Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.404
Peer-review started: November 14, 2019
First decision: December 12, 2019
Revised: December 18, 2019
Accepted: December 22, 2019
Article in press: December 22, 2019
Published online: January 26, 2020
Processing time: 62 Days and 18.4 Hours
Goodpasture syndrome (GS) is a rare disease, the morbidity of which is estimated to be 0.5-0.8 per million per year. Hemorrhage is the most serious complication in renal biopsy. Despite the fact that both GS and hemorrhage after renal biopsy are rare, it has not been reported that they are likely to occur in the same patient.
A 30-year-old man with diffuse pulmonary hemorrhage and rapid progressive renal function caused by anti-glomerular basement membrane disease presented atypical symptoms without hemoptysis, accompanied by life-threatening hypoxemia. Plasmapheresis was performed, and glucocorticoids and cyclophosphamide were administered. The patient started to show signs of improvement. Percutaneous renal biopsy is an appropriate diagnostic measure that is commonly safe, but this patient experienced hemorrhage after operation, thus necessitating embolization of the renal artery to stop the bleeding. The patient’s condition was improved, and the serum anti-glomerular basement membrane antibody level was 106 AU/mL (normal range: < 24 AU/mL) and slowly decreased. His discharge medications were oral daily prednisone (30 mg) and continued maintenance hemodialysis.
GS is a rare organ-specific autoimmune disease that is invariably ubiquitous in the lung and kidney areas. Renal biopsy is the appropriate procedure for the treatment of GS disease, although it is an invasive measure.
Core tip: Goodpasture syndrome was first identified by Dr. Ernest Goodpasture, who described it as an association between alveolar hemorrhage and glomerulonephritis. We report on a young male patient with life-threatening pulmonary hemorrhage without hemoptysis, accompanied by hemorrhage after renal biopsy. This case highlights the critical importance of prompt diagnosis and initiation of therapy. However, preventive measures, such as the addition of fresh plasma, should be considered to decrease the incidence of hemorrhage in similar situations, especially for dialysis patients.
- Citation: Li WL, Wang X, Zhang SY, Xu ZG, Zhang YW, Wei X, Li CD, Zeng P, Luan SD. Goodpasture syndrome and hemorrhage after renal biopsy: A case report. World J Clin Cases 2020; 8(2): 404-409
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/404.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.404
Goodpasture syndrome (GS) was first identified by Dr. Ernest Goodpasture, who described it as an association between alveolar hemorrhage and glomerulonephritis[1]. It is a rare disease, the morbidity of which is estimated to be 0.5-0.8 per million per year[2,3]. It can be mediated by anti-glomerular basement membrane (GBM) antibodies and is also the cause of rapidly progressive glomerulonephritis as well as diffuse alveolar hemorrhage[4]. The chest radiological findings were bilateral diffuse exudation, but lung cancer must be identified[5]. There was report that diffusion tensor imaging is correlated with proteinuria[6]. The morbidity is higher in men aged 20-30 years and women of older ages. GS is an autoimmune disorder characterized by autoantibodies directed against the alpha 3 chain of type IV collagen expressed in the glomerular or alveolar basement membrane[4].
The typical presentation is a combination of renal and pulmonary insufficiency. Hemoptysis is the most common symptom when the disease moves to the lung area, followed by symptoms such as cough, shortness of breath, or dyspnea. When affecting the kidneys, it may trigger hematuria or edema, high blood pressure, and oliguria.
Renal biopsy is the preferred invasive procedure to substantiate the diagnosis and prognosis of anti-GBM disease[7]. Hemorrhage is the most serious complication that can be depicted as a spectrum from hematuria to asymptomatic hemorrhage or death in renal biopsy.
We report on a young male patient with life-threatening pulmonary hemorrhage without hemoptysis, accompanied by hemorrhage after renal biopsy.
A 30-year-old Chinese man was admitted to our emergency department on August 28, 2019 with diarrhea, vomiting, and anuria that had been lasting for one week.
One week before admission, the patient experienced diarrhea, vomiting, and oliguria, and the symptoms could not be alleviated. He did not cough or show any symptoms of dyspnea or hemoptysis.
A previous routine investigation showed normal renal function (serum creatinine 1 year prior: 76 µmol/L). There was no history of special medicine use, including analgesics, illicit drug use, or alcohol abuse.
Physical examination showed no significant abnormalities (there were no bilateral rales heard or peripheral edema). His blood pressure was 129/72 mmHg, his pulse was 101 beats per minute, his peripheral oxygen saturation was 95% in ambient air, and his temperature was 36.5 °C.
On admission, serum laboratory data revealed the following values: hemoglobin, 53 g/L; creatinine, 2560 µmol/L; blood urea nitrogen, 51.5 mmol/L; K, 6.4 mmol/L; and C-reactive protein, 78 mg/L. Additionally, arterial blood gas analysis suggested that the oxygen partial pressure was 76 mmH2O, while the coagulation test showed that the fibrinogen level was 9.22 g/L. There were neither schistocytes on peripheral smears nor negative Coombs test results. Liver function was normal.
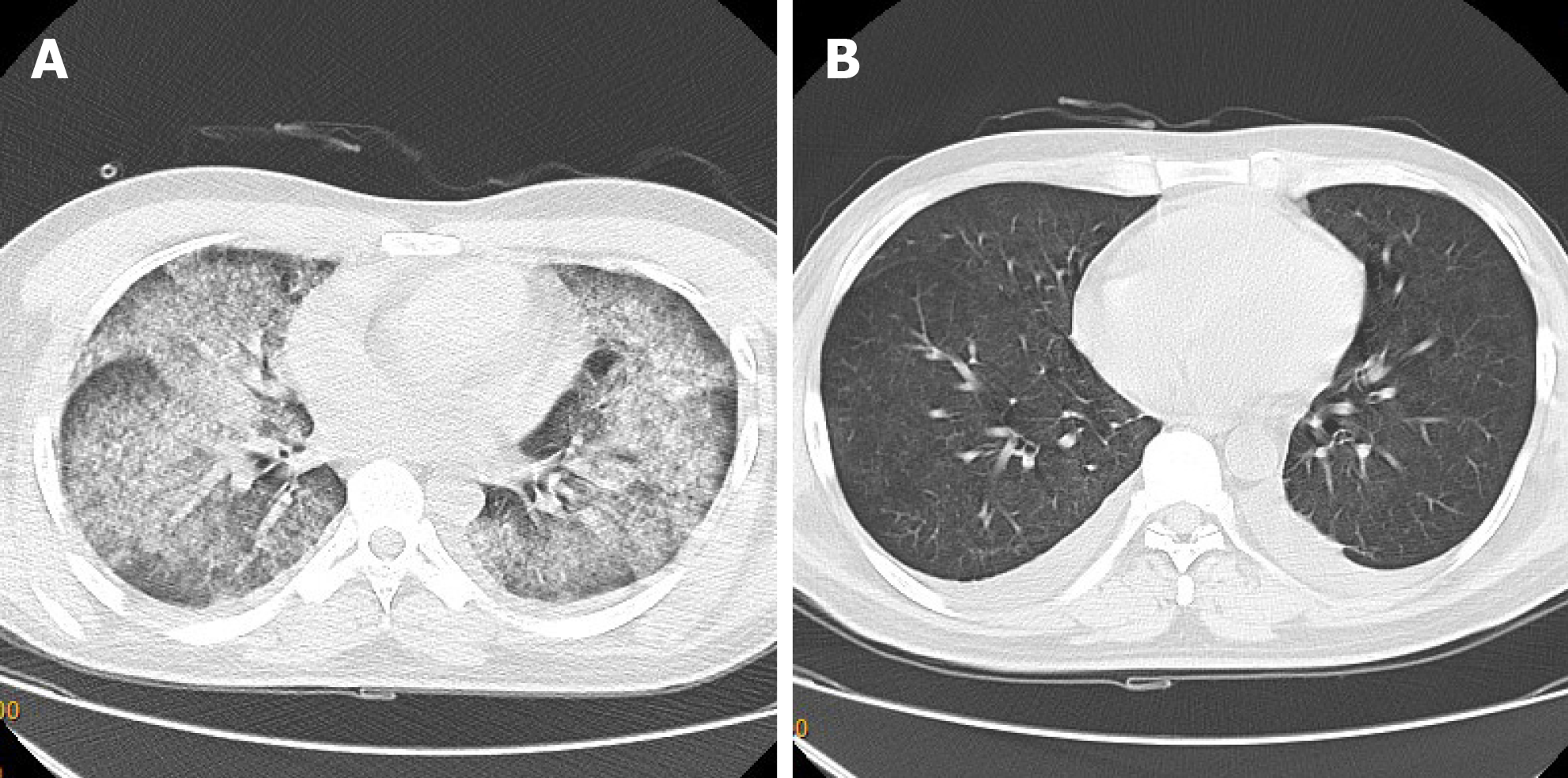
A computer tomography scan of the chest revealed a sign of bilateral diffuse exudation (Figure 1).
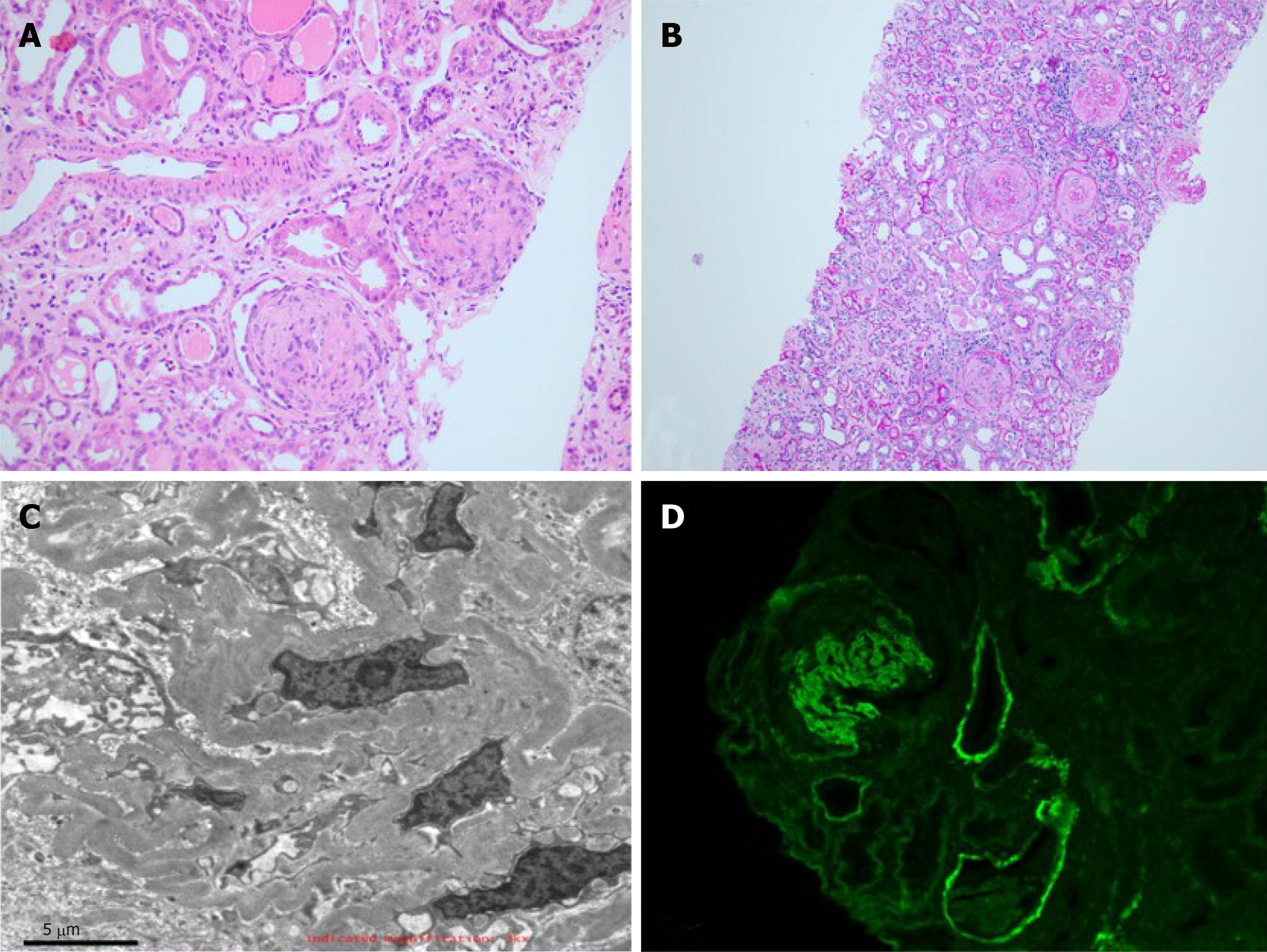
The histological examination of the renal biopsy demonstrated 33 glomeruli, of which 5 were globally sclerotic and 28 were crescent, and there was no duplication of basement membranes. Immunohistology revealed positive linear deposition of IgG(3+) and C3(2+) along the GBM; IgA, IgM PLA2R, and C1q were negative. According to additional tests, IgG1(3+), IgG2(1+), IgG3(-), and IgG4(3+) were positive. Forty percent of the tubulointerstitial cells were damaged multifocally with infiltration of inflammatory cells. Electron microscopy showed the occlusion of the glomerular capillary loops, which exuded plasma-like substances, and the infiltration of inflammatory cells in the interstitial region (Figure 2).
Further diagnostic work-up illustrated high concentrations of anti-GBM antibody (> 500 AU/mL), negative anti-neutrophil cytoplasmic antibody, and normal C3 concentrations.
We corrected the diagnosis from acute kidney injury to Goodpasture syndrome according to the typical imaging manifestation and a high titer of serum anti-GBM antibody (> 500 AU/mL).
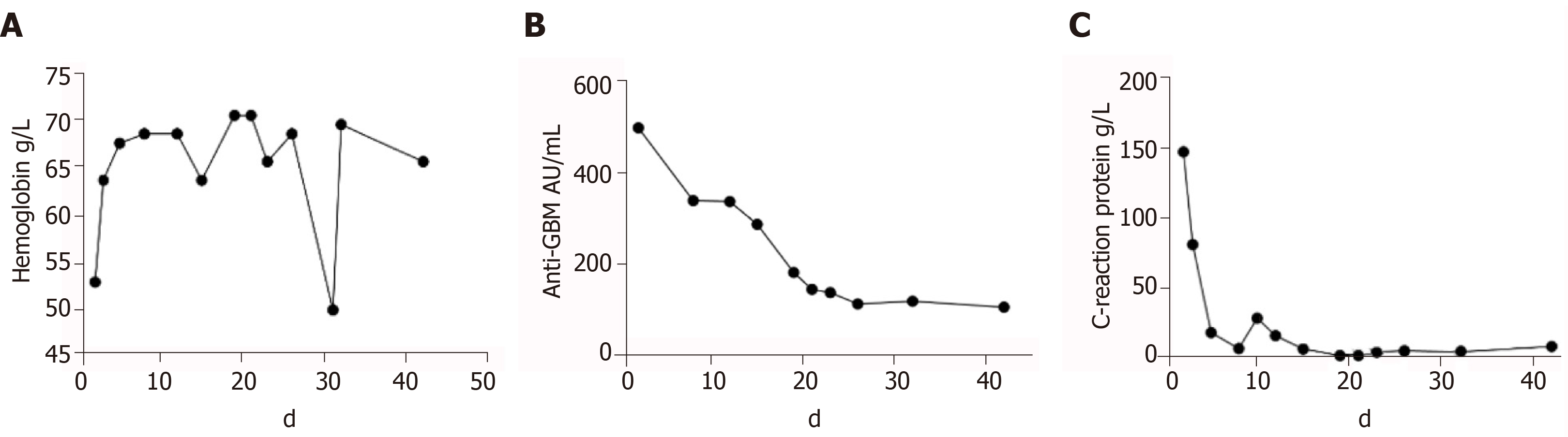
We immediately initiated plasmapheresis (single plasmapheresis, exchange dosage: 4000 mL fresh frozen plasma calculated by 1.0 plasma volume) and continued continuous renal replacement therapy. Meanwhile, we started to inject methylprednisolone (500 mg/d, 3 d in total) and cyclophosphamide (0.4 g/d, 2 d in total) on the same day after dialysis. The patient’s condition was improved, and his hemoglobin remained stable at 65 g/L without blood transfusion. The anti-GBM antibody decreased gradually after the performance of 35 plasmapheresis sessions in total, and the reexamination image also evidently improved. Therefore, we decided to prepare for renal biopsy.
Because the patient was young and had strong willingness to comprehend the prognosis, renal biopsy was performed at intervals of plasmapheresis after surgical contraindications were excluded. The operation was successful overall, and regular measures such as injecting thrombin and compression bandage were performed, but the patient complained of osphyalgia after the procedure when his blood pressure and hemoglobin started to drop. We had to stabilize his vital signs and initiate a blood transfusion. Radiography showed that the renal artery was bleeding. Subsequently, embolization of the renal artery occurred (Figure 3). The patient’s condition eventually stabilized.
The patient’s condition was improved, but his renal function was not recovered. When he was discharged on October 27, his serum anti-GBM antibody level was 106 AU/mL (normal range: < 24 AU/mL) and slowly decreased (Figure 4). His discharge medications were oral daily prednisone (30 mg) and continued maintenance hemodialysis.
Despite the fact that both the GS and hemorrhage of renal biopsy are rare, it has not been reported that they are likely to happen in the same patient[8]. It is also unusual that GS can be accompanied by a severe lesion in the lung even in the absence of hemoptysis[9].
The recommended regular therapies are plasmapheresis and corticosteroids. Moreover, immunosuppressive agents such as cyclophosphamide have dramatically improved prognosis. In this case, we initiated plasmapheresis and corticosteroid therapy immediately after we detected anti-GBM antibodies in the patient’s circulation. In addition, we started γ-globin impact therapy (20 g/d). The latest report suggested that rituximab may represent an additional therapy in the induction treatment of anti-GBM disease[10]. However, the therapy, which includes corticosteroids and rituximab, failed to be adopted due to the risk of infection, but its current therapeutic effect was proven to be adequate. Thus, it can serve as an alternative therapy when the patient’s condition is difficult to control.
A recent large study that included 9288 biopsies reported hemorrhage necessitating blood transfusion in 0.9% of cases and surgical intervention in 0.2% of cases[11]. However, the incidence of hemorrhage was drastically increased in the dialysis patient, even though the biopsy was performed at intervals of plasmapheresis and the coagulation remained normal. Some researchers have suggested the addition of fresh human plasma within 3 d of the invasive procedure, but a consensus has not been reached.
In conclusion, GS is a rare organ-specific autoimmune disease that is invariably ubiquitous in the lung and kidney areas. Renal biopsy is the appropriate procedure for the treatment of GS disease, although it is an invasive measure. However, preventive measures, such as the addition of fresh plasma, should be considered to decrease the incidence of hemorrhage for similar situations, especially for dialysis patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Razek AA, Zhou M S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Goodpasture EW. Landmark publication from The American Journal of the Medical Sciences: The significance of certain pulmonary lesions in relation to the etiology of influenza. Am J Med Sci. 2009;338:148-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Tang W, McDonald SP, Hawley CM, Badve SV, Boudville NC, Brown FG, Clayton PA, Campbell SB, de Zoysa JR, Johnson DW. Anti-glomerular basement membrane antibody disease is an uncommon cause of end-stage renal disease. Kidney Int. 2013;83:503-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Shiferaw B, Miro V, Smith C, Akella J, Chua W, Kim Z. Goodpasture's Disease: An Uncommon Disease With an Atypical Clinical Course. J Clin Med Res. 2016;8:52-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Marques C, Plaisier E, Cacoub P, Cadranel J, Saadoun D. [Review on anti-glomerular basement membrane disease or Goodpasture's syndrome]. Rev Med Interne. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Razek AA. Diffusion magnetic resonance imaging of chest tumors. Cancer Imaging. 2012;12:452-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Razek AAKA, Al-Adlany MAAA, Alhadidy AM, Atwa MA, Abdou NEA. Diffusion tensor imaging of the renal cortex in diabetic patients: correlation with urinary and serum biomarkers. Abdom Radiol (NY). 2017;42:1493-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Podzolkov VI, Makhnach GK, Ishina TI, Ponomarev AB, Medvedev ID. Difficulties in Goodpasture's syndrome diagnosing. Ter Arkh. 2019;91:64-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Longo L, Greco A, Rea A, Lo Vasco VR, De Virgilio A, De Vincentiis M. Relapsing polychondritis: A clinical update. Autoimmun Rev. 2016;15:539-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Hellmark T, Segelmark M. Diagnosis and classification of Goodpasture's disease (anti-GBM). J Autoimmun. 2014;48-49:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 10. | Touzot M, Poisson J, Faguer S, Ribes D, Cohen P, Geffray L, Anguel N, François H, Karras A, Cacoub P, Durrbach A, Saadoun D. Rituximab in anti-GBM disease: A retrospective study of 8 patients. J Autoimmun. 2015;60:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Tøndel C, Vikse BE, Bostad L, Svarstad E. Safety and complications of percutaneous kidney biopsies in 715 children and 8573 adults in Norway 1988-2010. Clin J Am Soc Nephrol. 2012;7:1591-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 188] [Article Influence: 14.5] [Reference Citation Analysis (0)] |