Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.464
Peer-review started: December 2, 2019
First decision: December 11, 2019
Revised: December 19, 2019
Accepted: December 22, 2019
Article in press: December 22, 2019
Published online: January 26, 2020
Processing time: 45 Days and 11.9 Hours
Gallbladder adenomyomatosis (GAM) is a benign lesion, characterized by thickening of the gallbladder wall and a focal mass, which overlap with the features of gallbladder malignancy. Consequently, differential diagnosis of GAM from gallbladder cancer is difficult and approximately 20% of suspected malignant biliary strictures are postoperatively confirmed as benign lesions. Herein, we report a case in which a preoperative diagnosis of GAM was made by a combination of endoscopic and imaging techniques.
A 40-year-old man was referred to our hospital chiefly for a fever and right upper abdominal pain with dark urine. Enhanced computed tomography showed thickening of the gallbladder wall and a mass in the gallbladder neck with involvement of the hepatic bile ducts, which was suspected to be malignant. Gallbladder malignancy with bile duct invasion was ruled out by subsequent endoscopic examinations, including endoscopic retrograde cholangio-pancreatography, intraductal ultrasound, and SpyGlass. Endoscopic examinations showed a homogeneous hyperechoic lesion with smooth margins of benign bile duct stricture suggestive of inflammatory stenosis of the bile duct. The patient underwent laparoscopic cholecystectomy. GAM was postoperatively diagnosed and confirmed based on the histopathology results, which are consistent with the preoperative diagnosis. Notably, no malignant event occurred in the patient during a 12-mo follow-up period.
A combination of endoscopic techniques may help in the differential diagnosis of GAM from gallbladder cancer.
Core tips: It remains a challenge to make an accurate preoperative diagnosis of gallbladder adenomyomatosis (GAM) mainly due to the overlapping features between GAM and gallbladder cancer. In this case report, enhanced computed tomography findings were initially indicative of a malignant gallbladder lesions, which were subsequently diagnosed as GAM by a combination of endoscopic techniques. Our findings suggest that multiple endoscopies can improve the accuracy of GAM diagnosis and help in differential diagnosis between GAM and gallbladder cancer.
- Citation: Wen LJ, Chen JH, Chen YJ, Liu K. Utility of multiple endoscopic techniques in differential diagnosis of gallbladder adenomyomatosis from gallbladder malignancy with bile duct invasion: A case report. World J Clin Cases 2020; 8(2): 464-470
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/464.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.464
Gallbladder adenomyomatosis (GAM) is a benign tumor, and the imaging characteristics, such as thickening of the gallbladder wall and a focal mass, usually overlap with the findings in gallbladder malignancy. These similarities have posed considerable difficulties in making an accurate diagnosis of GAM, in particular, distinguishing GAM from gallbladder cancer. It has been reported that approximately 20% of suspected malignant biliary strictures were postoperatively confirmed as benign lesions[1]. Computed tomography (CT) is widely used in the preoperative assessment of gallbladder lesions[2]. However, CT imaging alone has been shown to reach an overall accuracy of only 70%-80% for biliary stenosis[3]. Until now, there has been no definite consensus on the optimal clinical approaches for indeterminate biliary strictures. As such, it is necessary to improve the accuracy of GAM diagnosis and differential diagnosis between GAM and gallbladder cancer. In the present paper, we illustrate a case in which a preoperative diagnosis of GAM was made by a combination of endoscopic and imaging techniques.
A 40-year-old man was referred to our hospital chiefly for a fever and right upper abdominal pain with dark urine.
The patient’s symptoms started 7 d ago with right upper pain and fever, which had worsened over the last 72 h.
He had no special medical history.
None.
The patient had upper abdominal pain without abdominal distension or vomiting, as well as yellow sclera and film. He had a body temperature of 37.5 °C, heart rate of 72 bpm, blood pressure of 116/68 mmHg, and respiratory rate of 15.
Total bilirubin was 138.8 µmol/L, direct bilirubin was 117.3 µmol/L, CA19-9 was 161.3 U/mL, CA-125 was 15.76 U/mL, AFP was 1.77 ng/mL, carcinoembryonic antigen was 1.29 ng/mL, C-reaction protein was 81.3 mg/L, neutrophil granulocyte percentage was 0.83, and IgG4 was 0.2 g/L.
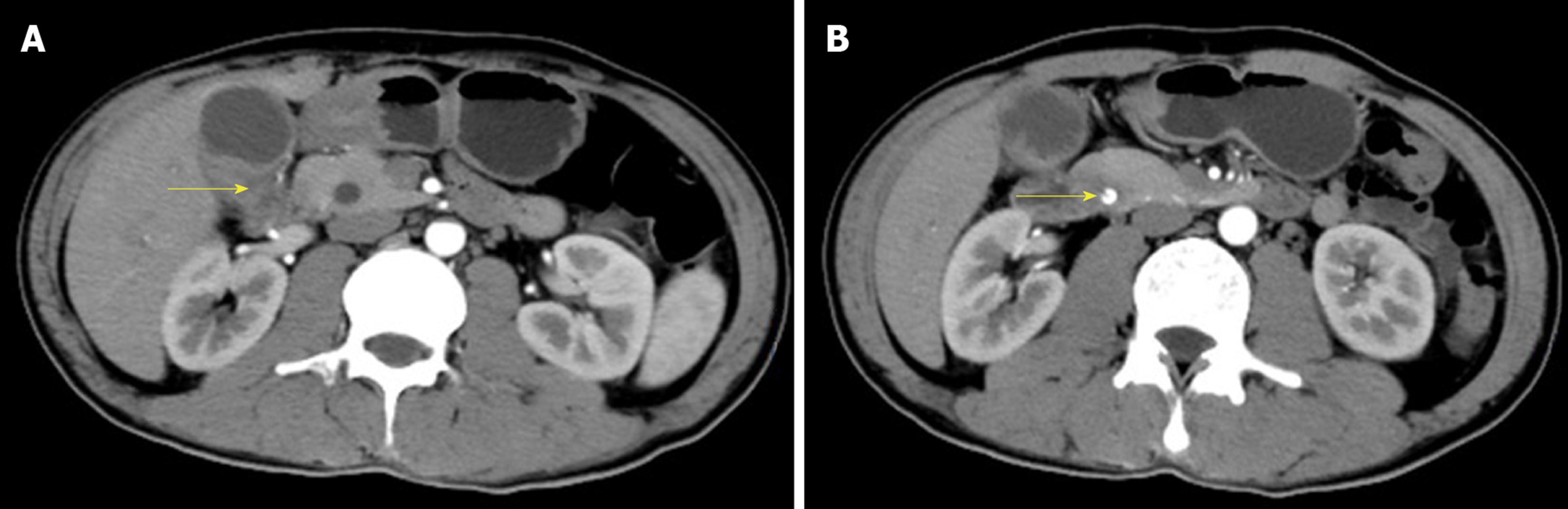
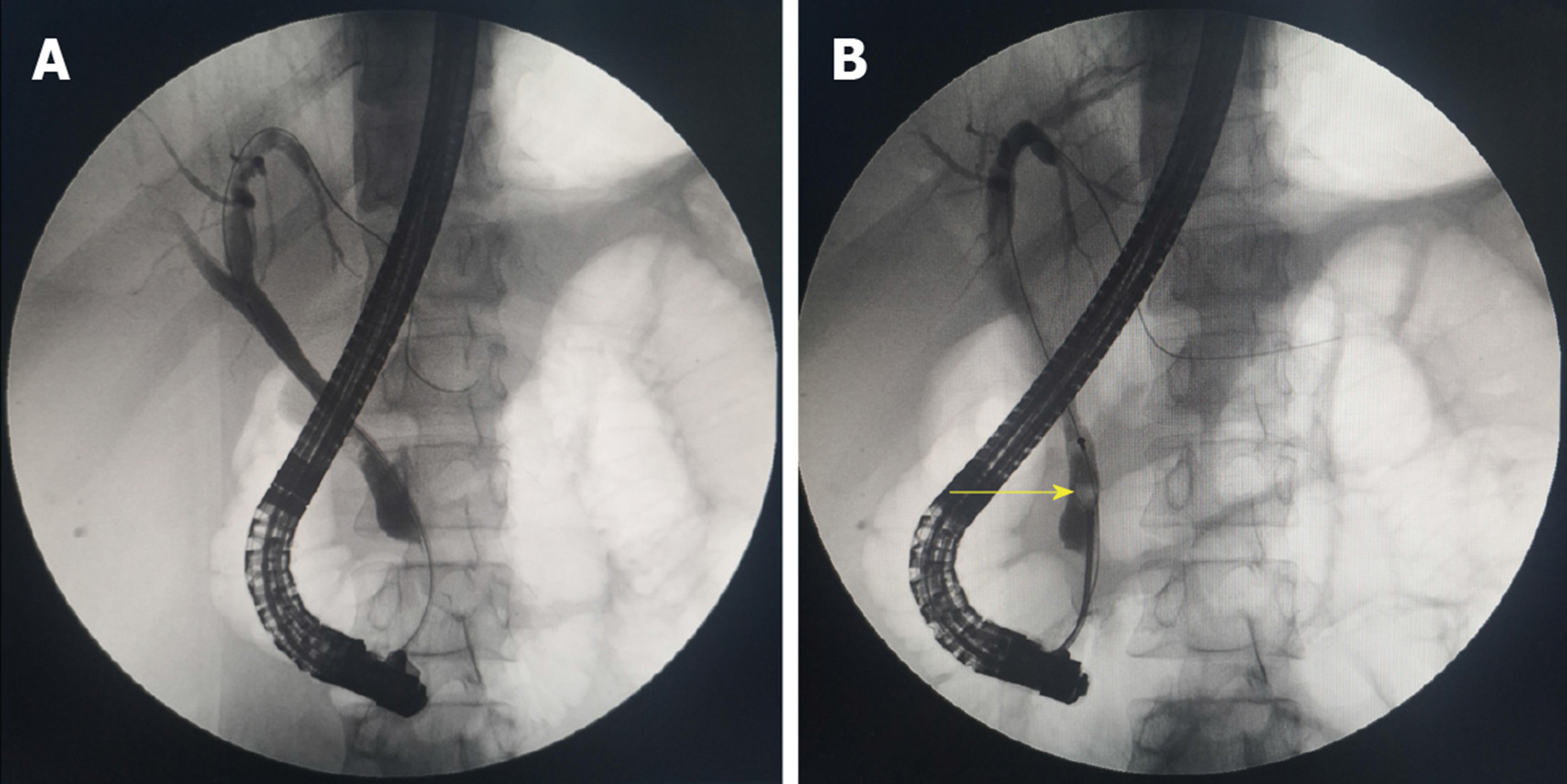
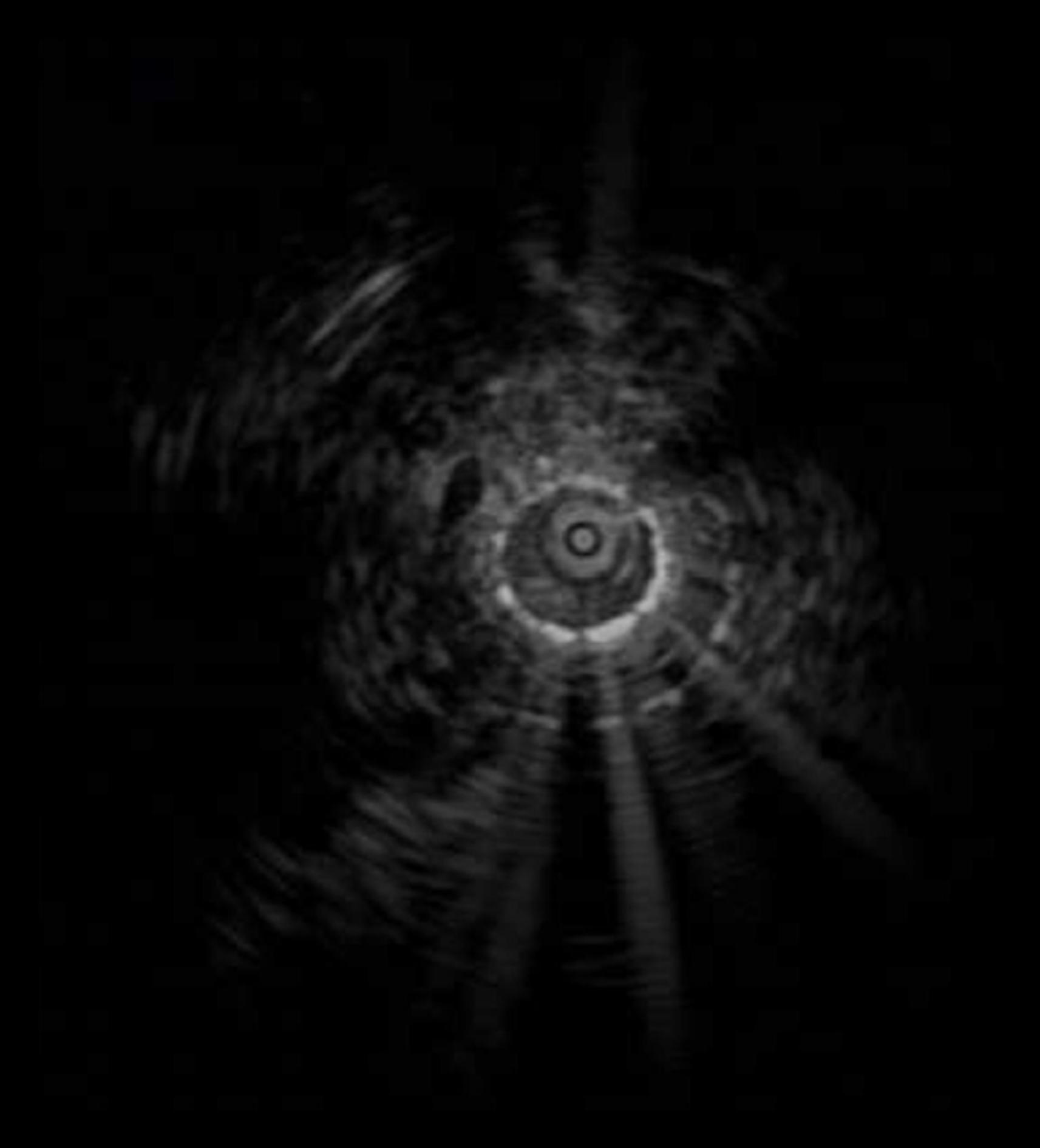
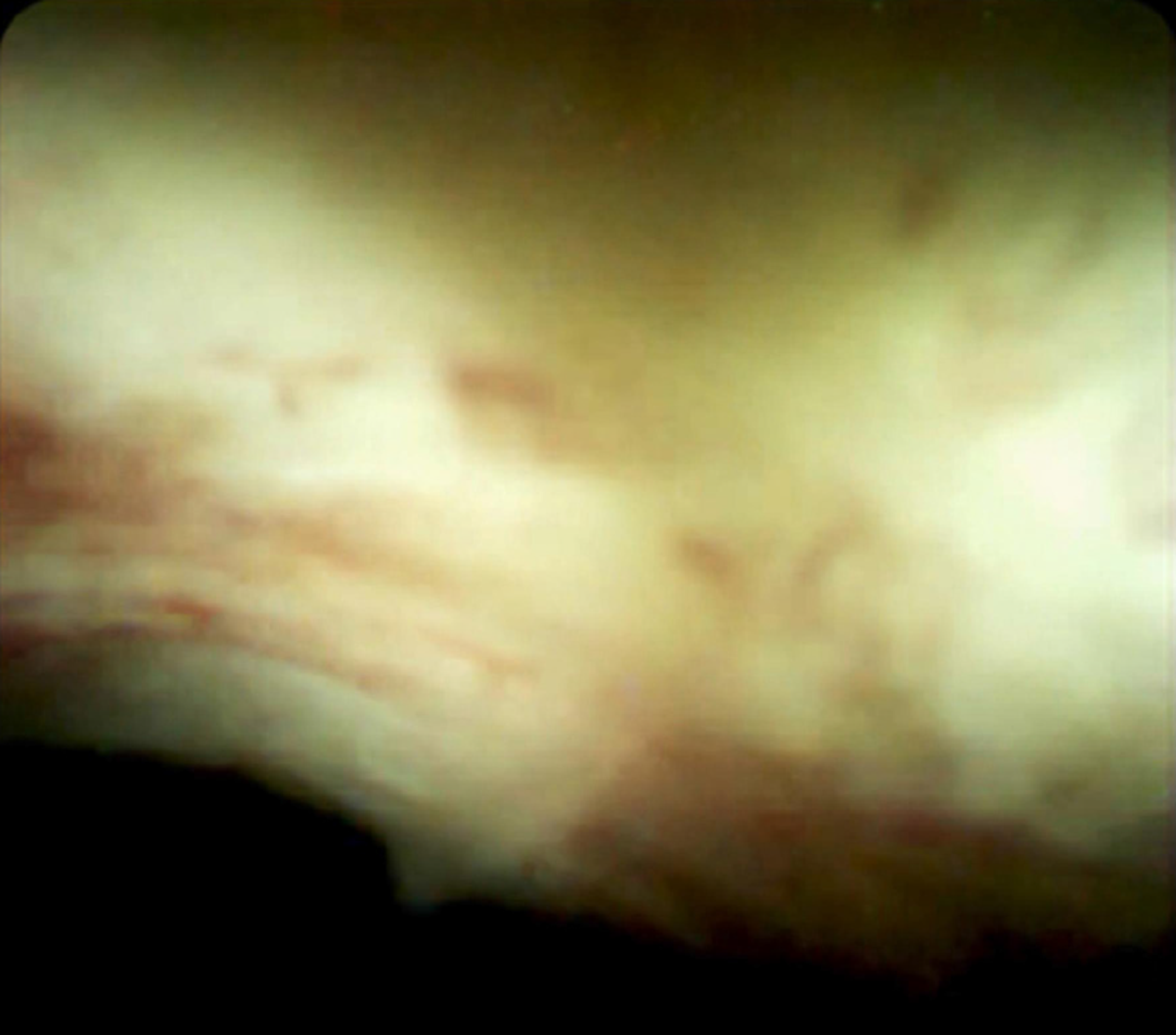
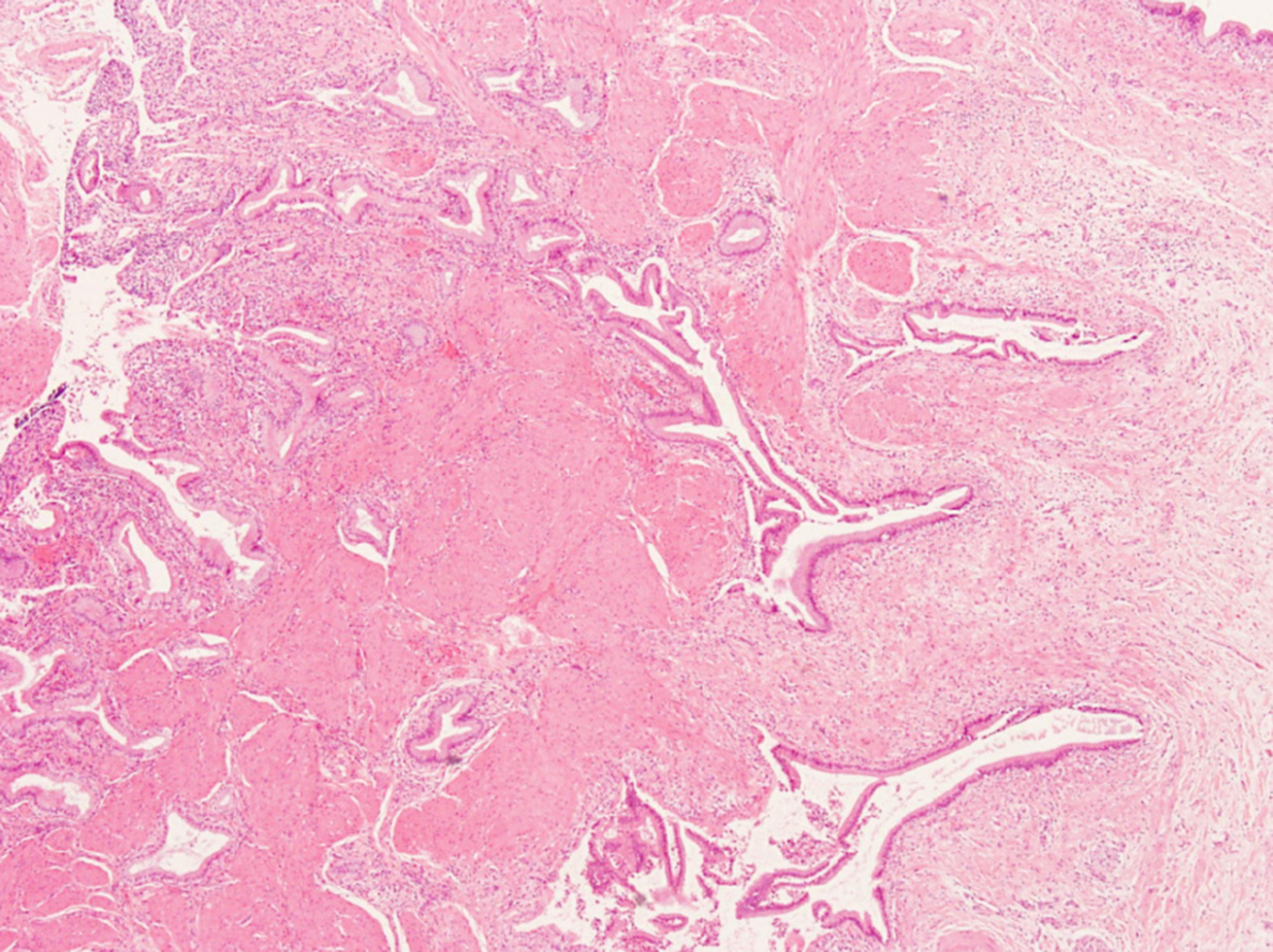
An enhanced CT scan revealed a mass at the neck of the gallbladder involving the bile ducts (Figure 1A) and a shadow was visualized at the end of the common bile duct (Figure 1B). Endoscopic retrograde cholangio-pancreatography (ERCP) showed bile duct dilatation (Figure 2A) and gallstones at the end of the common bile duct (Figure 2B), intraductal ultrasound (IDUS) suggested a benign bile duct stricture (Figure 3), inflammatory change in the bile duct mucosa was visualized by SpyGlass Direct Visualization System imaging (Figure 4), and final pathological examination revealed GAM with chronic cholecystitis and acute suppurative inflammation (Figure 5).
GAM and choledocholithiasis.
The patient underwent laparoscopic cholecystectomy.
Fortunately, neither recurrent GAM nor malignant tumor was observed in the patient during a 12-mo follow-up period.
Gallbladder carcinoma is the most common malignant tumor in the biliary system[4]. Some benign gallbladder diseases are misdiagnosed as gallbladder carcinoma, resulting in unnecessary surgery. For instance, GAM is an excessively proliferative disease of the gallbladder epithelium with intramural diverticula (Rokitanskye Aschoff sinuses) extending into the thickened muscular layer[2] and its imaging features have some overlaps with those of gallbladder carcinoma when it presents as focal thickening at the body and fundus and a mass with irregularly soft tissue density in the gallbladder, which may simulate a malignancy, resulting in a false-positive diagnosis of gallbladder carcinoma[5]. On the contrary, patients who suffer from gallbladder cancer may present with acute cholecystitis, misdiagnosed as a benign lesion. It has been reported that the hidden incidence of gallbladder cancer combined with cholecystitis ranges from 1%-9%[4]. Gallbladder carcinoma originating from the neck can invade the cystic and extrahepatic bile duct, making it difficult to distinguish from extrahepatic cholangiocarcinoma[6,7]. When a stricture of the mid-portion of the extrahepatic bile duct is found in patients presenting with obstructive jaundice, careful evaluation of the cystic duct and gallbladder neck is necessary to rule out gallbladder cancer with metastasis.
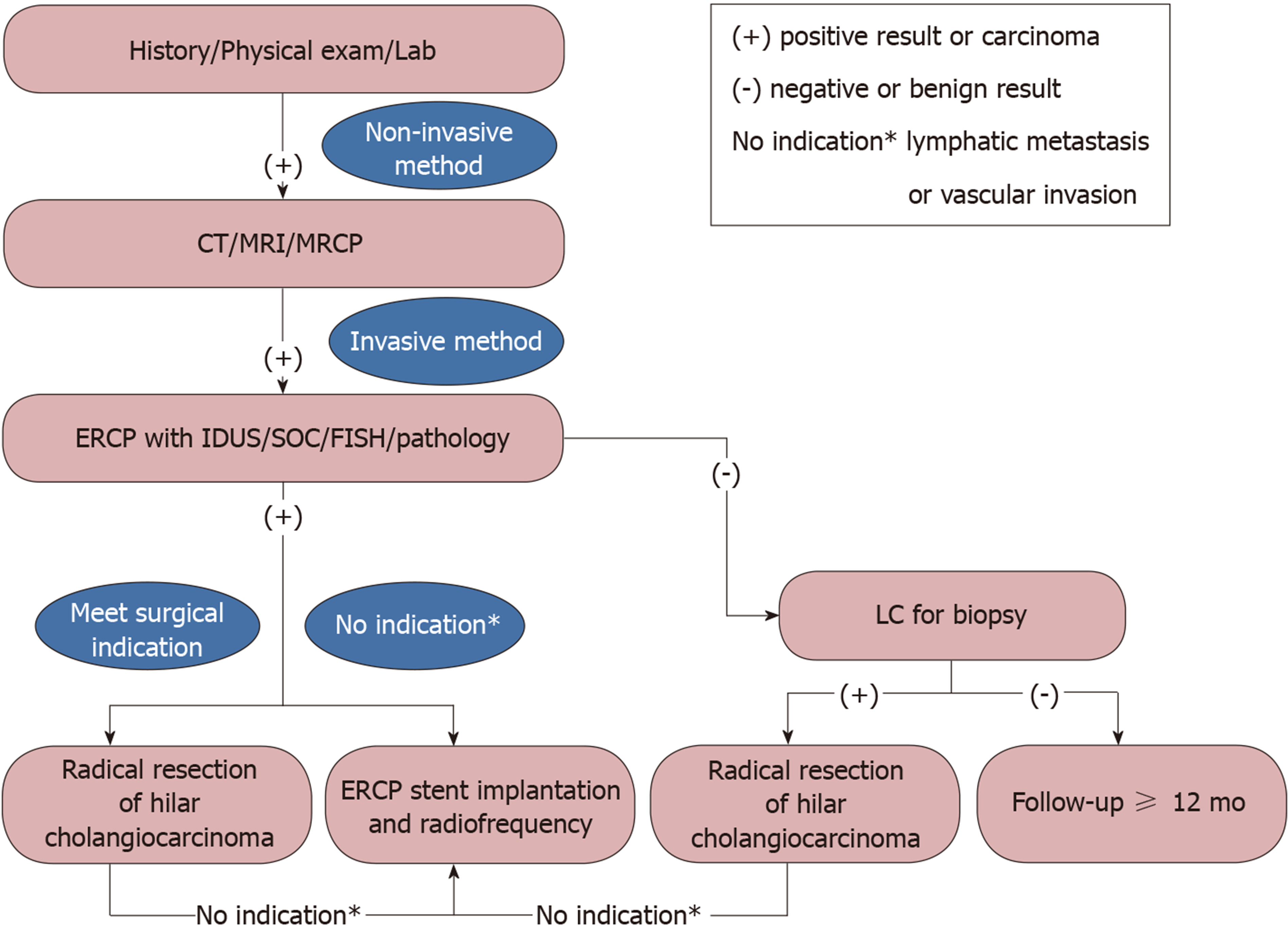
With recently developed novel biomarkers and endoscopic techniques, unnecessary surgeries on benign strictures of the bile duct have been greatly reduced. However, no single approach has been reliable in the differential diagnosis of benign and malignant lesions in the gallbladder mainly due to insufficient sensitivity, low specificity, and inaccuracy. By reviewing the published systematic reviews and meta-analysis (Table 1), we identified the diagnostic indices for the evaluation of suspected malignant biliary strictures (Table 1)[1,8-14]. We found that the clinical approach of various endoscopies in combination could significantly improve the diagnostic accuracy of indeterminate biliary stricture. It is worth noting in particular that contrast-enhanced ultrasound is very reliable in the differential diagnosis of gallbladder cancer with broad prospects[15,16]. CA19-9 should be used cautiously for patients with biliary obstruction because of the potential for a pseudo increase[17]. In this case report and review of the literature, we propose a strategy for the evaluation and preoperative diagnosis of gallbladder-occupying lesions with bile duct invasion (Figure 6), which may have great preoperative diagnostic utility. First, a detailed medical history should be obtained, with physical and laboratory examinations, along with abdominal ultrasound to provide the initial evidence for a non-invasive imaging method such as CT or magnetic resonance cholangiopancreatography. These imaging modalities can reveal both the hilar bile duct and gall bladder, which can guide future treatment. Second, an invasive method such as ERCP with IDUS/SpyGlass/probe-based confocal laser endomicroscopy/fluorescence in situ hybridization or pathology can be used as the primary measure. If endoscopy and laparoscopic cholecystectomy are positive, radical resection of hilar cholangiocarcinoma must be undertaken. If lymphatic metastasis or vascular invasion is found, ERCP stent implantation and radiofrequency ablation can be performed. Otherwise, 12 mo of follow-up is usually necessary.
| Diagnostic modality | Sensitivity (%) | Specificity (%) | Accuracy (%) |
| ERCP brush cytology + biopsy | 59 | 100 | 73 |
| CT/MDCT | 77 | 63 | 75 |
| MRI/MRCP | 88 | 95 | 80 |
| CA 19-9 > 100 | 75 | 80 | 78 |
| SOC-biopsy | 60 | 98 | 79 |
| FISH | 70 | 89 | 87 |
| EUS | 88 | 90 | 74 |
| ERCP + CLE | 90 | 72 | 81 |
| ERCP + IDUS | 93 | 89 | 91 |
In summary, preoperative diagnosis of GAM is challenging, particularly when it presents imaging features similar to those of gallbladder carcinoma. The findings in this case study suggest that the use of multiple endoscopic techniques in combination may improve the accuracy of GAM diagnosis and benefit the differential diagnosis of GAM from gallbladder cancer.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Soresi M S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Bowlus CL, Olson KA, Gershwin ME. Evaluation of indeterminate biliary strictures. Nat Rev Gastroenterol Hepatol. 2016;13:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Heinzow HS, Kammerer S, Rammes C, Wessling J, Domagk D, Meister T. Comparative analysis of ERCP, IDUS, EUS and CT in predicting malignant bile duct strictures. World J Gastroenterol. 2014;20:10495-10503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 49] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Saluja SS, Sharma R, Pal S, Sahni P, Chattopadhyay TK. Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: a prospective study. HPB (Oxford). 2007;9:373-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Yoshimitsu K, Irie H, Aibe H, Tajima T, Nishie A, Asayama Y, Matake K, Yamaguchi K, Matsuura S, Honda H. Well-differentiated adenocarcinoma of the gallbladder with intratumoral cystic components due to abundant mucin production: a mimicker of adenomyomatosis. Eur Radiol. 2005;15:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Kim SW, Kim HC, Yang DM, Ryu JK, Won KY. Gallbladder carcinoma: causes of misdiagnosis at CT. Clin Radiol. 2016;71:e96-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Nakata T, Kobayashi A, Miwa S, Soeda J, Miyagawa S. Impact of tumor spread to the cystic duct on the prognosis of patients with gallbladder carcinoma. World J Surg. 2007;31:155-61; discussion 162-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Shukla PJ, Barreto SG, Shrikhande SV, Ramadwar MR, Deodhar KK, Mehta S, Patil P, Mohandas KM. Simultaneous gallbladder and bile duct cancers: revisiting the pathological possibilities. HPB (Oxford). 2008;10:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Clemente G, Nuzzo G, De Rose AM, Giovannini I, La Torre G, Ardito F, Giuliante F. Unexpected gallbladder cancer after laparoscopic cholecystectomy for acute cholecystitis: a worrisome picture. J Gastrointest Surg. 2012;16:1462-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Cui XY, Chen HW. Role of diffusion-weighted magnetic resonance imaging in the diagnosis of extrahepatic cholangiocarcinoma. World J Gastroenterol. 2010;16:3196-3201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Gonda TA, Glick MP, Sethi A, Poneros JM, Palmas W, Iqbal S, Gonzalez S, Nandula SV, Emond JC, Brown RS, Murty VV, Stevens PD. Polysomy and p16 deletion by fluorescence in situ hybridization in the diagnosis of indeterminate biliary strictures. Gastrointest Endosc. 2012;75:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Mohamadnejad M, DeWitt JM, Sherman S, LeBlanc JK, Pitt HA, House MG, Jones KJ, Fogel EL, McHenry L, Watkins JL, Cote GA, Lehman GA, Al-Haddad MA. Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest Endosc. 2011;73:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 155] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 12. | Xie C, Aloreidi K, Patel B, Ridgway T, Thambi-Pillai T, Timmerman G, Khan A, Atiq M. Indeterminate biliary strictures: a simplified approach. Expert Rev Gastroenterol Hepatol. 2018;12:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Fugazza A, Gaiani F, Carra MC, Brunetti F, Lévy M, Sobhani I, Azoulay D, Catena F, de'Angelis GL, de'Angelis N. Confocal Laser Endomicroscopy in Gastrointestinal and Pancreatobiliary Diseases: A Systematic Review and Meta-Analysis. Biomed Res Int. 2016;2016:4638683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 14. | Park HJ, Kim SH, Jang KM, Choi SY, Lee SJ, Choi D. The role of diffusion-weighted MR imaging for differentiating benign from malignant bile duct strictures. Eur Radiol. 2014;24:947-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Serra C, Felicani C, Mazzotta E, Gabusi V, Grasso V, De Cinque A, Giannitrapani L, Soresi M. CEUS in the differential diagnosis between biliary sludge, benign lesions and malignant lesions. J Ultrasound. 2018;21:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Sidhu PS, Cantisani V, Dietrich CF, Gilja OH, Saftoiu A, Bartels E, Bertolotto M, Calliada F, Clevert DA, Cosgrove D, Deganello A, D'Onofrio M, Drudi FM, Freeman S, Harvey C, Jenssen C, Jung EM, Klauser AS, Lassau N, Meloni MF, Leen E, Nicolau C, Nolsoe C, Piscaglia F, Prada F, Prosch H, Radzina M, Savelli L, Weskott HP, Wijkstra H. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018;39:e2-e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 653] [Cited by in RCA: 587] [Article Influence: 83.9] [Reference Citation Analysis (1)] |
| 17. | Pearce S, Thornes H, Carr D, Tanner A. Diagnostic pitfall; interpretation of CA 19-9 concentrations in the presence of hepatic dysfunction. Gut. 1994;35:707-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |