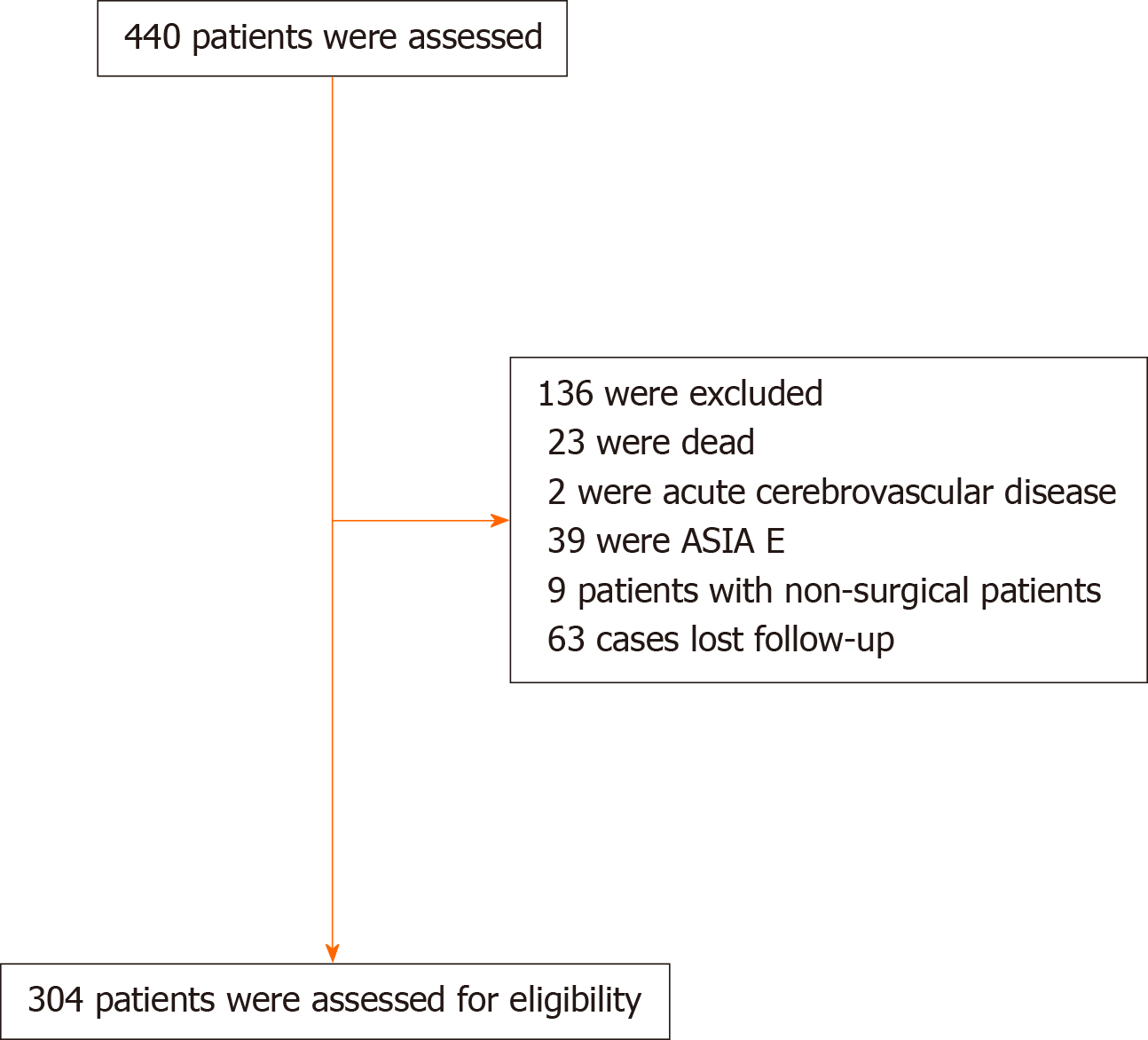
There were 440 ATSCI patients enrolled in the study. A total of 304 cases were included in the final analysis (Figure 1). Patient demographics are shown in Table 1.
| Total (n = 304) | Improved (n = 135) | Not-improved (n = 169) | P value | |
| Demographics | ||||
| Male, n (%) | 257 (84.5) | 111 (82.2) | 146 (86.4) | 0.318 |
| Age, yr (mean ± SD) | 49.81 ± 13.03 | 50.47 ± 12.78 | 49.28 ± 13.24 | 0.67 |
| Co-morbidity, n (%) | 92 (32.2) | 38 (28.8) | 53 (31.4) | 0.455 |
| ASCI characteristics | ||||
| Etiology, n (%) | 0.456 | |||
| Motor vehicle crashes | 90 (29.6) | 41 (30.4) | 49 (29.0) | |
| High-altitude fall injuries | 37 (12.2) | 13 (9.6) | 24 (14.2) | |
| Unintentional falls | 136 (44.7) | 66 (48.9) | 70 (41.4) | |
| Bruise by heavy object | 19 (6.3) | 6 (4.4) | 13 (7.7) | |
| Other | 22 (7.2) | 9 (6.7) | 13 (7.7) | |
| Multiple trauma, n (%) | 41 (13.5) | 13 (9.6) | 28 (16.6) | 0.078 |
| Fracture, n (%) | 137 (45.1) | 52 (38.5) | 85 (50.3) | 0.040a |
| Region of fracture, n (%) | 0.042a | |||
| Cervical | 269 (88.5) | 126 (93.3) | 143 (84.6) | |
| Lumbar | 24 (7.9) | 5 (84.6) | 19 (11.2) | |
| Thoracic | 11 (3.6) | 4 (3.0) | 7 (4.1) | |
| ASIA grade at admission | 0.0 | |||
| A | 78 (25.7) | 14 (10.4) | 64 (37.9) | |
| B | 33 (10.9) | 16 (11.9) | 17 (10.1) | |
| C | 66 (21.7) | 47 (34.8) | 19 (11.2) | |
| D | 127 (41.8) | 58 (43.0) | 69 (40.8) | |
| Time from event to visit | 3.06 ± 2.13 | 2.7 ± 1.96 | 32.9 ± 2.20 | 0.019a |
| Treatment (h) | ||||
| Time from event to surgery | 0.005c | |||
| Within 72 h | 133 (43.8) | 71 (52.6) | 62 (36.7) | |
| After 72 h | 171 (56.3) | 64 (47.4) | 107 (63.3) | |
| Steroid usage | 208 (68.4) | 87 (64.4) | 169 (71.6) | 0.182 |
| Complications | 100 (32.9) | 33 (24.4) | 67 (39.6) | 0.005c |
| Hospital stay (d) | 9.89 ± 10.11 | 7.79 ± 5.92 | 11.55 ± 12.25 | 0.002c |
| ICU admission, n (%) | 95 (31.3) | 34 (25.2) | 61 (36.1) | 0.041a |
ATSCI was more common among young and middle-aged men. The most common injury site was the cervical spinal cord. Falls and motor vehicle crashes were the two most common causes. The study found that patients with fracture had a worse prognosis than patients without fracture (P < 0.05). A shorter time from onset to treatment resulted in a better prognosis (P < 0.05).
In addition to preventive antibiotic therapy, other treatments such as proton pump inhibitors (PPIs), nutritional supplements and analgesia were administered. All patients underwent surgical treatment with 133 patients undergoing surgery within 72 h. 208 patients were treated with steroids (Table 2), and 44 patients were treated with high-dose steroids. 243 patients were treated with mannitol.
| Steroid | Non-steroid | P value | |
| Average hospitalization days | 10.32 ± 11.4 | 8.94 ± 6.4 | 0.117 |
| Average hospitalization days in ICU | 10.75 ± 11.9 | 7.68 ± 6.3 | 0.095 |
| Mean dose of steroids (mg/d) | |||
| Dexamethasone | 15.20 ± 5.0 | ||
| Methylprednisolone | 286.02 ± 213.4 | ||
| Total dose of steroids (mg) | |||
| Dexamethasone | 42.66 ± 23.5 | ||
| Methylprednisolone | 833.96 ± 717.8 |
There was no significant difference in mean hospitalization days or length of intensive care unit stay between the Steroid group and the Non-Steroid group (P > 0.05). There were no significant differences in the average number of hospitalization days and prognosis between the high-dose steroid group and the low-dose steroid group (P > 0.05).
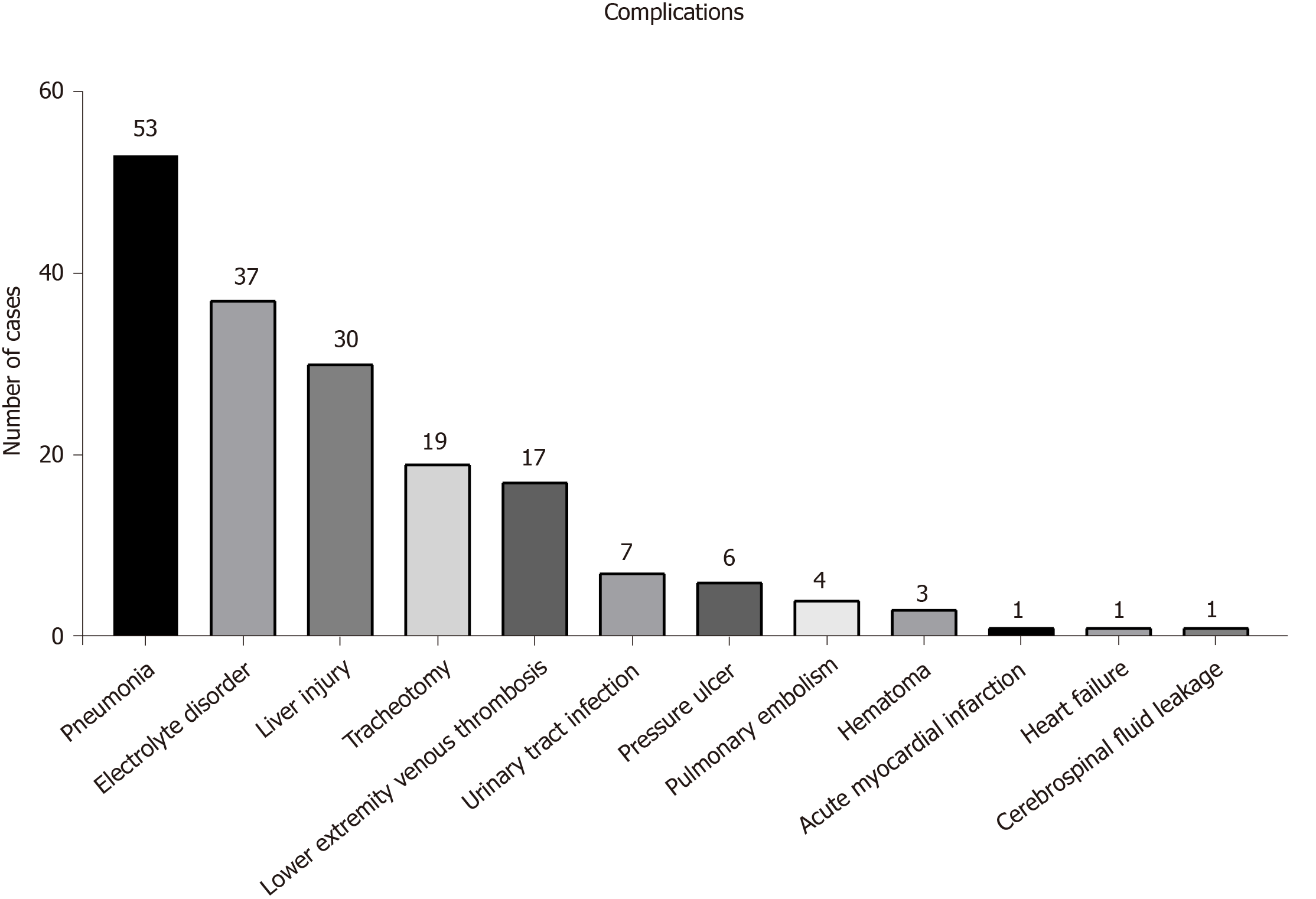
There was a difference in the prognosis between patients with complications and those without complications (P < 0.05). The presence of complications during hospitalization was documented, and included 53 cases of pneumonia, 37 cases of electrolyte disorder, 30 cases of liver injury, 19 cases of tracheotomy, 17 cases of lower extremity deep venous thrombosis, 7 cases of urinary tract infection, 6 cases of stress ulcer, 4 cases of pulmonary embolism, 3 cases of hematoma, 1 case of acute myocardial infarction, 1 case of heart failure, and 1 case of cerebrospinal fluid leakage (Figure 2). The presence of a significant association between common complications and steroid use is shown in Table 3.
| Steroid | Non-steroid | P value | |
| Pneumonia (n = 53) | 46 | 7 | 0.002c |
| Electrolyte disturbances (n = 37) | 29 | 8 | 0.164 |
| DVT (n = 17) | 11 | 6 | 0.734 |
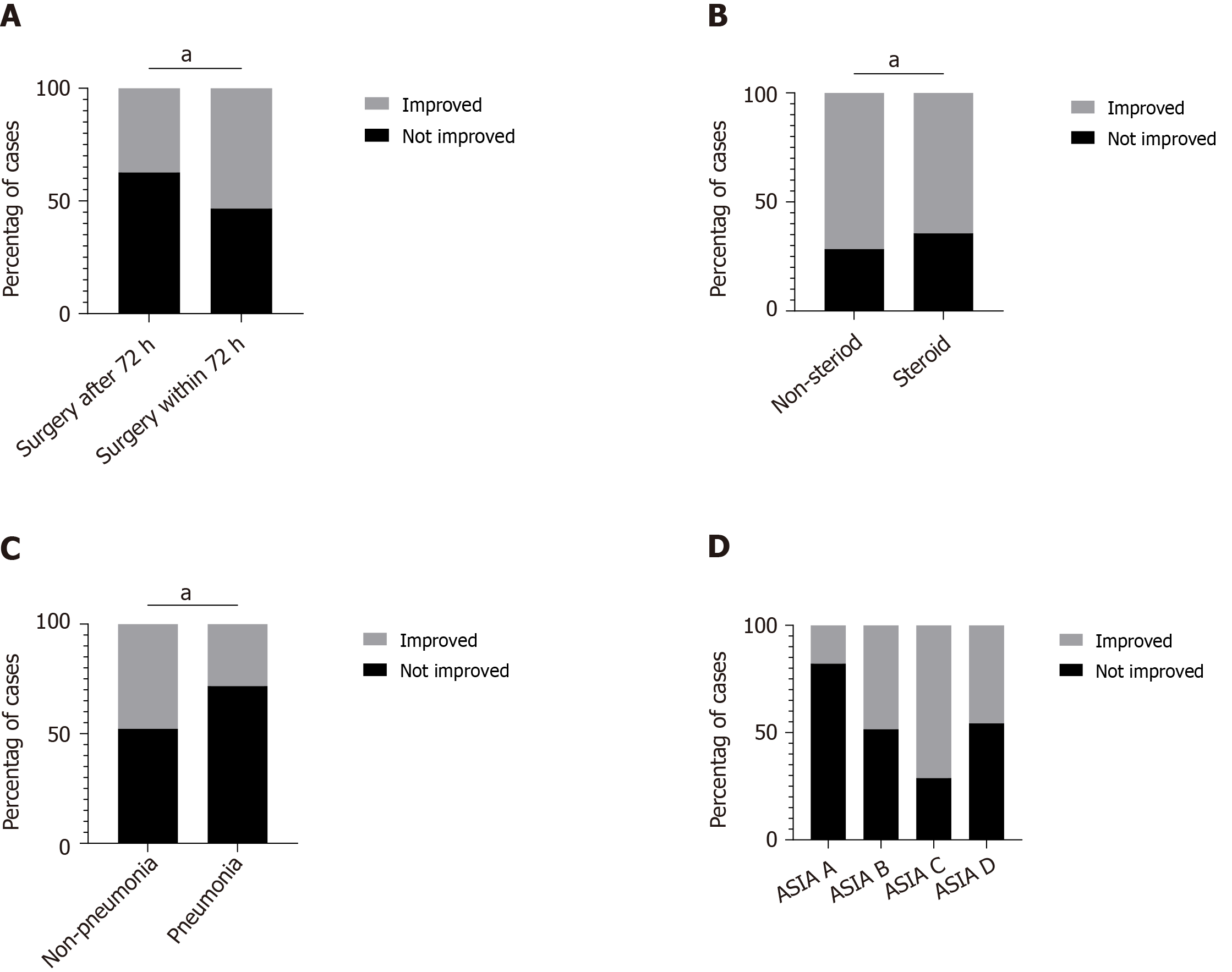
Of the 304 patients, 135 patients had improved follow-up ASIA grades (44.4%). Only 14 patients with ASIA grade A improved. There was a statistically significant difference in prognosis between patients who underwent surgery within 72 h and those who underwent surgery after 72 h (P < 0.05, Figure 3A). There were significant differences between the Steroid group and the Non-Steroid group only among patients with ASIA grades A and B (P < 0.05, Figure 3B). However, the incidence of pneumonia increased with steroid treatment (P < 0.05, Table 3). Patients with pneumonia had a worse prognosis than patients without pneumonia (P < 0.05, Figure 3C). Additionally, patients with an ASIA grade of A had the worst prognosis compared with other patients (P < 0.05, Figure 3D).
ATSCI severely affects daily life. The incidence of ATSCI is more common in young and middle-aged males. The cervical spine is the most commonly injured site. Frequent causes of injury are falls and traffic accidents. Beck et al[10] found that there were 706 cases of ATSCI, most of which were the result of transportation accidents or falls. The incidence of ATSCI resulting from falls increased by 9%/year (95%CI: 4%-15%). In the present study, of 304 patients, 44.4% had improved neurological function. Only 14 patients with ASIA grade A improved. The improvement rate was 17.9%. Of these patients, 5 improved from grade A to grade B, 6 improved from grade A to grade C, and 3 improved from grade A to grade D. None of these patients had normal neurological function at one-year follow up. At present, the guidelines and consensus indicate that surgery is an effective means of treating ASCI and that surgery can alleviate the symptoms of nerve compression. However, there are no standard or effective treatments for improving functional outcomes in these patients.
Our study found that patients with fracture and dislocation had a poorer prognosis than patients without fracture or dislocation, as these patients usually had complications such as spinal cord compression and thus the injury was severe. The shorter the time from onset to treatment (including surgery within 72 h and medication), the better the neurological prognosis might be. Yang et al[11] found that high-dose steroid therapy within 8 h and adequate spinal decompression after injury can effectively improve spinal cord function in thoracolumbar spinal injury. Prognosis was closely related to the timely treatment of patients in the early stage of the injury and the reduction of spinal cord compression. In addition, fewer complications indicated a better neurological prognosis. Patients with pneumonia had a worse prognosis. Hou et al[12,13] found that ASIA and moderate to severe respiratory complications were variables significantly correlated with tracheostomy. Jaja et al[14] found that pneumonia, wound infections, and sepsis (PWS) were the leading causes of acute mortality after ATSCI. Furthermore, as steroids can inhibit inflammation and reduce edema, they were often used as the first-line treatment in ATSCI[15]. However, the American Association of Neurological Surgeons has proposed guidelines issued in 2013 opposing the use of methylprednisolone as a routine treatment for ATSCI[16]. In recent years, an increasing number of clinical studies have shown that steroids have limited effects and benefits in ATSCI, and the use of high doses of steroids may cause serious complications, including gastrointestinal hemorrhage and respiratory tract infection[17-20]. Our study found that the prognosis of patients treated with surgery combined with steroid therapy was not significantly different from those treated with surgery alone, while patients with severe spinal cord injury (ASIA grade B patients) had an improved prognosis. However, the incidence of infections caused by steroids may increase.
This study was limited by the long course of spinal cord injury, slow recovery of neurological function, low improvement rate of the disastrous consequences of ATSCI and the current lack of mature treatments. Further improvements in the treatment plans are needed in order to preserve neurological function in patients. In addition, we also need to actively carry out randomized multicenter studies with improved sample size to provide more clinical evidence for the optimal management strategy in ATSCI patients.
Our study described the current clinical management of ATSCI patients with long-term follow-up and the findings of this study have important implications for future clinical practice. Surgery within 72 h resulted in a better prognosis. It was found that there was no significant difference in hospitalization time and prognosis between the Steroid group and the Non-Steroid group. However, patients with severe spinal cord injury (ASIA grades A and B) who underwent surgery combined with steroid therapy had a better prognosis than those who underwent surgery alone. The disastrous consequences of ATSCI and the lack of consensus on treatment require further study to improve the treatment strategy in order to obtain more reliable functional improvement.
Acute spinal cord injury is a common type of severe trauma in the emergency department, and can have catastrophic consequences in patients.
To describe the present treatment of acute traumatic spinal cord injury (ATSCI) and provide important suggestions for future clinical practice.
The objective of our study was to provide a systematic and basic theoretical basis for improving the treatment of ATSCI.
This retrospective study enrolled patients with ATSCI from 2012 to 2017, and recorded their demographic and clinical characteristics. Patients were followed-up at one year after discharge. The American Spinal Injury Association (ASIA) score was re-calculated, and the recovery of neurological function was evaluated according to ASIA guidelines.
A total of 440 ATSCI patients were enrolled in our study, and 304 of these patients were included in the final analysis. The results of the analysis indicated that ATSCI was more likely to occur in young and middle-aged males and the cervical spinal cord was the most commonly injured site. A statistically significant difference in prognosis was observed between patients who underwent surgery within 72 h and those who underwent surgery after 72 h (P < 0.05). A significant difference between the Steroid group and the Non-Steroid group in terms of outcome was noticed in the ASIA grade A and B subgroups (P < 0.05). In addition, patients with pneumonia had a worse prognosis when compared with those without pneumonia (P < 0.05).
Our study described the current situation in ATSCI patients with long-term follow-up and the findings in our study have important implications for future clinical practice. Surgery within 72 h resulted in a better prognosis. This study found that there was no significant difference in hospitalization time and prognosis between the Steroid group and the Non-Steroid group. However, patients with severe spinal cord injury (ASIA grades A and B) who underwent surgery combined with steroid therapy had a better prognosis than those who underwent surgery alone. The consequences of ATSCI are disastrous and there is still a lack of consensus on treatment. We need to further improve the treatment strategy in order to obtain more reliable functional improvement.
This research area requires randomized multicenter studies with a larger sample size to provide more clinical evidence for the optimal management strategy in ATSCI patients to achieve a better prognosis.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dinç T, Schietroma M S-Editor: Yan JP L-Editor: Webster JR P-Editor: Wang LL
| 1. | Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O'Connor KC, Garshick E. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313:2236-2243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 461] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 2. | Badhiwala JH, Wilson JR, Kwon BK, Casha S, Fehlings MG. A Review of Clinical Trials in Spinal Cord Injury Including Biomarkers. J Neurotrauma. 2018;35:1906-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Slotkin JR, Pritchard CD, Luque B, Ye J, Layer RT, Lawrence MS, O'Shea TM, Roy RR, Zhong H, Vollenweider I, Edgerton VR, Courtine G, Woodard EJ, Langer R. Biodegradable scaffolds promote tissue remodeling and functional improvement in non-human primates with acute spinal cord injury. Biomaterials. 2017;123:63-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Li X, Zhao Y, Cheng S, Han S, Shu M, Chen B, Chen X, Tang F, Wang N, Tu Y, Wang B, Xiao Z, Zhang S, Dai J. Cetuximab modified collagen scaffold directs neurogenesis of injury-activated endogenous neural stem cells for acute spinal cord injury repair. Biomaterials. 2017;137:73-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 5. | Ma YH, Zeng X, Qiu XC, Wei QS, Che MT, Ding Y, Liu Z, Wu GH, Sun JH, Pang M, Rong LM, Liu B, Aljuboori Z, Han I, Ling EA, Zeng YS. Perineurium-like sheath derived from long-term surviving mesenchymal stem cells confers nerve protection to the injured spinal cord. Biomaterials. 2018;160:37-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Bartus K, Galino J, James ND, Hernandez-Miranda LR, Dawes JM, Fricker FR, Garratt AN, McMahon SB, Ramer MS, Birchmeier C, Bennett DL, Bradbury EJ. Neuregulin-1 controls an endogenous repair mechanism after spinal cord injury. Brain. 2016;139:1394-1416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Kunte H, Farhadi HF, Sheth KN, Simard JM, Kronenberg G. Sulfonylureas--a novel treatment to reduce tissue damage after acute spinal cord injury? Lancet Neurol. 2015;14:352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Tran AP, Warren PM, Silver J. The Biology of Regeneration Failure and Success After Spinal Cord Injury. Physiol Rev. 2018;98:881-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 585] [Article Influence: 83.6] [Reference Citation Analysis (0)] |
| 9. | Tsolinas RE, Burke JF, DiGiorgio AM, Thomas LH, Duong-Fernandez X, Harris MH, Yue JK, Winkler EA, Suen CG, Pascual LU, Ferguson AR, Huie JR, Pan JZ, Hemmerle DD, Singh V, Torres-Espin A, Omondi C, Kyritsis N, Haefeli J, Weinstein PR, de Almeida Neto CA, Kuo YH, Taggard D, Talbott JF, Whetstone WD, Manley GT, Bresnahan JC, Beattie MS, Dhall SS. Transforming Research and Clinical Knowledge in Spinal Cord Injury (TRACK-SCI): an overview of initial enrollment and demographics. Neurosurg Focus. 2020;48:E6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Beck B, Cameron PA, Braaf S, Nunn A, Fitzgerald MC, Judson RT, Teague WJ, Lennox A, Middleton JW, Harrison JE, Gabbe BJ. Traumatic spinal cord injury in Victoria, 2007-2016. Med J Aust. 2019;210:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Yang ZW, Zhou F, Liu ZJ, Ji HQ, Tian Y, Zhang ZS. Factors influencing prognosis of thoracolumbar spinal injury combined with spinal cord injury. Zhonghua Chuangshang Zazhi. 2014;30:982-985. [DOI] [Full Text] |
| 12. | Hou YF, Lv Y, Zhou F, Tian Y, Ji HQ, Zhang ZS, Guo Y. Predictive model of tracheostomy in acute traumatic cervical spinal cord injury. Zhongguo Jizhu Jisui Zazhi. 2015;25:148-157. [DOI] [Full Text] |
| 13. | Hou YF, Lv Y, Zhou F, Tian Y, Ji HQ, Zhang ZS, Guo Y. Development and validation of a risk prediction model for tracheostomy in acute traumatic cervical spinal cord injury patients. Eur Spine J. 2015;24:975-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Jaja BNR, Jiang F, Badhiwala JH, Schär R, Kurpad S, Grossman RG, Harrop JS, Guest JD, Toups EG, Shaffrey CI, Aarabi B, Boakye M, Fehlings MG, Wilson JR. Association of Pneumonia, Wound Infection, and Sepsis with Clinical Outcomes after Acute Traumatic Spinal Cord Injury. J Neurotrauma. 2019;36:3044-3050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Bowers CA, Kundu B, Rosenbluth J, Hawryluk GW. Patients with Spinal Cord Injuries Favor Administration of Methylprednisolone. PLoS One. 2016;11:e0145991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, Harrigan MR, Rozelle CJ, Ryken TC, Theodore N; American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60:82-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 325] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 17. | Evaniew N, Noonan VK, Fallah N, Kwon BK, Rivers CS, Ahn H, Bailey CS, Christie SD, Fourney DR, Hurlbert RJ, Linassi AG, Fehlings MG, Dvorak MF; RHSCIR Network. Methylprednisolone for the Treatment of Patients with Acute Spinal Cord Injuries: A Propensity Score-Matched Cohort Study from a Canadian Multi-Center Spinal Cord Injury Registry. J Neurotrauma. 2015;32:1674-1683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Bydon M, Lin J, Macki M, Gokaslan ZL, Bydon A. The current role of steroids in acute spinal cord injury. World Neurosurg. 2014;82:848-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 19. | Liu Z, Yang Y, He L, Pang M, Luo C, Liu B, Rong L. High-dose methylprednisolone for acute traumatic spinal cord injury: A meta-analysis. Neurology. 2019;93:e841-e850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 137] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 20. | Liu LJW, Rosner J, Cragg JJ. Journal Club: High-dose methylprednisolone for acute traumatic spinal cord injury: A meta-analysis. Neurology. 2020;95:272-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |